Pathology Test 2
1/169
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
170 Terms
What are the three heart layers
Pericardium
Myocardium
Endocardium
Describe the flow of blood through the heart
- The left side of the heart pumps oxygenated blood through the aorta to the body.
- The vena cava carry deoxygenated blood from the body to the right atria.
- The right side of the heart pumps deoxygenated blood through the pulmonary trunk to the lungs.
- Pulmonary veins bring oxygenated blood from the lungs to the left atria.
What is coronary artery disease
a disorder in which plaque accumulates in the coronary arteries, causing narrowing and a reduction in blood supply to the heart tissues.
This increases risk of angina, due to decreased blood flow to the heart, or myocardial infarction, as plaque can rupture causing a blood clot to form via the help of immune cells.
What is angina?
A condition in which the heart muscles do not get enough blood supply, resulting from the blood supply being insufficient to meet the demands of the myocardium.
It usually implies narrowing or partially blocked coronary arteries.
It tends to occur when the hearts demands are increased, such as exercise, emotional stress, cold weather, or hypothyroidism, as these states increase demands of the myocardium, which are unable to be met by coronary blood vessels.
What are the risk factors for angina
- Family history
- Smoking
- Diabetes
- Hypertension
- Hyperlipidaemia
- Obesity
What are the two types of Angina?
Stable Angina
The more common form of angina.
It is episodic chest pain or discomfort which typically occurs with activity or stress, lasting 2 to 5 minutes.
Pain begins slowly, and progressively gets worse, before going away crescendo - decrescendo)
Medications and rest can relieve pain.
It indicates increased risk of heart attack, but does not indicate an imminent heart attack.
Unstable Angina
A type of acute pain caused by cardiac hypoxia which is a warning sign of a heart attack.
It first appears as a severe episode (crescendo pattern), and can occur at any time, even at rest.
Episodes can last over 10 minutes.
It should be considered and managed as a form of acute coronary syndrome.
What are the clinical manifestations of angina?
- Intense pain released by rest or vasodilators.
- Paleness
- Profuse perspiraDon (sweaDng)
- Dyspnoea (shortness of breath)
- Normal cardiac enzymes
- Electrocardiogram will someDmes show ischemic changes.
What is myocardial infarction?
The cell death of cardiac muscle due resulting from prolonged, unrelieved ischemia (insufficient blood flow) to the myocardium, causing irreversible cell damage, and cell death.
It is usually caused by a blood clot in a coronary artery, which prevents blood flow to the myocardium. The greater the infarcted area, the greater the loss of contraction, leading to a worse prognosis.
What are the 3 coronary arteries and how do they relate to myocardial infarction.
- Myocardial infarcDons occur when the coronary arteries become blocked.
- The coronary arteries supply the myocardium with blood, and include:
-Left circumflex artery: provides lateral supply. Make up 20% of MI cases. Poor prognosis.
-Left anterior descending artery: provides anterior supply. Make up 50% of MI cases.
-Right coronary artery: provides posterior supply. Make up 30% of MI cases.
What are the clinical manifestations of myocardial infarction?
cyanosis
sweating
dyponea
nausea and vomiting
chest pain lasting 30 to 60 minutes which is not relieved by rest or nitrates. It can radiate into the jaw and shoulder.
Increased cardiac enzymes
ECG abnormalities
What are the two types of MI and their impacts on an ECG?
NSTEMI (30%)
partial thickness damage to the myocardium caused by a complete occlusion of a minor, or partial occlusion of a major coronary artery.
there is no ST segment elevation, but ST depression or T wave inversion can be present.
STEMI (70%)
full thickness damage to the myocardium caused by a complete occlusion of a major coronary artery.
There is ST segment elevation in an ECG.
It is a medical emergency.
What are the possible complications of a myocardial infarction?
- Dysrhythmias due to electrolyte imbalance and conduction defects in the myocardium.
- Cardiogenic Shock: inadequate blood flow to tissues due to cardiac disfunction.
- Oliguria: acute kidney failure due to low blood pressure preventing filtration.
- Pericarditis: cells die, causing necrosis and inflammation which can spread to pericardium.
- Cerebrovascular accident: stroke due to lack of blood flow to the brain
- Rupture of wall of infarcted ventricle: blood build up causes ventricle to burst.
- Systemic thrombo-embolism: the blood clot travels to other body parts.
What is the prognosis of myocardial infarction?
In acute myocardial infarction:
-33% mortality rate.
-50% of deaths occur prior to a hospital arrival.
-5 – 10 % of survivors die within a year after an MI.
-50% of patients are hospitalised within a year.
What is heart failure?
- Occurs when the heart fails to pump sufficient blood to the tissues.
- This causes fluid to accumulate in the tissues, causing congestive heart failure.
What is left sided heart failure, its causes and manifestations?
- The output of the left ventricle is lower than the blood received from the pulmonary circulation.
