Plain Film Radiographs (X-Rays)
1/43
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No study sessions yet.
44 Terms
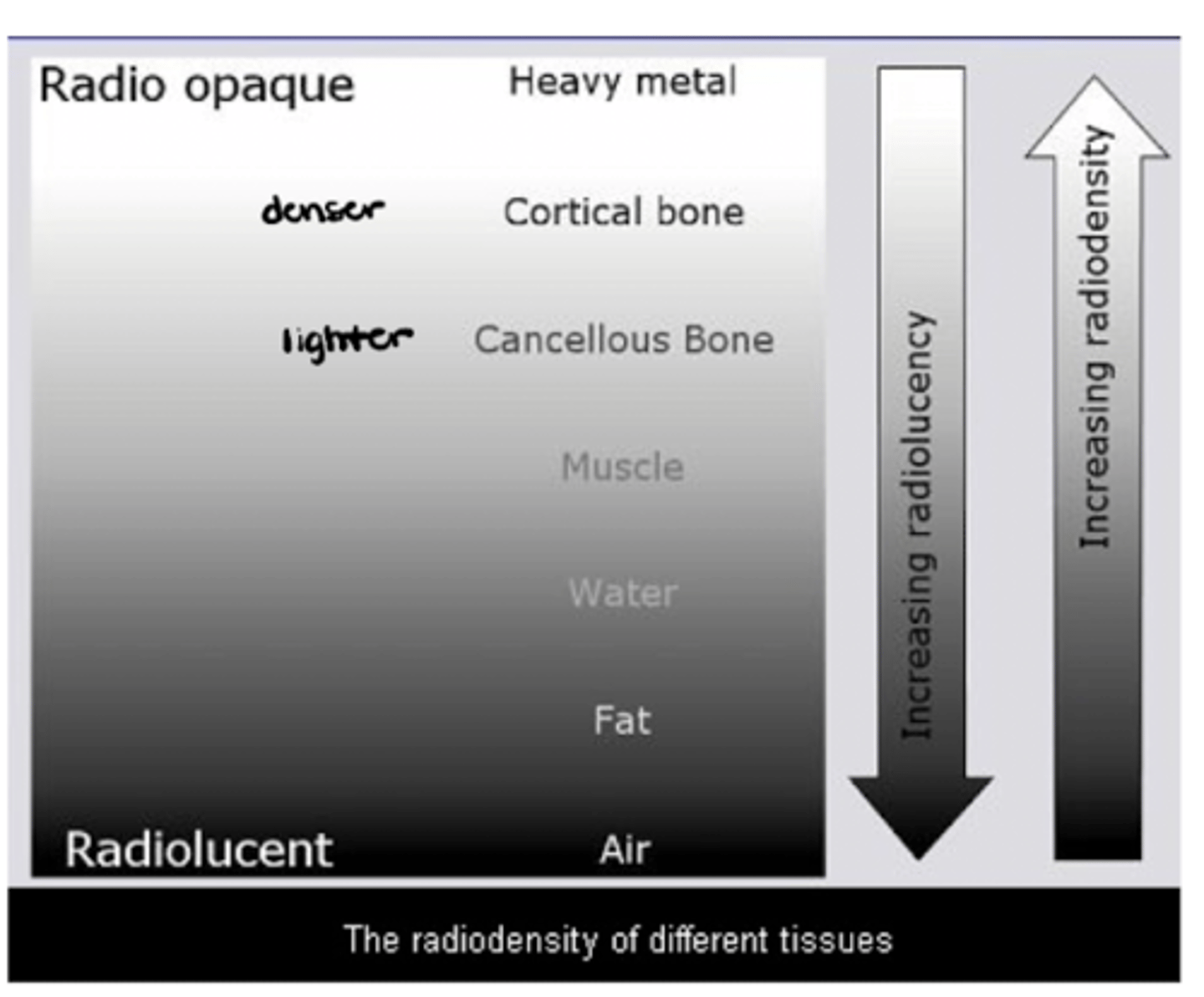
List the following in terms of MOST dense (i.e., radio opaque) to LEAST dense (i.e., radiolucent): cancellous bone, cortical bone, muscle, heavy metal, water, fat, air
Heavy metal --> cortical bone --> cancellous bone --> muscle --> water --> fat --> air
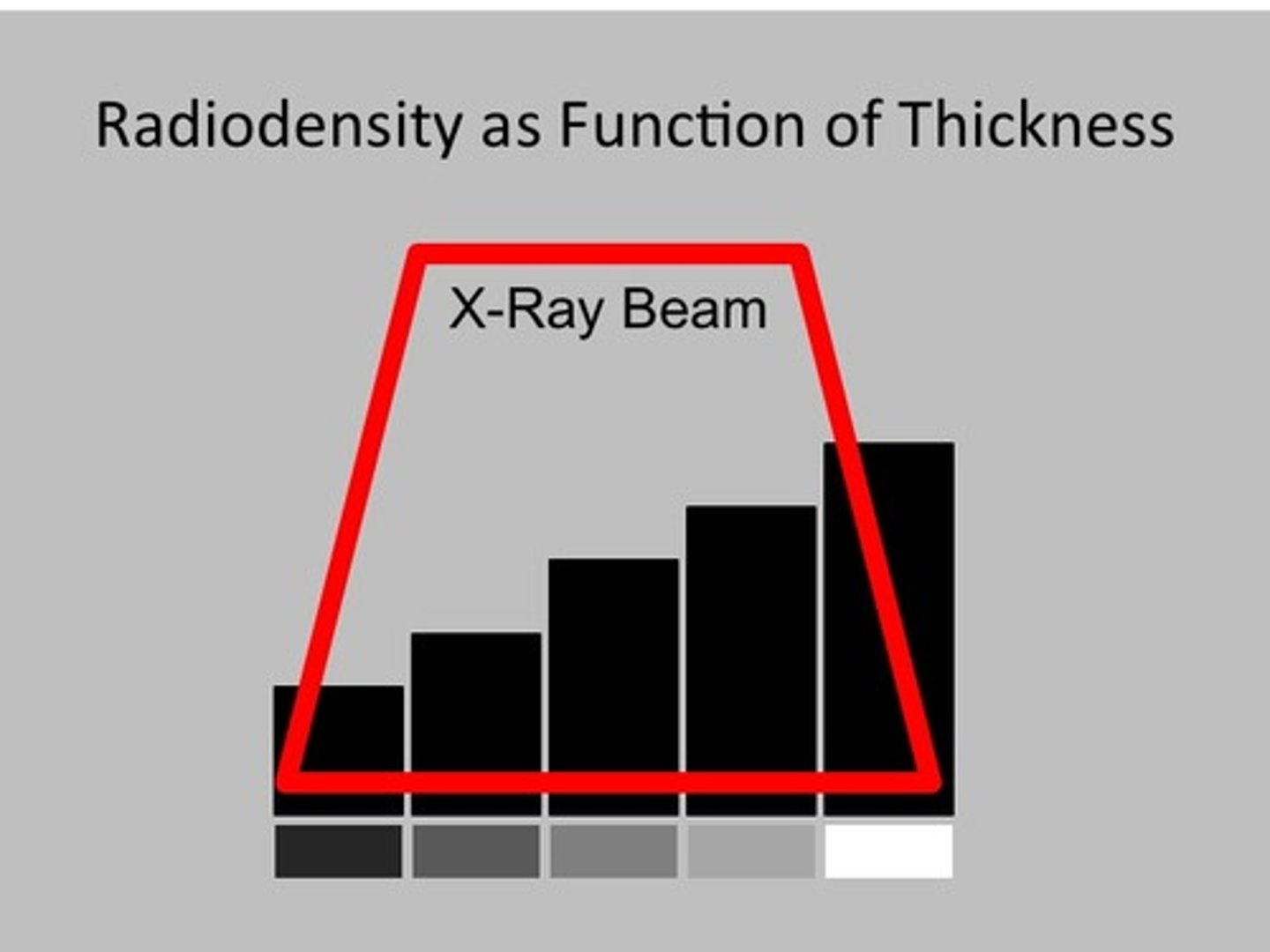
Per the concept of superimposition, density AND _________ impact radiodensity
