CT1 W6 Mod 20, 18, 19 Area specific Curets, Universal Curet, Subgingival Calculus Removal
1/27
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
28 Terms
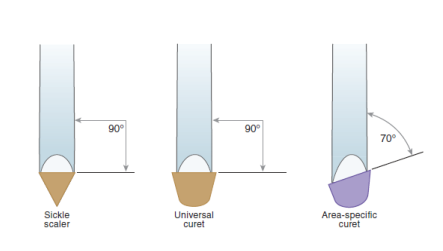
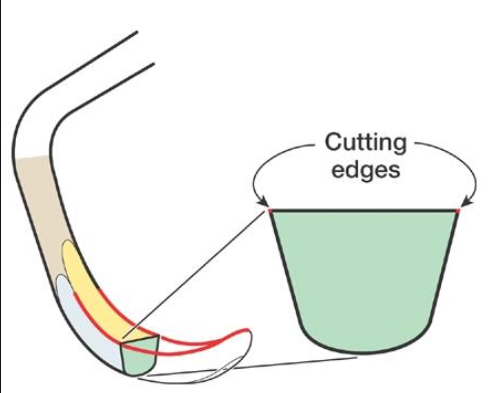
Describe the design of a Area-specific Curet
Long, complex functional shank
suited for instrumentation of root surfaces
Face tilted in relation to lower shank
Only ONY edge per working end is used.
Rounded back, rounded toe, semi-circular cross section
Curved cutting edge
**Difference to Universal Curets is that Area-Specific Curet’s face is TILTED in relation to lower shank.
causes one cutting edge to be lower than the other.
**Area specific curet is also called Gracey series.
What does working cutting edge mean?
Area Specific Curets have a tilted face, the lower cutting edge is the one that is being used therefore called the working cutting edge.
the non-cutting edge is angled away, protecting tissue from damage
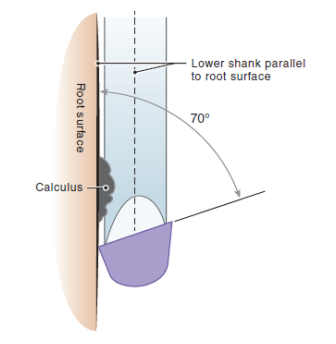
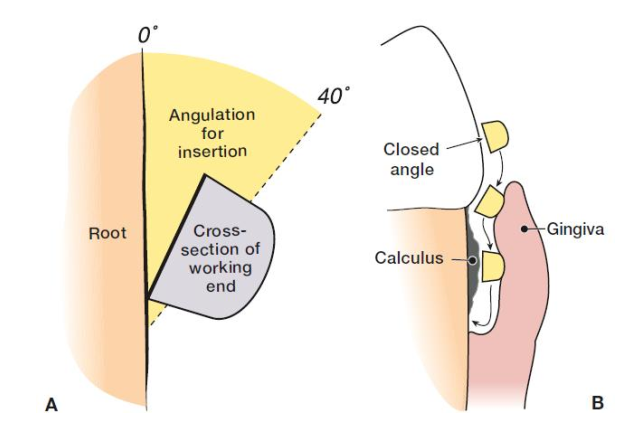
How do we angulate the Area-specific curet?
Since the lower cutting edge is already at 70 deg, we hold the instrument shank parallel to the tooth surface
The original Gracey series has how many instruments?
14 curets called Gracey 1- 14, they are paired, double ended instruments
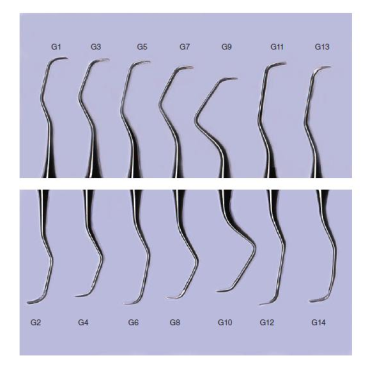
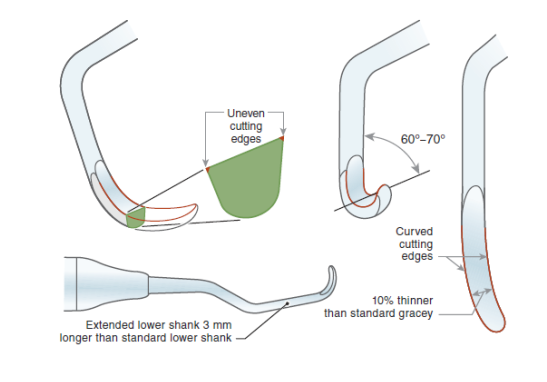
Modified versions of Gracey 11/12 and 13/14 is called…? What was the modification?