- This causes a falling in systemic blood pressure, and congestion of the pulmonary circuit.
Causes
Volume overload from valve abnormalities, systemic hypertension increasing pressure overload, restrictive filling or loss of muscle mass or functioning.
Clinical Manifestations
Decreased oxygenation and delivery of oxygenated blood leads to: dyspnea, increased respiratory rate, cough, cyanosis, fatigue.
What is right sided heart failure, its causes and manifestations?
- The output of the right ventricle is lower than the blood received from the vena cava.
- This causes congestion of the systemic circulation, and failure of the pulmonary circulation.
Causes
The major cause is left sided heart failure, but COPD or a pulmonary embolus can also cause.
Clinical Manifestations
ack of oxygenated blood flow to body tissues, but congestion of systemic circulation causes: oedema, fatigue, liver engorgement, cyanosis.
How can left sided heart failure lead to right sided heart failure?
left sided heart failure can lead to right sided heart failure by placing pressure on the right heart, as it must work harder to pump blood into the pulmonary circulation.
What is rheumatic fever?
An autoimmune response to an untreated infection of group A streptococcus bacterium. Repeated attacks of RF cause permeant damage to the heart, particularly the mitral (left) and aortic valves. This is because the antibodies produced mistakenly target these valves due to similar structures, and can also target joints. It is common in children in developing countries, and can lead to rheumatic heart disease.
What are the clinical manifestations and diagnostic tests of rheumatic fever?
Clinical Manifestations
- Murmurs
- Heart palpitations
- Breathlessness or exertion
- Oedema
- Stroke
Diagnostic Tests
- Complete blood count: check for anaemia
- Echocardiogram / ultrasound: check for abnormal heart sounds
- Imaging tests (x-ray, CT or MRI): check for heart enlargement.
What is infective endocarditis and its risk factors?
- Infection of the endocardium of the heart, usually involving the valves and endocardial lining.
Risk Factors
- Rheumatic fever or rheumatic heart disease.
- Illicit IV drugs with a contaminated needle.
- Scarring caused by damage to the heart valves, allowing the growth of bacteria and/or germs.
- Arrificial heart valves.
What is atherosclerosis?
The build up of fats, cholesterol and other substances on the arterial wall, forming plaque.
What is a serum lipid test, and what can it be used to diagnosed.
A measure of fats in the blood, looking at:
Total cholesterol
triglycerides
LDL
HDL
It is used to diagnose atherosclerosis
How are cholesterol levels in the blood determined, and what are the two kinds of cholesterol and their impacts?
Cholesterol levels in the bloodstream are determined:
-75% genetically by the liver
-25% by the diet.
- High Density lipoproteins (HDLs) carry 22% of cholesterol, transporting it from the tissues to the liver for
catabolism (conversion to bile salts).
- Low Density lipoproteins (LDLs) carry 60% of cholesterol, transporting cholesterol to cells via the bloodstream for synthesis of the cell membrane and steroids.
- High levels of LDLs in the bloodstream can damage the blood vessel walls, particularly endothelial cells.
How does an arterial thrombosis form?
Endothelial cells are damaged by high levels of LDL cholesterol, hypertension, or smoking.
White blood cells and platelets accumulate at the site of the injury.
Lipid accumulates at the site, and smooth muscle cells migrate.
Lipids and cholesterol are contained within plaque which deposits on the arterial wall over Dme.
Calcium deposits on these plaque deposiDons, causing hardening.
A fibrous collagen cap forms over the plaque, causing the walls to harden and the lumen to narrow.
This can lead to:
-Hypertension due to lumen narrowing.
-Thrombosis occurring elsewhere in the body if the deposit breaks off.
What are the risk factors and clinical manifestations of atherosclerosis
Risk Factors
- Age
- Gender
- Family History
- Hyperlipemia
- Hypertension
- Diabetes
- Smoking
Clinical Manifestations
- Are dependent on the blood vessels involved, and the extent of vessel obstruction.
- General signs and symptoms can include:
-Ischemia
-Sudden obstructions
-Aneurysm formation- In larger vessels, like the aorta:
-Thrombosis formation
-Weakening of the vessel wall
- In medium vessels, like the coronary or cerebral arteries:
-Ischemia
-Infarction
What is an embolism and the two key types?
A blockage in a blood vessel caused by a substance, or embolus, which travels through the bloodstream and lodges in a blood vessel, preventing blood flow.
Types of Embolism
- Thrombo-embolus: a blood clot formed in one located detaches from the vessel wall and travels to a distant site.
- Pulmonary-thrombo-embolus: a blood clot formed elsewhere travels to the lungs, blocking blood flow.
What is deep vein thrombosis?
- Involves a clot forming anywhere in a deep vein, which is not on the skins surface.
- It can occur anywhere but is o3en seen in the leg.
- The main symptoms include pain and swelling.
