4. Innate immunity I: The first lines of defense (barriers to infection)
1/22
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
23 Terms
What are the components of intrinsic innate immunity?
Humoral: complement system, cytokines/chemokines, antimicrobial peptides
Cellular: epithelial cells, neutrophils, eosinophils, monocytes/macrophages, dendritic cells (DCs), NK/NKT cells, γδ-T cells (Vδ1, Vδ2, Vδ3), innate lymphoid cells (ILC1, ILC2, ILC3)
Vδ1, Vδ2, Vδ3: Cutting edge of cancer immunotherapy
Microbial: bacteria (microbiota), viruses (virome)
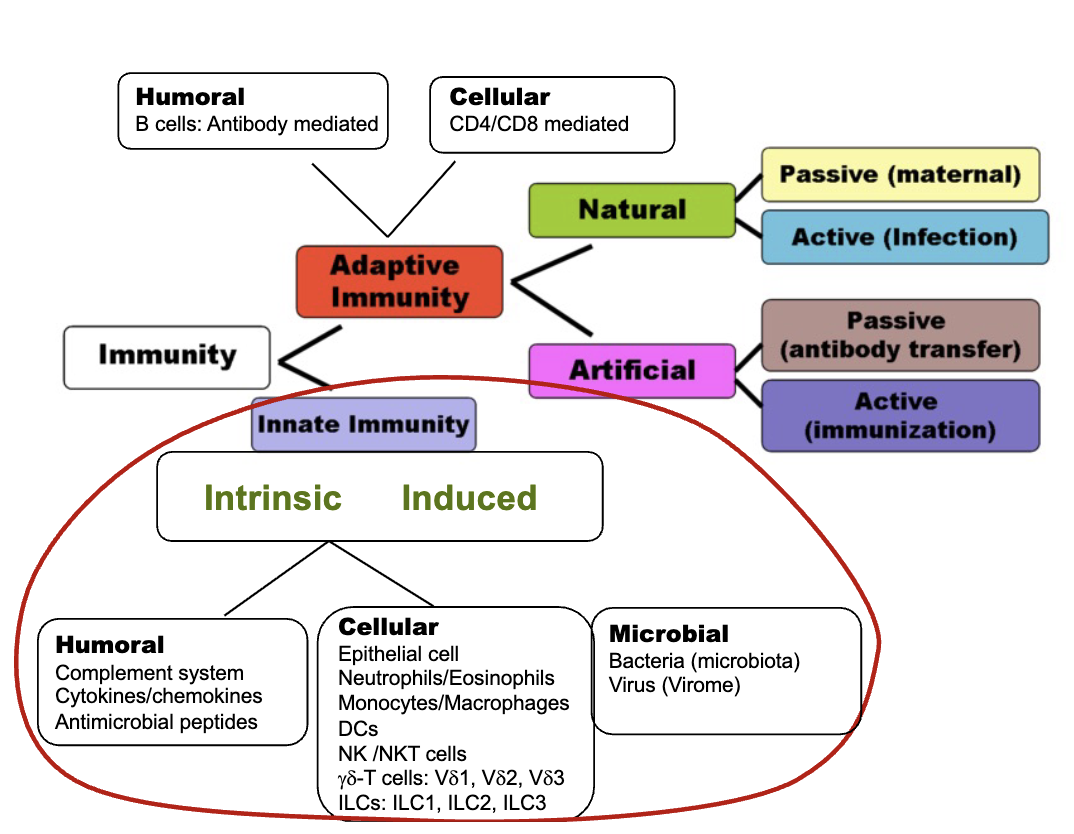
What are the properties of innate immunity?
Specificity: non-specific
Action time: quick
Persistence: short
Memory: none
Antigen: diverse (conserved, microbe-specific molecules etc)
Receptor: germ-line encoded
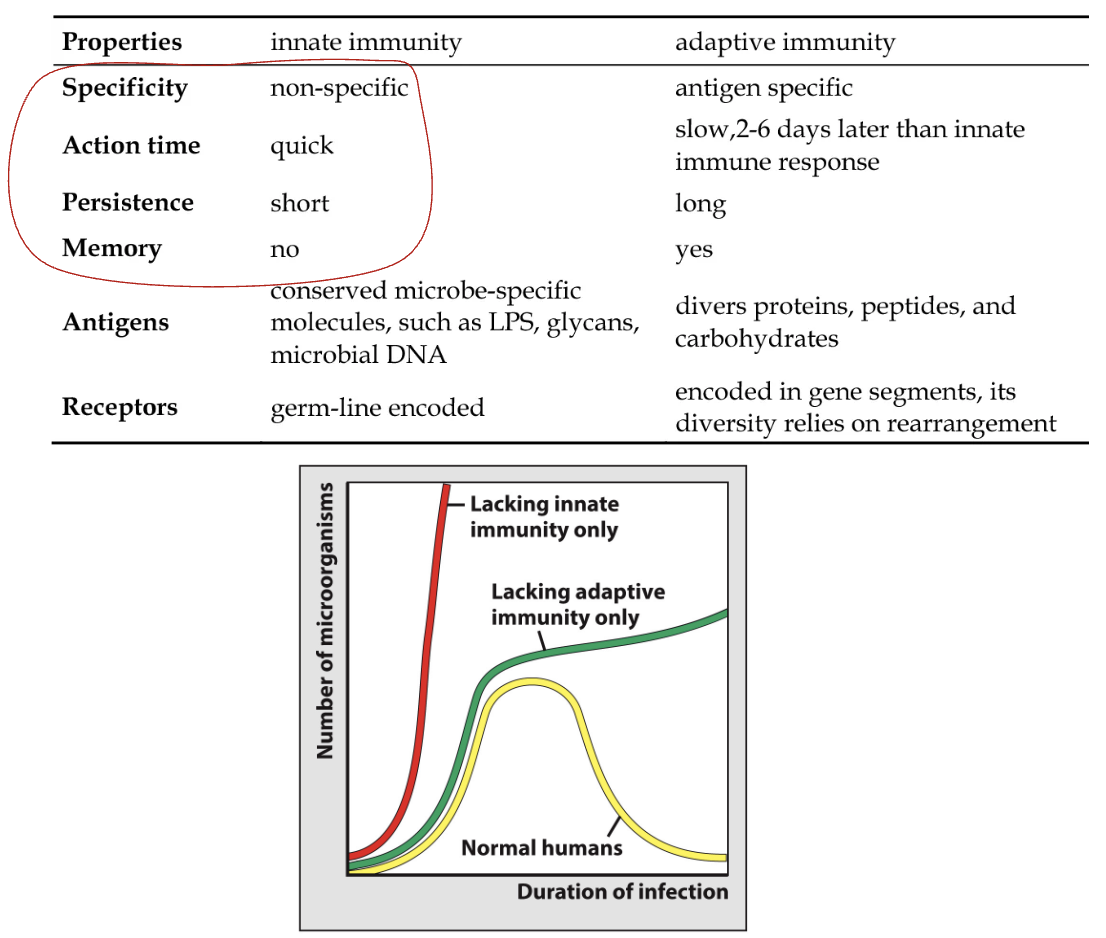
Graph takeaway:
Normal humans: infection controlled at low level
No adaptive immunity: higher infection load than normal
No innate immunity: even higher infection load → innate is essential first
What are the key functions of the innate immune system?
