L19: Trauma I Thermal Injury
1/82
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
83 Terms
What is frostbite and when do we suspect it
- frostbite: the freezing of body tissues due to prolonged exposure to cold temperatures, leading to cellular injury
- when we suspect it: pts with exposure to ≤0℃ for several mins/hours with inadequate protection to extremities
- physical exam will present pain/tingling/loss of sensation in digits or extremities

What are the commonly affected areas in frostbite
- extremities: eg. fingers, toes, ears, nose, chin
- overall areas with weaker circulation (peripheral) as capillaries are more thin

What do freezing temperatures do to cutaneous flow compared to normal temp
- normal cutaneous flow: 200 mL/min
- skin temp at 15 degrees: 20 mL/min (flow drops x10)

What overall happens in frostbite
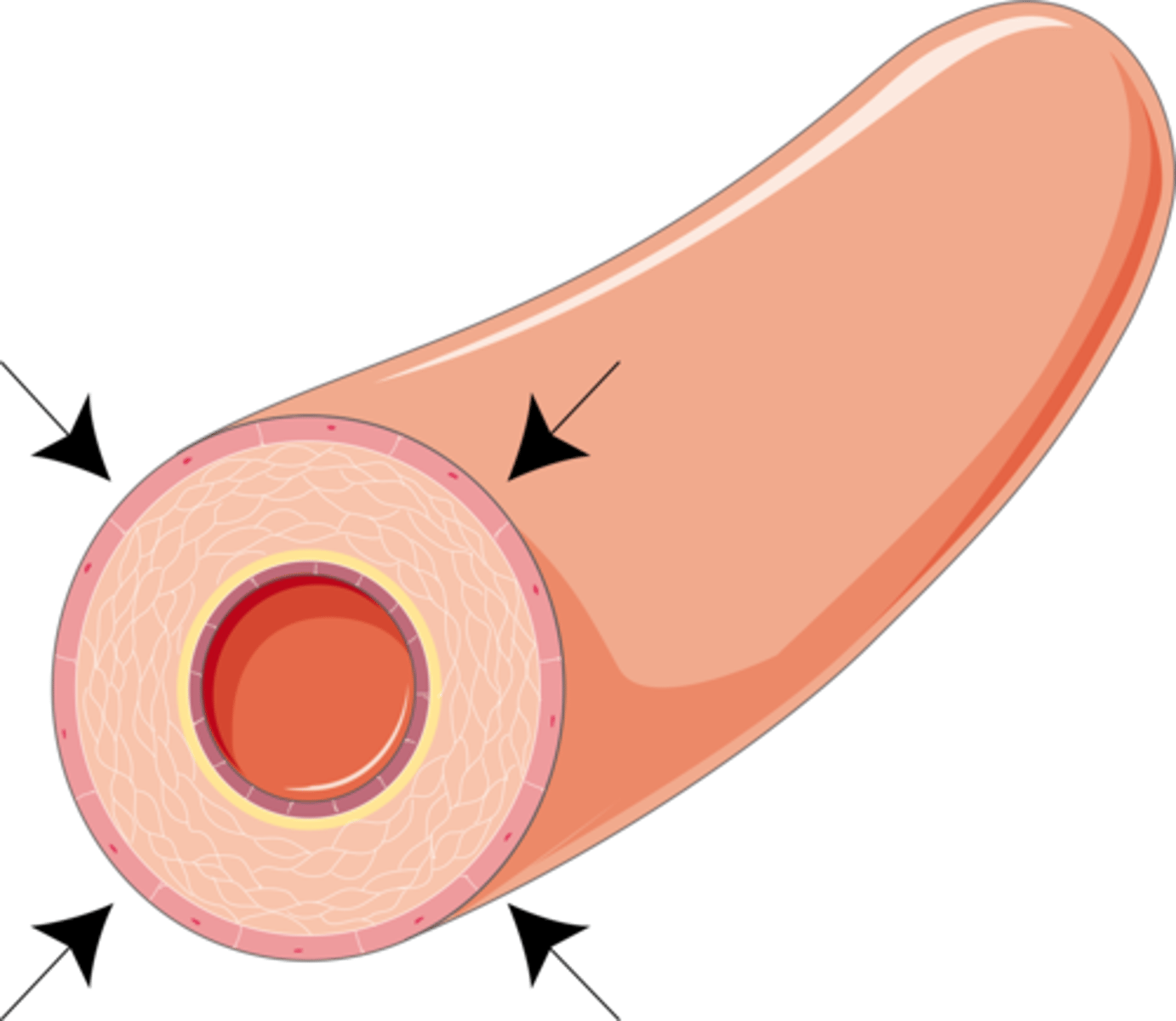
- vasoconstriction of vessels
- declining perfusion/temp
- inflammation

How does vasoconstriction occur in frostbite
- due to reflex action of blood vessels (aka Hunting reflex cause vasoconstriction, reducing blood flow to limit heat loss but after long exposure body may intermittently vasodilation & increase blood flow to prevent tissue damage)
