Lecture 25 – Centrally acting anti-obesity agents
1/21
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
22 Terms
What are the BMI (kg/m²) classifications for adults as per NICE guidelines?
1st Class Note: BMI is not a perfect measure, as it can be high in individuals with large muscle mass who are not carrying excess fat.
Classification | BMI (kg/m 2 )* |
Healthy weight | 18.5–24.9 |
Overweight | 25–29.9 |
Obesity I | 30–34.9 |
Obesity II | 35–39.9 |
Obesity III | 40 or more |

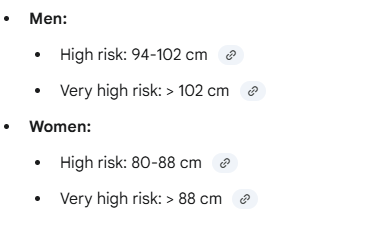
What waist circumference measurements indicate 'high risk' and 'very high risk' in men and women?
•Men 94-102 cm high risk; > 102 cm very high risk
•Women 80-88 cm high risk; > 88 cm very high risk
Describe the prevalence of overweight and obesity in English adults, highlighting the key age-related trend
Prevalence increases significantly with age.
16-24 age group, ~72% are of a healthy weight.
ages 45-74, almost three-quarters of people being overweight or obese.
Due to small, gradual energy imbalance over many years.
What is the "more concerning" trend regarding childhood obesity prevalence in England?
Obesity is already prevalent in children as they enter primary school.
4-5 year olds: 101/1000 are obese and 121/1000 are overweight.
10-11 year olds: 234/1000 are obese and 143/1000 are overweight.
1st Class Note: This is described as "storing up potential health care problems in the future".
What are the 4 levels of intervention for obesity, and what factors determine them?
Level 1: General advice on healthy weight and lifestyle.
Level 2: Diet and physical activity.
Level 3: Diet/activity + consider drugs.
Level 4: Diet/activity + consider drugs + consider surgery (e.g., bariatric surgery/gastric band).
How is obesity defined as a disorder of homeostatic control?
It's a disorder of energy balance.
Normally, energy intake = energy expenditure
keeping body weight stable.
Obesity occurs when excess energy is consumed (driven by an environment of cheap, energy-dense food) and/or expenditure declines (sedentary lifestyles) , leading to storage of excess energy as fat.
What is "adiposity negative feedback"?
Adipose tissue (fat) is not inert; it secretes the hormone leptin in proportion to body fat content.
Leptin circulates to the brain and acts on leptin receptors (LepRs).
Its function is to reduce food intake by enhancing the brain's response to short-term satiety signals.
What are the key short-term and long-term signals that regulate feeding and satiety?
Short-term (Satiety - terminate a meal):
Gut peptides: GLP-1 and CCK, released in response to food.
Nutrients: Glucose and free fatty acids in the blood.
Gut distension: Stretch signals sent to the brain via the vagus nerve.
Long-term (Adiposity):
Leptin: From adipose cells.
Insulin: From the pancreas.
Describe the anorexigenic (inhibitory) pathway in the hypothalamic arcuate nucleus (ARC).
This pathway inhibits feeding behaviour (anorexigenic).
It involves POMC neurons.
Leptin stimulates these POMC neurons.
POMC is cleaved to produce α-MSH (α-melanocyte stimulating hormone).
α-MSH acts on MC4 receptors (MC4R) in the PVN (paraventricular nucleus).
This activation (along with input from the NTS) leads to a decrease in food intake.
Describe the orexigenic (stimulatory) pathway in the hypothalamic arcuate nucleus (ARC).
This pathway stimulates feeding behaviour (orexigenic).
It involves AGRP (Agouti-related protein) and NPY (Neuropeptide Y) neurons.
These neurons inhibit the anorexigenic (POMC/PVN) pathway.
Leptin inhibits these AGRP/NPY neurons.
Result: When leptin is high, this pathway is suppressed, allowing the anorexigenic pathway to dominate and decrease feeding.
What is the significance of the Ob/Ob mouse in obesity research?
The Ob/Ob mouse has a rare spontaneous mutation and is a model for type 2 diabetes (overweight, insulin-resistant, high blood sugar).
1st Class Note: In the 1990s, the mutated gene (Ob) was identified as the gene responsible for producing leptin. These mice lack leptin and therefore have no adiposity negative feedback, leading to excessive eating. While revolutionary, this mutation is extremely rare in humans.
What is the role of serotonin (5-HT) in feeding behaviour?
5-HT plays a key role in satiety.
Increasing synaptic 5-HT (e.g., with precursors like tryptophan) decreases food intake.
Destroying 5-HT neurons (lesioning the dorsal raphe) induces hyperphagia (overeating).
