Carbohydrates
1/36
Earn XP
Description and Tags
still refer back to lecture
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
37 Terms
what is the acceptable macronutrient distribution ranges for cabohydrates
45-65% of total calories
how much recommended dietary allowance for carbohydrates
130 g/day for brain fundtion
whole vs refined carb
refined carbs retains energy and carbohydrates of a food but removes most of the other nutrients such as purified carbs flour, sugar, etc. whereas whole are things like whole fruit, grain and vegetables
simplest form of carb
monosaccharides
oligosaccharides vs polysaccharide
oli is 3-10 units of the monosaccharide chain whereas poly is over 10
chain of glucose breakdown to ATP
Glucose -> glycolysis -> Pyruvate -> acetyl Coa -> oxaloacetate -> Citric acid cycle/ Krebs cycle/ TCA cycle -> NADH, succinate ->Electron transport chain -> ATP
how is does the availability of carb control metabolism
if carb is available oxaloacetate is present as this is synthesized in the Krebs cycle where glucose is further broken down into ATP, and Acetyl-CoA form fatty acid oxidation has oxaloacetate to combine with in the TCA cycle. however if there is no carb available, oxaloacetate is minimal, and the liver would use the Acetyl-CoA instead to make ketone for the brain
what is GLUT 1
found in the blood, blood brain barrier, and to a lesser extent in the heart. this is insulin-independent where it is always on and does not get modulated by the presence or absence of insulin
what is GLUT 2
found in the liver, pancreas and small intestine. it is insulin independent, high Km (amount of substrate needed to have an attraction) and low affinity
what is GLUT 3
found in the brain, neurons and sperm. insulin-independent and low Km (low amount of substrate needed to have attractions due to high affinity) with high affinity
what is GLUT 4
found in the skeletal muscles, adipose tissue, and heart. insulin-dependent with moderate Km and affinity
regulation of high blood glucose
beta cell in pancreas sense high blood glucose → release insulin
insulin signals target cells such as skeletal muscle and liver to uptake glucose and store it as glycogen
as this is done → decrease blood glucose → sensed by beta cells → stop insulin release
regulation of low blood glucose
alpha cells in the pancreas sense low blood glucose → release glucagon
glucagon signals its target cells to breakdown glycogen and release glucose
increase i blood glucose levels will make alpha cells stop releasing glucagon
what is glycemic response
is the effect of a food on blood glucose, this can be impacted by carbohydrate content of food and composition (simple and complex), amount of protein, fat, fibre included in meal and activity level
what is a glycemic index
ranking systems that communicates the ability for a food to increase our blood sugar, with glucose typically given as a 100 for reference. eg, high glycemic index = bigger increase in our blood sugar
what is glycemic load
this combines a food’s GI with the amount of carbohydrates in a serving of food= estimates rate and magnitude of blood sugar increase, and the amount of carbohydrate in the food is multiplied by glycemic index
what is diabetes mellitus
is an endocrine disorder that impacts >460 million people, it is characterized by sustained high blood glucose levels
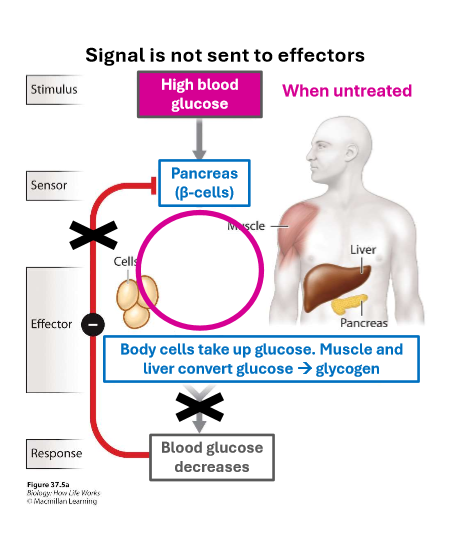
what happens in type 1 diabetes
this is caused by autoimmune destruction of beta cells in the pancreas, hence signal to uptake glucose is not sent to effectors
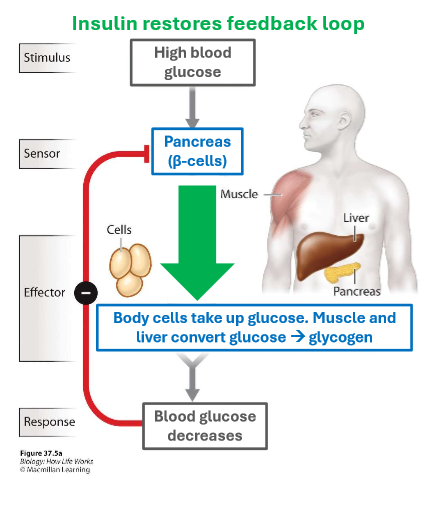
treatment of type 1 diabetes