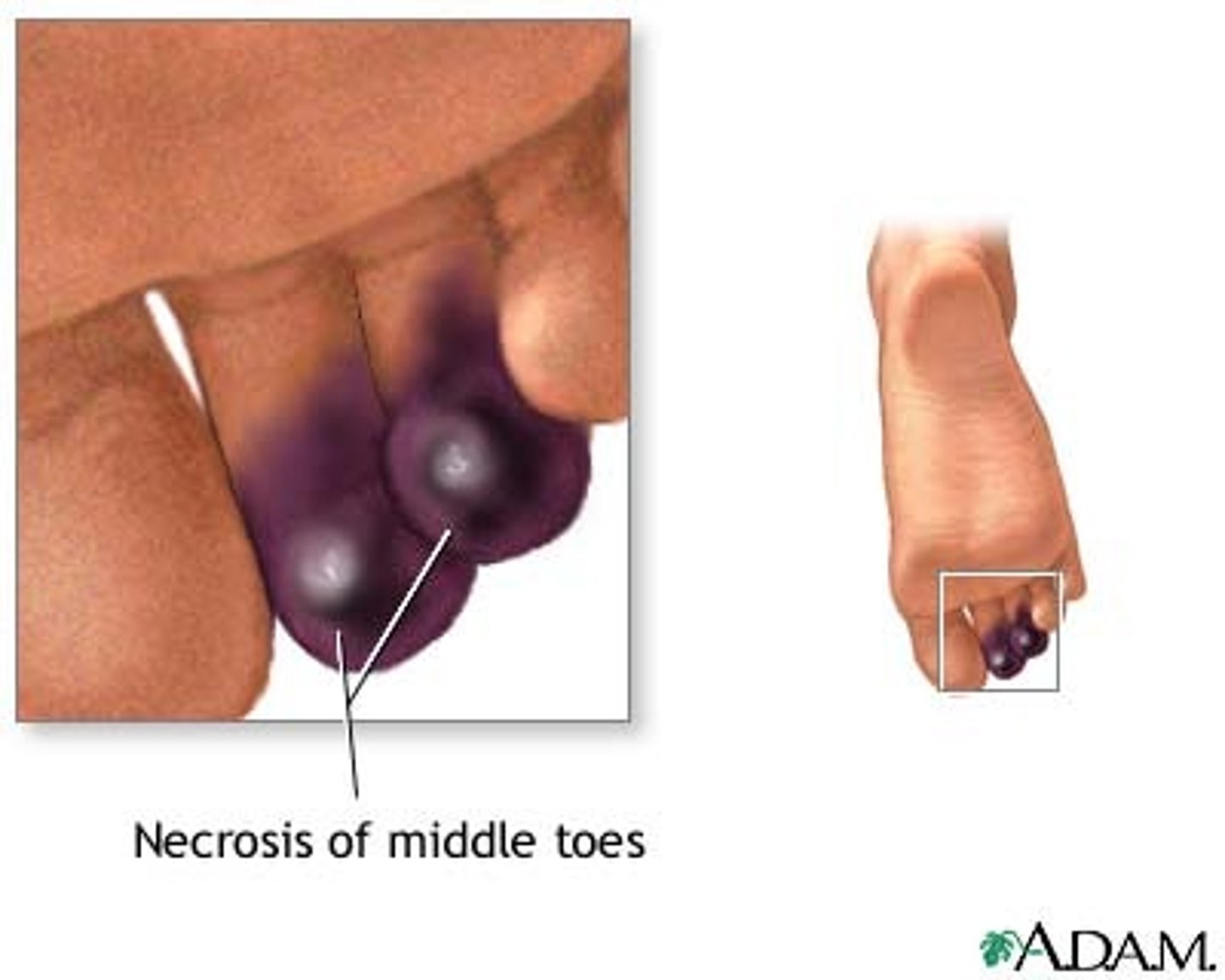
- result: decreased flow to nerves = numbness => tissue hypoxia, if prolonged => necrosis
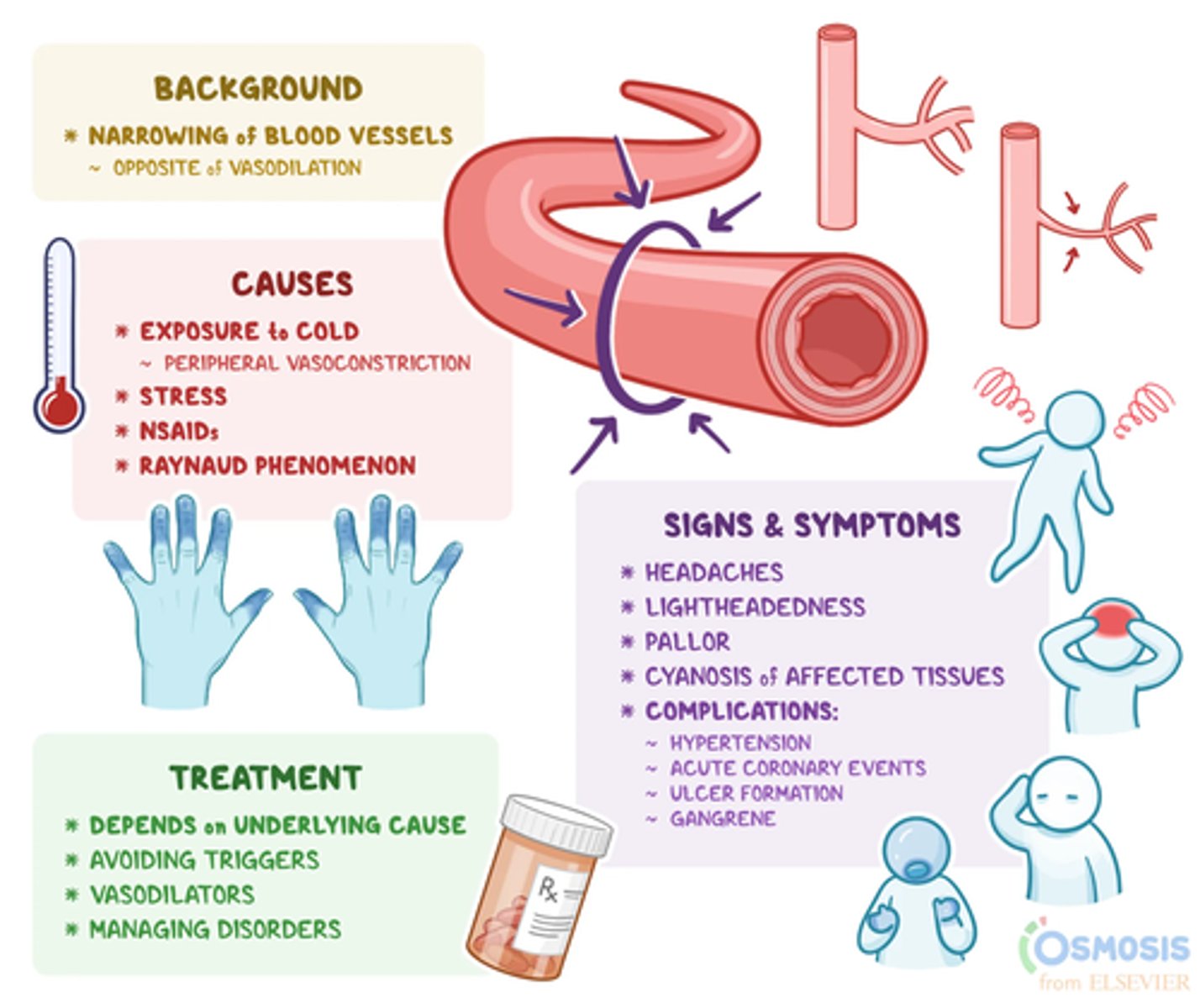
How does declining perfusion & temperature occur in frostbite
=> decreased blood flow (stasis) (due to vasoconstriction) => thrombosis (clots form in non-
flowing blood) => more tissue hypoxia
How does inflammation occur in frostbite
=> capillary permeability => fluid shift = edema + ROSs (Reactive Oxygen Species) release => tissue hypoxia => necrosis
What happens initially in frostbite at cellular level (aka extracellular freezing injury)
- exposure to cold temp => vasoconstriction => reducing blood flow to peripheral tissues (body prioritizes core temp maintenance) => tissue temp drops below 0°C
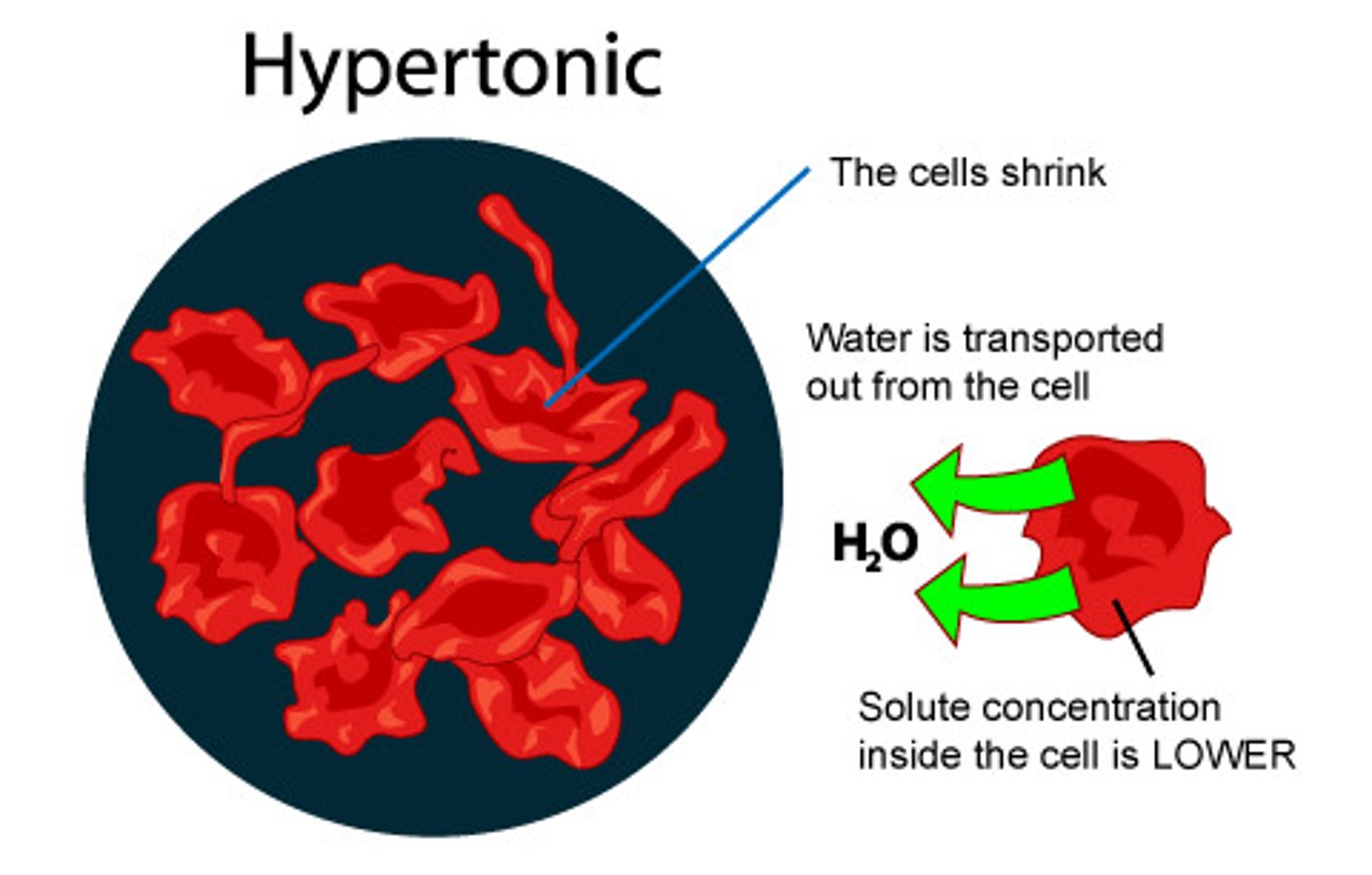
what happens in frostbite as tissue temp drops below 0°C (extracellular freezing injury)
extracellular fluid begins to freeze first because of its higher water content