Thickness
Superimposition _________ (increases/decreases) radiopacity
INCREASES

More x-rays are absorbed creating a BRIGHTER image on the _________ (wider/narrower) end of an object
WIDER (thicker)
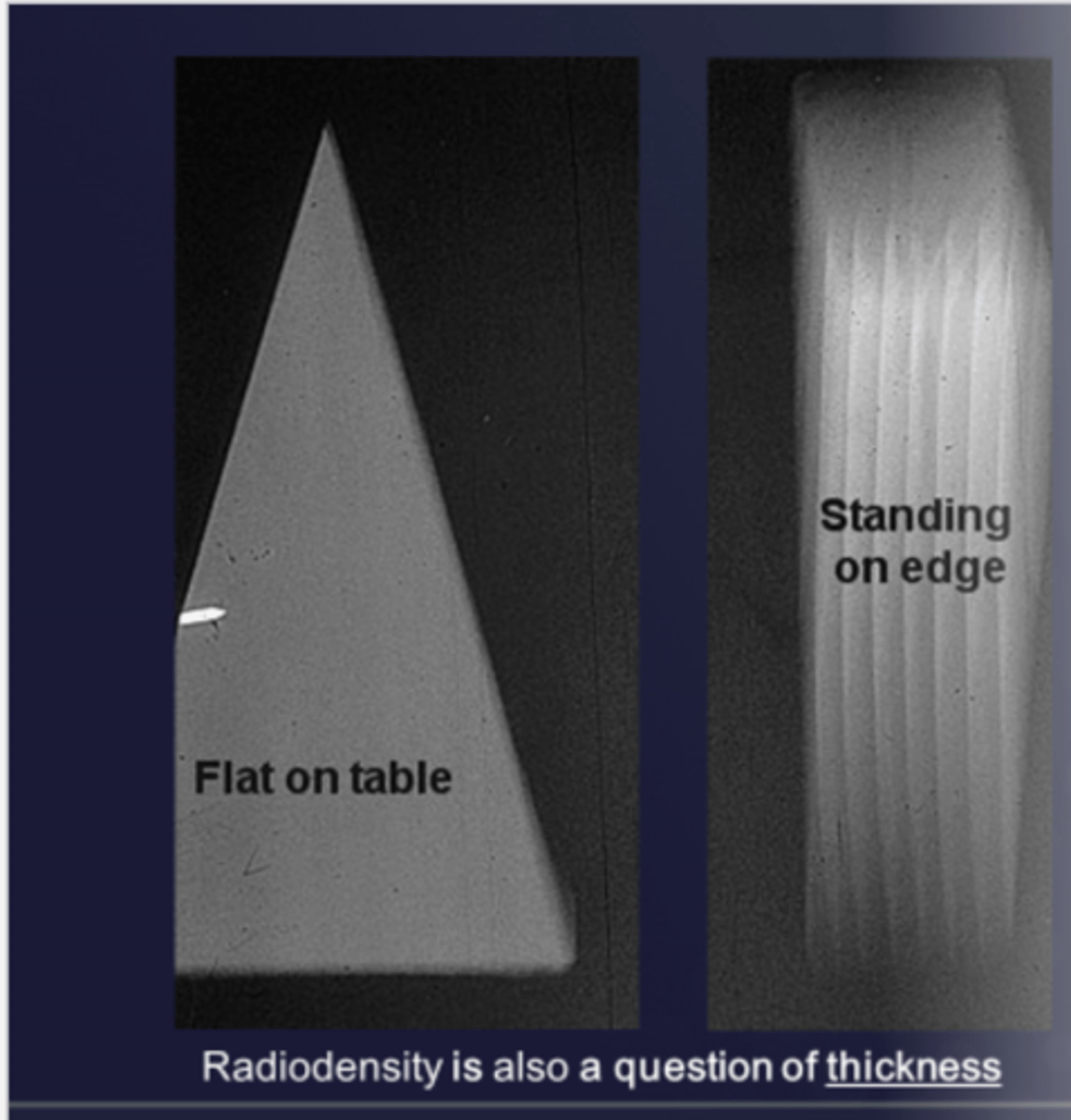
Less x-rays are absorbed creating a DARKER image on the _________ (wider/narrower) end of an object
NARROWER (thinner)

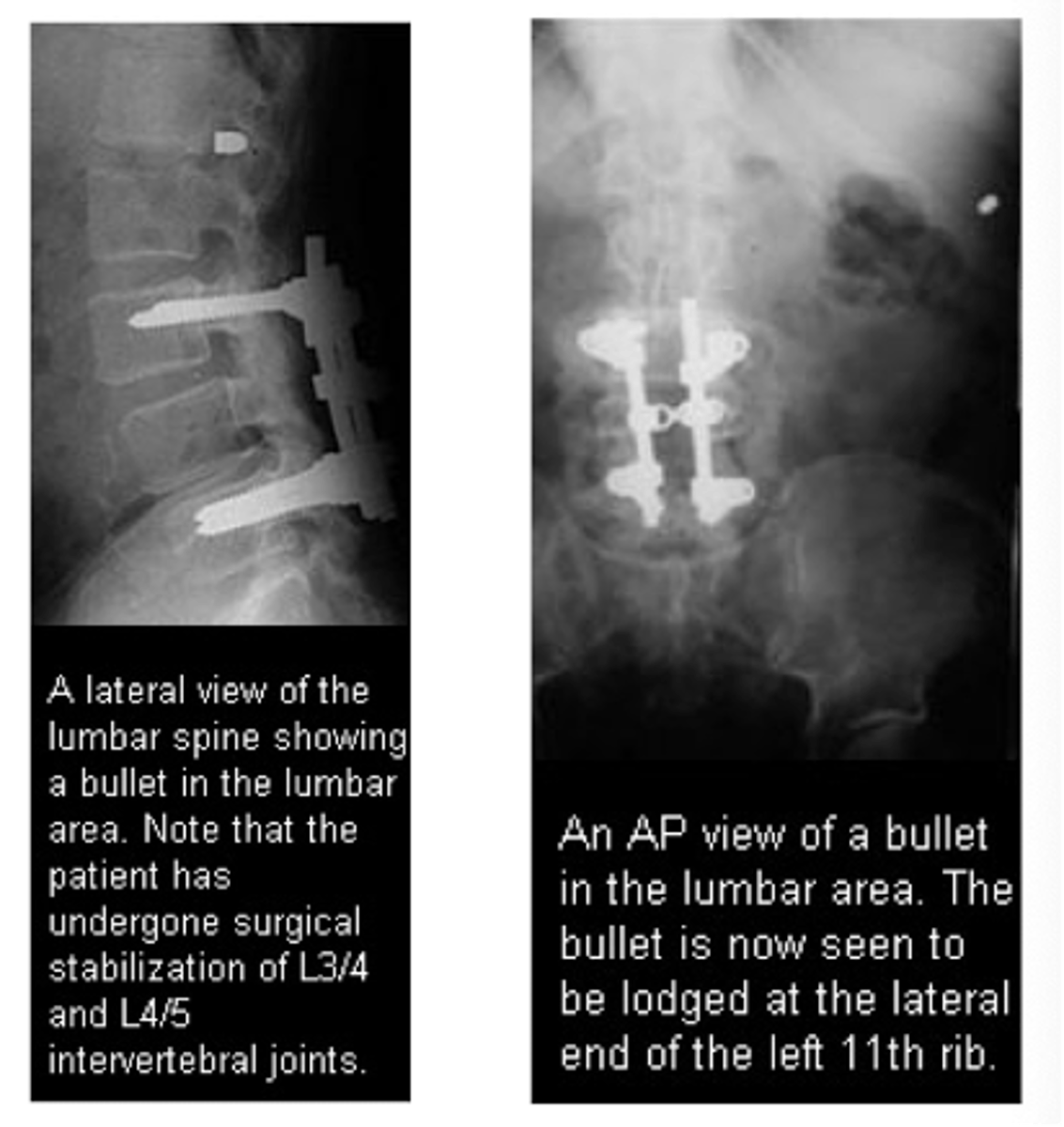
You will need at least ________ views at right angles to each other to adequately image a structure
