11. Persistent (Chronic) Viral Infections: Retroviruses (HIV & HTLV) - Audia
1/26
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
27 Terms
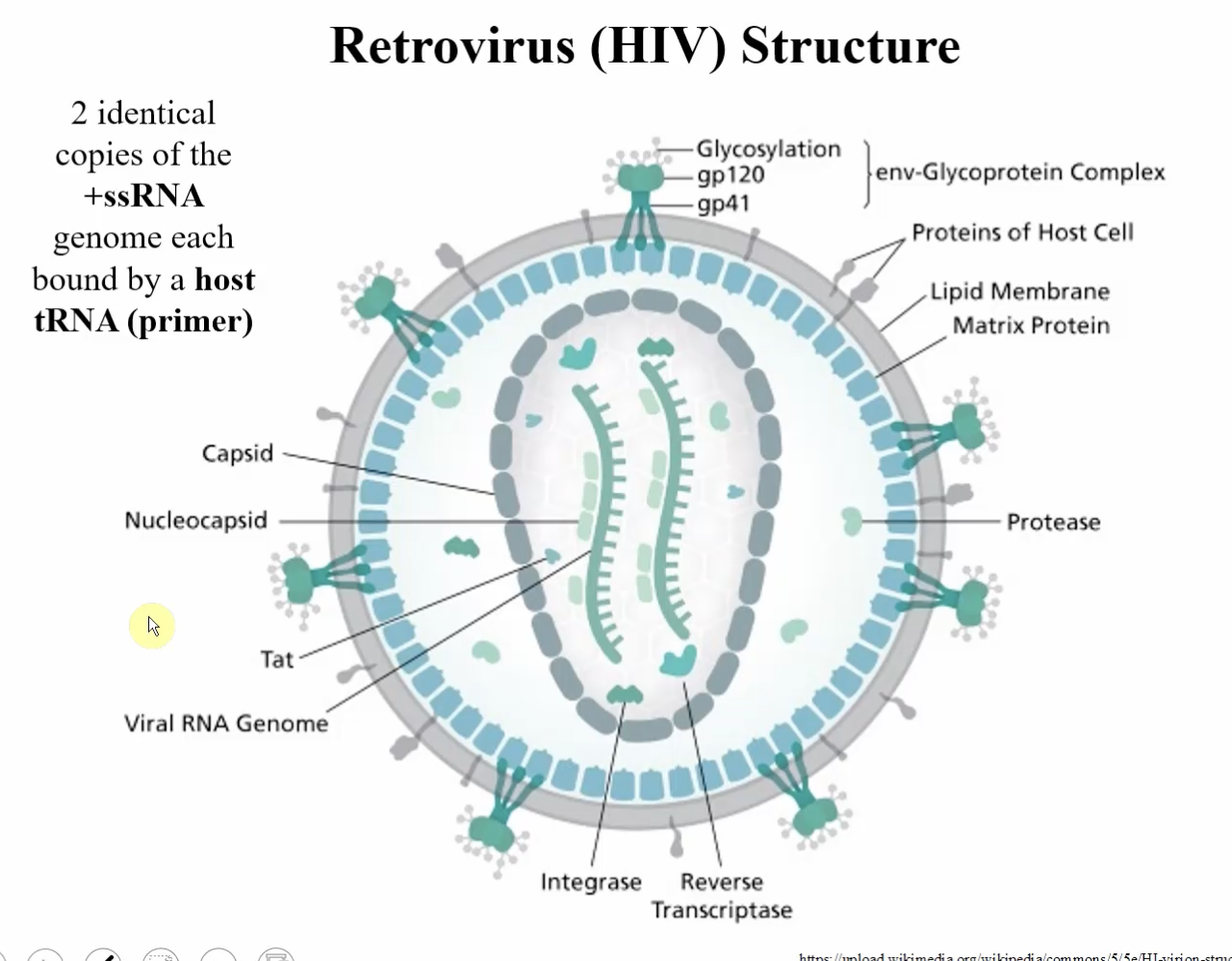
Retrovirus (HIV):
Structure
bound by what?