=> formation of ice crystals in the extracellular space => hypertonic shift (draws water out of cells => edema)

what happens when ice crystals in tissues trigger edema in frostbite (extracellular freezing injury)
- result: cellular dehydration and shrinkage => mechanical and metabolic damage
- if the cold exposure persists: intracellular ice crystals form => direct cell membrane rupture and necrosis
What is reperfusion injury in frostbite
- delayed reperfusion, fast & hasty response leads to further damage (what follows after extracellular freezing injury)
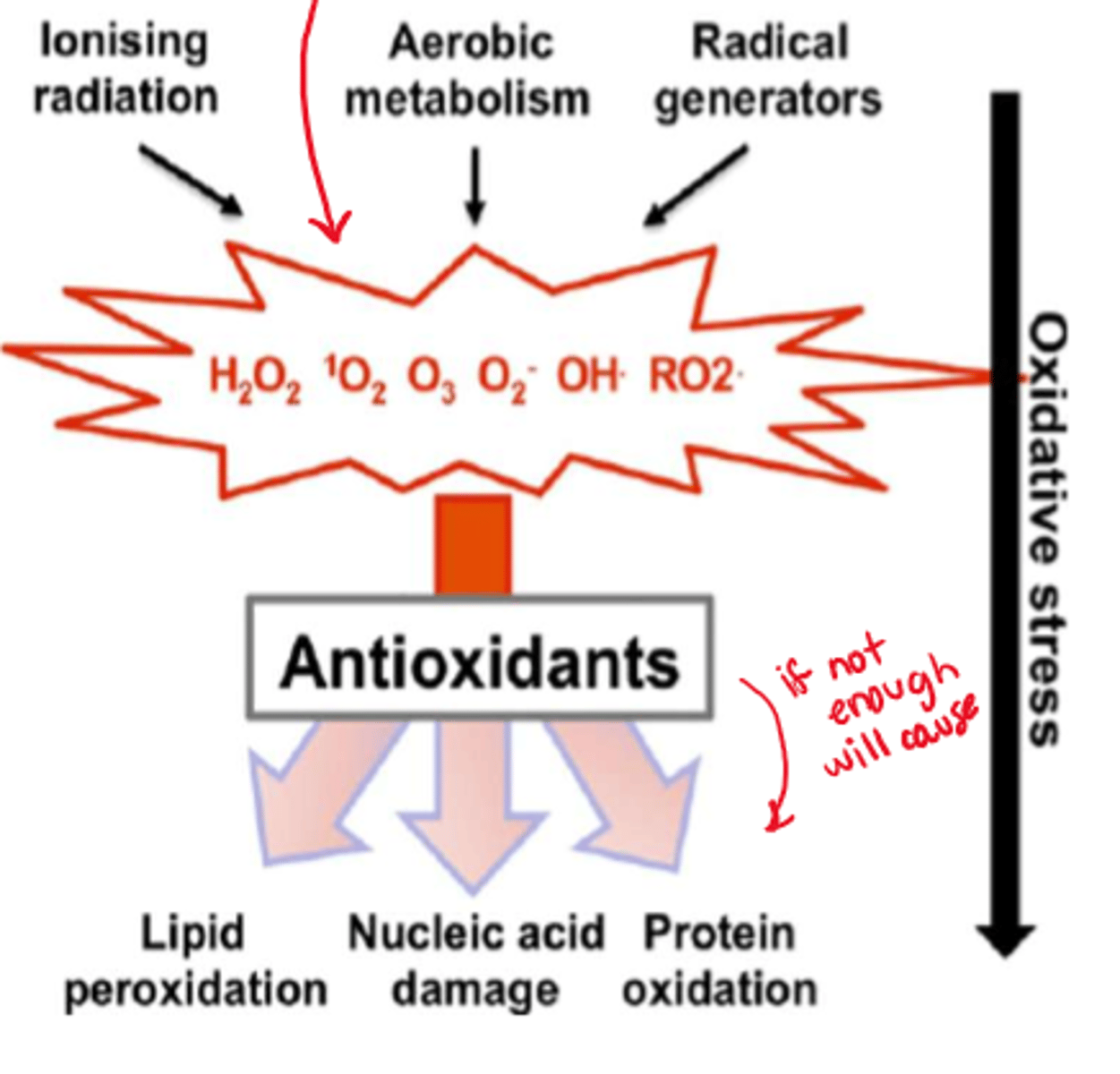
- affected tissues begin to rewarm, blood flow is restored, but this process can cause further damage as it triggers: vasoconstriction & microthrombosis, inflammatory responses, and oxidative stress

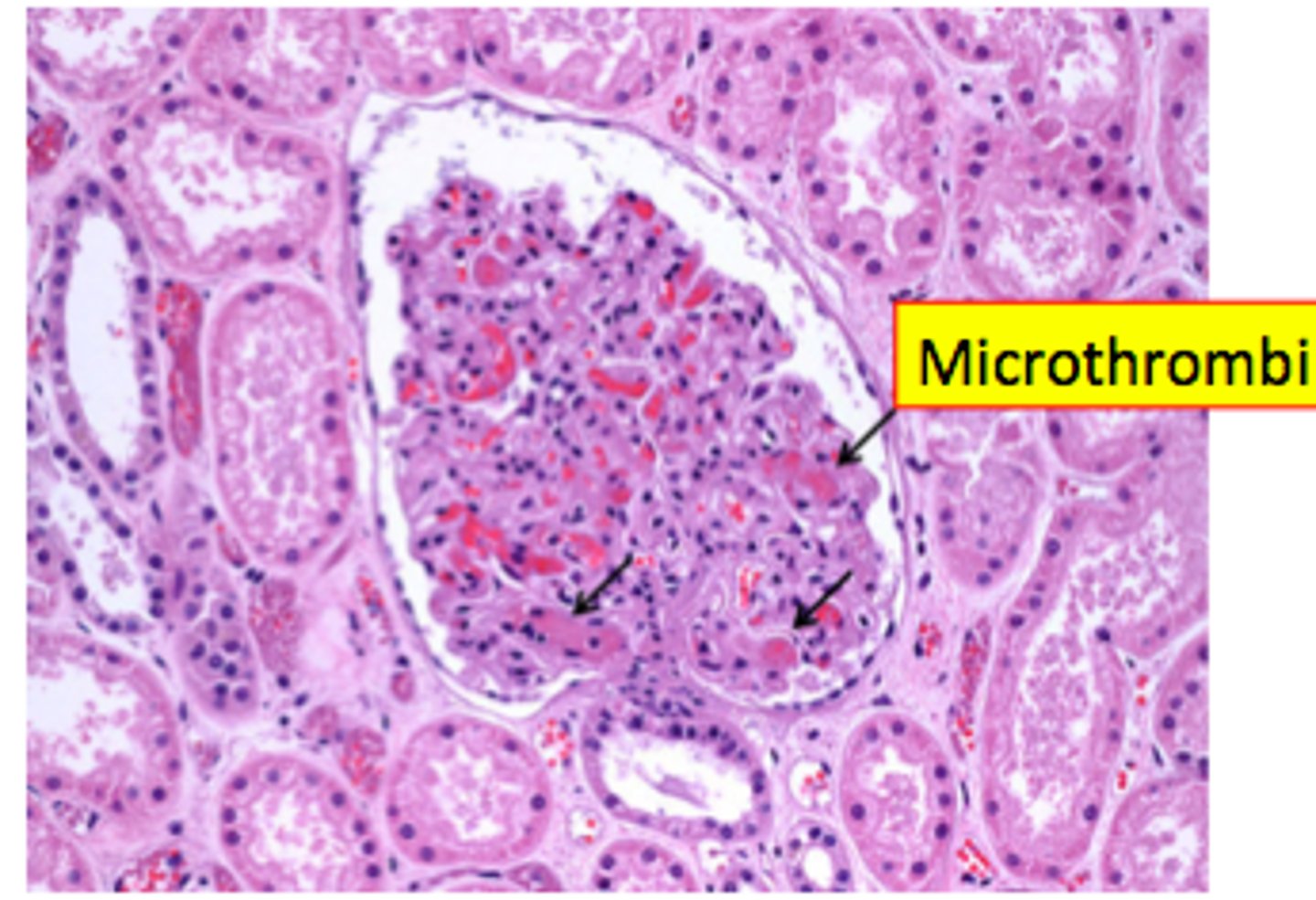
How does vasoconstriction and microthrombosis occur in reperfusion injury
- prolonged exposure to cold induces severe vasoconstriction and endothelial damage (no more hunting reflex, only vasoconstriction)
- promotes formation of microthrombi (obstructs circulation)