2 views!! (pay attention to this case example!!)
VIEWS are named according to ________
Direction of the x-ray beam
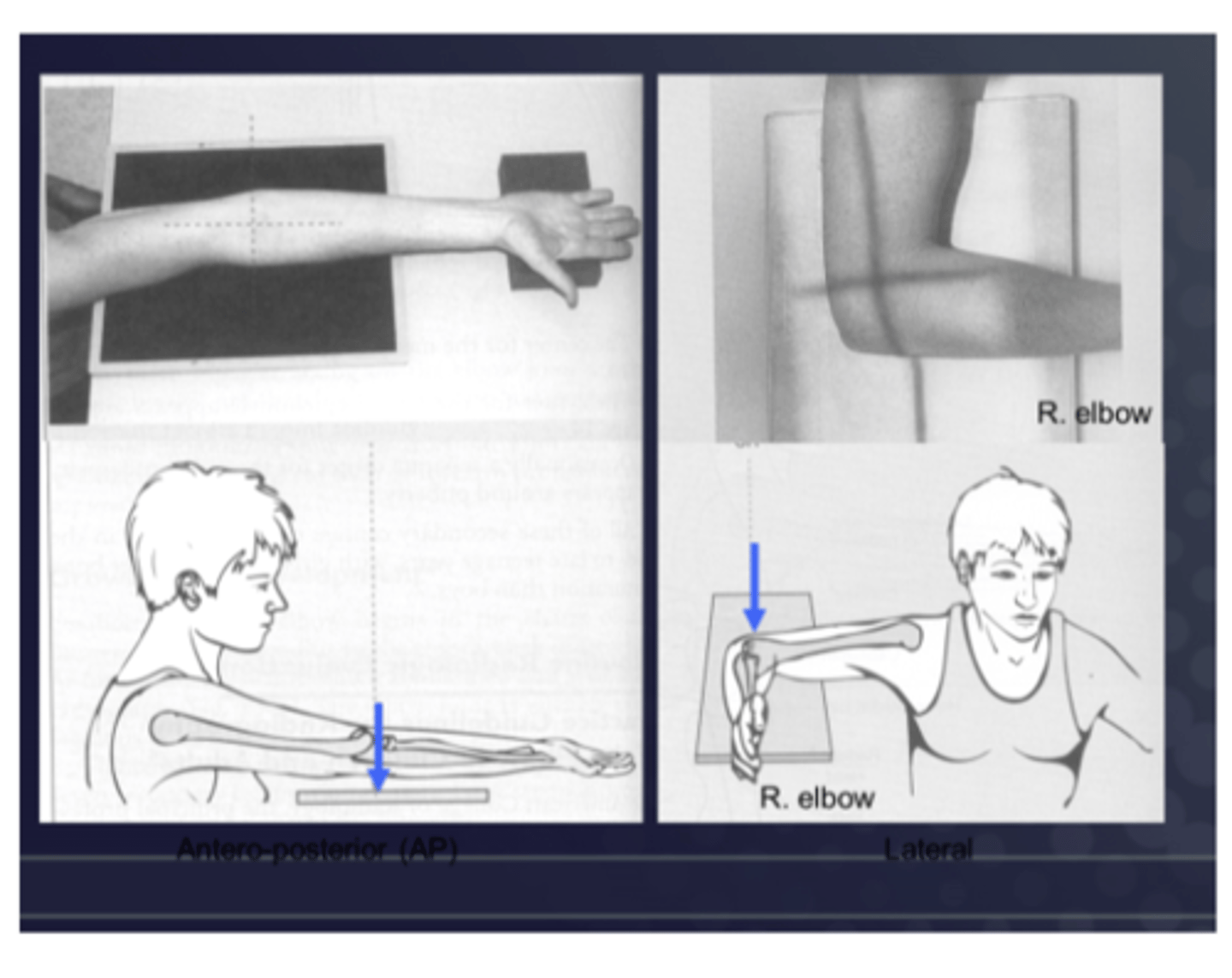
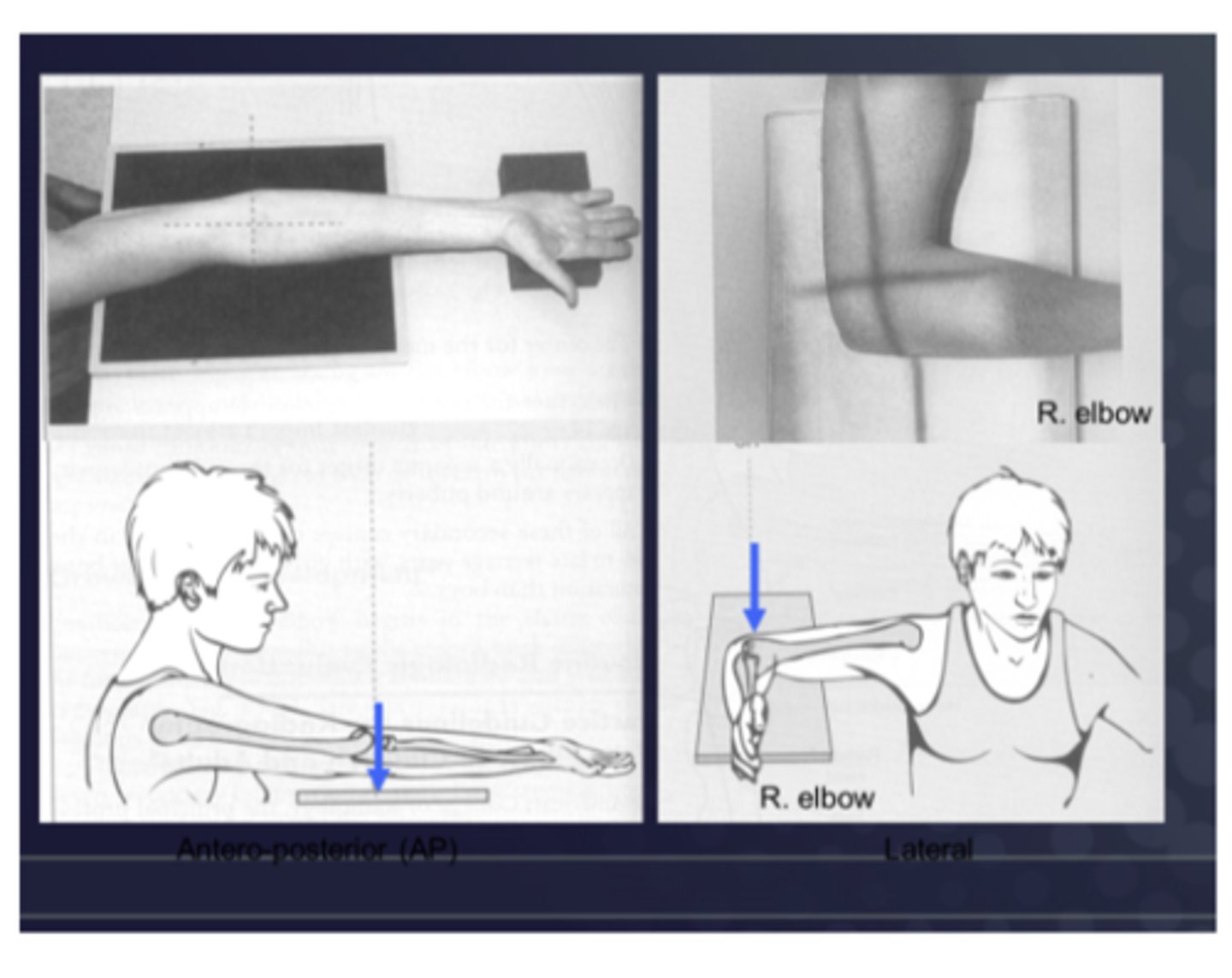
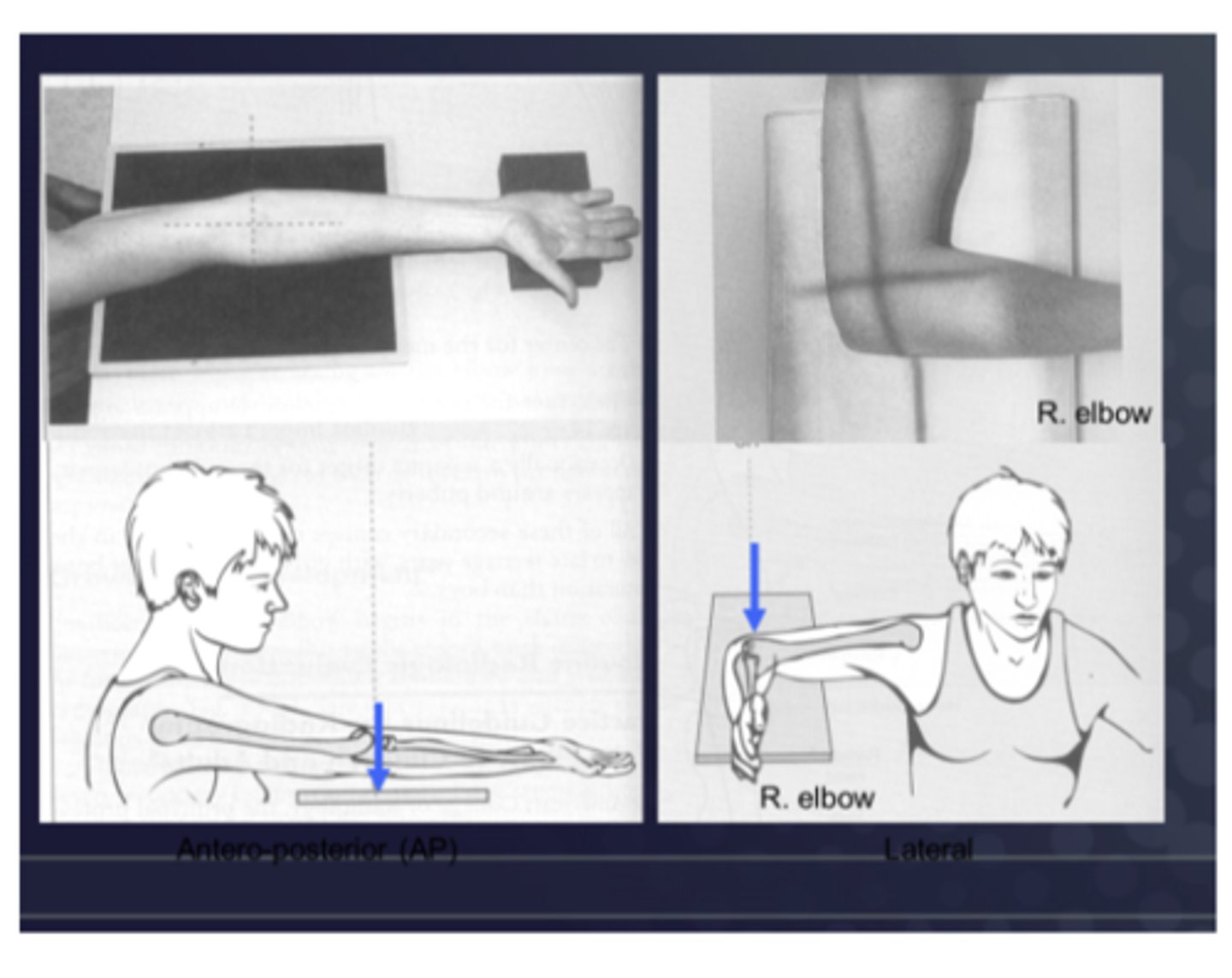
An antero-posterior (or AP) of the elbow means that the x-rays enter ________ & exit ________ where the film is placed (A in the image provided)
Enter ANTERIORLY & exit POSTERIORLY
For the MSK system, exposures for the coronal plane are typically ________ (type of view)...except for which body region?