Prevent pathogen attachment/entry while allowing beneficial microbes
Recognize, control, eliminate danger
Induce inflammation, bring help to infection site
Orchestrate adaptive immune response
Regulate disease resistance and tolerance
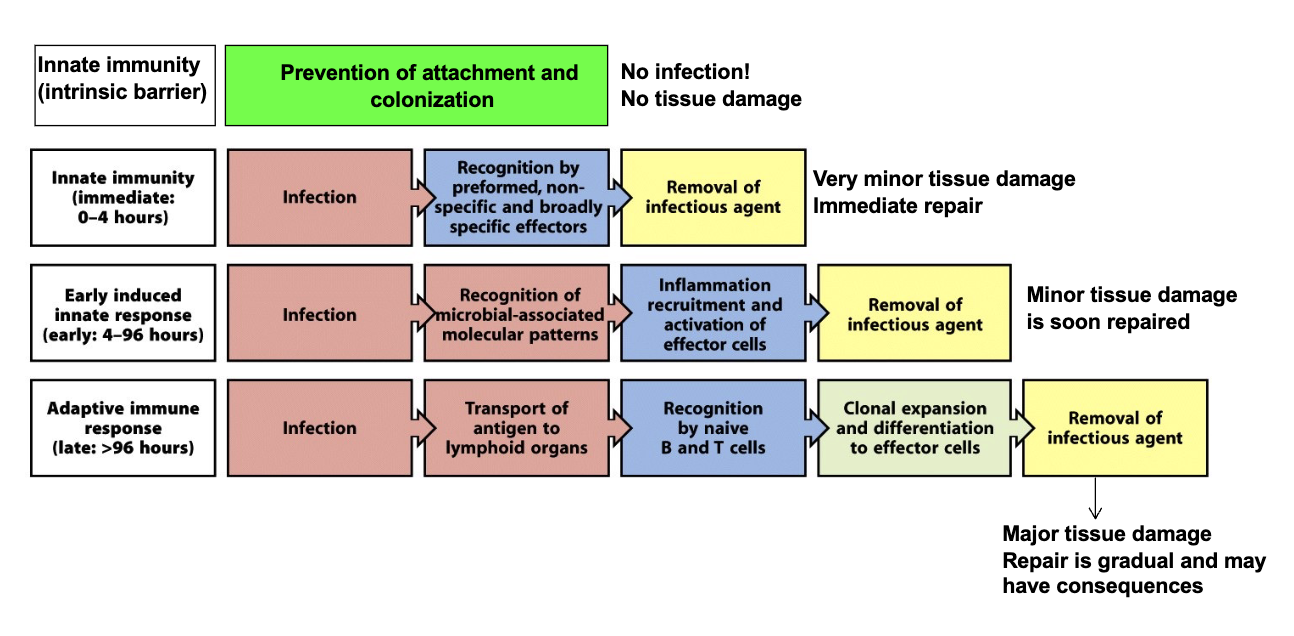
How does the body respond to potential pathogens?
Innate Immunity: No infection → No tissue damage
Innate Immunity (immediate: 0-4 hours): Very minor tissue damage → Immediate repair
Early induced innate response (early: 4-96 hours): Minor damage → Soon repaired
Adaptive immune response (late: >96 hours): Major damage → Gradual repair, may leave consequences
Important to have both innate and adaptive immunity
What is the role of intrinsic barriers in innate immunity?