How does inflammation occur in reperfusion injury
- rewarming prompts a surge of inflammatory mediators (eg. prostaglandins, thromboxane A2, ROS)
- inflammatory mediators increase capillary permeability => edema => further ischemia => tissue necrosis
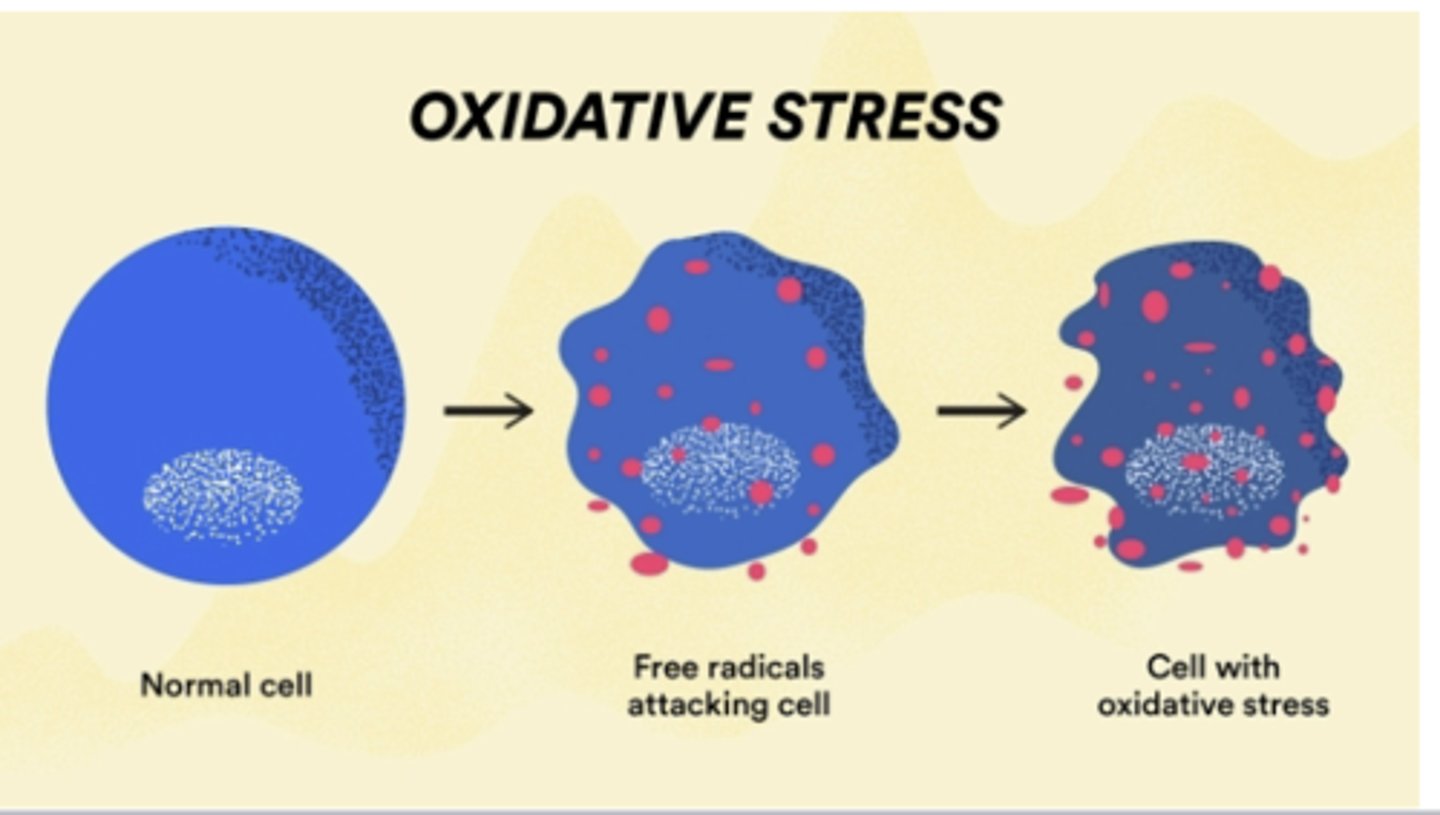
How does oxidative stress occur in reperfusion injury
- the restoration of oxygen-rich blood to damaged tissues triggers oxidative stress and free radical formation
- further compromises cell membranes and exacerbates tissue destruction
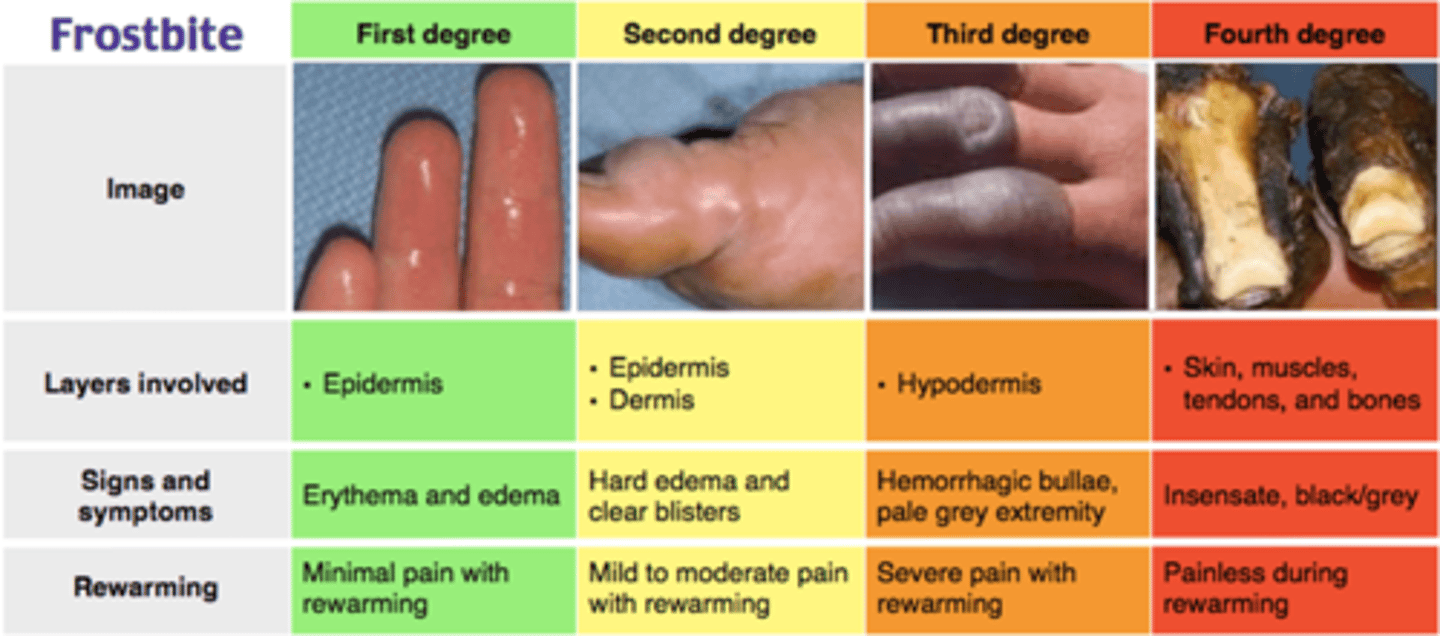
What are the different classifications of frostbite
1. First Degree: Superficial involvement with erythema and edema (full function remains, get warmth (eg. water) to the affected area asap!)
2. Second Degree: Formation of clear blisters; the skin remains soft (still functional/pliable)
3. Third Degree: Hemorrhagic blisters indicating deeper injury (filled with blood, SOME fx remains)
4. Fourth Degree: Full-thickness damage affecting muscles, tendons, and bones (cannot move affected joint, DEEP injury, may not be saveable)
what is frostbite a result of (cellular level)
