Respiration and Excretion
1/84
Earn XP
Description and Tags
Includes the 5 overarching questions
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
85 Terms
What is the function of the nasal cavity?
Filters (has hairs/cilia), warms, and moistens incoming air before it enters the lungs.
How does exercise affect oxygen delivery to muscles?
During exercise, muscle cells work harder and produce more Co2 and lactic acid (lowers pH in the muscle tissue).
inc. CO2 and lower pH in tissue reduces Hb’s affinity for O2; Hb lets go of O2 more easily, delivering more O2 to active muscles
Why is there a pause before normal breathing resumes after several rapid, deep breaths?
rapid deep breathing lowers blood CO₂ levels, reducing the stimulus to breathe, causing a temporary pause until CO₂ levels rise again.
Why does a small puncture in the chest cavity (pleural cavity), even if the lung itself is not punctured, cause lung collapse
The pleural membrane surrounds the lungs and lines the chest cavity,, creating negative presure; keeps lungs inflated by sticking the lungs to the chest wall
A puncture will let air into the pleural cavity, breaking the negative pressure, causing the lung to collapse even if the lung tissue is intact
What are the key functions of the distal convoluted tubule (DCT)?
Absorbs excess/unecessary molecules in the blood (antibiotics, H+)
Sodium and calcium balance (responds to hormones like aldosterone)
Blood may require molecules from urine (like H+ if the blood pH is high)
What would hapen if the collecting duct didn’t pass through the renal medulla before reaching the ureter?
The urine would be hypotonic to the blood plasma. Without the salty medulla, there’s no osmotic gradient to draw water out of the collecting duct, even if ADH is present. Results in dilute urine being excreted
What condition must the medulla surrounding the loop of Henle and collecting duct meet for the kidney to produce urine more concentrated than plasma?
The medulla must be hypertonic (have a high solute concentration). This allows water to move out of the filtrate by osmosis, esp. in the collecting duct when ADH is present, resulting in concentrated urine
What are some of our wastes
bile, ammonia (NH3, from amino acid breakdown), urea (from ammonia breakdown), creatinine (from muscle contraction), CO2, ions
What would happen if glucose wasn’t absorbed back into the blood at the kidneys?
Low cellular ATP production/metabolism reduced
What would happen if amino acids weren’t absorbed back into the blood at the kidneys?
The body would lack the components needed to produce structural parts/inhibits protein synthesis
Function of skin in excretion
Sweat glands excrete salt/urea/H2O/ions
Cools body
Function of liver in excretion
Breaks down hemoglobin from old RBCs; produces urochrome, filtered out by kidneys into urine
Produces urea
Function of intestines in excretion
Iron and calcium are excreted into the intestinal cavity, leaves body in feces
dialysis
medical process that removes waste, excess fluids, and toxins from the blood when the kidneys can’t do so.
Describe the structure of the kidney, and what parts of the nephrons are at each of the followign locations: renal cortex, medulla, renal pelvis
Renal Cortex: Outer layer of the kidney. contains the glomeruli and Bowman's capsules (involved in pressure filtration) and the proximal and distal convoluted tubule.
Renal medulla: Inner region, arranged in pyamid shaped structures; contains the loops of Henle and parts of the collecting ducts (involved w/ water reabsorption and salt balance)
Renal pelvis: Funnel-shaped cavity collectin gurine from the collecting ducts; drains into ureter, which sends urine to the bladder
What is the pleural membrane?
Double layered membrane surroudnding each lung that maintains negative pressure to help lungs stay expanded/stick to chest wall, allowing them to inflate as thoracic cavity expands during inhalation
What is the pharynx?
A muscular tube that connects the nasal cavity to the larynx and esophagus; also called the throat.
What is the larynx?
Connects the pharynx to the trachea; contains vocal cords for sound and has the epiglottis to prevent food from entering the airway.
What is the trachea?
A cartilage-supported tube (windpipe) that carries air to the bronchi; lined with cilia to push particles out.