Prevent pathogen attachment and colonization
Result: No infection, no tissue damage
Types of intrinsic barriers: Mechanical, Chemical, Microbiological
Chemical: Sebaceous glands (fatty acids) in skin, low pH in stomach, skin and vaginal tissue
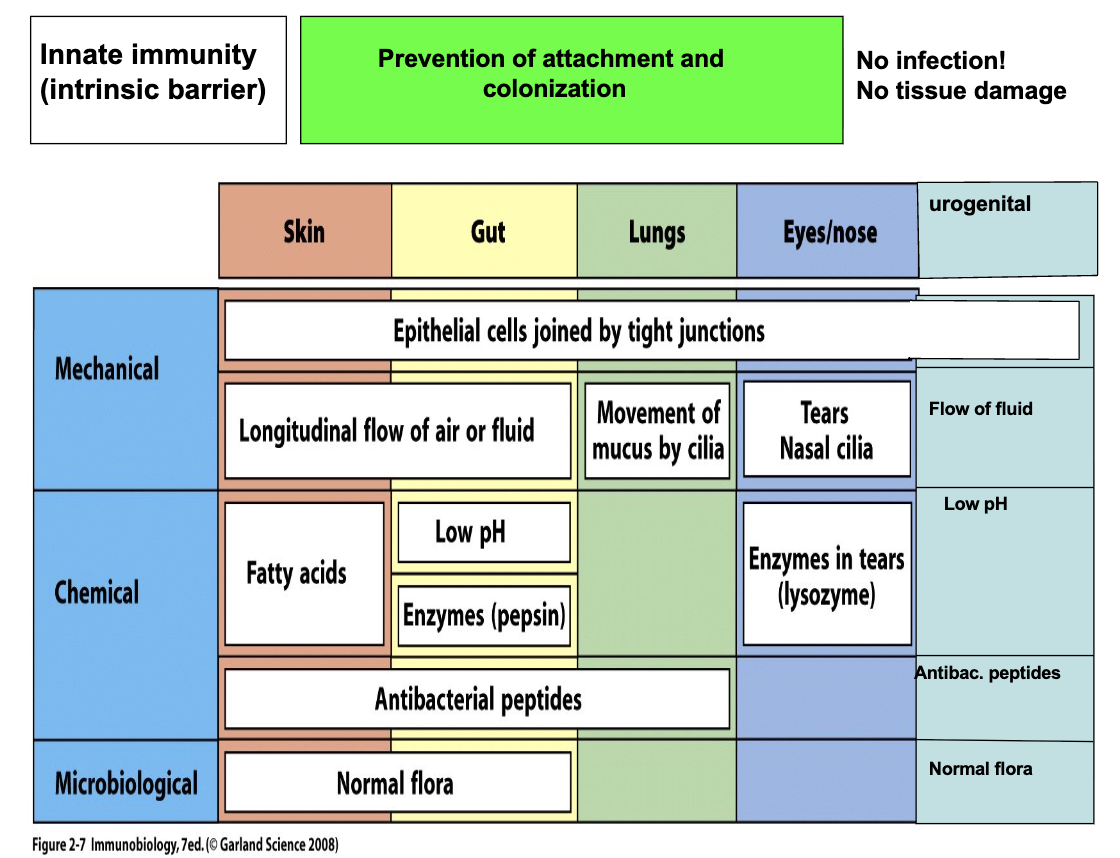
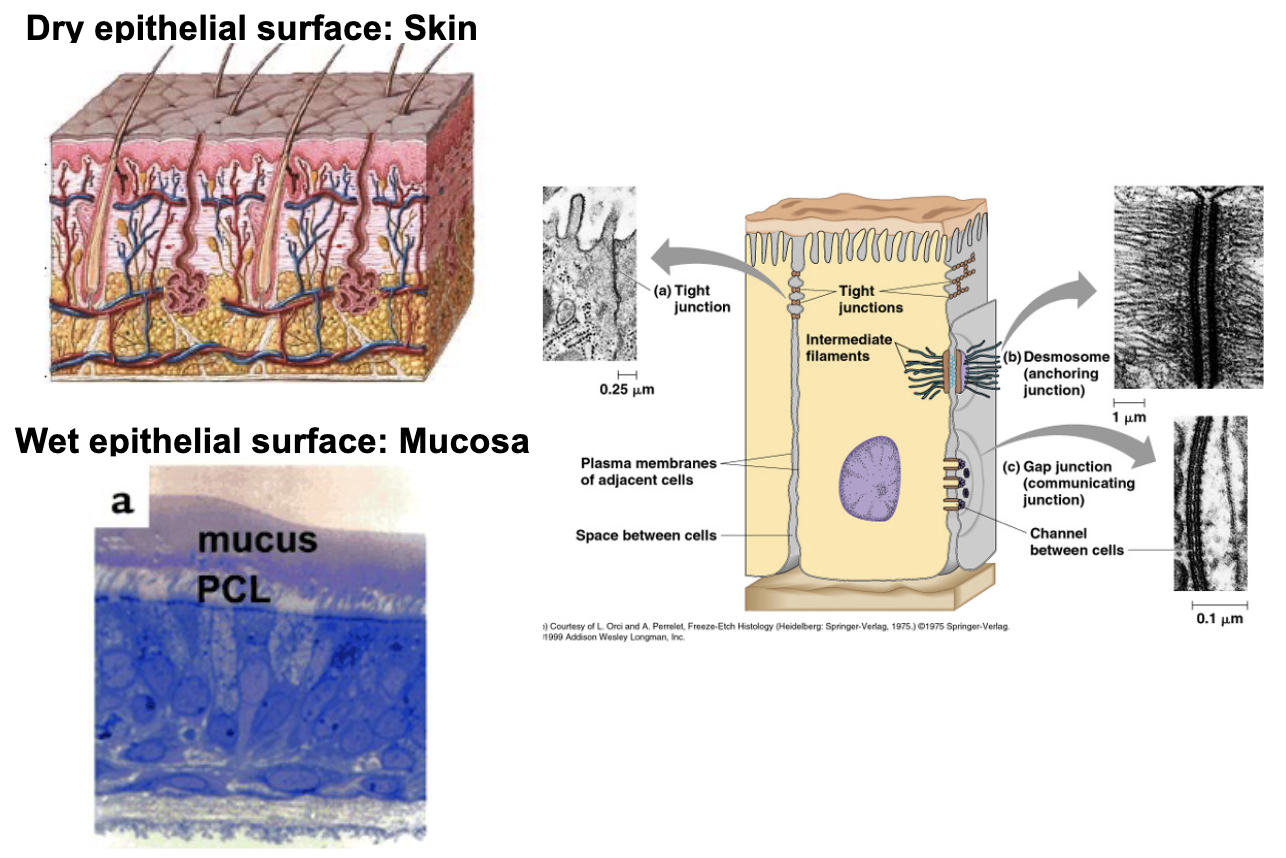
What epithelial surfaces provide the first line of defense?
Dry surfaces: skin
Wet surfaces: mucosa
Epithelial cells are immune cells
Why is skin important in immunity?