* result of an initial extracellular freezing injury followed by a reperfusion injury due to vasoconstriction and microthrombosis in affected tissues

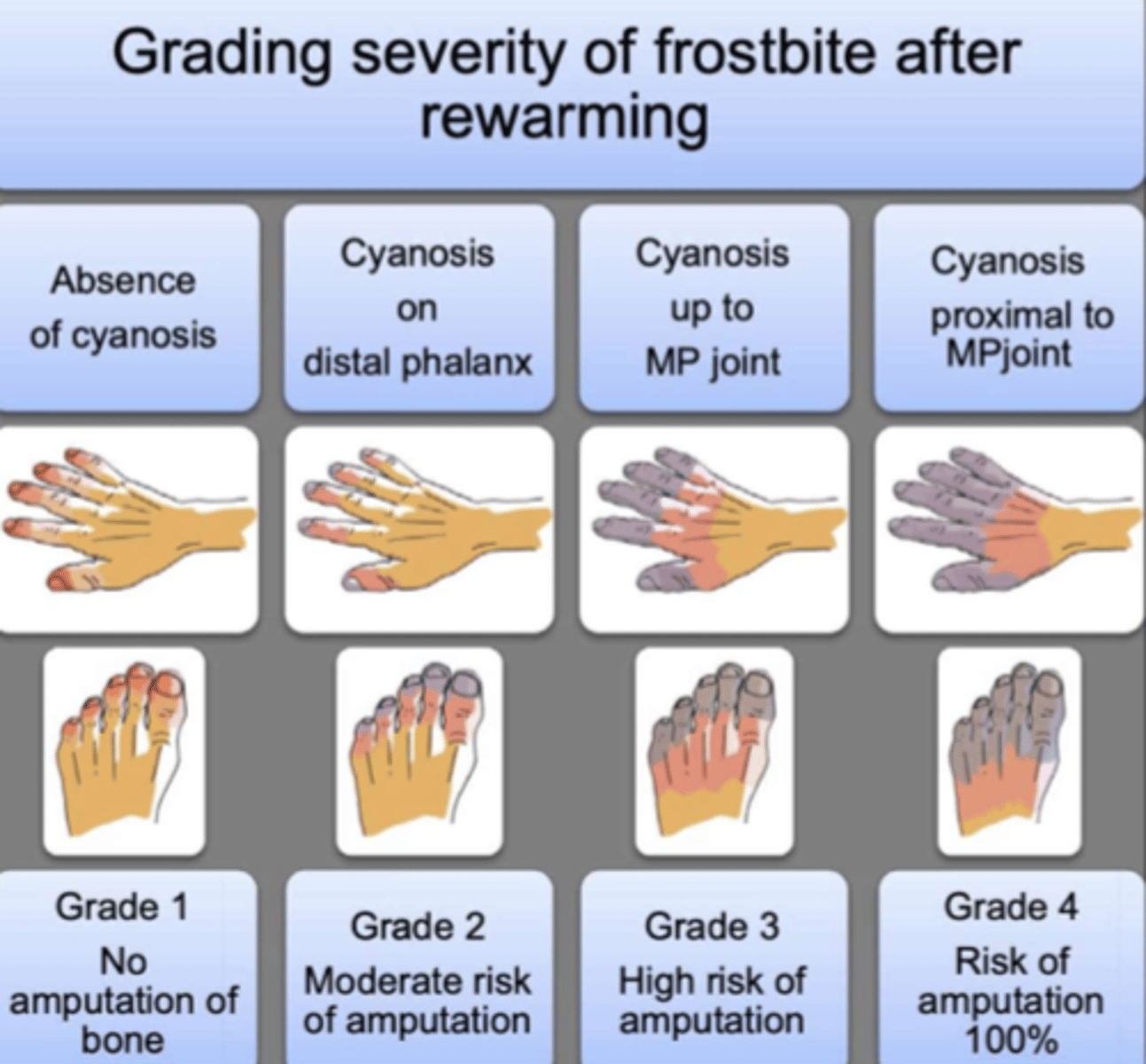
How do we grade severity of frostbite after rewarming
- Grade 1: absence of cyanosis - no amputation of bone
- Grade 2: cyanosis on DISTAL phalanx - moderate risk of amputation
- Grade 3: cyanosis up to metaphalangeal (MP) joint (eg. knuckles) - high risk of amputation
- Grade 4: cyanosis proximal to MP joint (eg. past knuckles, reaching palm) - risk of amputation 100%
What do we do FIRST to manage frostbite (initial actions)
- immediate actions: remove pt from cold environment and avoid refreezing
- rewarming: use warm water baths (37-39°C) for 15-30 minutes
- pain management: administer analgesics PRN
How do we manage frostbite pharmacologically
- NSAIDs (eg. Ketorolac IV, Ibuprofen) => need to address inflammation BEFORE/during rewarming to avoid reperfusion injury & therefore further damage
- analgesics => opioids (eg. Morphine, Hydromorphone) (*body will have a harder time healing in stress/pain!)