what other structures on the virus? (4)
2 identical copies of the +ssRNA genome
each bound by a host tRNA (primer)
VAPs: gp120, gp41
Integrase
Reverse Transcriptase
Protease
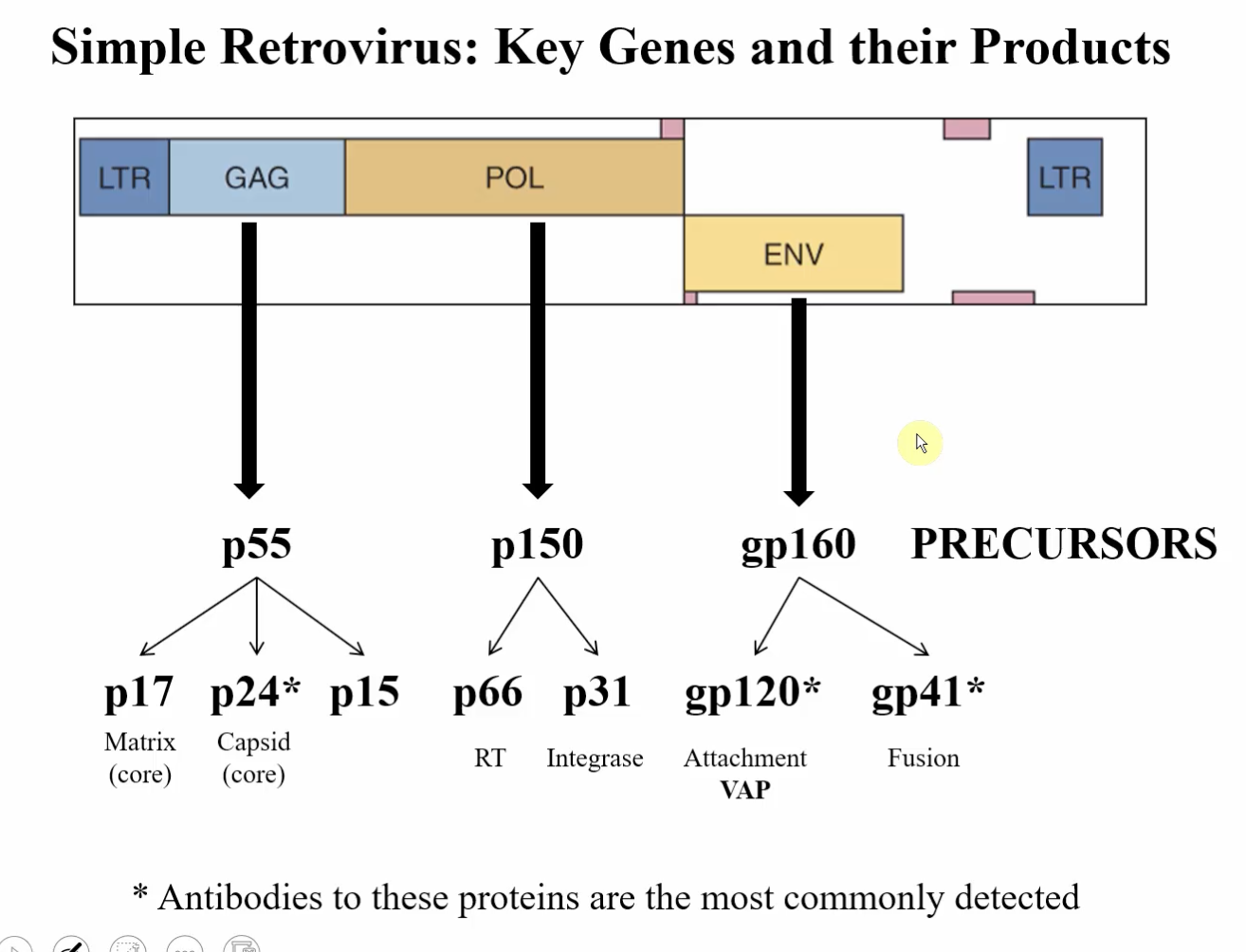
Retrovirus (HIV):
Which proteins encoded are most commonly detected? (3)
p24 (capsid - core)
gp120 (attachment VAP)
gp41 (fusion)
Retrovirus (HIV): Attachment, Fusion, Entry
____-restricted
what cells are targeted initially?
requirements of Retrovirus to recognize the cells (2)
Method of Penetration?