Antero-posterior (AP)...except for the wrist & hand where the exposure is PA
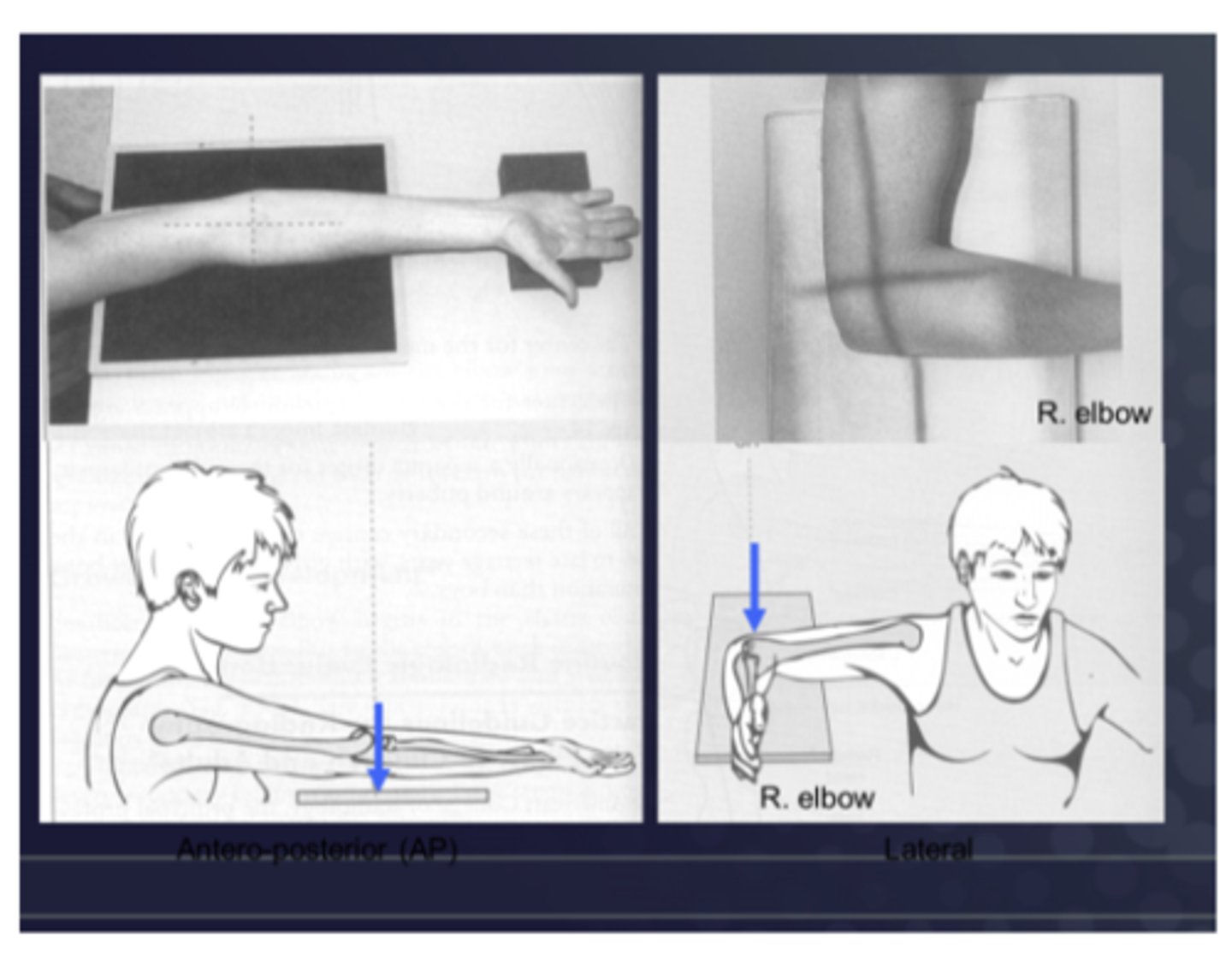
In a lateral view, film is against the medial side of the elbow and the x-rays enter ________
Laterally
Lateral and oblique projections are named according to ________
Side of the body that is closest to the film (ex: left lateral means the film is on the left side of the body)

A left lateral x-ray results in the ________ side being the most definitively represented
Left
What are the "ABCS" of interpreting a plain film radiograph?
A: alignment
B: bone density
C: cartilage spaces
S: soft tissue
List the 3x components of (A) alignment when interpreting a plain film radiograph
1. General architecture
2. General contour
3. Alignment related to adjacent bones
List the sub-components of (A) alignment: general architecture
- Aberrant size of bones
- Supernumerary bones (i.e., extra bones)
- Congenital abnormality
- Absence of any bones
- Developmental deformities

List the sub-components of (A) alignment: general contour
- Irregularities
- Cortical outline
- Spurs and osteophytes
- Fracture

List the sub-components of (A) alignment: alignment related to adjacent bones
- Dislocation
- Subluxation

List the 3x components of (B) bone density when interpreting a plain film radiograph
1. General bone density
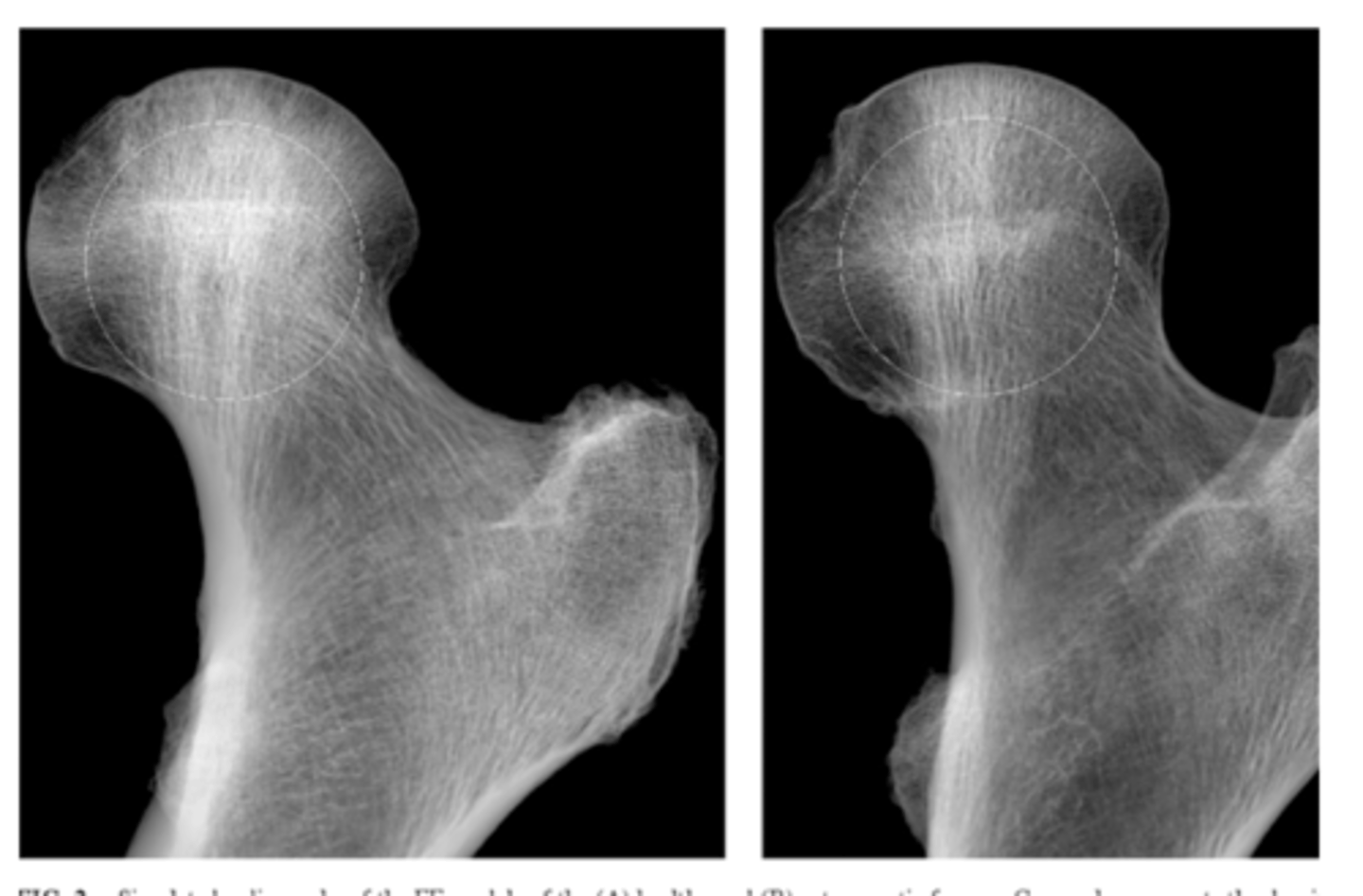
2. Textural abnormalities - trabeculae
3. Local density changes - sclerosis
List the sub-components of (B) bone density: general bone density
- Contrast b/w bone and adj. soft tissue
- Contrast within the bone itself (cancellous vs. cortical bone)
Explain why evaluating (B) bone density: textural abnormalities - trabeculae is clinically relevant
A decrease in bone density may indicate osteoporosis
**be careful in distinguishing osteoporosis from what normally looks radiolucent (i.e., it is normal for trabecular bone to be less dense than cortical bone)**
What is sclerosis?
