SINUSITIS
1/18
Earn XP
Description and Tags
CC
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
19 Terms
Sinusitis
Sinusitis, also known as rhinosinusitis, is the inflammation of the mucous membranes that line the paranasal sinuses
What is sinusitis, and how is it classified based on duration?
Sinusitis is the inflammation of the mucous membranes lining the paranasal sinuses. It is classified into:
Acute: <4 weeks
Subacute: 4-12 weeks
Chronic: >12 weeks
Recurrent Acute: 4 or more episodes per year, each lasting <4 weeks with complete resolution between episodes.
Relevant Anatomy
Paranasal Sinuses: These are air-filled cavities located within the bones of the skull and face. They include:
Maxillary Sinuses: The largest sinuses, located in the cheekbones.
Frontal Sinuses: Located in the forehead above the eyes.
Ethmoid Sinuses: A group of small sinuses located between the eyes.
Sphenoid Sinuses: Located behind the ethmoid sinuses, near the center of the skull.
Ostia: Small openings that connect the sinuses to the nasal cavity, allowing mucus to drain.
Nasal Mucosa: The lining of the nasal cavity and sinuses, which contains ciliated epithelium that helps in mucus clearance.
Blood Supply: The sinuses are vascularized by branches of the internal and external carotid arteries. Venous drainage is primarily via the facial vein and the cavernous sinus.
Innervation: The sinuses receive sensory innervation from branches of the trigeminal nerve (cranial nerve V), which is why sinusitis can cause facial pain.
Pathophysiology
The pathophysiology involves:
Trigger (e.g., URI, allergens)
Mucosal inflammation
Ostial obstruction
Impaired mucus drainage
Mucus accumulation
Bacterial, viral, or fungal growth
Infection and inflammation
Sinusitis symptoms (pain, discharge, congestion)
Investigations
Clinical Evaluation:
History: Important to ascertain symptom duration, nature of discharge (purulent or not), facial pain, nasal obstruction, and associated symptoms like fever or cough.
Physical Examination: Nasal endoscopy may reveal mucosal swelling, purulent discharge, or polyps.
Imaging:
CT Scan: The gold standard for imaging, showing mucosal thickening, air-fluid levels, or complete sinus opacification. It helps in identifying complications and is essential in evaluating chronic sinusitis.
MRI: Used when there is a suspicion of fungal sinusitis or to evaluate potential intracranial complications.
Laboratory Tests:
Microbiological Cultures: Obtained from nasal or sinus aspirates, useful in chronic or refractory cases.
Allergy Testing: If allergic rhinitis is suspected as a contributing factor.
C-reactive Protein (CRP) and Erythrocyte Sedimentation Rate (ESR): May be elevated in cases of acute bacterial sinusitis.
Differential Diagnosis
Allergic Rhinitis: Characterized by sneezing, itching, and clear rhinorrhea, often seasonal.
Migraine Headache: May mimic sinusitis with facial pain but lacks purulent discharge or nasal congestion.
Dental Abscess: Maxillary sinusitis can be confused with dental infection, especially with upper molar involvement.
Neoplasms: Nasal or sinus tumors can present with similar symptoms but often include unilateral obstruction or epistaxis.
Viral upper respiratory Infection
Granulomatosis with polyangiitis (Wegener’s Granulomatosis)
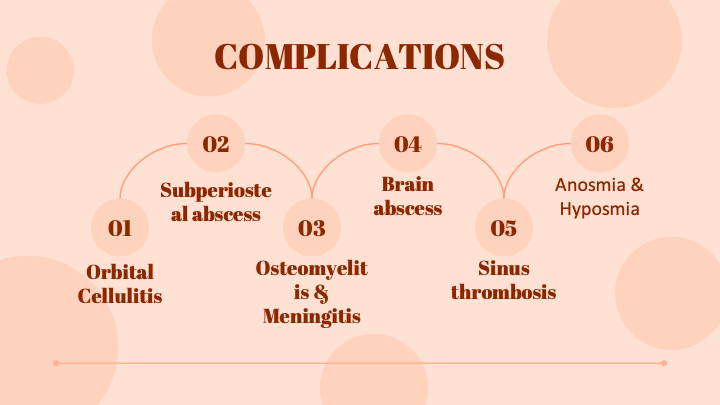
Complications
Orbital Complications: Including orbital cellulitis, subperiosteal abscess, and orbital abscess. These are more common with ethmoid sinusitis and can lead to vision loss.
Intracranial Complications: Meningitis, brain abscess, and cavernous sinus thrombosis can occur, particularly with frontal or sphenoid sinusitis. These are life-threatening and require prompt intervention.
Osteomyelitis: Particularly of the frontal bone (Pott's puffy tumor), which is a rare but serious complication.
