Introduction to Occupational Therapy & Hospital Settings Practice Key Terminology
1/116
Earn XP
Description and Tags
Key terminology used across both Introduction to Occupational Therapy Practice and Occupational Therapy in Hospital Settings (flashcard 8 onwards) at UniSA
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
117 Terms
Occupation
There are many definitions but generally, its groups of activities and everyday tasks named, organised, that have meaning and value to individuals and/or to a culture or community.
Health
A state of complete physical, mental, and social wellbeing, as well as a positive concept emphasizing social and personal resources and physical capacities.
Wellbeing
How someone feels and how being in environments or situations that match their needs can impact one’s self-esteem and sense of belonging.
What are the four main categories of wellbeing?
Physical, mental, social, and spiritual.
What are the nine categories of occupation?
Work, leisure, activities of daily living (ADL), instrumental activities of daily living (IADL), rest and sleep, health management, play, education, and social participation.
What is the difference between ADL and IADL?
Although both are categories of occupation, ADL is basic and everyday tasks like eating and showering whereas IADL are more complex and specific tasks to an individual like caring for others or mode of transport.
What are eight categories of ADLs?
Bathing/showering
Toileting/toilet hygiene
Dressing
Eating/swallowing
Feeding
Functional mobility
Personal hygiene/grooming
Sexual activity
What is the difference between independence and self-determination?
Independence is not depending on the existence or actions of others, not subject to external control or support whereas self-determination is a part of independence which is being able to make choices about what is done, how, and when.
Why do OTs assess self-care (3 points)?
To measure change and monitor progress
To facilitate communication and decision making
To evaluate programs and conduct research
When assessing self-care/ADLs of a client, what five things should you consider?
Client needs, interests, and perceived difficulties
Clearly define the nature and meaning of the activity for the client
Understand the potential impact of persons’ condition on OP
Identify contextual factors (e.g. social, personal, cultural) which may affect assessment
Features of assessment tools
What is the difference between non-standardised and standardised assessment tools?
Non-standardised where therapists can decide on structure to cater to client needs, interests, and goals whereas standardised is standard procedure to follow which may require some training/experience depending on the tool.
When conducting a standardised assessment, what six things should you consider?
Cultural bias of an instrument
Requirements of a test like if there’s any specific environmental conditions and questions to be asked
Physical focus of the assessment like is it cognitive or behavioural perspectives
Time to conduct
How data should be collected (either observational or interviews)
If reassessing occurs, consider any time limitations and if its sensitive enough to one’s condition and prognosis
When conducting a non-standardised assessment, what does the therapist do?
Decide the structure of the assessment and the way it is conducted, where the client’s performance is not compared to normative data. This assessment could include an interview to gather info from the client or direct observation of the client carrying out the self-care task.
When preparing for a non-standardised or standardised assessment, what four things must be done?
Collect everything needed for the assessment and set up the environment
Schedule assessment with client/patient and relevant staff
Be sensitive to persons’ needs for modesty and privacy
Include relevant others like carers
During the assessment, what three things should be observed and analysed?
What are the possible causes for the OP deficits?
What else might you need to assess/think about?
Are there any differences in what you are observing compared to what the clients or others have reported? If so, why do you think this is the case?
What is the performance criteria used to assess self-care/ADL (4 points)?
Ability to get all supplies, set up tasks, perform, and terminate
Ability to complete in a reasonable time and energy consumption
Ability to perform safely
Ability to complete activities in all appropriate environments
Interventions
Strategies/techniques/environmental adaptations when we work with a client after an assessment is completed.
When selecting interventions, what are five things to consider?
Clients’ ability to learn
Clients’ prognosis
Time allocated for intervention
Discharge plan and their environment when discharged
Clients’ ability to follow through with new routines or techniques
What are seven common intervention techniques?
Adaption
Compensation
Remediation
Prevention
Health promotion
Education
Consultation
Compensation and what are three examples?