- It is o3en detected using a doppler ultrasound.
- The most serious complicaDon is a pulmonary embolism, which can be life threatening.
What is an aneurysm and its causes?
- An abnormal localised dilation of a blood vessels.
- There is no way to predict when they will rupture.
- They are usually discovered by CT or MRI, but often require imaging like angiography before management decisions are made.
- Common locations include the brain or aorta.
Causes include weakening of the arterial wall, hypertension, atherosclerosis, or family history
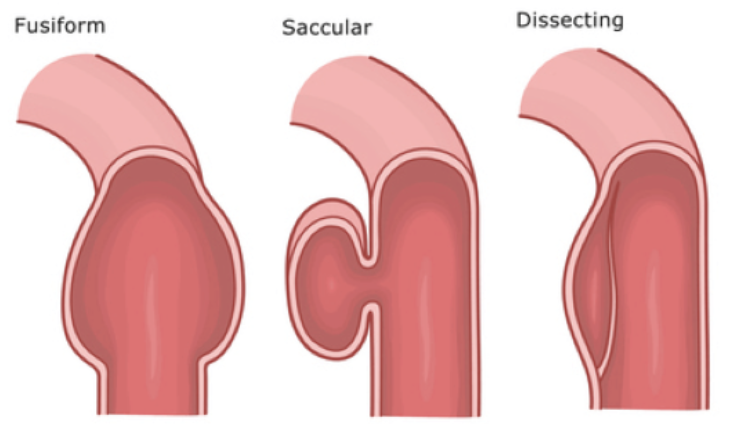
what are the 3 classifications of aneurysms
Fusiform
- Less common, and rarely rupture.
- Often caused by atherosclerosis
Dissecting
- Include injuries to innermost blood vessel layers.
- Cause is unknown.
- Age, atherosclerosis and hypertension contribute.
Sacculated
- The most common type.
- Often associated with growth and rupture.
- The most common cause is hypertension.
What are 3 common locations of aneurysms?
1. Cerebral Aneurysm
- Affect about 5% of the population.
- They are commonly saccular.
- Usually less than 1.5cm in diameter and found in the circle of willis.
- It generally has no symptoms before rupture, and symptoms after rupture include sudden, severe headaches, nausea, and vomiting.
2. Abdominal Aortic Aneurysm
- Asymptomatic, and generally found accidentally.
- Severe back and abdominal pain can indicate an imminent rupture.
- When ruptured, there is a 90% mortality rate, and results in the classical triad of pain, hypotension and apulsatile mass.
- It has 100% diagnostic accuracy with sonography.
- A focal aortic dilation of greater than 50% increase in diameter is accompanied by distension and a weakenedaortic wall.
3. Thoracic Aortic Aneurysm
- Located primarily in the thorax.
- They can be fatal if left untreated.
- Can be divided into ascending and descending.
What are the 2 kinds of thoracic aneurysm?
Ascending Thoracic Aneurysm
- Occur in the chest area above the diaphragm.
- Commonly diagnosed in older adults in their 60s.
- They do not always cause symptoms, especially when smaller.
- When they increase in size, they can cause back pain, tenderness in the thoracic region, shortness of breath anda cough.
Descending Thoracic Aneurysm
- Occurs in the posterior chest cavity, it refers to any aspect of the thoracic aorta distal to the origin of the left subclavian artery.
- Can be caused by atherosclerosis, hypertension or age.
- Symptoms can include pain in the abdomen, chest, or back.
- It can be diagnosed via a chest x-ray, CT or MRI scan, angiography or echocardiogram.
What is hypertension and the two different types of classifications?
Defined as blood pressure exceeding 140 mmHg systolic, and 90 mmHg diastolic pressures.
- Primary hypertension: makes up 90% of cases and has no specific cause.
- Secondary hypertension: makes up 10% of cases and has an underlying cause (i.e. renal or endocrine).
- It can also be classified as:
-Benign: the gradual elevaDon of blood pressure over many years.
-Malignant: accelerated elevaDon over a short period of Dme.
What are the risks and clinical manifestations of hypertension?
Risks
- Increased Salt Intake
- Obesity
- Stress
- Alcohol
Clinical Manifestatons
- Often asymptomatic, but can cause the following mild to moderate symptoms:
-Dizziness
-Unsteadiness
-Blurred vision
- Renal Failure
- Cerebrovascular Accident
What is the passage of air through the respiratory system?
The passage of air from the nose into the lungs includes the larynx, trachea, main bronchi, bronchioles, terminal bronchioles and alveoli. Capillaries surround the alveoli, allowing gas exchange between air and blood to occur across the pulmonary/respiratory membranes.
What are the two classifications of lung disorders and examples of each?
Obstructive lung disorders: The entry of air into the alveoli is obstructed in some way.
Destruction of capillaries and elastic fibres in emphysema.