- abx => prophylactic use (prevents infection in cases with tissue necrosis) (eg. cephalexin, clindamycin, zosyn)
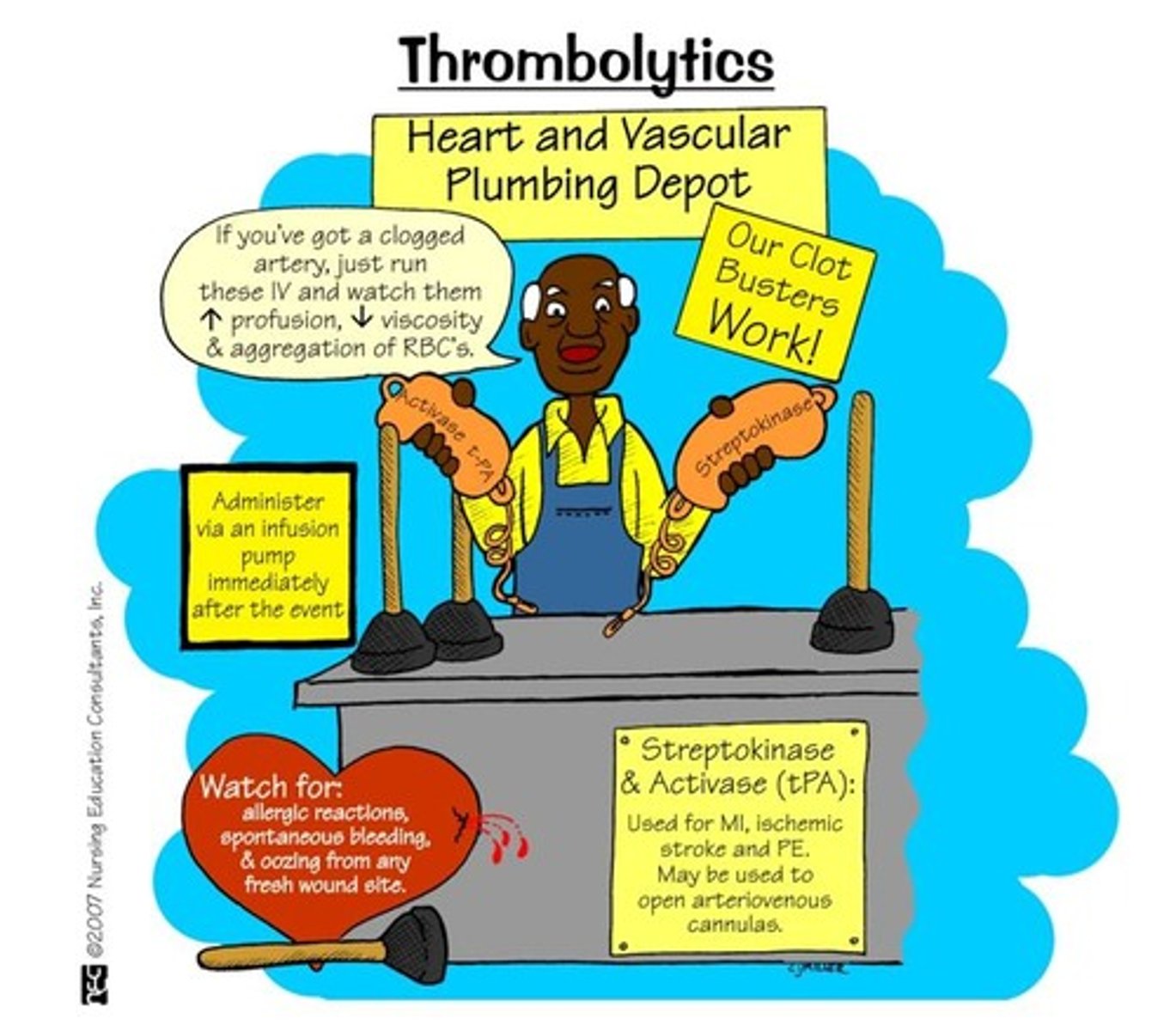
- thrombolytics: agents like tPA (eg. alteplase) may be considered to restore blood flow in severe cases if clotting occurs (dissolving the clot)

How do we manage systemic hypothermia in frostbite cases
- SLOW rewarming (don't want reperfusion injury)
- correct acidosis, hyperglycemia, hyperkalemia, and organ dysfunction

What should we NOT do in frostbite cases (tx)
- do NOT rub hands => tissue is already damaged, do not want to damage it more
What would enoxaparin be used for in frostbite
- prevention of clot formation (anticoagulant)
What would we use vasodilators in frostbite cases
- to expand blood vessels => increases blood flow to affected tissues
(eg. Nifedipine, Prostacyclin analogs like Iloprost)
- NOTE* hypotension risk which may further compromise circulation
How does wound care/infection prevention work in frostbite cases