A type of intervention strategy which is changing the activity and the environment to match client which may be use of adaptive techniques, routines or equipment’s/devices; environmental modifications; and use of family members/personal care attendants to assist with or carry out the self-care activities.
Remediation
A type of intervention strategy which involves changing a person's capabilities by impacting upon body functions.
Prevention
A type of intervention strategy which involves identifying and reducing risk factors through anticipatory action.
Health promotion
A type of intervention strategy which enables person to identify resources.
Education
A type of intervention strategy which involves educating ways to manage occupation.
Consultation
A type of intervention strategy which involves providing expert advice and information.
What is client-centred practice and why it’s important to OTs?
Client-centred practice is all about building a therapeutic relationship with clients on the basis of respect and partnership. Client-centred practice is pretty much the basis for OTs because it involves equal participation from both parties to negotiate, communicate, discuss and having the client as a very active contributor to their own goals with the help of an OT to make a plan centred around their goals.
What are four key aspects of the client-centred practice philosophy?
Collaboration, providing choice, involved in decision making, and clients actively contribute to their own goals.
How can we relate to clients (6 points)?
Through advocating, collaboration, empathy, encouragement, instructing, and problem-solving.
What is the difference between practice and conceptual models?
Practice are uniform frameworks that guide our practice, acting as the basis to help predict or explain a set of phenomena or behaviour whereas conceptual are more abstract and theoretical which provide a framework for understanding our client and the many factors that affect our clients.
Paradigm (concept, theory, hypothesis)
Used to describe distinct concepts, a philosophical and theoretical framework (e.g. occupational performance).
Theory (concept, theory, hypothesis)
Used to describe the principles of an art or science rather than its practice.
Model (representation, prototype)
Used to represent something physical or abstract.
What are two key conceptual models used in healthcare and OT?
International Classification of Function (ISEF) and People Environment Occupation (PEO) Model.
What are two key practice models used in healthcare and OT?
American Association of OT (AOTA) and Occupational Performance Process Model (OPPM).
What are Frames of Reference and how they are used.
A theoretical blueprint or philosophy within which programme planning may occur, depending on the situation, resources, and the therapist’s education and experience. It can be used as a conceptual lens (theory) which is determined before the client is encountered or as a tool (process/intervention) where a range of approaches is adopted, as long it is specific and meets the needs of the client.
Approaches (Method)
The practical application of a model or frame of reference on how you carry out intervention with a particular client(s) in a particular setting.
What are the seven frame of references in OT (only for this specific course)?
Biomechanical
Rehabilitation
Cognitive-Behavioural
Developmental
Cognitive-Perceptual
Motor Learning (re-learning)
Sensory Intergration
What is the difference between occupational performance and occupational performance issue?
Occupational performance is the person or client performing the occupation whereas occupational performance issue is where the person or client is having difficulty or is incompetent to complete a specific occupation.
What are the seven steps in OPPM?
Name, validate, and prioritise occupational performance issue
Select potential intervention models
Identify body functions and environmental conditions
Identify strengths and resources
Negotiate targeted outcomes and develop action plans
Implement plans through occupation
Evaluate occupational performance outcomes
Clinical reasoning
There are multiple definitions of clinical reasoning however across all four definitions, clinical reasoning is a process used by therapists to determine an optimal and appropriate intervention(s) for a client from a holistic viewpoint based on one's experience and client's needs.
Why is clinical reasoning important in OT (5 points)?
Allows to develop flexible treatment plans that considers the patients values, interests, and meaningful occupations.
Helps us to balance evidence-based knowledge with client-centred practice.
Assists us to make decisions based on our treatment context (e.g. acute setting, public, private, and community).
Supports our ability to articulate justifications for treatment plans and recommendations.
Allows us to engage in dynamic learning processes with other therapists.
What are the main seven client resonings?
Scientific: Diagnostic
Scientific: Procedural
Narrative
Ethical
Conditional
Pragmatic
Interactive
Scientific: Diagonostic clinical reasoning
A type of clinical reasoning which applies logical and scientific methods in decision making, may be focused on the condition and known populations statistics (e.g. People with uncontrolled diabetes have a higher risk of complications with vision).