Skin is the largest immune organ
Makes up 12–15% of body weight
3 Important Factors for Healthy Skin
Thick cretinoid layer
Lots of microbiota at the top of skin
Thin emulsion (oil) layer
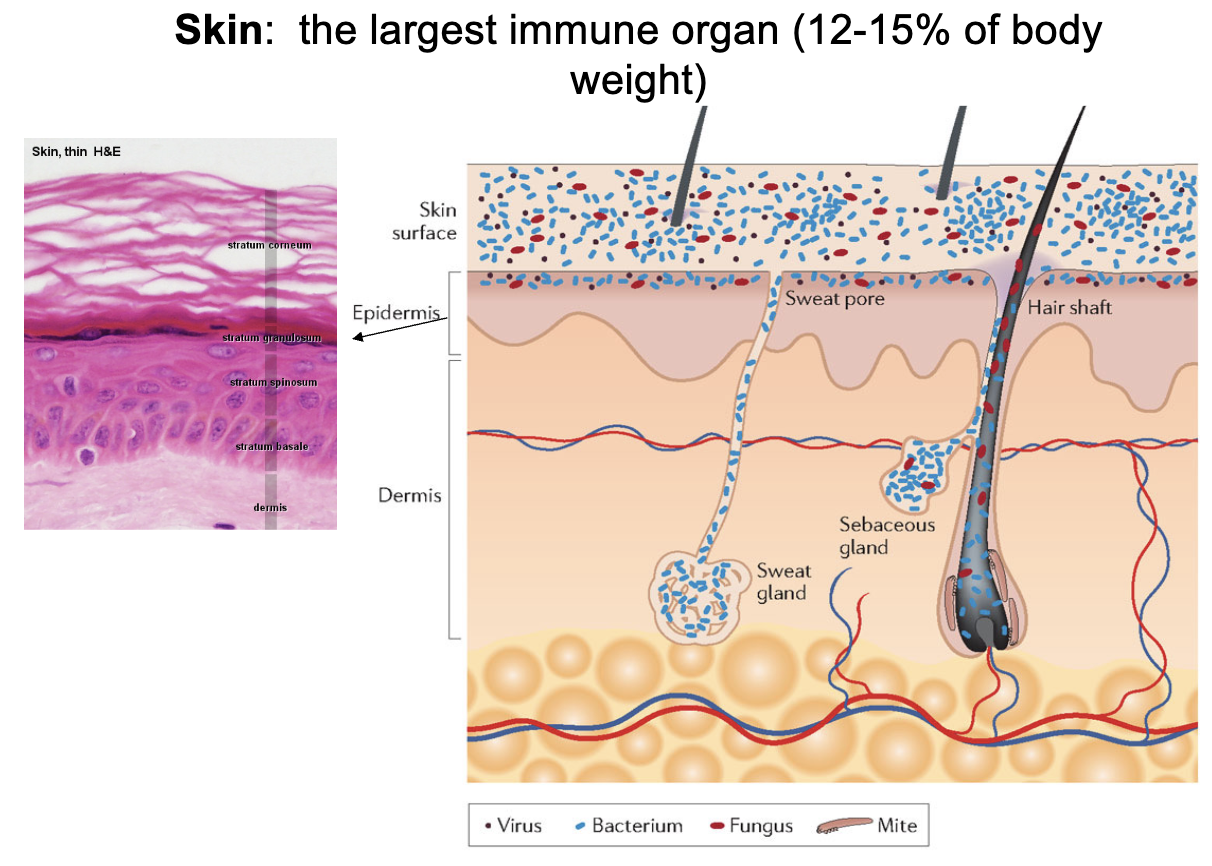
Why is healthy skin resistant to infection?
No viable virus receptors
Virus needs receptors → receptors are only on live cells → skin is dead cells → no virus receptors
Lowest water activity in body
High fatty acid + salt levels
Harbors ~200 bacterial genera
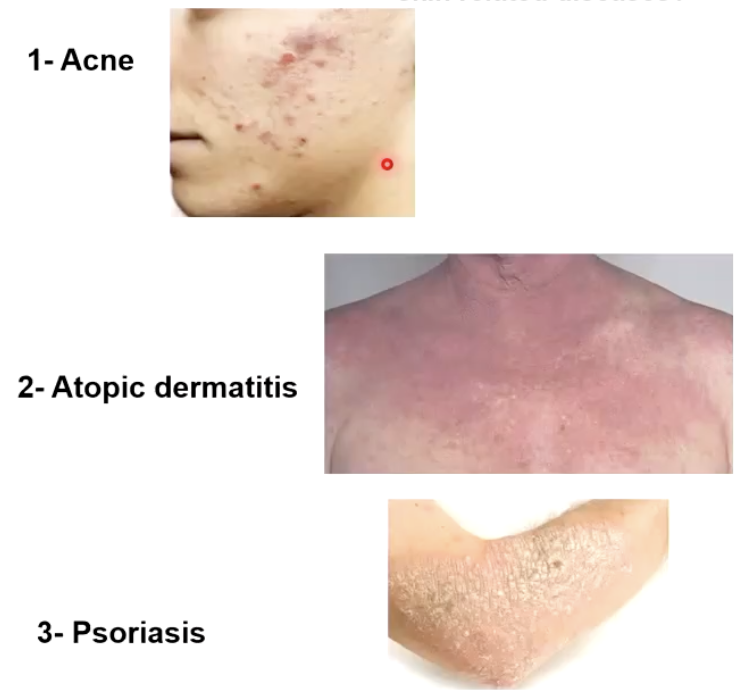
Can normal skin microbiota help treat skin diseases?
Potential treatments for:
Acne
Atopic dermatitis
Psoriasis
Example: Facial microbiota transplantation
What is another key epithelial barrier besides skin?