Bronchoconstriction, oedema or hypersecretion of mucus in asthma.
Hypersecretion of mucus in chronic bronchitis.
Restrictive lung disorders: The expansion capacities of the lung tissue are restricted, reducing lung volume and capacity.
Lung fibrosis causing stiff lungs as lung tissue is replaced by fibrous tissue.
Pitwick syndrome where excessive subcutaneous fat restricts lung expansion ability.
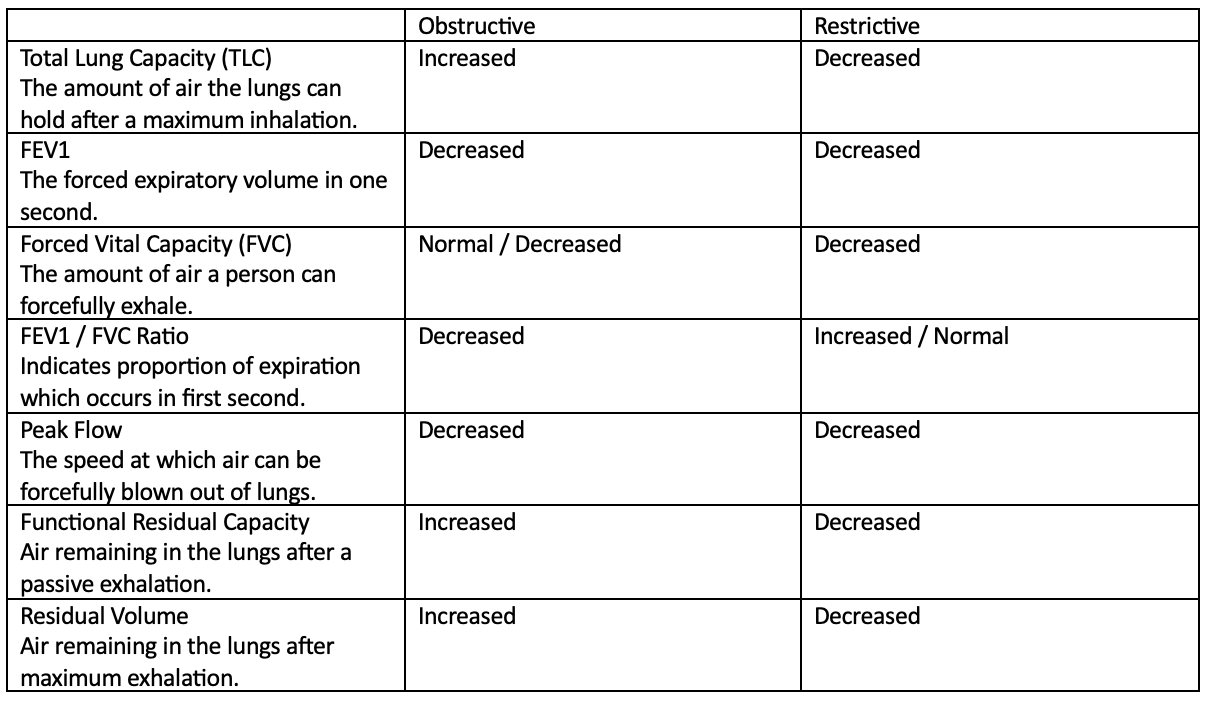
What do lung function tests show in obstructive vs restrictive disorders?
What is chronic obstructive pulmonary disease?
- An umbrella term which includes both emphysema and chronic bronchitis.
- Patients can have both disorders, or a mix of both.
- They are non-curable, but treatment can slow the development of the disease.
- Most patients with COPD have a mixture of bronchial inflammation and alveolar destruction.
What is emphysema?
- A type of chronic, obstructive pulmonary disease characterised by destruction elastic fibres, leading to destruction of alveolar sacks and the pulmonary capillary bed.
- Larger, less elastic sacks remain, preventing gas diffusion and causing air to become trapped inside alveoli.
- This causes the lungs to become permanently inflated.
What are the causes and pathogenesis of emphysema?
Causes: Smoking, air pollution, alpha-1 antitrypsin deficiency
1. Smoking or air pollution attracts inflammatory cells, triggering the release of elastase.
2. Alpha-1 antitrypsin is released to inhibits the actions of elastase.
3. Repeated exposure leads to an alpha-1 antitrypsin deficiency, meaning damage occurs to elastic fibres.
4. This causes emphysema.
What are the two types of emphysema?
Centre-acinar: The proximal portion of the acini, the bronchioles, are affected, while distal alveoli are spared. This typically occurs in smokers.
Pan-acinar: The acini are uniformly enlarged, but the distal alveoli become enlarged first. This typically occurs in an alpha-1 antitrypsin deficiency.
What are the clinical manifestations of emphysema?
- Decreased FEV1, increased TLC and residual volume.
- Reduced gas exchange.