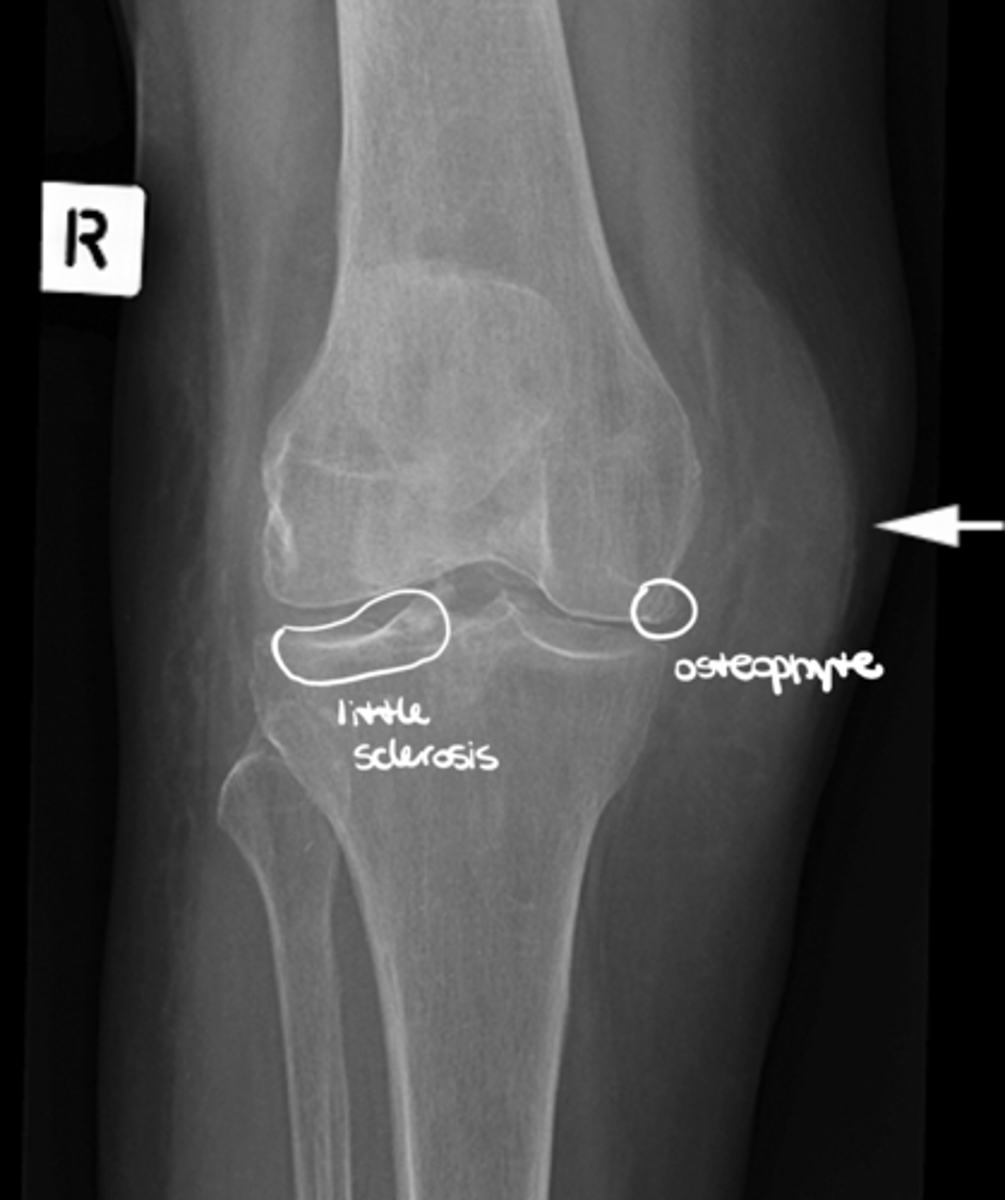
Hardening of the bone tissue at the joint line (often a primary indicator of OA)

List the 3x components of (C) cartilage space when interpreting plain film radiographs
1. "space" can be an indirect assessment of radiolucent cartilage
2. Subchondral bone -- sclerosis vs. erosions
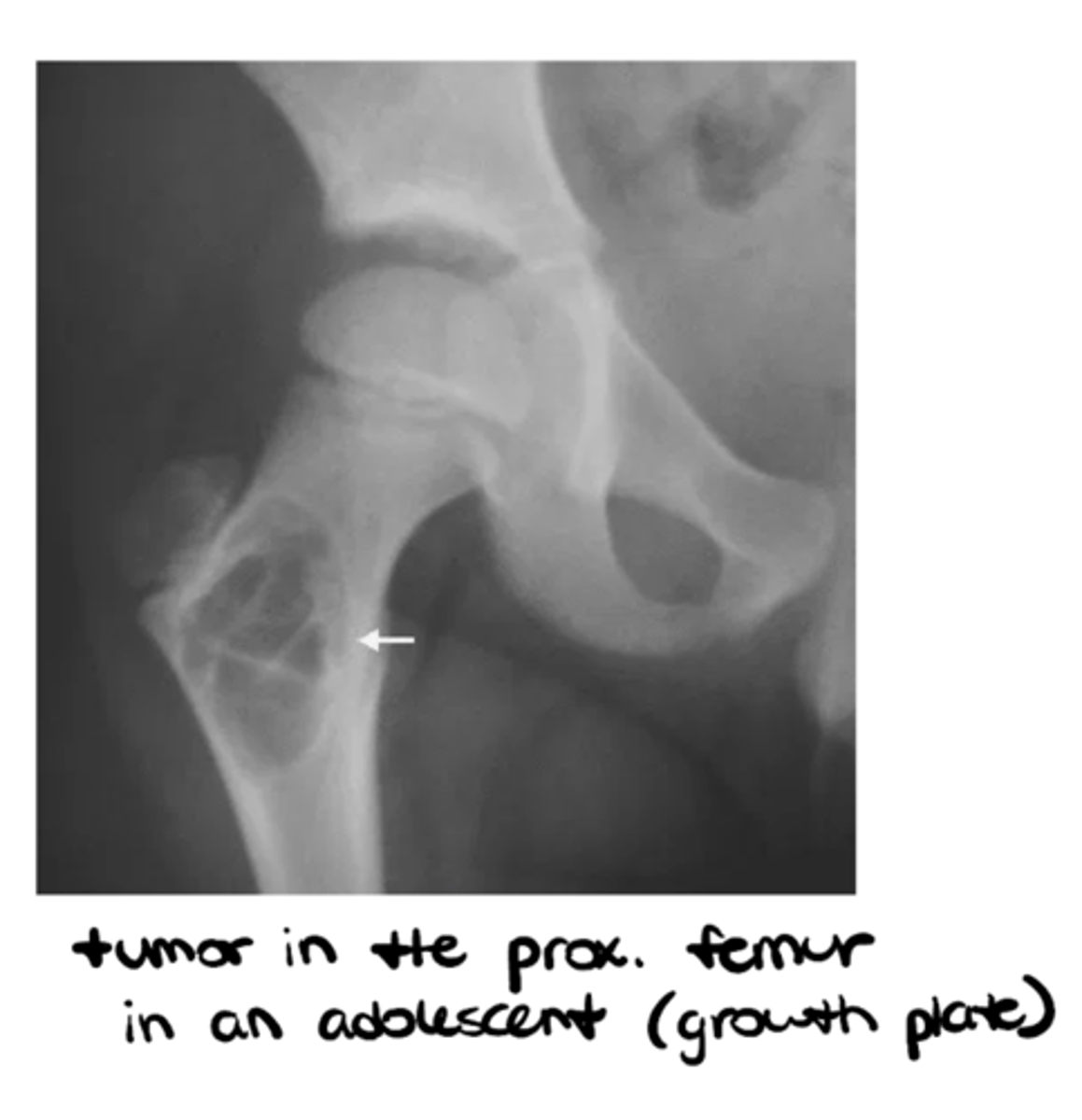
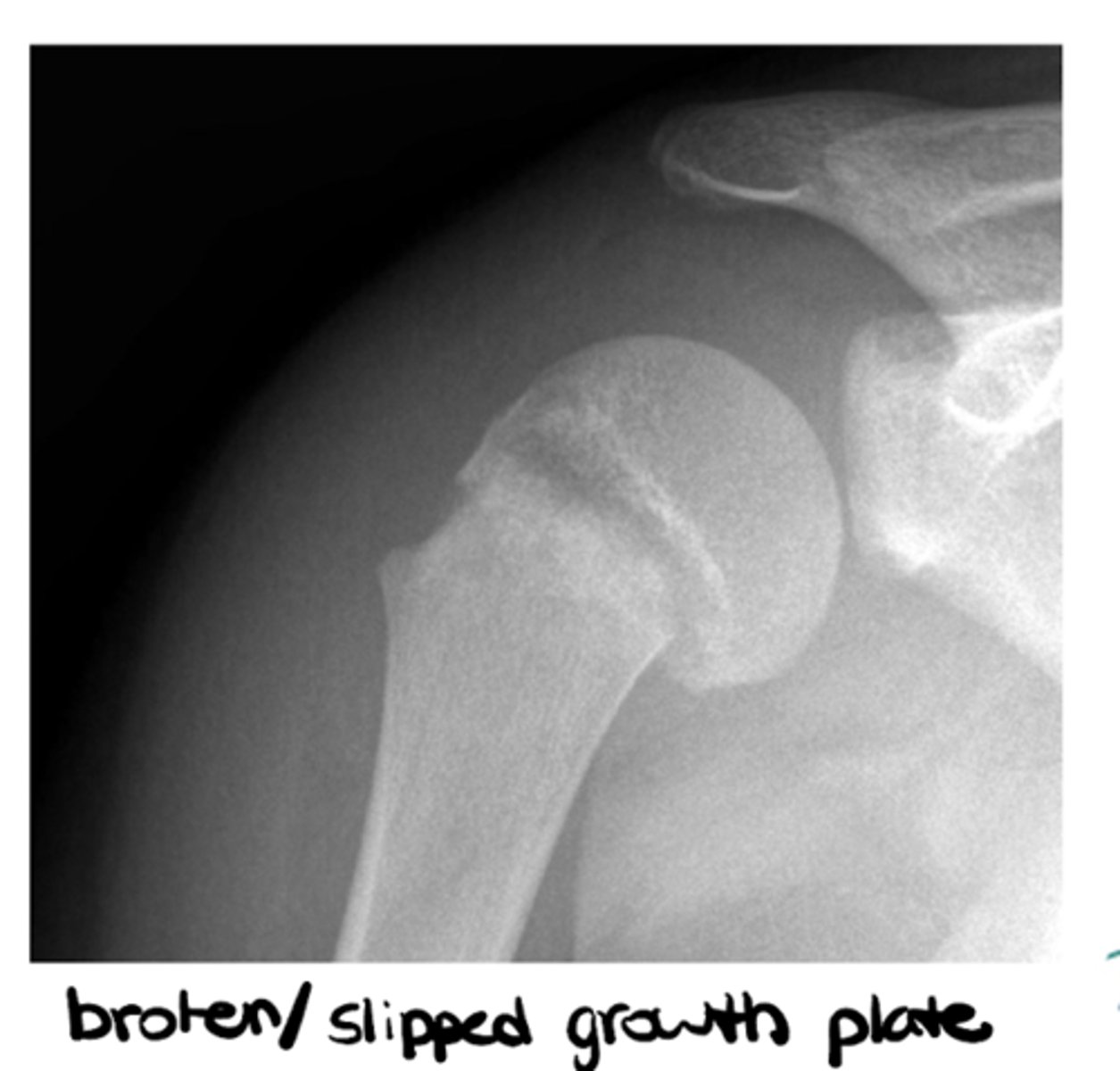
3. Epiphyseal plates
True or false: we cannot really see cartilage w/ a plain film radiograph because it is mostly H2O
TRUE!!