What cells are targeted later?
requirements of Retrovirus to recognize the cells? (2)
tropically-restricted since major receptor is CD4 cells
macrophages and dendritic cells are infected initially because they express CD4
retrovirus must recognize CD4 AND CCR5 by gp120
undergoes conformational change
Enters by Direct Fusion
T-cells are targeted later
retrovirus must recognize CD4 and CXCR4 by gp120
undergoes conformational change → direct fusion into cell
HIV Replication Steps (5)
Attachment, Fusion, Entry
Reverse Transcriptase → cDNA synthesis (complementary DNA)
makes a copy of the RNA in DNA form → degrades the RNA → makes a dsDNA molecule → DNA circularizes (LTRs on front and end merge) → integrates into host chromosome through integrase
Genome Integration → Transcription
viral proteins and new viral RNA genomes
Viral genome encapsidation
package RT, INT, PRT
reverse transcriptase
integrase
protease - cleaves the pro-proteins into their active forms
final step in maturation
Release via Budding
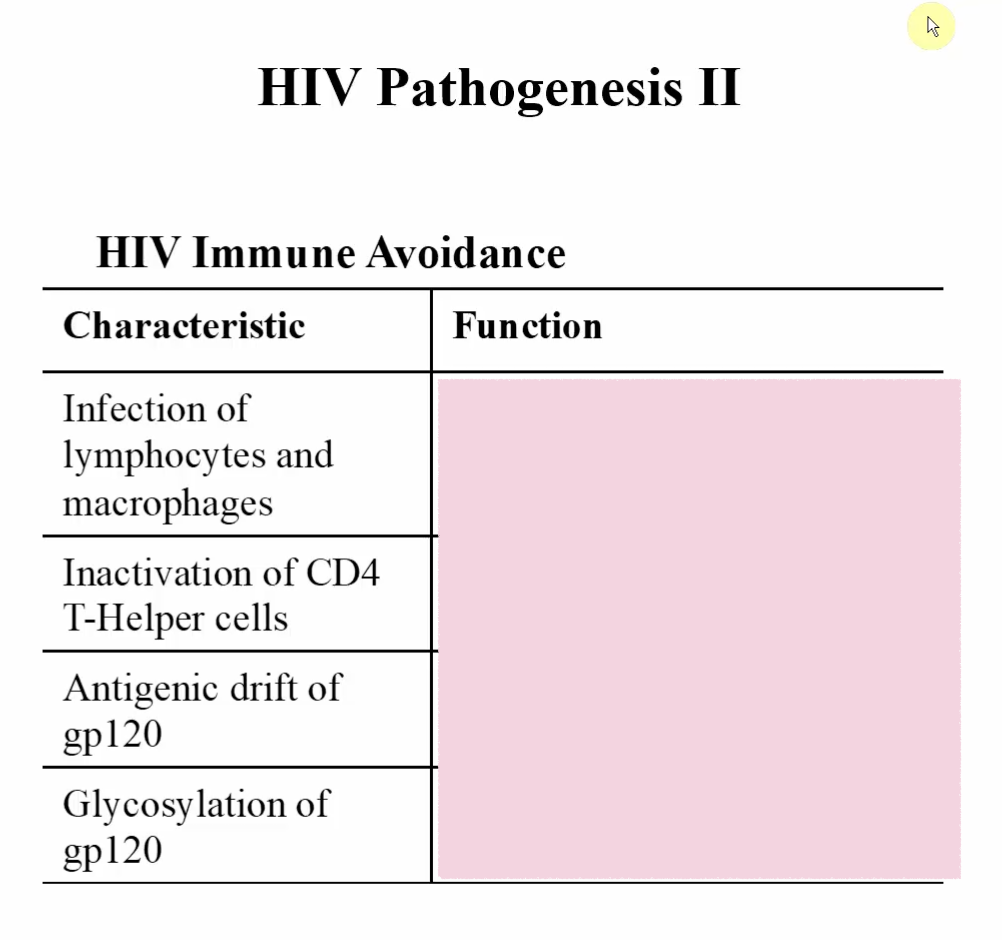
HIV Pathogenesis I
initial infection of what?
what leads to infection of T-cells?
virus infection can lead to formation of what?
what happens in a 10 year time period? (untreated)
Initial infection of Macrophages (R-5 variants, can also infect Dendritic Cells)
Antigenic drift leads to tropism change and infection of T-cells (X-4)
virus infection can lead to formation of syncytia (makes cell fragile and prone to lysis)
loss of TH function leads to decrease CD8 T cell function → AIDS
CD4 T cells help maintain viability of other cell types
Why is HIV so hard to treat?
always undergoes genetic drift!! so it constantly evolves and develops resistance to therapies.