Mucosal surfaces
Covered with mucus + water, supporting microbiota growth
Contain mucin (traps microbes)
Rich in antibacterial + antimicrobial peptides
Have enzymes that break down pathogens
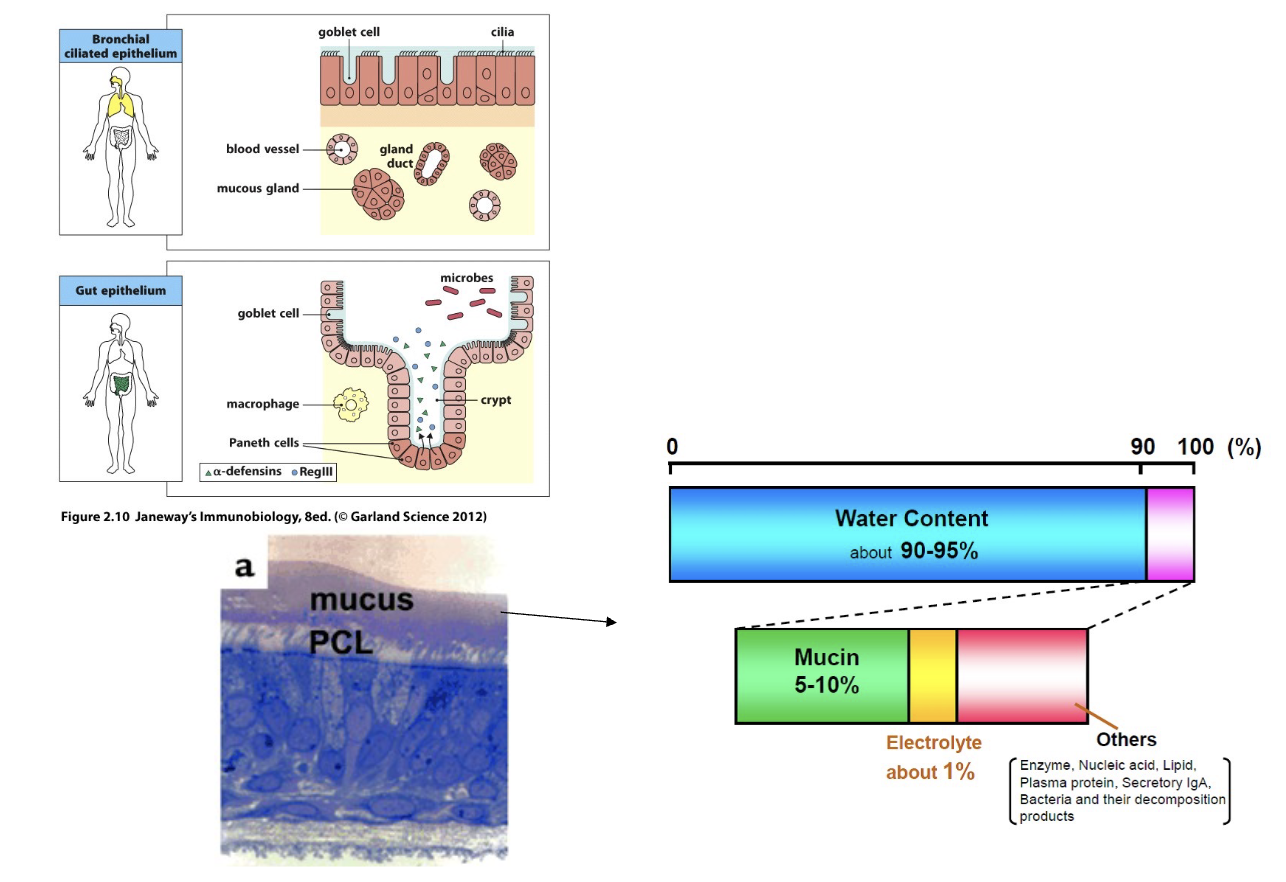
How does frequent renewal of mucosal epithelial cells aid defense?
Renew every 24–48 hrs
Rapid shedding removes attached pathogens
Constantly provides fresh, healthy barrier
How do microbiological barriers (normal bacterial and viral flora) prevent infection?
Microbiota: Important player of innate immunity and more
GI tract: ~400 bacterial species (~2.8 kg in gut mucosa!)
UG tract: high Lactobacillus concentration
Upper respiratory: Gram+ (Strep/Staph)
Normal Flora (Microbiota) Mechanisms:
Occupy all available space (block bad bugs)
Produce antibacterial/viral components (bacteriocins, defensins, cationic proteins) to directly kill bad bags

Could we survive without normal flora? (Lessons from germ-free animals)
Underdeveloped immune system
Highly susceptible to infection
Need ~30% more food than controls to get same nutrients/energy

How can first-line defenses treat GI diseases?
Examples:
Clostridium difficile (C. defficile): Causes diarrhea and colon inflammation
Treatment: Fecal Microbiota Transplant to transfer healthy gut bacteria from a donor to the patient
Inflammatory bowel disease (IBD)
Other gut-related conditions (obesity)
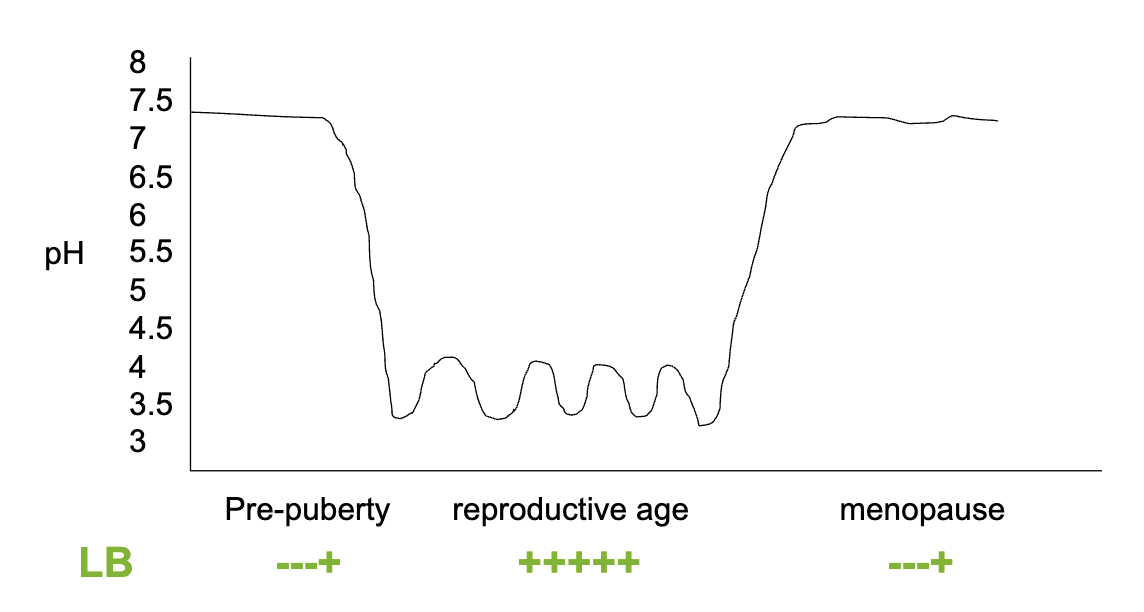
How does natural immunity vary in the female reproductive tract (pH + Lactobacillus)?