Key Receptor: The satiety effects are mediated by multiple receptors, but especially the 5-HT2C receptor in the ARC. HYPOTHALAMIC ARCUATE NUCLEUS (ARC)
What is the mechanism of Orlistat (Xenical/Alli)? What are its key features and side effects?
Mechanism: It is NOT centrally acting. It is a triacylglycerol lipase inhibitor that works in the gut to prevent the breakdown of dietary fats.
Features: It decreases the absorption of ~30% of dietary fat. It is available over-the-counter and is considered very safe as it is not absorbed.
Side Effects: Gastrointestinal issues, notably "oily stools" or faecal incontinence, especially if a high-fat diet is maintained.
What is the mechanism of Semaglutide (Wegovy) and Liraglutide (Saxenda)?
They are GLP-1 receptor agonists.
They are analogues of the natural incretin hormone GLP-1 (glucagon-like peptide-1). binds to glp-1
Originally antidiabetic drugs, they also act on the hypothalamic satiety circuitry to reduce food intake.
1st Class Note: different mechanism from failed centrally-acting agents and (so far) lack significant psychiatric side effects.
What is the mechanism of Setmelanotide (Imcivree) and for whom is it approved?
Mechanism: It is an MC4R agonist. It mimics α-MSH to activate the MC4 receptors in the PVN, stimulating the brain's primary anorexigenic (feeding inhibition) pathway.
Approval: It is only approved for children (>6yrs) with rare genetic disorders of obesity, such as POMC deficiency or LEPR (leptin receptor) deficiency .
What was "Fen-Phen" and why was it withdrawn?
What: A combination of Fenfluramine (a 5-HT releasing agent/reuptake inhibitor) and Phentermine.
Withdrawal: Withdrawn in 1997 due to serious side effects, including heart valve problems and pulmonary hypertension.
1st Class Note: The drug company (Wyeth) paid >$7 billion in lawsuits. This failure was later linked to Fenfluramine's action on 5-HT2B receptors (cardiac) rather than the intended 5-HT2C receptors (satiety).
What is the mechanism of Phentermine/Topiramate (FDA approved)? How does it differ from "Fen-Phen"?
A fixed-dose combination:
Phentermine: A sympathomimetic amine that acts as a non-selective releasing agent of NA, 5HT, and DA to suppress appetite.
Topiramate: An anticonvulsant. Its weight-loss mechanism is unknown but may involve mitochondrial effects. The dose used is much lower than for epilepsy.
This combination is more effective and better tolerated than either drug alone. It does not contain fenfluramine.
What is the mechanism of Naltrexone/Bupropion (Contrave) (FDA approved)?
A fixed-dose combination that acts on the brain's reward pathway:
Bupropion: A NA and DA reuptake inhibitor. This boosts dopamine, increasing the reward value of eating.
Naltrexone: An opioid receptor antagonist. This is thought to block negative feedback on the reward system, sustaining the effect.
1st Class Note: It is considered safer than phentermine-based drugs as it doesn't have the same noradrenergic cardiovascular risk.
Why was Lorcaserin (a "designer" 5-HT drug) withdrawn?
Mechanism: It was a highly selective 5-HT2C receptor agonist.
Rationale: It was designed to selectively target the 5-HT2C (satiety) receptor while avoiding the 5-HT2B (cardiac/heart valve) receptor responsible for the "Fen-Phen" disaster. It worked by stimulating POMC neurons.
Withdrawal: Withdrawn in 2020 due to a (slight) increased occurrence of cancer.
Why was Sibutramine withdrawn? (Distinguish its mechanism from Fenfluramine)
Mechanism: A NA and 5-HT reuptake inhibitor.
Mechanism Distinction: It was NOT a releasing agent like fenfluramine/phentermine, which was thought to make it safer. It worked by increasing anorexigenic (POMC) and decreasing orexigenic (NPY) signals in the ARC.
Withdrawal: Withdrawn in 2010 due to significant cardiovascular risks (e.g., increased heart rate and blood pressure).
Why was Rimonabant withdrawn?
Mechanism: A cannabinoid CB1 receptor inverse agonist.
Rationale: Endocannabinoids are known to stimulate feeding behaviour (colloquially, "the munchies"). The idea was that blocking the CB1 receptor would reduce this drive.
Withdrawal: Withdrawn in 2009 due to severe psychiatric side effects, including a significantly increased risk of suicide.
What is the general conclusion regarding the efficacy and safety of most centrally-acting anti-obesity drugs?
The clinical benefit is often modest and not balanced by the risk of side effects.
Efficacy: Most drugs only produce a 5-10% body weight loss. Patients do not lose weight indefinitely; they reach a new, lower set point.
Safety: The side effects are often severe (cardiovascular or psychiatric), leading to most drugs being withdrawn. This is why there is only one centrally-acting agent licensed in the UK (Setmelanotide, for rare genetics)