What are the bronchi?
Two main branches from the trachea that direct air into each lung.
What are bronchioles?
Smaller branches of the bronchi; lack cartilage but have smooth muscle to control airflow.
What are the lobes of the lungs?
Right lung has 3 lobes; left has 2 lobes to make room for the heart.
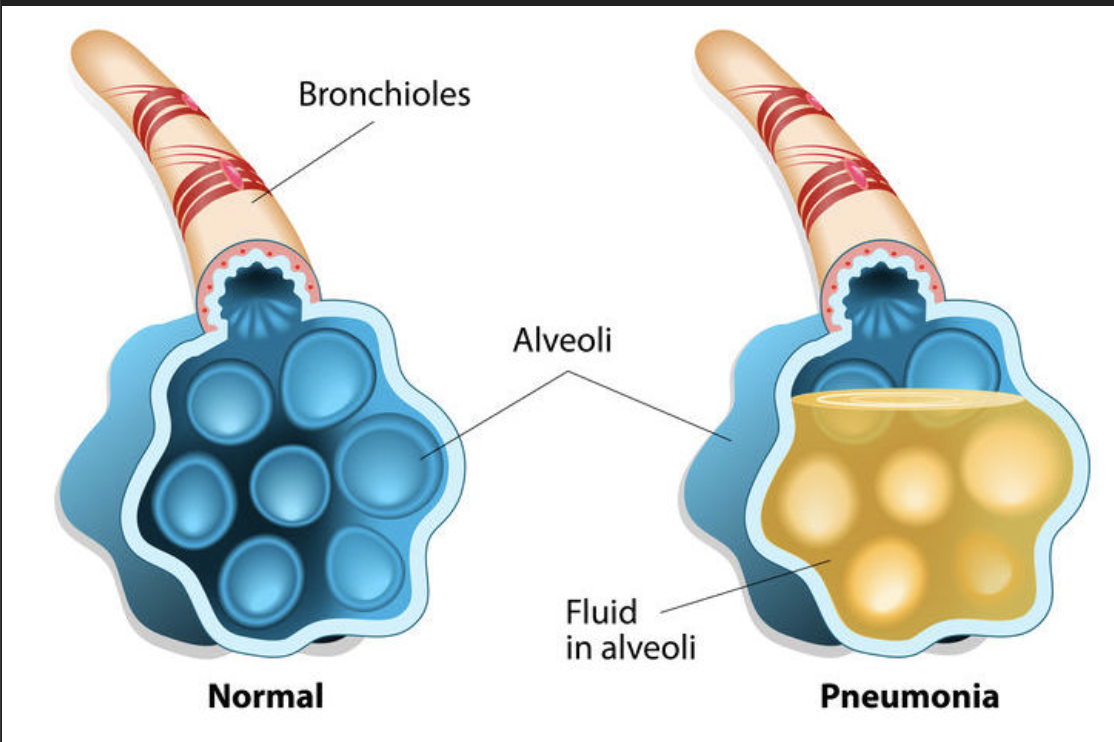
What are alveoli?
Tiny air sacs where gas exchange occurs; coated with a surfactant (lipoprotein) to prevent collapse.
What are capillaries (in the lungs)?
Tiny blood vessels around alveoli for gas exchange with blood.
What is the diaphragm?
A dome-shaped muscle that contracts to increase thoracic volume during inhalation and relaxes during exhalation.
What are intercostal muscles?
Muscles between the ribs that expand and contract the chest cavity.
What happens during inhalation?
Diaphragm contracts and flattens; intercostal muscles lift ribs; thoracic volume increases, drawing in air.
What happens during exhalation?
Diaphragm relaxes; ribs move down and in; thoracic volume decreases, pushing air out.
What initiates inspiration?
The medulla oblongata sends signals (via the phrenic nerve) after chemoreceptors detect changes in O₂, CO₂, or H⁺ levels.
Why does air flow into the lungs during inhalation?
Because pressure in the lungs is lower than atmospheric pressure.