Scientific: Procedural clinical reasoning
A type of clinical reasoning focused on following protocols designed for the relevant condition or identified concern (e.g. Educating a client following total hip replacement on precautions they need to follow when it comes to getting dressed for example).
Narrative clinical reasoning
A type of clinical reasoning used by therapists to consider the individual as an occupational being and make decisions based on client interests, roles, and occupational profile, mainly through interviewing the client. This links to the grounding theories of the profession such as the importance of meaningful engagement and client-centeredness (e.g. Prioritising certain performance skills that will assist with a client returning to a valued role such as caring for others or leisure activities).
Ethical clinical reasoning
A type of clinical reasoning used by therapists to determine what ‘should’ be done within the practice context which can include balancing client's values and wishes (often motivated by therapists) and is often seen where there is a conflict with family members' desires and/or the organisational context/limitations (e.g. Discharging a client to their home, in line with their wishes and providing support to minimise ongoing risks that may be present).
Conditional clinical reasoning
A type of clinical reasoning used by typically long-term experienced therapists which is a flexible and reflective process where therapists are able to predict and imagine different potential outcomes based on how known factors like the client's condition, environment, and context will interact.
Pragmatic clinical reasoning
A type of clinical reasoning where the environmental context and constraints are considered, which can be physical (e.g. limited resources), organisational, or socio-political (e.g. Equipment that is available under funding schemes is not a best fit however still supportive of functioning; time limited interventions due to length of stay, and prioritising intervention focus based on this).
Interactive clinical reasoning
A type of clinical reasoning where decisions are made based off the interactions with clients in order to foster a therapeutic relationship based on improving the client's wellbeing and outcomes for the client, which may be demonstrated through active listening, empathy, or motivational interviewing techniques to support the therapy process (e.g. Discussing a patient's interests while providing hand therapy exercises, asking questions about family members to further develop working relationship or incorporating humour).
Reflective practice and the benefit of it?
The process by which practitioners reflect on their clinical reasoning, decision making, and practice outcomes and how our professional and personal lenses affect interaction with clients, which can be done in action (during) or on action (after)
This helps identify what went well and wrong so alternative approaches can be applied to a situation or a person to achieve a more successful outcome.
What is the purpose of an OT assessment (6 points)?
To understand the occupations that are important to a client.
To identify the client's occupational performance, specifically looking at areas of current and potential difficulty.
To identify what environmental factors impact client's occupations.
To inform clinical reasoning about the factors which facilitate or constraint occupational performance for the client.
To inform collaborative goal setting and planning for intervention.
Assessment may be used later in the OT process to monitor progress.
Why is OT assessment important in hospital settings?
Useful for anticipating the potential impact of changed capacity for OP, which is used as the basis for helping the client (and others) anticipate and effectively plan for changed OP after discharge.
What does a typical/general OT assessment process look like?
Client is admitted to hospital > referral to an OT > initial assessment (typically interview) > observational assessment > standardised assessment > planning for future (which could include setting goals, intervention plans, and follow-up).
What are five considerations for assessment in hospital settings?
Time
Location
Patient characteristics
Cultural responsiveness and safety
Access to services to assess with assessment
What information might a hospital OT need to understand a clients’ OP before admission (4 points)?
Usual routines.
Areas of OP importance in client's life (valued occupations and responsibilities).
Any areas of OP in which the client experienced difficulty (refer to the nine categories of occupations).
Any strategies/supports which facilitated OP.
What information might a hospital OT need to understand a client’s OP during hospital stay (6 points)?
How is the client managing OP within the hospital settings?
How consistent/variable has OP been in hospital?
Has the client's capacity or OP changed significantly from before admission?
What have the opportunities been for OP?
What factors might be limiting OP or underlying capacity?
What is the client's/carers expectations/concerns for OP on discharge?
What information might a hospital OT need to understand a client’s OP after discharge (5 points)?