- Dyspnoea
- Wheezing and cough
- Barrel chest.
- Hunched forward breathing.
- Pursed lip breathing
- Weight Loss
What diagnostic tests are used for emphysema?
- Lung function tests
- Chest X-ray
- CT
- Pulse oximetry
What is chronic bronchitis?
- The hypersecretion of mucus, and a chronic productive cough for at least 3 months of the year, 2 years in a row.
- It is obstruction caused by excessive mucus production which is not effectively cleared.
- The initial disease is in the larger bronchi, but later stages can cause disease in the smaller airways.
What are the causes and clinical manifestations of chronic bronchitis?
Causes: Smoking and air pollution
Clinical Manifestations
- Cough
- Wheeze
- Cyanosis
- Increased TLC and residual volume
What is used for the diagnosis of chronic
Diagnosis
- Lung function tests
- Arterial blood gasses
- Pulse oximetry
- Chest x-ray
- CT scan
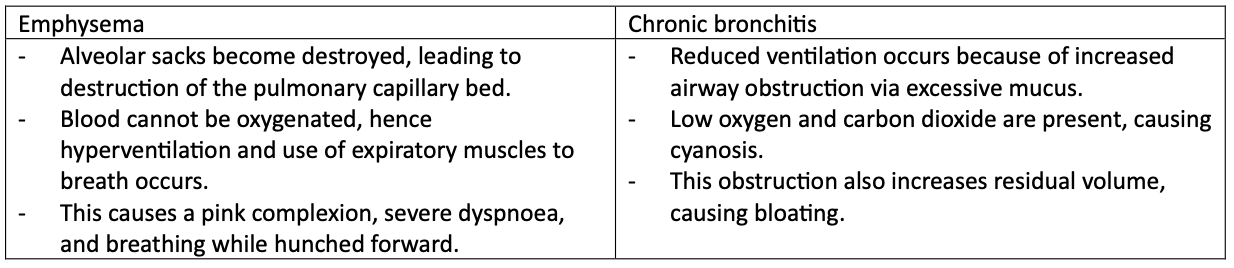
What are the differences between emphysema and chronic bronchitis?
What is asthma?
- A chronic disease of the airways.
- It involves airway inflammation, intermittent airflow obstruction, and bronchiole hyperresponsiveness.
- Small bronchi and bronchioles undergo episodic airway obstruction and air trapping due to exaggerated
bronchoconstriction, and excessive mucus production.
What are the etiological factors contributing to asthma?
- Environmental factors
- Respiratory tract infections
- Food
- Exercise
- Tobacco or occupational exposure.
What are the two types of asthma
Extrinsic or Atopic
- Occurs due to IgE immune response to environmental antigens (type I hypersensitivity)
Intrinsic or non-atopic
- Triggered by non-immune stimuli such as aspirin, psychological stress, or exercise.
What do the bronchi look like normally vs in asthma?
In a normal bronchial:
- The lumen is wide
-Contains normal numbers of smooth muscle cells, and mucus glands present.
In asthma:
-The lumen is narrow
-Contains large amounts of smooth muscle cells and mucus glands.
-Inflammatory cells are present.
What are the clinical manifestations of asthma?
- Wheezing during attacks
- Chest tightness
- Dyspnoea
- Prolonged expiration
- Tachypnoea
- Tachycardia
- Respiratory acidosis
What is a pulmonary embolism?
- A sudden blockage of a lung artery by a circulating thrombotic agent, including fat, air or amnionic fluid.
- A pulmonary thrombo-embolism is very common and is when the thrombotic agent is a blood clot.
- 95% originate from deep vein thrombosis in the legs or hips.
What are the risk factors for a pulmonary embolism
- Old age
- Pneumonia
- Surgery
- Fractures
- Immobility
- Sickle cell disease
- Diseases of the coagulation cascade.
- Chronic obstructive pulmonary disease
What are the signs and symptoms of a pulmonary embolism?
- Coughing blood
- Chest pain
- Heart palpitaDons
- FainDng
- Shortness of breath
- Shock and low blood pressure.
- Instant death can occur
what is used for the diagnosis and treatment of a pulmonary embolism
Diagnosis
- CT pulmonary angiography is the preferred method as it provides accurate and non-invasive images.
- Pulmonary angiography can also be used, but is invasive.
Treatment
- Anticoagulants
- Surgery
What is pneumonia?
- Inflammation of the lungs, which can be acute or chronic.
- It is usually caused by microorganisms like bacteria.
- Most are community acquired, but they can also be nosocomial.
- It is a common infection in immunocompromised people.
what pathogens commonly cause pneumonia?
- Common pathogens include:
-Streptococcus pneumoniae
-Hemophilus influenzae
-Staphylococcus aureus
- Microbe entry can occur via inhalaDon, or a blood borne infecDon from elsewhere in the body.