Gracey 15/16 and 17/18
Modification: developed to provide better access to proximal, mesial/distal surfaces of POSTERIOR teeth.
What are some downsides to the Gracey/Area-specific Curet?
Effectiveness of the Gracey decreased with increasing pocket depth
Treatment of periodontally involved patients required more specialized instruments to reach into pockets and to work in smaller, tighter spaces because of furcation, and root concavities
How many Gracey curets are needed to complete the FACIAL aspect of posterior sextant?
at least 2 double ended
ex. Gracey 11/12, 13/14 or 15/16 and 17/18
What is an advantage of the modified pairing in Gracey Curets?
The entire aspect of a sextant can be completed without changing instrument
Gracey uses what type of stroke to remove calculus below the gingival margin?
Horizontal strokes below gingival margin → especially useful for deposits near distofacial/distolingual line angle of posterior teeth AND midline of facial/lingual surfaces of anterior teeth.
What are the 3 most important concepts for deciding when to apply pressure onto the instrument when using a Area-Specific Curet/Gracey?
Gauge amount of pressure → use as little force as possible to remove calculus
Apply brief pressure → pressure applied before and during calculus removal; NOT constant pressure between strokes
Relax after each stroke to prevent self-injury
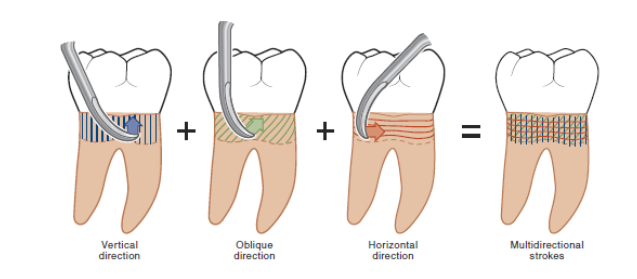
A combination of vertical, oblique and horizontal strokes are used to….
create a grid that covers the entire root surface when instrumenting on root surfaces
Subgingival calculus deposits are most commonly located….
Just apical to the CEJ, on line angles, and within root furcation areas
Define Insertion
Insertion is the act of gently sliding the working-end of an subgingival instrument beneath the gingival margin into the sulcus or gingival pocket
During insertion, the face-to-tooth surface angulation is …? This angle is called?
0-40 deg → called a Closed Angle since the face is closed against the tooth
Define Periodontal Instrumentation.
Periodontal instrumentation is defined as the removal or disruption of plaque biofilm as its by-products, and calculus deposits from coronal and root surfaces.
Goal: re-establish periodontal health and restore balance between bacterial flora and host immune response
What are the 5 Rationales for Subgingival instrumentation.
Completely remove biofilm/calculus deposits
Induce positive changes in the bacterial flora
Create environment that permits tissue healing
Increase effectiveness of patient self-care
Prevent recurrence of disease during periodontal maintenance
What are non-responsive disease sites?
Non-responsive disease sites are periodontal areas that do not improve after initial therapy (e.g. scaling). → recheck is 4-6 weeks after debridement completed
Signs:
Redness
Inflammation
Continued bleeding on probing
Deep pockets remain
Attachment loss persists or worsens
May indicate:
Residual calculus
Poor oral hygiene → patient self-care has not improved
Systemic factors (e.g. diabetes)
Need for surgical intervention
How does a clinician ensure they are able to locate and remove subgingival calculus since we cannot see it clinically?
Develop a systematic pattern for subgingival calculus removal
Stroke width of 1-2mm on most root surfaces, 60-80 degree angulation
Utilize multidirectional strokes to completely scale the root surface
Work on one tooth at a time. All deposits to be removed from one tooth before starting a second tooth.
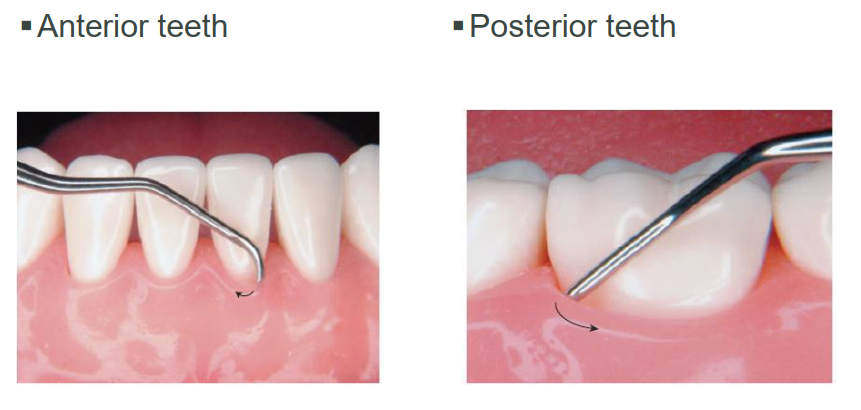
Why is a universal curet called universal?