Where will the client go after discharge?
Requirements for OP (routines and responsibilities).
Environmental barriers to successful OP.
Resources available.
Experience after previous DC (issues, strategies).
What are three main components of the overall OT assessment process?
Initial assessment
Observational assessment
Standardised assessments
What are three important objectives of the initial assessment?
Establishing therapeutic relationship
Gathering information
Determine and communicate plan
When doing an observational assessment, what should be done (2 points)?
Assessing interaction of person, environment, and occupation factors.
Completing functional tasks in a natural setting (ideally home environment but sometimes in a hospital setting, but will have limited access)
Standardised assessments
A systematic method of administration and scoring which generally provides quantifiable data which can compare clients over time to determine improvement and can compare client's performance against those of the general population.
ISBAR method
A common verbal reporting method which is a mnemonic created to improve safety in the transfer of critical information.
The mnemonic stands for Identify, Situation, Background (clinical), Assessment, and Recommendation.
When writing progress notes, what should it include (11 points)?
What happened, when, where, why (rationale), how the client/patient has responded, date of treatments, activities performed, goals achieved, problems remaining, treatment plan modification (including discharge plans), and evidence to support decisions.
What are some rules to writing clinical documentation (10 points)?
Using black ink
Don't use white out or scribble out mistakes instead, put a single line through any mistakes and sign and date corrections
Don't use any jargon
Don't use any generalities
Don't leave any blank spaces
Must include date of service
Date of recording
Signature, print name, and position
Countersigned by therapist (if written by student)
Always be client centred and concise.
SOAP method
A widespread method of documentation used across multiple health disciplines which contains crucial information about a client/patient.
The mnemonic stands for Subjective, Objective, Assessment, and Plan.
What are six principles of andragogy?
Collaborate to determine what the learners need to know
Self-directed approach. Teacher becomes facilitator/consultant
Learner’s prior experience influences learning
Readiness to learn impacts on learning
Problem or life-centred learning
Motivation - to achieve goals and resolve problems
What is it meant by ‘self-efficacy’ in relation to health promoting behaviours?
Self-efficacy is defined as an individual’s belief in their capacity to execute behaviours necessary to produce specific performance outcomes.
Giving individuals the opportunity to set goals and participate in planning how one engages in health-promoting behaviour to improve their health and wellbeing is crucial for health professionals to consider when wanting to collaborate together and equally contribute to discussing plans that are appropriate and led by the client but also, meets the requirements set by the health professional to ensure the client can successfully change their behaviour for long-term engagement and overall improve quality of life.
Health belief model (HBM) and when can it be applied (3 points)
A psychological framework that explains how personal beliefs about health issues influence health behaviours. It can be applied to facilitate behaviour change in clients, address the client’s consideration of pros and cons in decision-making, and address their self-efficacy for coping and resisting temptations or intensity of urges.
What are seven key elements of the learning and education process?
Each education task requires some analysis of the learning theory or approach to be used
Consider personal needs and readiness
Set goals (SMART)
Building knowledge/skills
Practice new behaviours
Facilitate strategies to consolidate and sustain success
Evaluate outcomes
What are six key concepts of behaviour approaches?
All behaviour is learned (other than that acquired by maturation)
Learning is derived from experience
Behaviour and learning are influenced by environment
Reinforcement influences development and maintenance of behaviour
Behaviour occurs in chains or sequences
Modelling can enable learning by imitation
Grading
Adjusting the demands of the occupation including physical, cognitive, social, and emotional demands.
What is the difference between grading up and down?
Grading up focuses on increasing the challenge/activity for the client whereas grading down focuses on making the activity easier, or providing assistance at difficult points, to enable success.
What are seventeen (not limited to) considerations of an activity/occupation to grade?
Duration
Frequency
Intensity/rate of work
Resistance/weights
Postures used
Position of the activity in relation to the person
Arrangement of objects in relation to each other
Nature and texture of materials
Level of difficulty
Size and shape of objects
No of steps
Complexity
Method or technique used
Tools used
When the activity is performed
The quality of the result required
Communication/social aspects
What are six considerations when grading?