Why does air flow out of the lungs during exhalation?
Because pressure in the lungs becomes greater than atmospheric pressure.
What is the correct path of air from outside to alveoli?
Nose ↔ Pharynx ↔ Larynx ↔ Trachea ↔ Bronchi ↔ Bronchioles ↔ Alveoli
What happens at the alveoli during external respiration?
Oxygen diffuses into capillaries, and carbon dioxide diffuses into the alveoli to be exhaled.
Why are alveoli good for gas exchange?
They have a large surface area, are one cell thick, moist, and are surrounded by capillaries.
What type of blood enters the alveoli from the pulmonary artery?
Deoxygenated blood high in carbon dioxide.
What type of blood leaves the alveoli through the pulmonary vein?
Oxygenated blood low in carbon dioxide.
What happens to the diaphragm during inhalation?
It contracts and flattens, increasing thoracic cavity volume.
What happens to intercostal muscles during inhalation?
They contract, lifting the ribcage up and outward.
What happens to the diaphragm during exhalation?
It relaxes and returns to its dome shape, decreasing thoracic volume.
What happens to intercostal muscles during exhalation?
They relax, letting the ribs drop and compress the lungs.
Process of exhalation
Diaphragm relaxes and moves upward, ribs move downward and inward; thoracic cavity volume decreases, creating positive pressure that pushes air out.
Phrenic nerve
Nerve that controls the diaphragm’s contraction during inhalation; originates in the cervical spinal cord.
Vagus nerve
Cranial nerve that carries signals from stretch receptors in the lungs and chemoreceptors to the brainstem to regulate breathing rate.
Alveoli receptors
Stretch receptors in the alveolar walls that detect lung expansion and signal the brain via the vagus nerve to prevent over-inflation.
Carotid bodies
Chemoreceptors located at the carotid arteries; detect changes in blood CO₂, O₂, and pH to help regulate breathing.
Aortic bodies
Chemoreceptors in the aortic arch that monitor blood CO₂, O₂, and pH levels, sending signals to the brain to adjust respiratory rate.
Role of [CO₂] in breathing
High CO₂ increases acidity (lowers pH) of blood (because it can bind to H2O, form carbonic acid that dissociates into H+, HCO3-; central chemoreceptors detect this and stimulate increased breathing rate to remove CO₂.
Role of [H⁺] in breathing
[H⁺] is a key trigger for adjusting ventilation rate to maintain blood pH balance
[H⁺] increases → pH drops (acidosis) → breathing rate increases.
Role of stretched alveoli
Stretching activates receptors that send inhibitory signals via the vagus nerve to reduce inhalation effort and prevent overexpansion.
Process of inhalation
Diaphragm contracts and moves downward, ribs lift upward and outward, expanding thoracic cavity; this creates negative pressure inside lungs, drawing air in.