HIV Disease Progression
Notable Timestamps (4)
1-3 weeks post-infection
3-6 weeks
10 years
beyond 10 years
HIV Disease Progression
Characteristics of each Timestamp (4, 2+2+3+0)
1-3 weeks post-infection
acute, flu-like symptoms
viremia
3-6 weeks
begin generating immune responses
begin slow decline in CD4
10 years
large decrease in CD4 cells
increase viral loads
disease progression
beyond 10 years
Treatment I
Classes (2)
Example of first class
What do they target?
Nucleoside Analogue Reverse Transcriptase Inhibitors (NRTI)
ex.) Azidothymidine (AZT) - Zidovudine/Retrovir
targets reverse transcriptase → can’t make cDNA → can’t integrate
alters the active site of the enzyme synthesizing viral DNA from RNA
Non-nucleoside Reverse Transcriptase Inhibitors (NNRTI)
targets reverse transcriptase
Treatment II
Classes (4)
What do they target?
Protease Inhibitors
prevents cleavage of pro-protein into RT-integrase → prevents infection
Binding and Fusion Inhibitors
Integrase Inhibitor
Highly Active Antiretroviral Therapy (HAART)
HIV Treatment
Treatment style
Combinatorial Therapy
give 3 different types of drugs
usually 2 nucleoside analogs + integrase inhibitor (example)
treats patient and prevents the emergence of resistance
HIV Clinical Syndromes (4)
Lymphodenopathy and fever → AIDS-Related Complex (ARC) with presence of 2 or more of:
fever
fatigue
diarrhea (persistent)
weight loss
night sweats
Opportunistic Malignancies → human herpes virus 8-associated Kaposi, sarcoma, non-Hodgkin lymphoma, EBV- related lymphomas
AIDs-related Dementia
Opportunistic Infections:
Protozoan
Fungal
Mycobacterial
Latent viral re-activation
Recurrent bacteremia
HIV Transmission (6)
Exposure to open wound, mucous membranes
Intravenous drug. use
Tattoo needles
Sexual transmission
Perinatal transmission
Breast milk
Can HIV be transmitted through casual contact? (kissing, handshake, close quarters, etc..)
NOOOOOO
Test for HIV infection is performed in order to do what? (4)
Identify infection to initiate therapy
Identify carriers to limit spread
Follow progression of disease
Evaluate treatment efficacy
HIV Laboratory Diagnosis
Methods (3)
examples of each (1, 2, 1)
Genomic-based Testing
detecting viral genome load in blood by PCR/RT-PCR
Serology
detection of antibodies to p24, gp41, gp120
ELISA, Western Blot, and Agglutination tests for antibody titres
Immunological Studies
assess CD4 and CD8 T cell levels
HIV structure characteristics (4)
enveloped
spherical
encloses a capsid
capsid contains 2 copies of +ssRNA
What is carried in the virion? (2)
reverse transcriptase (RNA-dependent DNA polymerase)
integrase enzyme
What is the initial determinant of tissue tropism?
How so?
Virus receptor
Requires CD4
Co-Rc can either be:
CCR5 (macrophages)
CXCR4 (T-cell)
What can undergo genetic drift to change Co-Rc specificity and antigenicity?
gp120
What does the provirus do? (2)
integrates randomly into host chromosome and becomes a cellular gene
Simple retroviruses encode what? (3)
Complexes viruses also encode what? (5)
Simple Retroviruses:
gag
pol
env
Complex Viruses:
tat
rev
nef
vif
vpu
What protein is associated with progression to “full-blown AIDS”?
nef protein
Final morphogenesis of HIV requires what?
protease cleavage of gag and gag-pol polypeptides after envelopment!!!
Stable or unstable virus?
Transmitted primarily how?
Environmentally, unstable virus
transmitted by bodily fluids