Should be related to the client's OP goals and where possible, include activities that are related to the occupation that they are wanting to do.
Requires an activity/occupational analysis to look at what body functions/performance skills are required and what demands can be graded (see cards 12 & 13).
The activity needs to address the body functions and performance skills you are targeting.
It needs to provide the 'just-right challenge' enough to build skills but not too much to decrease motivation.
Scaffolding/assistance may be provided and graded over time.
It is a dynamic process where demands are modified in response to client's changing performance.
Adaption
A type of intervention strategy which involves modifying elements of an occupation and/or the environment to allow for successful participation. This requires flexibility and coming up with alternative ways of doing an occupation.
Discharge planning
The process of developing a personalised plan for a patient getting discharged from a health organisation.
What is the first step of discharge planning?
Review medical/health records for any relevant information on each occasion prior to seeing the patient.
What is the second step of discharge planning?
Establishing the patient and/or caregiver’s goals related to future functioning/discharge.
What is the third step of discharge planning?
Consulting (with permission) with family/caregiver regarding ability/willingness to support discharge goals/destination & current living situation. If unable to provide support, check other available sources for the patient.
What is the fourth step of discharge planning?
Assessing physical, cognitive, and ADL functioning through functional assessment process and obtaining collateral information from family/carer/support agencies and direct observation of occupational performance.
What is the fifth step of discharge planning?
Determine recovery of rehabilitation potential and access to community services.
What is the sixth step of discharge planning?
Consider the persons’ ability to participate in care including factors such as motivation, ability to apply new knowledge, capacity for new learning, ability to problem-solve, confidence, judgement, and safety insight.
What is the seventh step of discharge planning?
Utilise clinical reasoning to analyse assessment findings and establish discharge plan and consider discharge options available and match with patients’ needs.
What is the eighth step of discharge planning?
Provide treatment and education, and arrange equipment, home modifications, and referral to community agencies as indicated.
What is the ninth step of discharge planning?
Document following department guidelines including recommendations for discharge.
What to consider when curating a discharge plan (3 points)?
Patient’s physical environment and ability for social participation
Need for counselling or need for increased community support
Identify risk for discharge and consider urgent help support, equipment safety, and environmental modifications
What are three key indicators to plan and organise a home visit?
Cognitive impairment
Likely mobility/transfer/access issues
Lives alone or care provided ability is unclear
What are nine protocols and safety concerns to consider when conducting a home visit?
Arranging an appropriate time with relevant ward staff and advice of return time
Check for any medical risks & if needed, develop risk management with senior staff and for standardised operating procedures and follow these
Book transport
Arrange for partner/family to meet or be aware of visit (as relevant)
Complete risk safety assessment and develop risk management with senior staff
Ensure you have the key or is it being opened by someone else
Take all relevant equipment for client and any required medication
Having a mobile phone at all times and ensure hospital staff have this number
Ensure patient understands purpose/process of a home visit and if patient refuses to return, advice hospital ASAP, if possible, get patient to sign a waiver form for risk and document ASAP on return
What are three ethical issues that may arise?
Ethical uncertainty
Ethical distress
Ethical dilemmas
Ethical uncertainty
An ethical issue which occurs when an individual is uncertain about which moral principles apply or whether a situation is indeed a moral problem.
Ethical distress
An ethical issue which occurs when an individual knows the right course of action but, feels constrained to act otherwise by institutional or organisation rules.
Ethical dilemmas
An ethical issue which occurs when an individual faces two or more equally pleasant or unpleasant situation that are mutually exclusive.
What are six potential resource and system ethical issues that may arise?
Inadequate time, staff, funding
Working in a biomedical FOR
Excessive caseloads
Meeting the pressure to discharge clients
Who says the criteria we use to prioritise patients is correct?
Delegation of OT tasks to other professionals
What are three potential upholding values and ethical principal issues that may arise?