- debridement: removal of necrotic tissue to promote healing
- topical abx: application to prevent local infections (eg. silver sulfadiazine, mupirocin)
- tetanus prophylaxis: ensure vaccination is up to date (Tdap, Td vaccine)
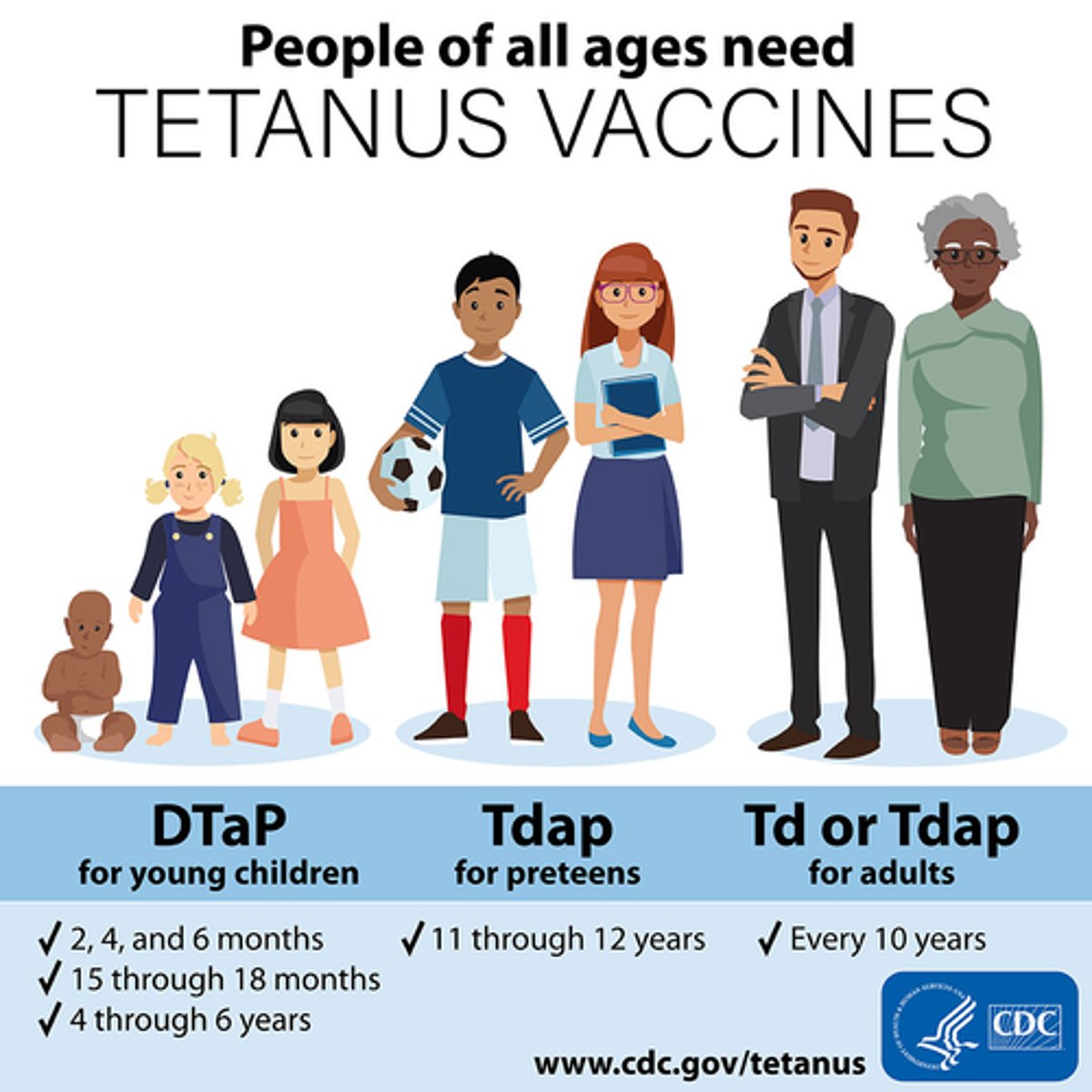
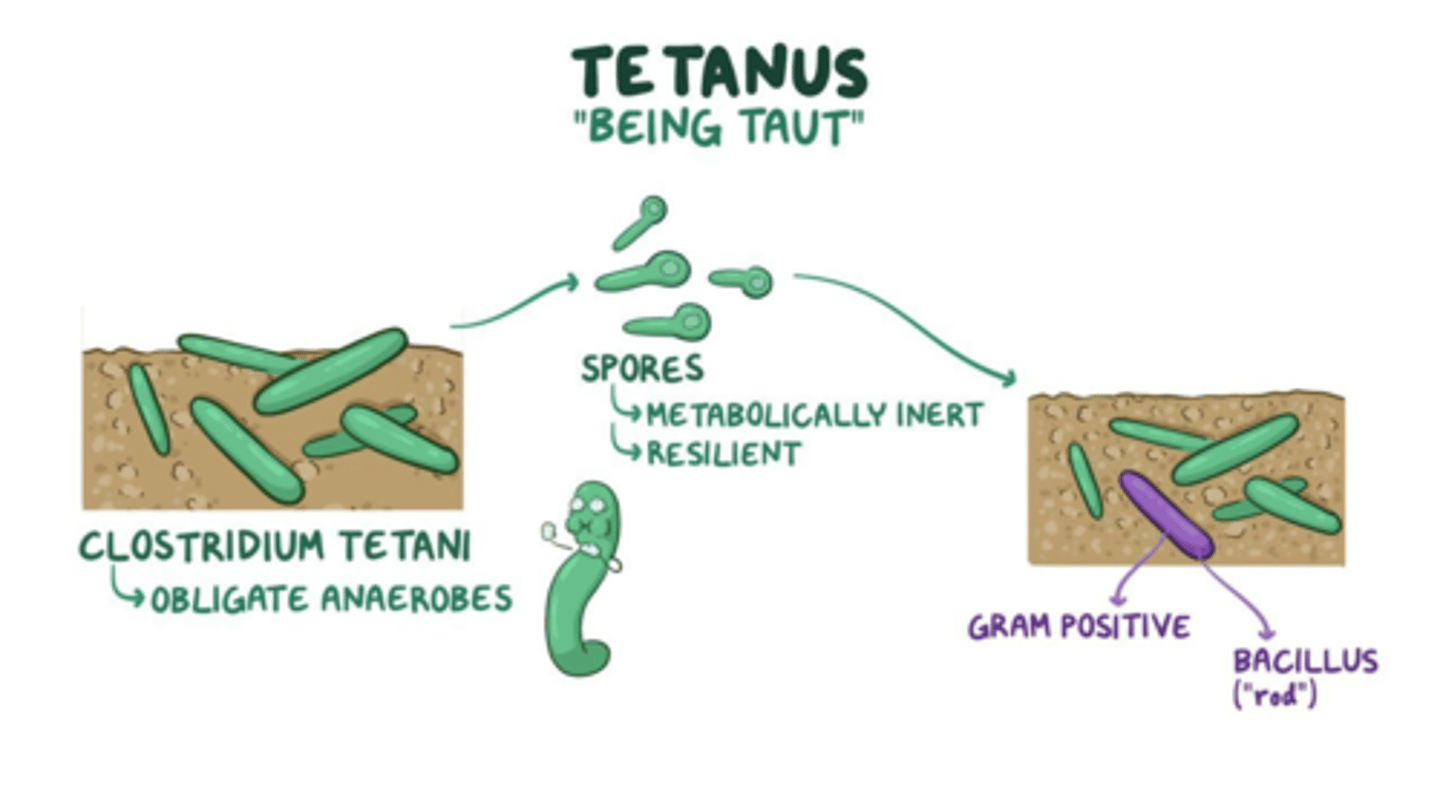
Why do we want pts to have their tetanus vaccine (esp. in frostbite)
- b/c tetanus is an anaerobic bacterium that lives in low O2 areas
=> necrotic tissue from frostbite may bring this infection to life w/o a vaccine
A patient recovering from frostbite asks what long term management includes, you say:
- physical therapy: to return function and mobility
- monitoring for complications: such as chronic pain or sensory deficits
- patient education: on preventing future cold injuries

A patient with frostbite is prescribed an NSAID for to reduce inflammation and provide pain relief. Which drugs would this include?
Ketorolac IV or Ibuprofen

Which opioids may be given to treat frostbite?