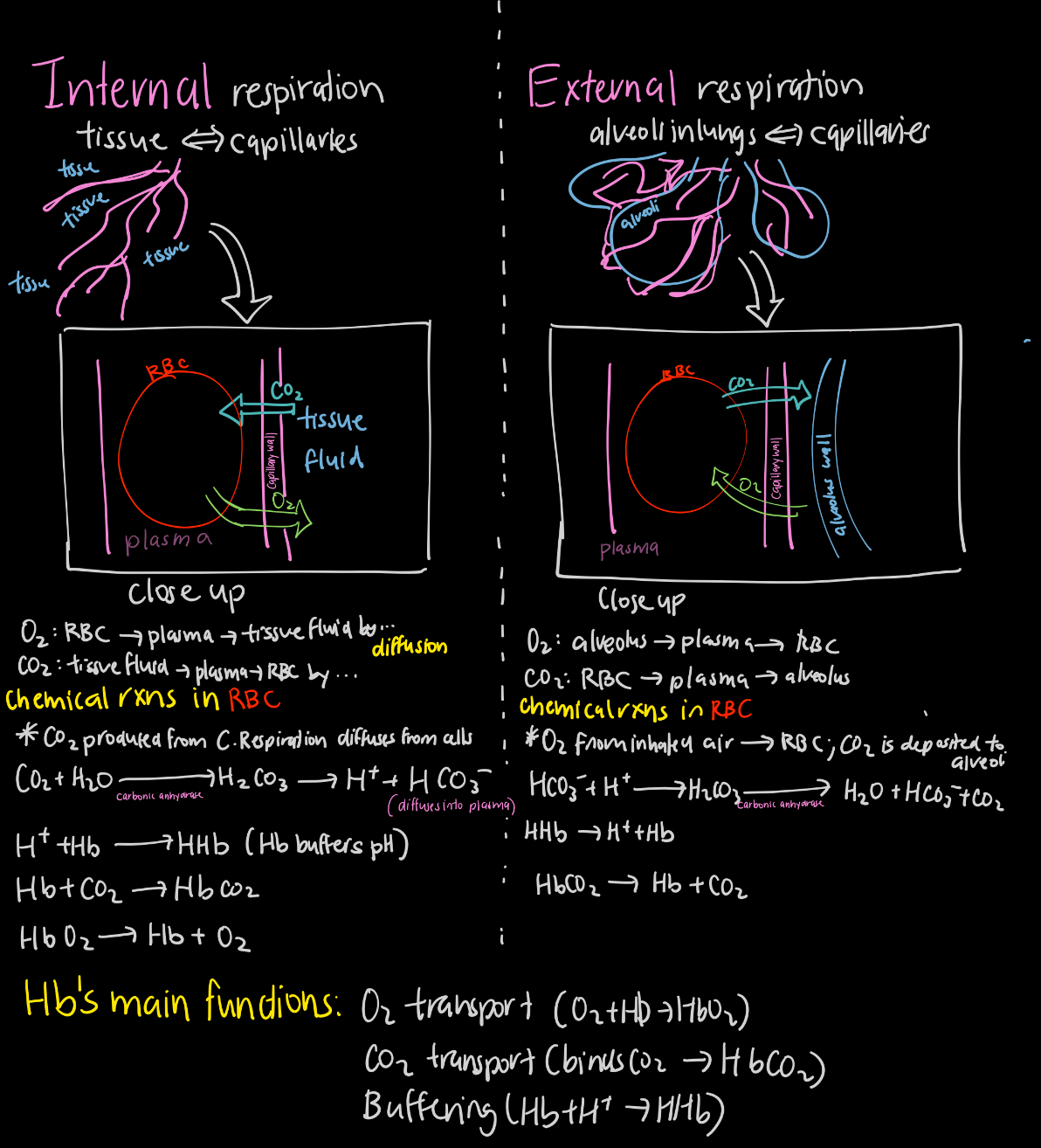
What is external respiration?
Gas exchange between the alveoli and the blood in the lungs.
What is internal respiration?
Gas exchange between blood and body tissues.
In external respiration, where does oxygen go?
From the alveoli into the capillaries (blood).
In external respiration, where does carbon dioxide go?
From the capillaries into the alveoli.
In internal respiration, where does oxygen go?
From capillaries into the body tissues.
In internal respiration, where does carbon dioxide go?
From body tissues into the capillaries.
What is asthma?
A chronic inflammatory condition where the bronchi and bronchioles constrict, swell, and produce excess mucus, making breathing difficult.
What is pneumonia?
An infection that inflames the alveoli, filling them with fluid or pus and impairing gas exchange.
What is lung cancer?
Uncontrolled growth of abnormal cells in the lungs, often starting in the bronchi, that blocks airways and damages tissue.
What is emphysema?
A condition where alveolar walls are damaged, reducing surface area for gas exchange and causing breathlessness.
What is bronchitis?
Inflammation of the bronchi causing narrowed airways, excess mucus, and persistent coughing.
What is the role of the pulmonary artery?
Carries deoxygenated blood from the right side of the heart to the lungs.