If we identify a loss of joint space on a plain film radiograph, what may this imply?
Loss of cartilage (primary indication of OA, along with bone spurs and sclerosis)
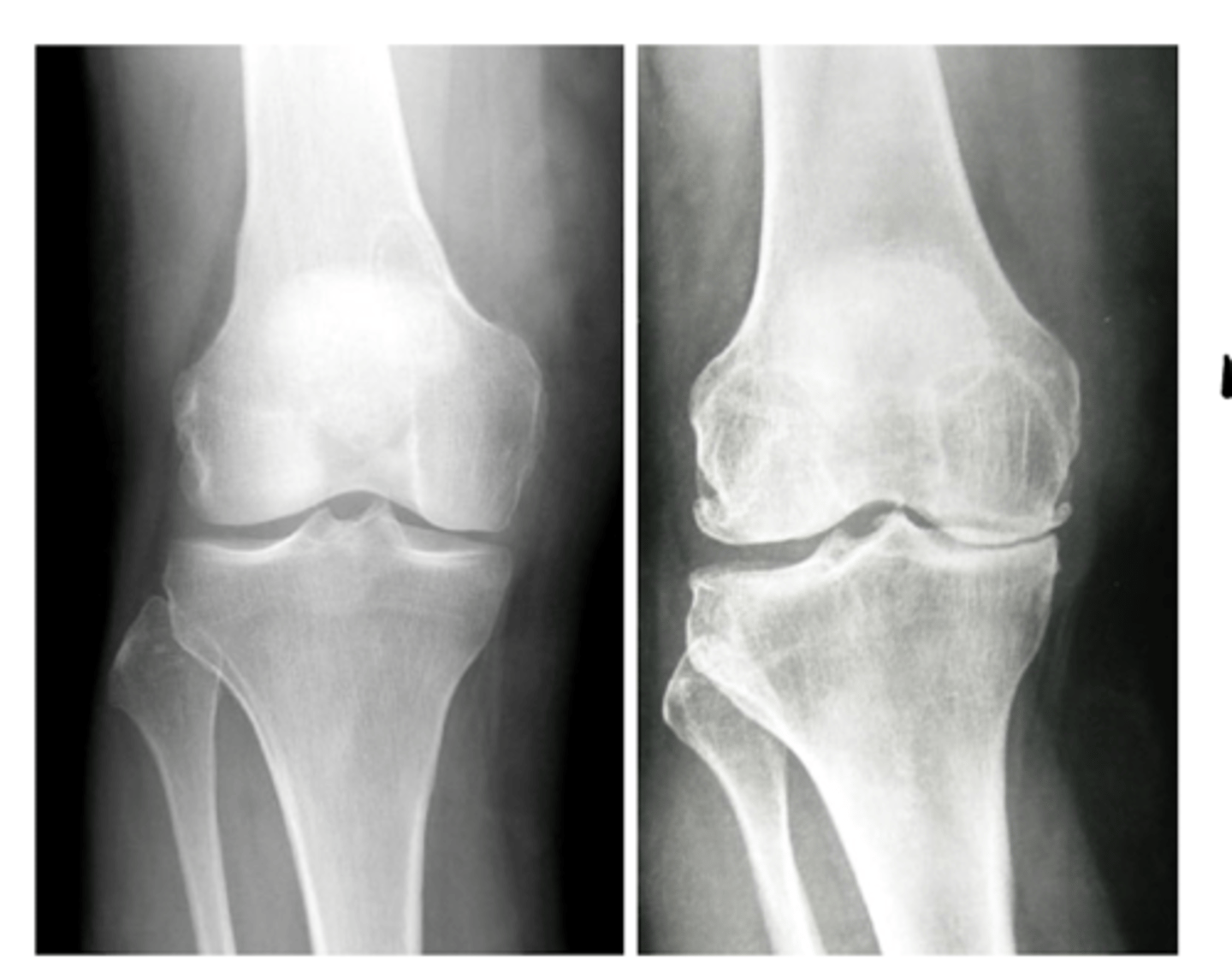
What are erosions? What do they indicate?
Scalloped, notched edges that indicate cartilage damage and wearing away of bone -- think rheumatic diseases (RA, PA, etc.)

What are epiphyseal plates? What do they indicate?
Cartilage in the middle of bone that gives the bone room to grow and solidifies over time -- think pediatric patients
List the 5x components of (S) soft tissues when interpreting plain film radiographs
1. Muscles - atrophy - swelling (ex: swelling around the knee joint as seen in this image)
2. Fat pads and fat lines
3. Joint capsules - effusion
4. Periosteum
5. Miscellaneous
What is a "sail sign"? What is it caused by?
Elevation of a fat pad (ex: when the elbow is injured, it fills up with fluid that pushes the fat pad and lifts it away from the bone itself)
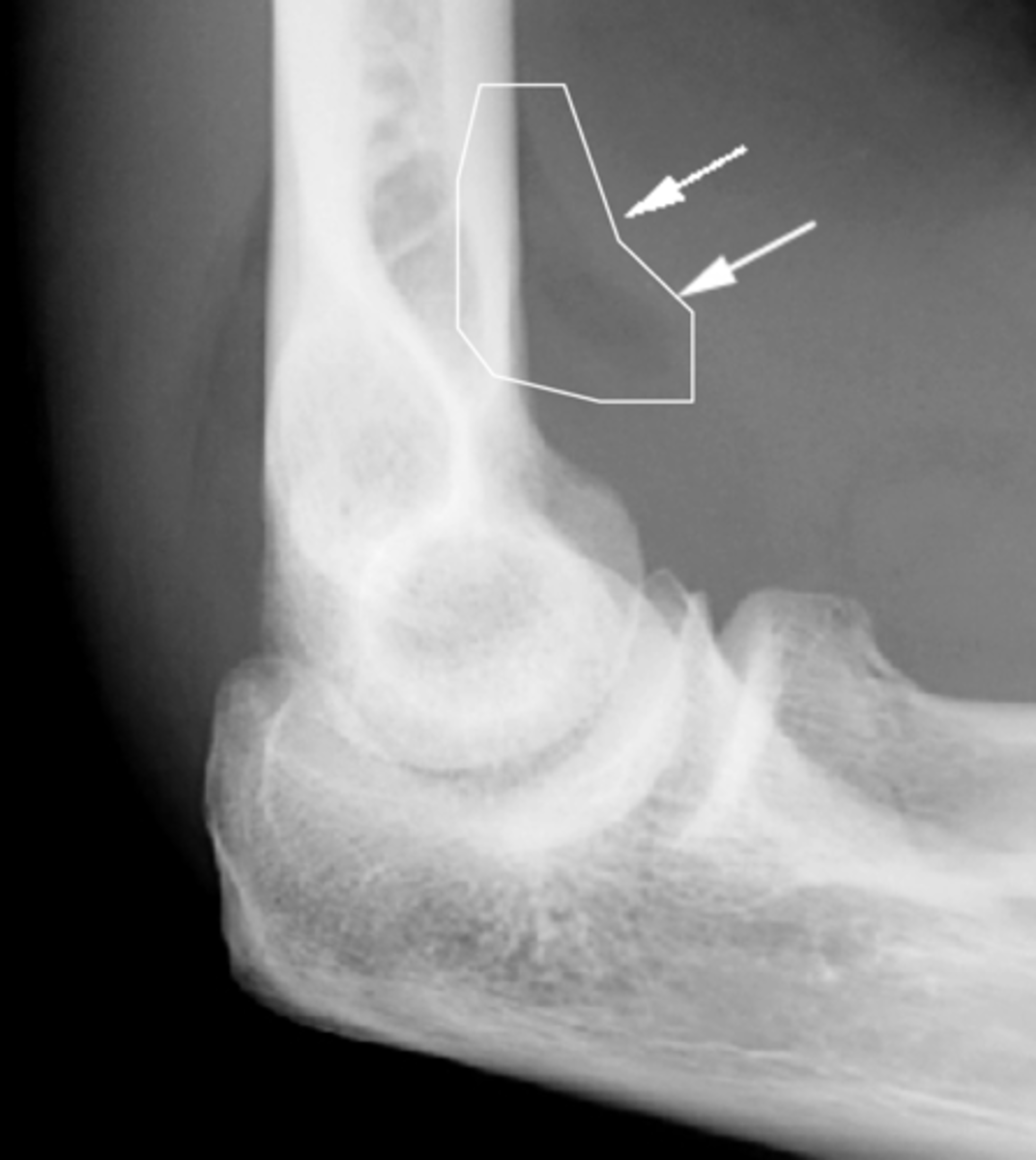
What indicates effusion of a joint capsule on a plain film radiograph?