Telling clients the truth when it can cause more harm
Being part of a team vs disagreeing with the team decision when it is not in the best interest of the client
Doing what's best for the client vs being seen as delaying discharge
What are eight potential client safety/vulnerability issues that may arise?
Having knowledge of unsafe client behaviour (ie drug use) vs confidentiality vs client safety
Client wanting to go home and it may not be safe vs client-centred practice
Client's capacity to make decisions cannot be fully determined
You as the OT make an error in treatment
Other staff are disrepecting the client behind their back
Client/family disagrees with treatment
Using treatment that has little evidence behind it but, it may help the client
Client gives you a gift/asks you on a date vs maintain client-therapist relationship
Pressure injury (aka pressure sore, pressure ulcer, or bed sores)
A localised injury to the skin and/or underlying tissue usually over a bony prominence as a result of pressure, or pressure in combination.
What are four types of pressure injury and what defines it? (which are also extrinsic risk factors that develop pressure injuries)
Pressure (force applied)
Shear (perpendicular force)
Friction (resistance to motion in a parallel direction relative to the boundary of two surfaces)
Moisture (presence of liquid, especially water)
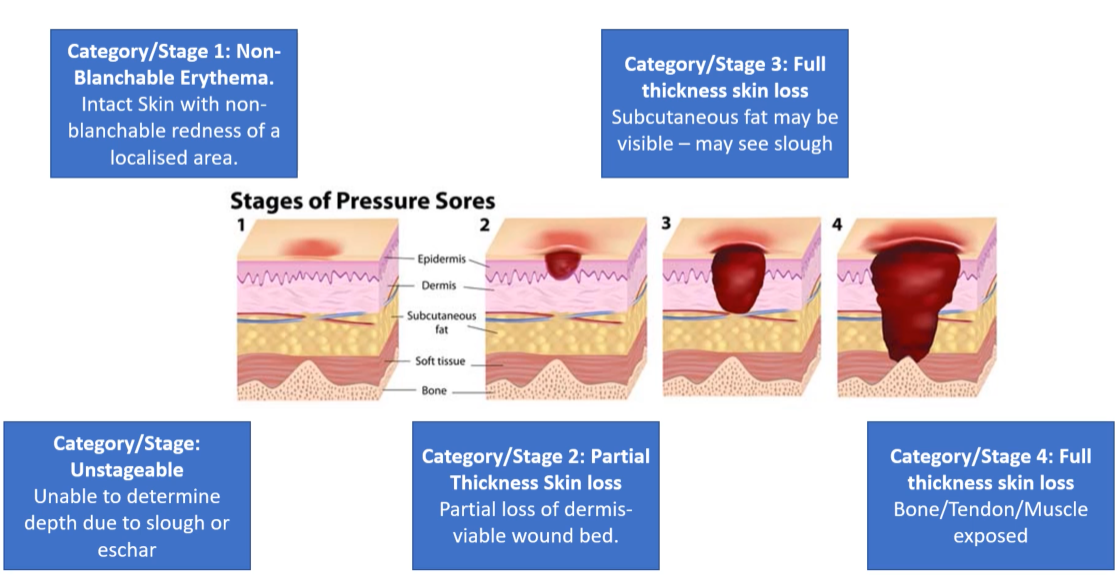
What are four stages of pressure sores?