What are the two types of pneumonia
Bronchopneumonia
-Alveolar inflammation is widespread and patchy, leaving some alveoli unaffected.
-Occurs in older or younger people of both genders.
-Occurs via secondary infection.
-Not limited by anatomical bounds.
-Usually, bilateral.
Lobar pneumonia
-All alveoli in a lobe are involves by intense acute inflammation
-Occurs in Middle Ages, more commonly in male.
-Occurs via primary infection.
-Limited by anatomical bounds.
-Usually, unilateral.
What are the 4 stages of lobular pneumonia?
Congestion (24 hours): vasodilation occurs, and blood vessels become congested.
Red Hepatisation (2-3 Days): vascular permeability is increased, causing alveoli to become filled with red blood cells, white blood cells and fibrin. This causes the lungs to become read, firm, airless and liver-like.
Grey Hepatisation (4-6 Days): more white blood cells, including neutrophils and macrophages, enter the alveoli. The lungs appear grey and firm.
Resolution (less than 6 Days): macrophages undergo phagocytosis and exudate is digested enzymatically. The lung returns to normal, spongy consistency.
What are the clinical manifestations of pneumonia
- Cough
- Dyspnoea and tachypnoea
- Fever
- Sharp pain with breathing if the pleura is inflamed.
- Sputum (bacterial)
- Hypoxemia, causing hypoxia.
- Bacterial pneumonias have more severe symptoms than viral pneumonias.
What tests are used for the diagnosis of pneumonia?
- Blood tests
- Chest X-rays
- Pulse oximetry
- Sputum test
- CT Scan
What is lung cancer?
- The lungs are a common site for secondary cancer via metastasis.
- The most common primary cancer in the lungs is bronchogenic carcinoma.
- This is the leading cause of cancer death.
- Risk increases with age, with 80% of cases being diagnosed over age 60.
- Early symptoms are non-specific, and a late diagnosis leads to a poor prognosis.
What is the ethology / risk factors for lung cancer?
- Genetic mutations increase risk of cancer developing.
- Smoking.
- 80-90% of cancers occur in current or former smokers.
- Asbestos or other inhaled industry exposures can also increase risk.
What are the two types of bronchogenic carcinoma?
1. Small Cell Carcinoma
- Arises within the bronchiole epithelium, in small cells with a large nucleus.
- It has a strong association to cigarette smoking.
- It is highly invasive with an early metastasis.
- Surgery is not possible, but radiotherapy can cause remission.
- It has a very poor prognosis.
2. Non-Small Cell Carcinoma
Squamous Cell Carcinoma
- Bronchiole ciliated columnar epithelium undergoes squamous metaplasia, causing dysplacia, causing carcinoma
in situ.- It is highly invasive, but it has a slow growth rate, and lower incidence of metastasis.
- It has a strong connection to smoking, and is more common in males.
Adenocarcinoma
- Cells are of glandular origin, and are well differentiated.
- They arise in the small bronchi of the peripheral lung.
- They have a slow growth, but early metastasis.
- They have the best prognosis of the lung cancer.
- It is associated with formation of scars in the lungs, and often requires surgical resection.
What are the clinical manifestations of lung cancer?
- Smokers cough and sputum production.
- Hoarseness.
- Haemoptysis
- Airway wheezing
- Dysponea
- Chest pain
- Weight loss
- Pneumonia
What diagnostic studies are done for lung cancer
- X-ray
- CT
- Sputum cytology
- Staging tests can be done a3er diagnosis, i.e. MRI, PET and Bone scans.
What is Atelectasis
The collapse of a lung or part of a lung due to fluid in the alveoli.
What is a Pneumothorax?
a collapsed lung due to disruption of interpleural pressure.
What is Cor Pulmonale
abnormal enlargement of the right heart due to a disease of the lungs or pulmonary blood vessels.
What is Bronchiectasis
damage to the airways causing airway widening, flubbing and scarring, as well as inhibiting mucus clearance, increasing risk of lung infection. It usually results from an infection.
What are the key tests used for lung disorders?
- Lung function tests using spirometry.
- Arterial blood gas analysis
- Blood tests
- Chest X-ray
- CT scan
What is a fistula?
An abnormal connection or passageway connecting two organs or vessels which do not normally connect. Most lie around the anus, and common ones include between the vagina and anus, or between skin and an intestine.
What is an abscess?
a tender mass generally surrounded by a coloured area, which can range from pink to deep red, from inflammation in response cell death. They can be palpated, and are usually caused by an infection, making them full of pus, bacteria and debris.
Both are an abnormal pocket of fluid which forms in different areas of the body, including on the skin, or internal viscera or organs.
Cysts have a closed structure, and contain an epithelial cell lining separating it from nearby tissues.
Pseudocysts aren’t closed, and don’t contain a separating epithelial lining.