What is the role of the pulmonary vein?
Carries oxygenated blood from the lungs to the left side of the heart.
What carries oxygen to body tissues?
Red blood cells with hemoglobin transport oxygen from the lungs to tissues.
What carries carbon dioxide from tissues back to the lungs?
Blood plasma and red blood cells transport carbon dioxide to the lungs for exhalation.
When and how is deoxyhemoglobin (HHb) formed?
HHb is formed during internal respiration, when O2 is released from Hb and H+ bind to it
What is carbaminohemoglobin (HbCO₂) and what does it do?
Carbaminohemoglobin forms when carbon dioxide binds directly to hemoglobin (not at the oxygen site). It transports about 20–23% of CO₂ from tissues to the lungs.
What is bicarbonate (HCO₃⁻) and how is it created?
Bicarbonate is the main form of CO₂ transport in the blood (~70%). It is formed in red blood cells when CO₂ reacts with water to form carbonic acid, which then dissociates into H⁺ and HCO₃⁻.
What is carbonic acid (H₂CO₃) and what is its role in respiration?
Carbonic acid is an intermediate formed when CO₂ combines with H₂O in red blood cells. It quickly dissociates into H⁺ and HCO₃⁻, helping regulate blood pH and facilitate CO₂ transport.
What is the hydrogen ion (H⁺) and why is it important in respiration?
H⁺ is released when carbonic acid dissociates. It lowers blood pH, stimulating chemoreceptors to increase breathing rate, and is buffered by deoxyhemoglobin in RBCs.
How does bicarbonate (HCO₃⁻) re-enter red blood cells in the lungs?
In the lungs, bicarbonate re-enters RBCs and combines with H⁺ to form carbonic acid, which breaks down into CO₂ and water. The CO₂ is then exhaled.
Where is carbonic anhydrase found, and what does it do?
Carbonic anhydrase is found in red blood cells and catalyzes the rapid conversion of CO₂ and water into carbonic acid (and vice versa), enabling fast CO₂ transport and pH balance.
What is oxyhemoglobin (HbO₂) and what is its role?
Oxyhemoglobin is formed when oxygen binds to hemoglobin in red blood cells, mainly in the lungs. It allows efficient transport of oxygen from the lungs to the tissues.
What substance would be found at its highest concentration in blood leaving tissue capillaries?
Bicarbonate ions HCO3-
Why would alveoli not be characterized as muscular?
Specialized for gas exchange, not movement/contraction
They are thin-walled, vascularized, and secrete a surfactant (a lipoprotein) to reduce surface tension.
What is most of the carbon dioxide produced by tissues carried back to the lungs as?
Bicarbonate ions.
What would cause a decrease in the pH of the blood during internal respiration?
During internal respiration, Co2 produced by cells diffuses into RBCS
CO2 reacts with H2O to form carbonic acid (H2CO3), catalyzed by carbonic anhydrase.
Carbonic acid then dissociates into bicarbonate (HCO3-) and H+
This increase in H+ lowers pH of the blood.
When you exercise, your muscles undergo more cellular respiration → increased production of CO2
As blood becomes more acidic in muscle tissues, hemoglobin will carry less of what?
Oxygen, because lower pH and higher Co2 levels in active tissues (like muscles during exercise) cause Hb’s affinity for O2 to decrease.
Hb unloads more oxygen to tissues that need it most, making less oxygen carried in the blood
What reaction occurs in the capillary of the leg/or any actively respiring tissue and why?
Hb + H⁺ ↔ HHb.
CO2 from cellular respiration diffuses into the blood + RBCs, combines with H2O to form H₂CO₃ (carbonic acid), catalyzed by carbonic anhydrase. H2CO3 then quickly dissociatres into H+ and HCO3-. The free H+ lowers pH; Hb acts as a buffer by binding to the H+, maintaining blood pH in a safe range
Compare internal and external respiration by describing the movement of molecules between tissue fluid, blood plasma, and the alveoli. Include the role of hemoglobin as a transport molecule and buffer
(see diagram) In external respiration, O₂ diffuses from alveoli into plasma and RBCs to form HbO₂; CO₂ (as HCO₃⁻) is converted to CO₂ gas in RBCs and exhaled.