Stage 1: Non-blanchable erythema
Stage 2: Partial thickness skin loss
Stage 3 & 4: Full thickness skin loss
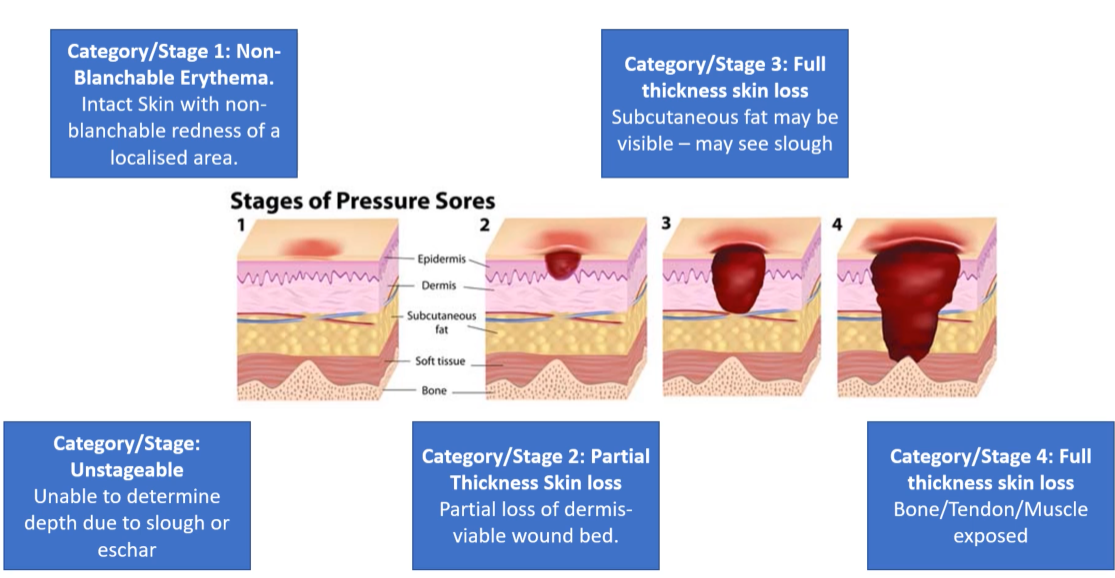
Stage 1: Non-blanchable erythema
The first stage of development of pressure sores where the intact skin is in contact with a non-blanchable redness of a localised area.
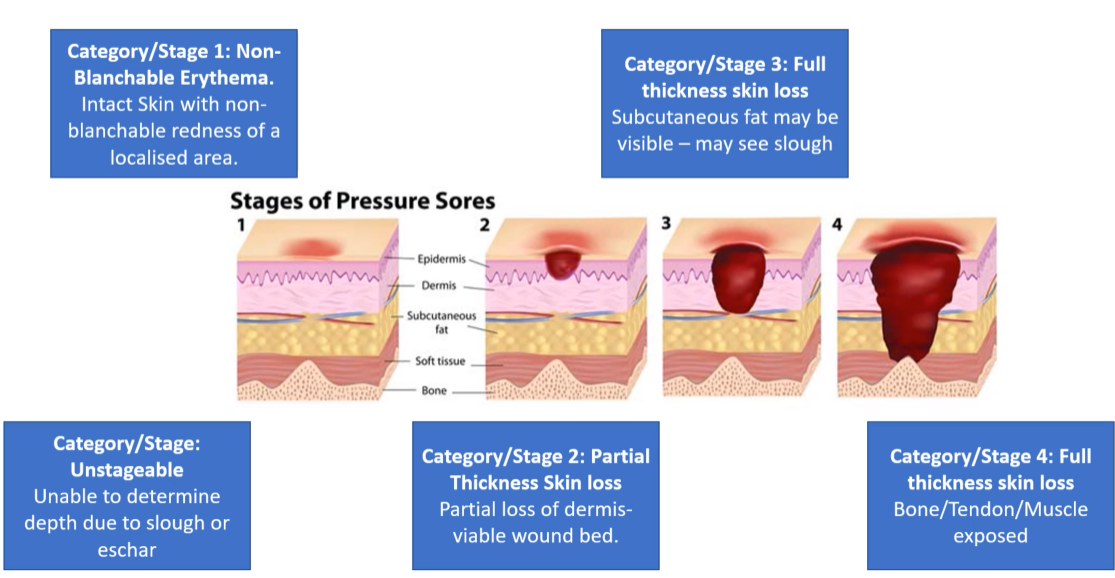
Stage 2: Partial thickness skin loss
The second stage of development of pressure sores where there is a partial loss of dermis-viable wound bed.