Pre-puberty: higher pH (less acidic), little/no LB
Reproductive age: lower pH (acidic), +++++ LB
Normal pH = below 3.5
LB peak at ovulation because that’s the only time animals mate (exception: humans)
Menopause: higher pH again, reduced LB
What dominates the vaginal microbiota in reproductive-age females?
Healthy: high LB (80%)
Sub-clinical BV: reduced LB
BV: very low/no LB
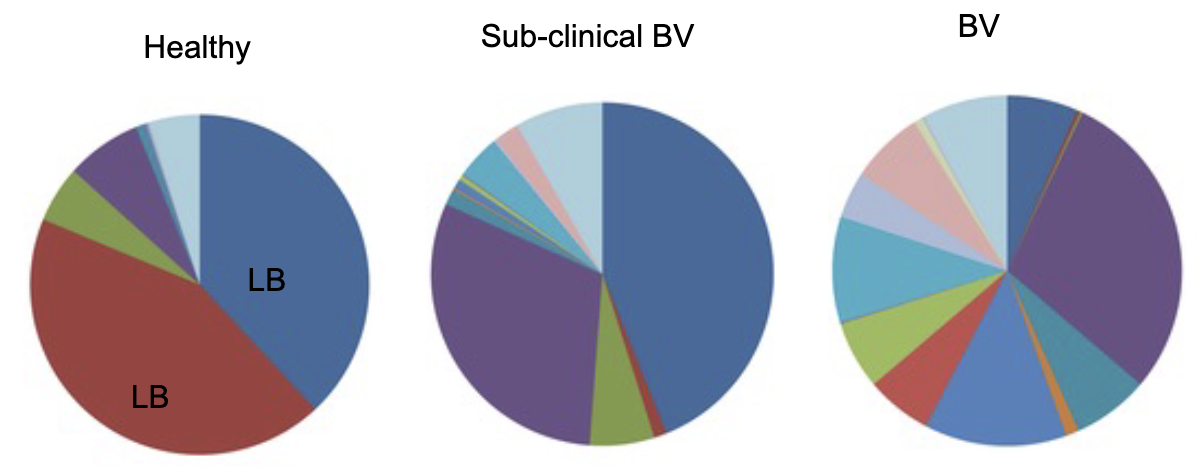
What trends are seen in BV (bacterial vaginosis) and STIs?
STI rate ↑ 2–5× among over-55s (2005–2015, still rising)
BV ↑ in adolescents + elders
Drug-resistant BV ↑
Best treatment/prevention? → Support healthy vaginal microbiota
Transplantation of vaginal microbes or lactobacilli
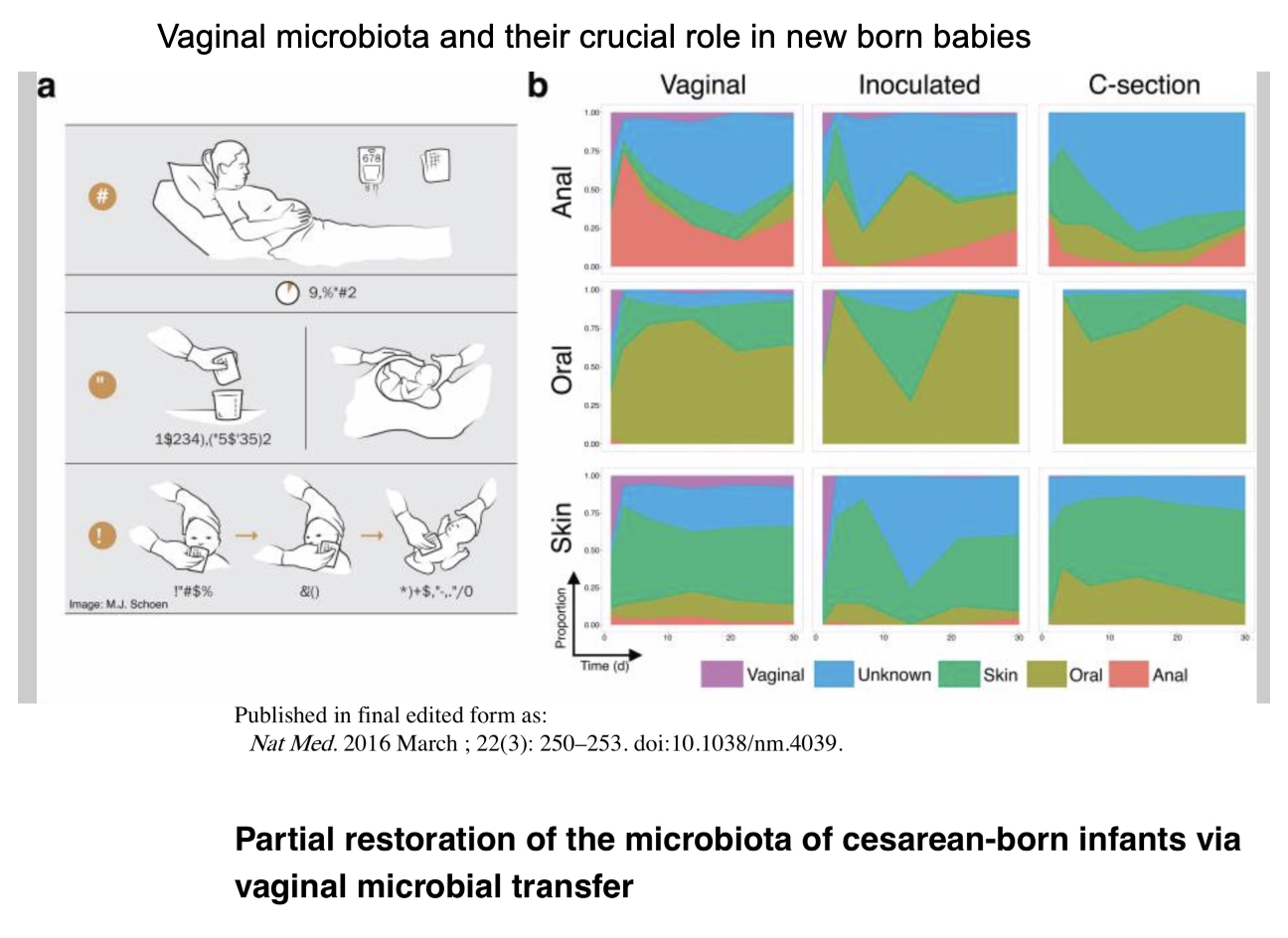
What role does vaginal microbiota play for newborns?