Radiolucent joint recess due to joint swelling (i.e., effusion) that pushes the proximal superior recess out

List the sub-components of (S) soft tissues: periosteum (sheath outside of cortical bone that sits on top of it)
- Solid
- Laminated
- Sunburst
- Codman's triangle

List the sub-components of (S) soft tissues: miscellaneous
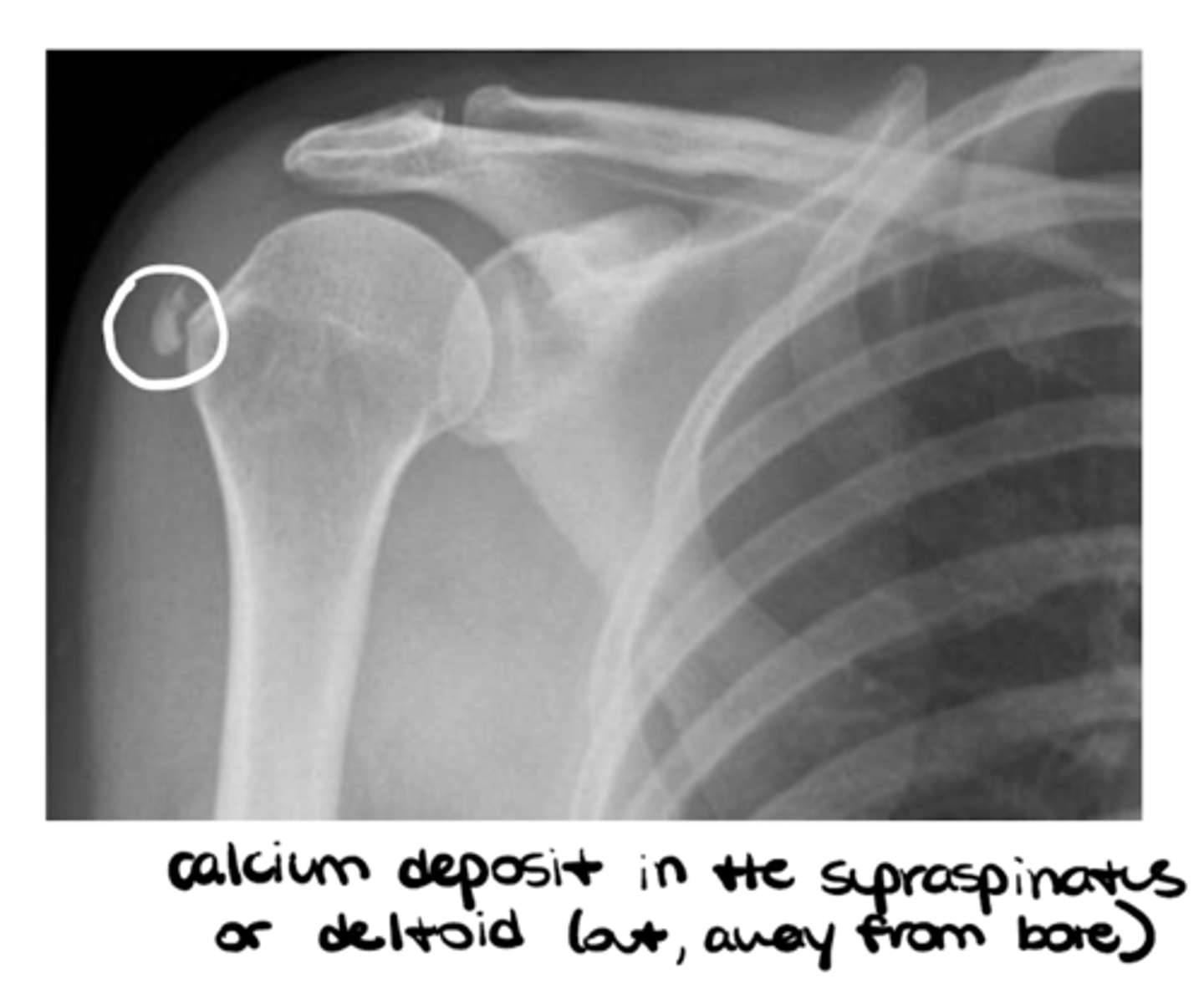
- Foreign body
- Calcifications
List the 9 requisite skills a PT must have to refer a patient for MSK imaging
1. Triaging the patient
2. Utilizing evidence-based imaging guidelines (esp. ACR criteria)
3. Considering risk/benefit of imaging
4. Requesting imaging (either directly to a radiologist or through an intermediary such as a PCP)
5. Suggesting an imaging modality
6. Reviewing imaging reports
7. Educating patients on imaging findings
8. Integrating findings into the treatment pan
9. Referring to another provider when outside SOP
What are 5 reasons America performs excessive and unwarranted imaging?
1. Medical liability fears
2. Patient demand
3. Economic motivation
4. Physicians unaware of guidelines
5. Lack of complete history and physical exam
What are 5 questions to ask to determine the risk vs. benefits of imaging (per Choose Wisely)?
1. Do I really need this test or procedure?
2. What are the risks and side effects?
3. Are there simpler, safer options?
4. What happens if I don't do anything?
5. How much does it cost, and will my insurance pay for it?
What are some risks associated with imaging modalities?
Harm (ex: radiation), expense, may be waste of time, can increase anxiety, can lead to more tests
What does VOMIT mean? Provide an example.
Victim of Medical Imaging Technology (ex: imaging shows pathology --> patient automatically gets tx that may/may not ACTUALLLY be necessary)
What does BARF mean? Provide an example.
Brainless Application of Radiological Findings (ex: poor physical exam --> lazy ordering of imaging)
True or false: often, radiological findings are normal, healthy part of aging
TRUE!! (HOWEVER, don't go TOO extreme to think that imaging NEVER matters)
Generally speaking, when is imaging indicated? (hint: 3x)
1. "Significant" trauma (severity, suspected fracture, dislocation, radiating pain)
2. No improvement after 4-6 weeks
3. Red flags - infection/cancer
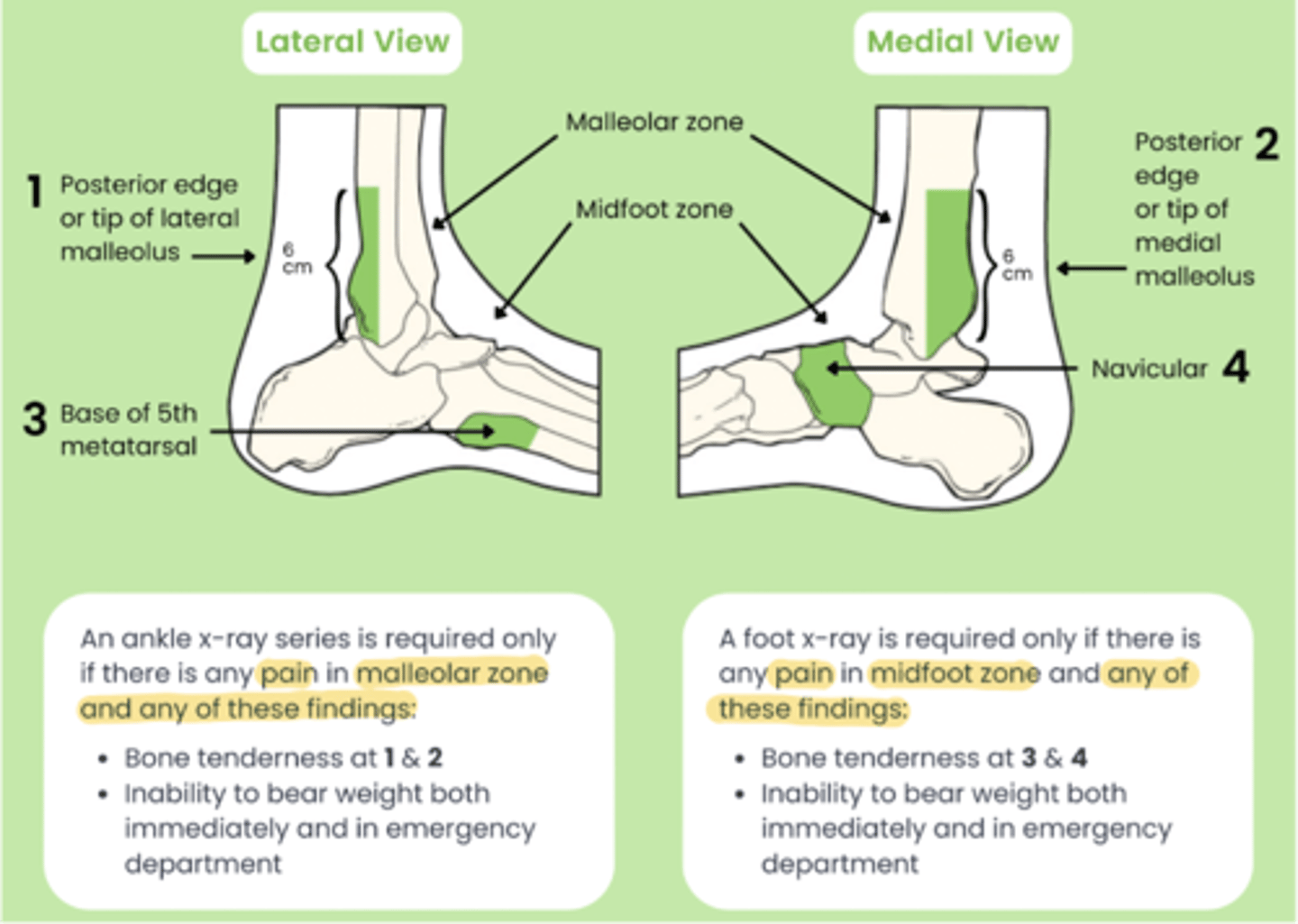
What are 3x HUGE evidence-based guidelines to rule OUT the need for imaging in the MSK world?