What is a polyp
A projecting growth of tissue from a surface in the body, usually from a mucus membrane. Common locations include the colon, rectum, or cervix.
What organs make up the upper GI tract, and lower GI tract?
Upper GI: Oesophagus, stomach and duodenum
Lower GI: Jejunum, ileum, colon and rectum/anus
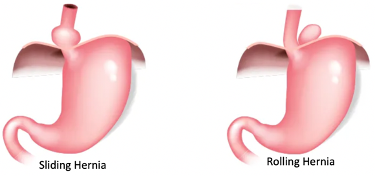
What is a hiatal hernia and the two types?
- The protrusion of an organ, typically the stomach, through the oesophageal opening in the diaphragm.
- Common symptoms include heartburn, epigastric or chest pain, and difficulty swallowing.
- It is a common cause of gastro oesophageal reflux disease.
Type 1 (Sliding): the stomach and lower oesophagus slide up and into the chest through the diaphragm.
Type 11 (Rolling): part of the stomach protrudes through the diaphragm next to the oesophagus.
What is gastro-oesophageal reflux disease and its causes and consequences?
It is the travelling of the stomach contents and acids into the oesophagus. This causes reflux oesophagus, inflammation of the oesophagus due to exposure to stomach acids.
Causes include: Hiatal hernia, increased abdominal pressure, abnormal functioning of lower oesophageal sphincter.
It can lead to Barrett oesophagus, where normal squamous epithelium is damaged, and metaplasia into gastric epithelium occurs. From here ulcers can arise, and the further dysplasia of cells can cause cancer to develop. Complications can include ulcers, bleeding, perforation, and scarring, and cancer metastasises early.
What is peptic ulcer disease
- A break or ulceration in the protective mucosal lining.
- This could occur in the oesophagus, stomach, or duodenum.
- Duodenal ulcers are 2-3 times more common than gastric ulcers.
- Regions distally to the duodenum are not affected.
What are the causes, symptoms, and complications of peptic ulcer disease
Causes:
Helicobacter pylori increases urease, which splits urea into ammonia and CO2. Ammonia causes damage to the mucosal lining of the stomach. H. Pylori generally colonises areas of the lower stomach as there is lower concentrations of hydrochloric acid.
NSAIDs like aspirin thin the mucus membrane, increasing risk of ulcer formation.
Stress, alcohol, smoking and spicy foods increase stomach acids, damaging the mucosal layer.
Symptoms: epigastric pain, nausea and vomiting, dyspepsia (difficulty swallowing), haematemesis.
Complications: perforation, bleeding and scarring.
What are the three key diagnostic tests for peptic ulcers?
Urea breath test: a capsule containing urea, made from an isotope of carbon, is swallowed. If h. pylori is present, the urea is broken down, and carbon dioxide is produced and absorbed across the stomach lining, into the blood. Carbon dioxide released via breath is then analysed, and the isotopic carbon in the exhaled breath is measured.
Endoscopy: Used to detect ulcers or take a biopsy to check for H. pylori presence.
Barium Meals: Used to visualise the oesophagus, stomach and duodenum on an X-ray. It cannot be used in perforated areas where the ulcer has passed through all 4 layers.
What is a small intestine obstruction, and the main causes.
Intestinal obstruction is caused by any condition preventing the normal flow of chyme through the intestinal lumen.
Causes:
Hernia: portions of the intestinal wall can move through abdominal muscles, preventing flow.
Intussusception: the intestine invaginates on itself, causing congestion.
Torsion: bowel twisting which prevents flow of chyme.
Tumour: adenocarcinoma of the colon is a common obstruction.
Paralytic Ileus: a loss of motor activity in the intestine prevents cyme flow.
Adhesions: two parts of the SI sticking together can cause obstruction.
What are the manifestations of a small intestinal obstruction?
It is dependant on the location and length of the obstruction, but generally includes
Distension (visible swelling of abdomen)
Copious vomiting
Severe dehydration -> hypovolemic shock.
Metabolic alkalosis
Colicky intermittent pain
Severe pain if obstruction causes ischemia, necrosis or perforation occurs
What are the diagnostic tests used for a small intestinal obstruction?
- Physical Exam: demonstrates swollen / tender abdomen.
- Abdominal X-ray: can show some intenstinal obstructions.
- CT scan: provides a detailed overview of intestinal obstruction.
- Ultrasound: preferred viewing method.
- Air or Barium Enema: enhanced imaging done for certain suspected causes.
What is inflammatory bowel disease and in who is it common?
- An idiopathic, autoimmune, chronic inflammatory disorder which occurs in the GI tract.
- It affects people of any age, and usually begins in teens or young adults.
- It is most common for white people of European ancestry, and both sexes are effected equally.
What are the two key types of inflammatory bowel disease
Crohn’s Disease:
- Begins in and affects the small intestine, and can extend below.