C-section babies lack full exposure to maternal microbiota
Vaginal microbial transfer → partially restores infant microbiota
Take clean cloth, absorb vaginal secretion and rub it on newborn
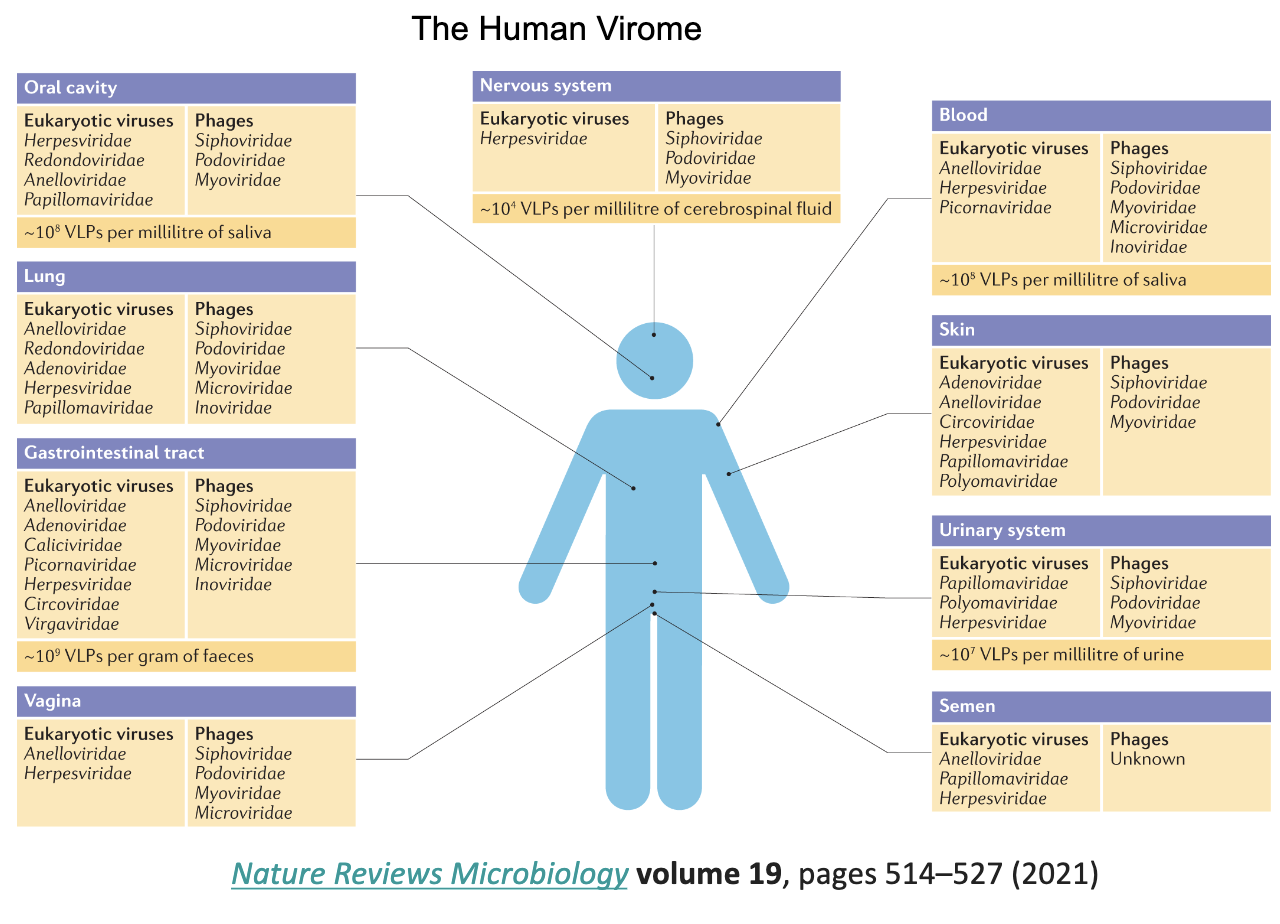
What is the human virome?
The collection of viruses that naturally exist in/on the human body
Part of innate microbial environment
In GI tract there is more viruses than bacteria!
GI tract has lots of phage virus
What antimicrobial substances do epithelial cells produce?
Cryptidins & α-defensins (produced at base of small intestine crypts)
β-defensins (produced within skin, respiratory tract)
Surfactant proteins A & D (present in lung, vaginal tract) → act as opsonins (enhance efficiency of phagocytosis)
How do tears and saliva defend against bacteria?