It can be used on BOTH anterior and posterior teeth AND used to remove BOTH supragingival and subgingival calculus deposits
What are the unique characteristics of the Universal Curet?
Used to remove SMALL to MEDIUM sized calclus
Rounded back, rounded toe
Two cutting edges per working end
Semi-circular cross section
Face us PERPENDICULAR to the lower shank, 2 cutting edges
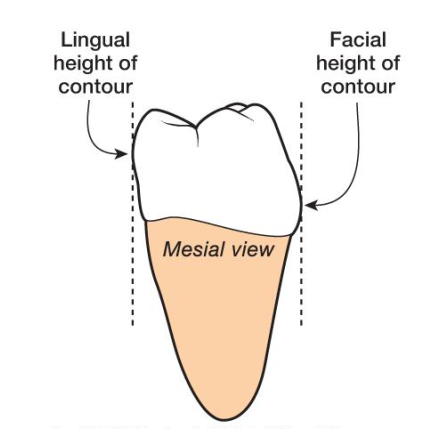
Curets with shorter lower shanks are limited to….Where do we use long lower shank curets?
use within NORMAL sulci or shallow pockets.
Longer lower shank curets are used on root surfaces and deep pockets.
What is the correct angulation for Universal curets working end?
70-80 deg towards tooth surface
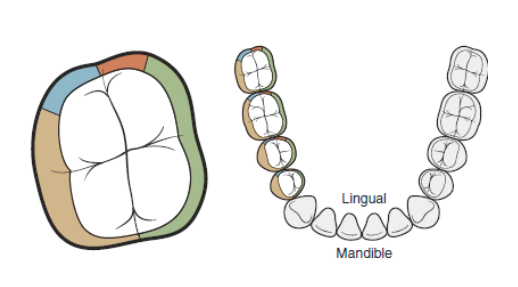
What are 2 reasons it may be challenging to adapt the working end to the FACIAL/LINGUAL root surfaces of the MANDIBULAR POSTERIOR TEETH?
Your hand may block your vision of the lingual surface
Rounded posterior crowns make it difficult to place the working end on the root surface
DO NOT tilt handle towards you, keep it upright
Which stroke is the most effective for removing calculus at line angles and midlines?
Horizontal stroke at LA of posterior and Midline of anterior
Which Gracey is used to instrument anterior teeth on all surfaces?
Gracey 1 / 2
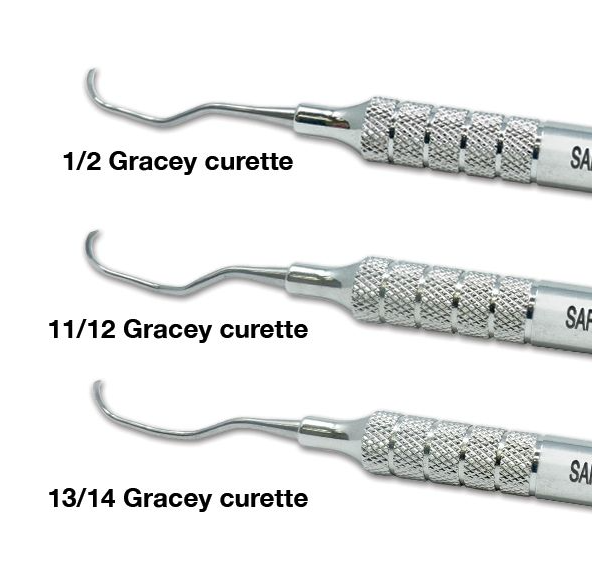
Which curette should you pick if you wanted to instrument the broad surfaces of posterior teeth?
Gracey 7/8

Which gracey curette would you pick to instrument posterior mesials? distals?
Mesial surfaces → 11/12 or 15/16
Distal surfaces → 13/14 or 17/18
Why might a 15/16 be preferred over 11/12 when instrumenting mesial surfaces? *same reasons for 17/18 and 13/14 distal surfaces
Modified shank and blade angulation allow better adaptation to posterior mesial/distal surfaces without excessive hand repositioning
Provides easier access to deep pockets and tight interproximal spaces
Can improve ergonomics by reducing the need for awkward wrist movements