- The walls become hypertrophied and containing fissures andiIntestinal walls become thickened, and inflammation occurs through the full thickness of the wall.
- The lumen is narrowed and linear and deep ulcers occur within the wall.
- Areas of normal bowel lie within areas of affected bowel.
- Slight increase in colon cancer risk.
- Crampy abdominal pain is common.
Ulcerative Colitis
- Confined to the colon, and usually begins in the rectum.
- There is continuous involvement, and no normal areas of the bowel are skipped.
- Intestinal walls remain thin, and the mucosal layer becomes inflamed.
- Superficial ulcers form, and pseudo-polyps form from cycles of inflammation and regeneration of ulcerated epithelium.
- Increased risk of colon cancer.
- Bloody diarrhea is common.
What are the symptoms of inflammatory bowel disease, and the diagnostic tests used?
Symptoms
- Often have exacerbations and remissions.
- Intermittent diarrhea
- Colicky pain
- Malabsorption and weight loss
- Malaise and fever
- Intestinal obstruction.
Diagnosis
Blood tests, faecal occult blood tests, endoscopy, colonoscopy, X-ray, CT, MRI
What is colorectal cancer and its outcome.
- Cancer in the colon or rectum.
- It has a low survival rate, as it is often present for a long time before producing symptoms.
What are the risk factors and common distributions of colorectal cancer?
Risk Factors
- Diet high in fat and low in fibre.
- Ulcerative colitis
- Adenomatous polyps.
- Family history of colon cancer.
Distribution
- 50% occur in rectum.
- 20% in sigmoid colon
- 16% in caecum and ascending colon
- 8% in transverse colon
- 6% in descending colon
What are the two key classifications of colorectal cancer?
Right Sided Colon Cancer
- Occurs in the ascending colon.
- This side is wider, so tumours tend to grow larger, so go longer without producing symptoms, meaning it has a lower survival rate.
- They embed themselves within the wall, and do not block the flow of faeces.
- Older people and females are commonly affected.
- Weakness, malaise and weight loss occur.
Left Sided Colon Cancer
- Occurs in the descending colon and rectum.
- Blocks the flow of faeces earlier due to the smaller lumen.
- It can undergo a direct biopsy for diagnosis.
- Blood in the stool, diarrhea and constipation can occur.
What are the symptoms of colorectal cancer?
- Blood in the faeces
- Change in bowel habits.
- ObstrucDon
- Pain is a late symptom.
Name the 5 key tests of hepatobilliary function?
Bilirubin levels
Liver Enzymes
Plasma proteins
Portal Pressure
Imaging Tests
How is Billirubin levels used to test hepatobilliary functioning?
Billiverdin is a waste product produced in the breakdown of red blood cells. It is found in the plasma as free bilirubin, which becomes plasma bound, and is converted to water soluble bilirubin in the liver, where it can then be excreted by the kidneys.
Increased bilirubin in the blood (Serum bilirubin) indicates impaired functioning of the liver.
What is jaundice and the three types?
Characterised by the accumulation of bilirubin in the blood. Bilirubin accumulates in elastic tissue, causing it to have a yellow tint, i.e. skin and eyes.
Type A (pre hepatic): increased levels of unconjugated bilirubin, usually caused by excess haemolysis (RBC breakdown)
Type B (hepatic): increased levels of conjugated or unconjugated bilirubin, meaning there is interference with liver abilities.
Type C (post-hepatic): Increased levels of conjugated bilirubin, usually by an obstruction of bile flow.
How is liver enzymes used to test hepatobilliary functioning?
Liver enzymes are released into the bloodstream when liver cells are damaged.Hence, high levels in the blood indicate damage to liver cells.
Alkaline phosphatase is release during biliary tract obstruction. High levels hence indicate an obstruction.
Gamma glutamyl transferase is often high in those who abuse alcohol, and is an index of liver abnormalities.
How is plasma proteins used to test hepatobilliary functioning?
Synthesised in the liver, hence low levels indicate impaired liver function. Include albumin, coagulative factors and prothrombin.
How is Portaln pressure used to test hepatobilliary functioning?
Portal pressure: a measure of blood pressure within the portal venous system. Rises or falls indicate disorders which impact the haemodynamics of the liver.
How is imaging tests used to test hepatobilliary functioning?
Imaging tests can indicate visible abnormalities to the liver and its functioning.
What is cirrhosis
- Characterised by liver necrosis, fibrosis, and conversion of normal architecture into abnormal nodules.
- It includes widespread scarring of the liver, which is progressive, irreversible, and incurable.
- Liver cells usually regenerate in response to damage, but continual damage can become permeant as cells cannot cope with the stress they are placed under.
what are the two key types of cirrhosis
Portal Cirrhosis
- The most common, making up 60% of cases.
- It is caused by alcohol or viral hepatitis.
Biliary Cirrhosis
- Not very common.
- Can be caused by obstruction from gallstones.