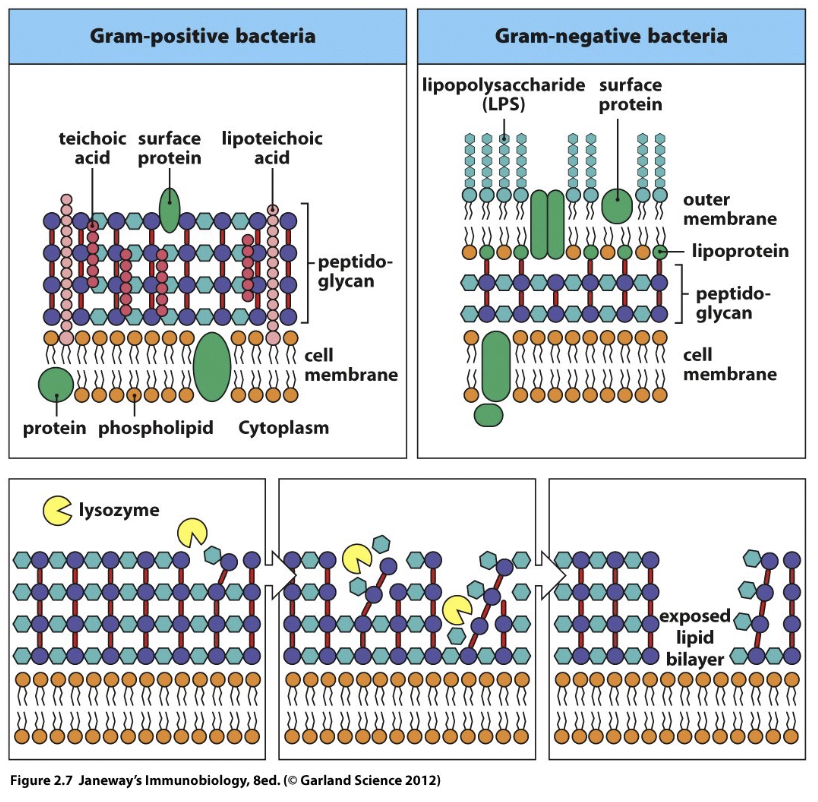
Contain lysozyme (natural disinfectant/potent antimicrobial agent)
Effective against Gram+ and Gram– bacteria
Composition of tears varies per condition: Foreign object in eye (high in lysosomes), sadness (cortisol)
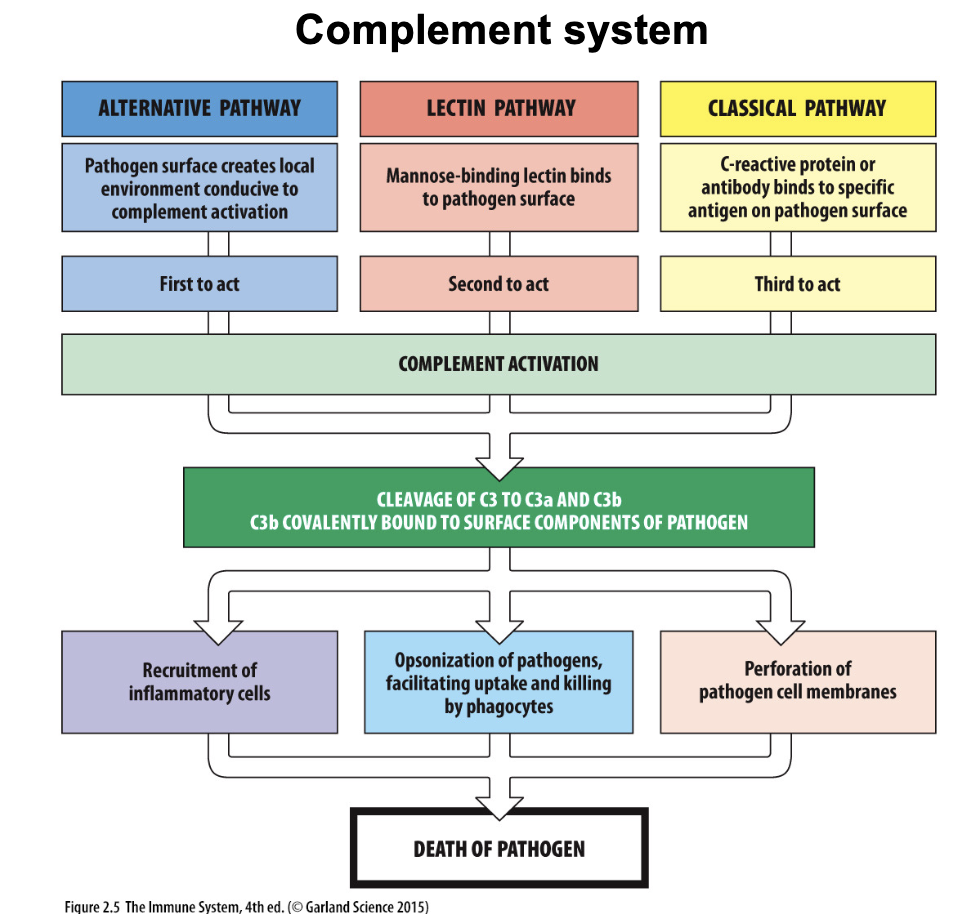
What are the complement pathways and their effects?
Main idea: Complement system are proteins normally produced in the liver, and increased production during injury → liver sends to blood so entire body soaked with complement protein
Part of humoral innate immunity
Once activated, 2 main jobs:
Remove pathogen
Induce inflammation
Alternative pathway: triggered by pathogen surface (first)
Lectin pathway: mannose-binding lectin binds pathogen (second)
Classical pathway: antibody or C-reactive protein binds antigen (third)
All → C3 cleavage → C3a, C3b
Results:
Recruit inflammatory cells
Opsonization → phagocytosis
Pathogen membrane perforation
Outcome: pathogen death
What are the take home messages about innate immunity?
Intrinsic barriers prevent infection
Epithelial cells = crucial defense
Normal flora (microbiota) of skin and mucosal surfaces = first-line defense
Strengthening natural immunity may treat/cure infectious diseases