In internal respiration, HbO₂ releases O₂, which diffuses into tissues, and CO₂ from tissues diffuses into plasma and RBCs, forming H⁺ and HCO₃⁻; H⁺ is buffered by Hb (forming HHb), and some CO₂ binds to Hb as HbCO₂.
Hb carries/trasnports O2, CO2 and acts as a buffer
You are severely dehydrated. Describe the hormonal response to low blood volume and low Na⁺, and the effect on water absorption
Low blood volume and Na⁺ trigger aldosterone (from adrenal cortex) and ADH (from posterior pituitary). Aldosterone increases Na⁺ reabsorption and K⁺ secretion in the loop of henlet; water follows Na⁺ by osmosis. ADH increases water permeability in the collecting duct, allowing more water reabsorption. Both increase blood volume and restore fluid balance.
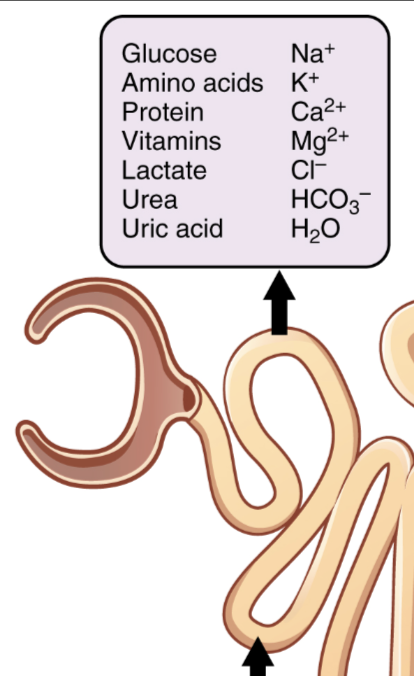
Outline pressure filtration. Include where it occurs, molecules involved, and WHY molecules move
Pressure filtration @ glomerulus, adense network of capillaries inside the Bowman’s capsule of the nephron. Blood enters glomerulus thru afferent arteriole, which is wider than the efferent arteriole - this difference in diameter creates high BP in the glomerulus - forces small molecules like H2O, gluvose, salts/ions, urea, amino acids out of the blood and into the Bowman’s capsule, forming filtrate. Large molecules like plasma proteins/RBCs don’t pass through bc they are too large to fit through the capillary walls.
Outline selective reabsorption. Include where it occurs, molecules involved, and WHY molecules move
Selective reabsorption occurs in the proximal convoluted tubule. Using active transport and ATP (lots of mitochondria lining the tubule), essential molecules like glucose, amino acids, ions, and salts are reabsorbed into the blood (surrounding peritubular capillaries) via carrier proteins and channel proteins.
Water follows by osmosis due to the increasing solute concentration in the surrounding tissue. This ensures useful substances are conserved and not lost in urine; helps establish osmotic gradient in the kidney, which is later important for water reabsorption in other parts of the nephron
Describe the process of inspiration. Outline the path air takes as it enters your body until the time it reaches your alveoli. Include how inspiration is affected by CO₂ and H⁺ concentrations, stimulation to various nerves, changes in pressure and volume
Inspiration is controlled by the medulla oblongata, which receives input from chemoreceptors in the carotid and aortic bodies when CO₂ or H⁺ rises (or O₂ drops). The medulla sends signals via the phrenic nerve to contract the diaphragm, increasing thoracic volume and decreasing pressure to draw air in. Air passes through nasal passages -> pharynx ->larynx ->trachea ->bronchi ->bronchioles ->alveoli. Stretch receptors in alveoli send signals via the vagus nerve to stop further inhalation, preventing overexpansion.
The exchange of oxygen and carbon dioxide in external respiration occurs by what process?
Diffusion.