1. Ottawa Ankle Rules
2. Ottawa Knee Rules
3. Canadian C-Spine Rules
Pop off Canada

Per the Ottawa Ankle Rules, when is an ankle x-ray series required?
Any pain in malleolar zone AND any of these findings:
- bone tenderness at 1 & 2 (i..e, posterior edge or tip of either malleolus)
- inability to bear weight both immediately and in ER
Any pain in midfoot zone AND any of these findings:
- bone tenderness at 3 & 4 (i.e., base of M5 or navicular)
- inability to bear weight both immediately and in ER
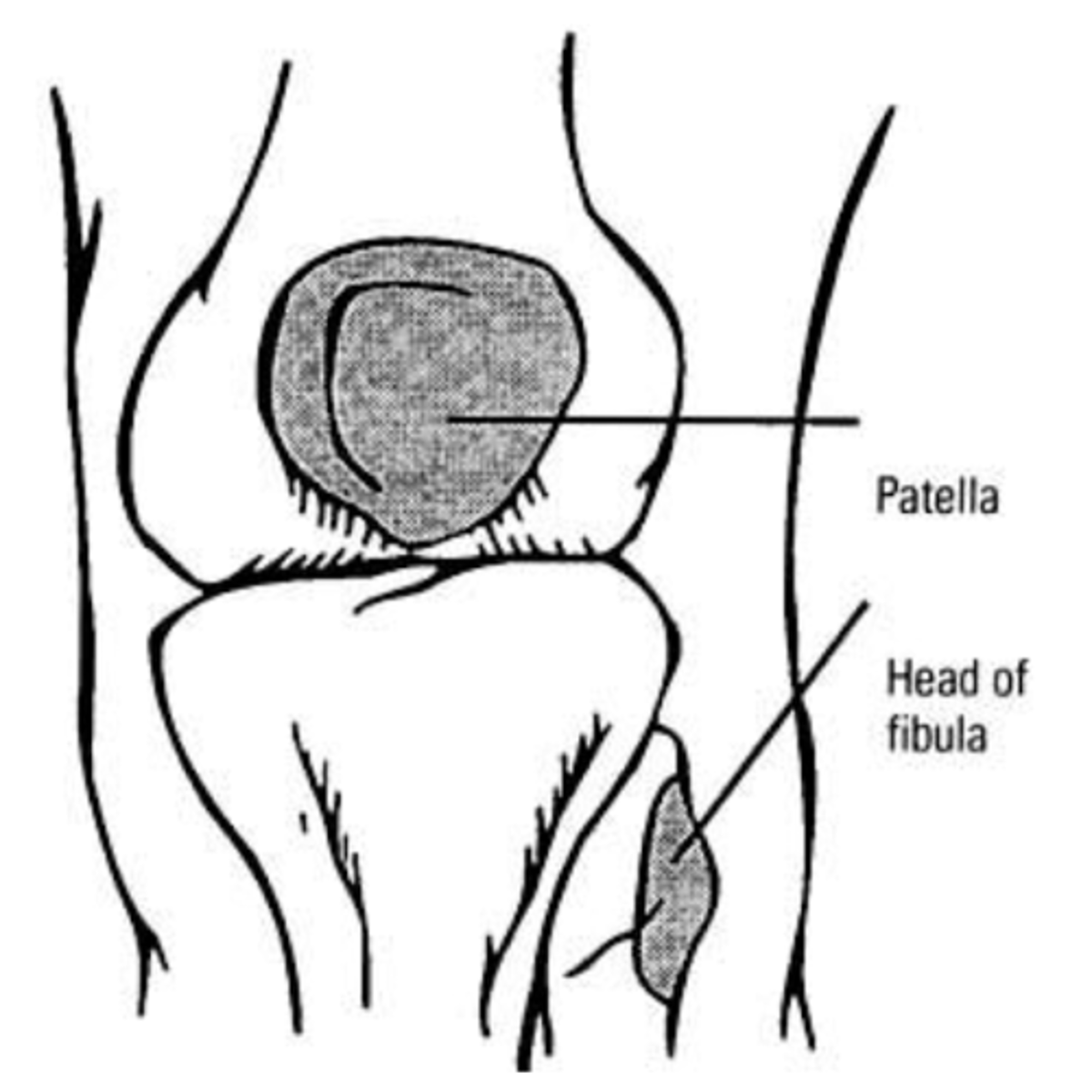
Per the Ottawa Knee Rules, when is a knee x-ray series required?
Knee injury patients with ANY of these findings:
1. Age 55+
2. Isolated tenderness of patella
3. Tenderness at head of fibula
4. Inability to flex to 90
5. Inability to bear weight both immediately and in the ER (4 steps)
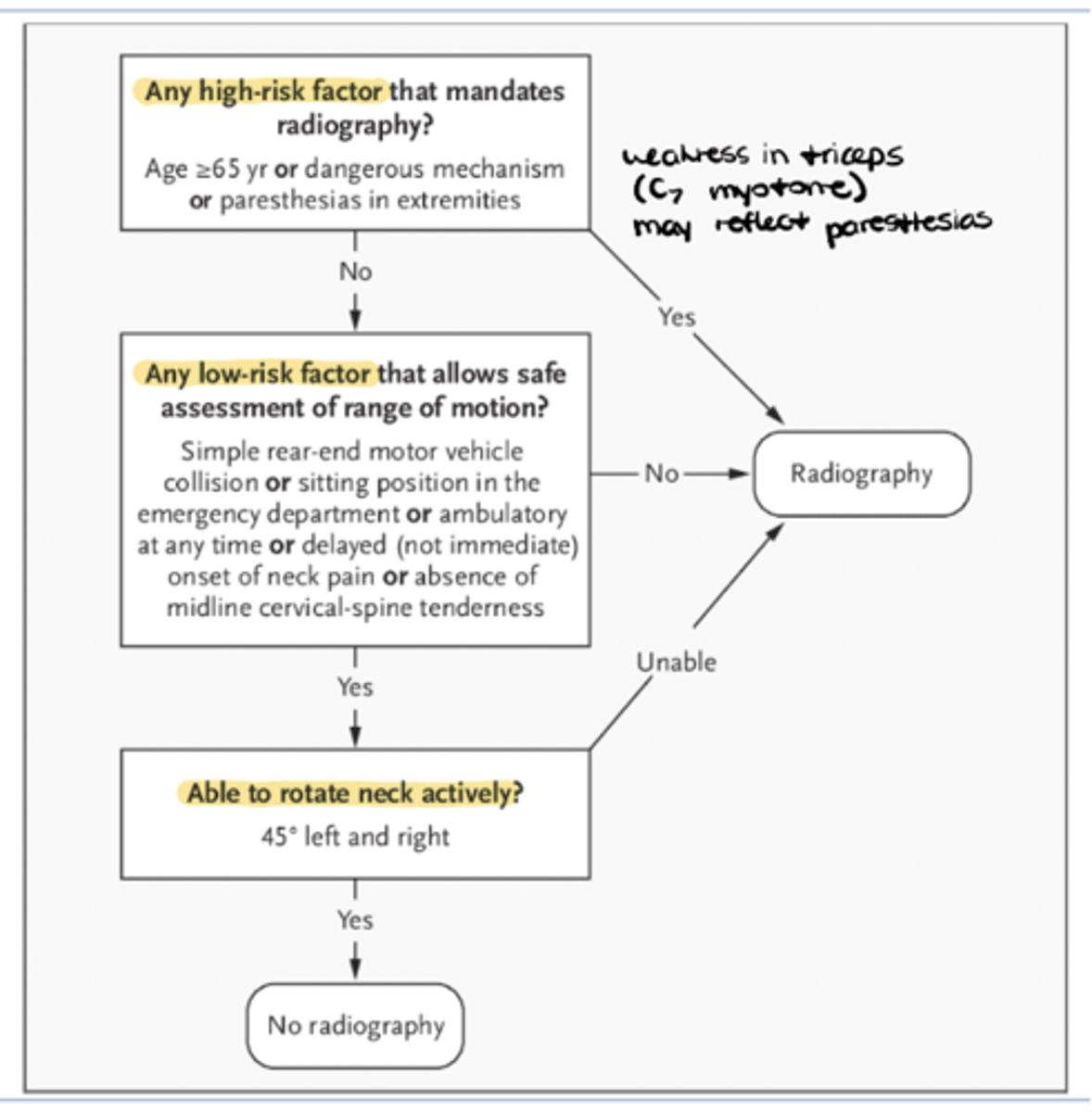
Per the Canadian C-Spine Rules, when is a cervical spine x-ray series required?
1. Any high risk factors = YES RADIOGRAPHY
- age 65+
- dangerous MOI
- paresthesias
2. Low-risk factors that allow safe assessment of ROM = NO RADIOGRAPHY
- simple rear-end MVC
- able to sit in ER
- ambulatory at any time
- delayed onset of neck pain
- absence of midline c-spine tenderness
3. Able to rotate neck activity 45 left AND right = NO RADIOGRAPHY
How do we apply the ACR appropriateness criteria to cases of MSK pain or injury?
Enter in your specific patient case and determine what types of imaging are DEFINITELY NOT appropriate and recognize that a lot of green lights aren't necessarily indicated