exogenous insulin to replace the critical role of the beta cells in the body
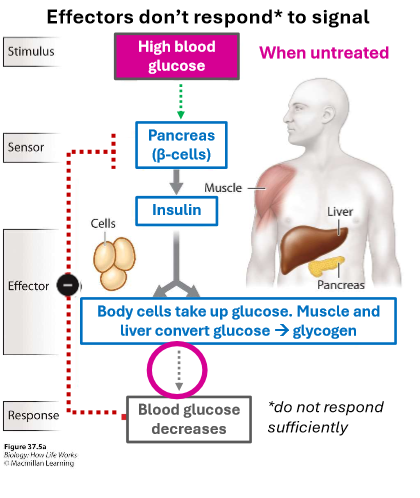
what is type 2 diabetes
caused by insulin resistance in target cells (insulin stimulation does not cause sufficient glucose uptake). the feedback loop exist but it is weak, hence effectors does not respond to signal
treatment of type 2 diabetes
include exogenous insulin, medications to increase insulin sensitivity or secretion or other effects, lifestyle changes including ozempic
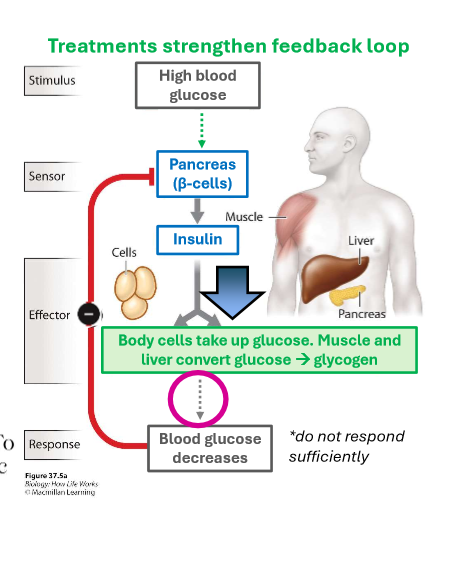
significance of ozempic
it is a more stable version of the hormone GLP-1 which enhances insulin secretion by activating an alternative pathway
population high risk for DM
First nations
what are long-term complications of diabetes
constant exposure to high levels of blood glucose causes biochemical changes such as
glycation of proteins (advanced glycation endproducts (AGE) formation, this damages vasculature, leading to more diseases)
conversion of glucose into other potentially toxic molecules (polyol pathway)
increased oxidative stress
changes in gene expression (insulin as growth factor)
what are the carb recommendations in Canada
WHO recommends that no more than 10% of calories come from free sugars (sugars added during processing)
Canada’s food guide recommends more unrefined carbohydrates- whole grains, fruits, vegetables and legumes
risk of too much sugar
increased risk of T2DM
increased risk of mortality, primarily through cardiovascular diseases
pros of decreased sugar intake
substantial decrease in the incidence of T2DM, cardiovascular disease and mortality
where to we get most of our carb
sugar and fibre
what is the difference in whole grains vs refined grains
refined grains only contain the endosperm which are starch and some protein
whole grains contain bran (fibre and vitamins), germ (vegetable oils an vitamin E) and endosperm (starch and some protein)
does fibre have an enzyme that breaks it down
no, fibre consist of polysaccharides that cannot be digested because we lack enzymes to break it down
soluble vs insoluble fibre
soluble fibre forms a gelatinous solution with water in the intestine and can be partly digested in large intestine by bacteria
insoluble fibre does not dissolve in water and are excreted whole
what are functional fibre
is added to processed food for nutritional benefit; soluble or insoluble
function of fibre
fibre helps to slow nutrient absorptionGI tracts contents are diluted by soluble fibre making it more difficult for enzymes to interact with the food resulting in slower digestion and lots of absorption of nutrients in the small intestine
fibre effect on cholesterol and bile salts
dietary fibre helps to lower total cholesterol by preventing their reabsorption in the intestine, and by forcing the liver to remove cholesterol from the blood (to synthesize bile salts)
fibre impact on health
greater quantities of fibre in the diet slow (increase) absorption time but overall speed up (decrease) transit time as fibre slows movement through small intestine and increases movement through large intestine. allowing stool weight to be higher and able to get rid of waster products quickly and effectively
pros of fibre intake
higher fibre diets have been correlated with lower rate of colon cancer, due to faster transit time decreasing contact with toxins
cons of lots of fibre intake
high fibre diet allow faster transit throughout the GI tract that excess pressure can cause the colon wall to bulge out, forming pouches called diverticula. and once fecal matter collects in these pouches, it may case pain, inflammation, infection = diverticulitis