Chronic Sinusitis: Can lead to persistent symptoms and a significant reduction in quality of life, requiring long-term medical or surgical management.
Treatment
Medical Management:
Antibiotics: Indicated in bacterial sinusitis, with first-line options including amoxicillin-clavulanate. Macrolides or doxycycline are alternatives in penicillin-allergic patients.
Nasal Corticosteroids: Effective in reducing inflammation, particularly in chronic sinusitis or if associated with allergic rhinitis.
Decongestants: Both oral and nasal, though the latter should be used short-term to avoid rebound congestion.
Saline Irrigation: Helps in mucus clearance and provides symptomatic relief.
Antihistamines: Useful if allergic rhinitis is present.
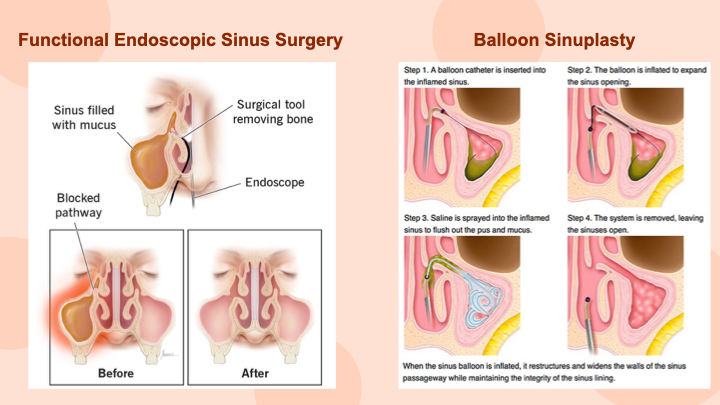
Surgical Management:
Functional Endoscopic Sinus Surgery (FESS): Indicated for patients with chronic sinusitis unresponsive to medical therapy, or for complications. The goal is to restore normal sinus drainage by removing obstruction and enhancing sinus ventilation.
Ballon surgery
Caldwell-Luc procedure
What are the main sinuses affected in sinusitis?
The main sinuses affected are the frontal, maxillary, ethmoid, and sphenoid sinuses.
How is acute sinusitis typically triggered?
Acute sinusitis is often triggered by a viral upper respiratory infection that leads to inflammation and obstruction of the sinus ostia.
What are common symptoms of sinusitis?
Common symptoms include nasal congestion, facial pain or pressure, purulent nasal discharge, and reduced sense of smell.
Which imaging modality is preferred for evaluating sinus anatomy in sinusitis?
A CT scan is preferred for detailed evaluation of sinus anatomy in sinusitis.
What treatment is commonly used to reduce inflammation in chronic sinusitis?
Intranasal corticosteroids are commonly used to reduce inflammation in chronic sinusitis.
What type of testing can be done to identify allergens contributing to sinusitis?
Allergy testing can be done to identify allergens contributing to chronic sinusitis.
Which condition involves a fungal infection that can spread from the sinuses to the brain?
Rhinocerebral mucormycosis is a fungal infection that can spread from the sinuses to the brain.
What is a common first-line antibiotic treatment for acute bacterial sinusitis?
Common first-line antibiotics include amoxicillin or amoxicillin-clavulanate.
What is the role of the microbiome in the pathogenesis of chronic sinusitis and how might this influence treatment strategies?
The nasal and sinus microbiome plays a role in maintaining mucosal health and preventing pathogenic overgrowth. In chronic sinusitis, an imbalance or dysbiosis in the microbiome can contribute to persistent inflammation and infection. This understanding influences treatment strategies by potentially including probiotics or microbiome-modifying therapies as adjuncts to traditional treatments, aiming to restore a healthy microbial balance and enhance overall sinus health.
Discuss the potential impact of environmental factors and lifestyle on the development and progression of chronic sinusitis.
Environmental factors such as air pollution, tobacco smoke, and exposure to allergens can exacerbate or contribute to the development of chronic sinusitis by irritating the mucosa and altering immune responses. Lifestyle factors, including poor hydration and inadequate nasal hygiene, can also impair mucosal function and drainage. Addressing these factors through lifestyle modifications, such as reducing exposure to irritants, improving indoor air quality, and ensuring adequate hydration, can be integral to managing and preventing chronic sinusitis.
Analyze the implications of sinusitis in the context of systemic diseases such as cystic fibrosis or autoimmune disorders.
In systemic diseases like cystic fibrosis, chronic sinusitis is a common complication due to thick, viscous mucus obstructing sinus drainage and promoting persistent infections. In autoimmune disorders, such as granulomatosis with polyangiitis, sinusitis can be a manifestation of systemic inflammation. The management of sinusitis in these contexts requires a multidisciplinary approach, including treating the underlying systemic condition with specific therapies, as well as targeted sinusitis treatments to address both the local and systemic components of the disease.