Morphine or Hydromorphone for severe pain relief

Why is Alteplase prescribed to treat frostbite?
it's a thrombolytic that dissolves blood clots
What are the 4 main mechanisms that occur in cellular injury (an injury may contain all of these mechanisms - depends on injury severity)
- inflammation
- hypoxemia/hypoxia = ischemia
- electrolyte dysfunction
- free radicals
How does inflammation occur in cellular injury
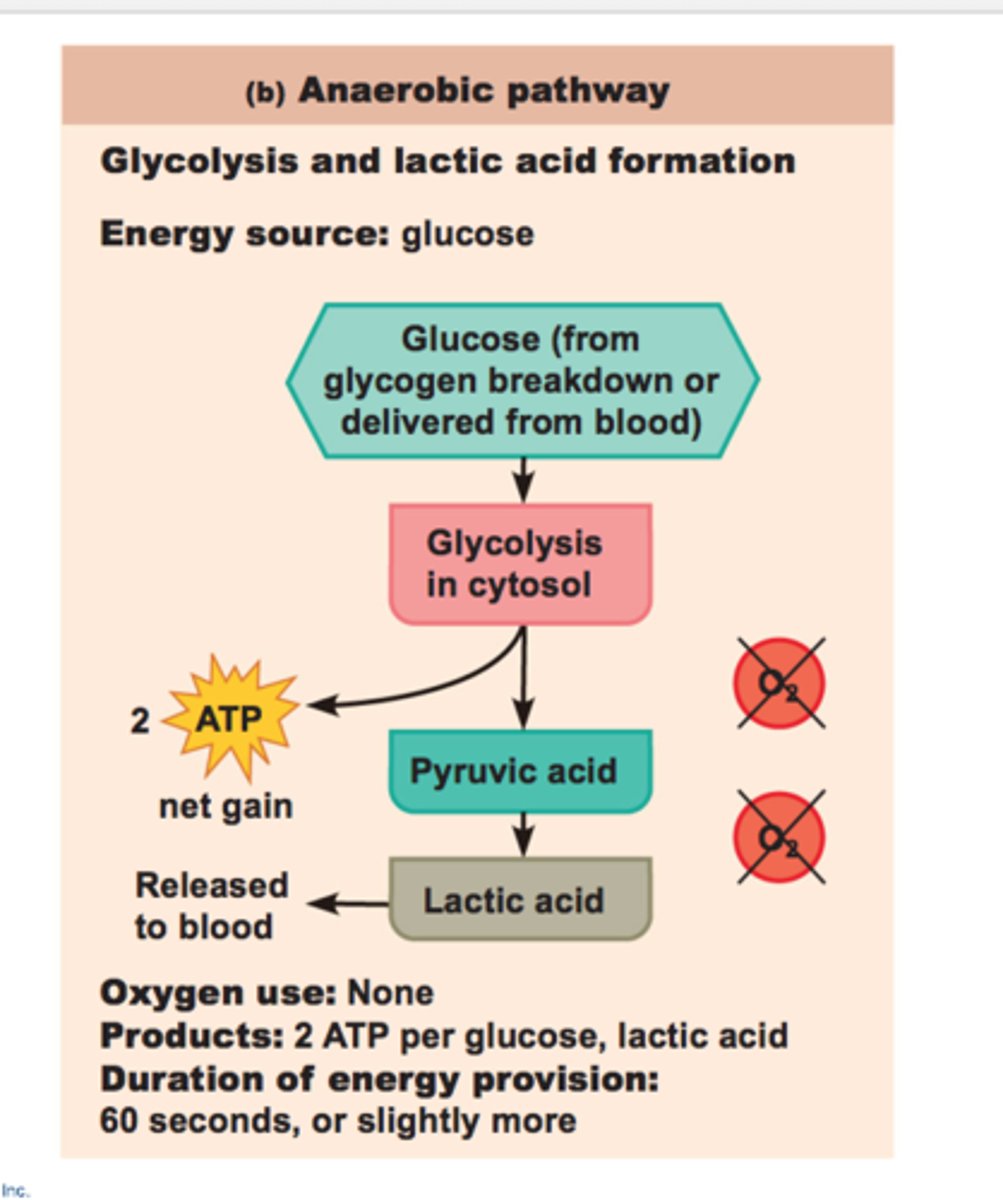
- tissue edema causes high tissue pressure, decreased perfusion to cells, and hypoxia/ischemia resulting in anaerobic metabolism
- vasodilation causes further risk of low perfusion pressure leading to ischemia + anaerobic metabolism (metabolic acidosis risk)
- clotting (can trigger severe hypotension)
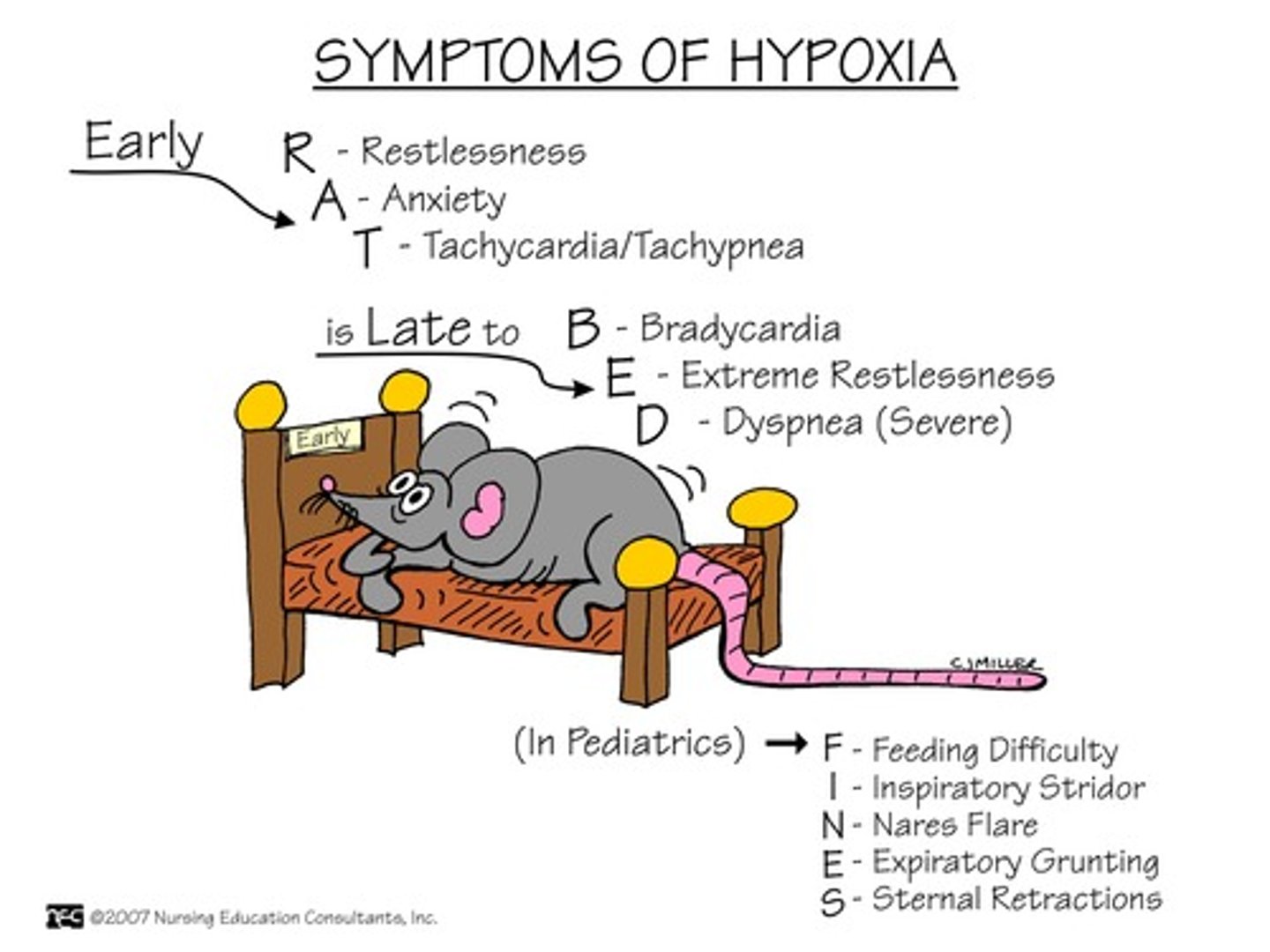
How does hypoxemia/hypoxia (& therefore ischemia) occur in cellular injury
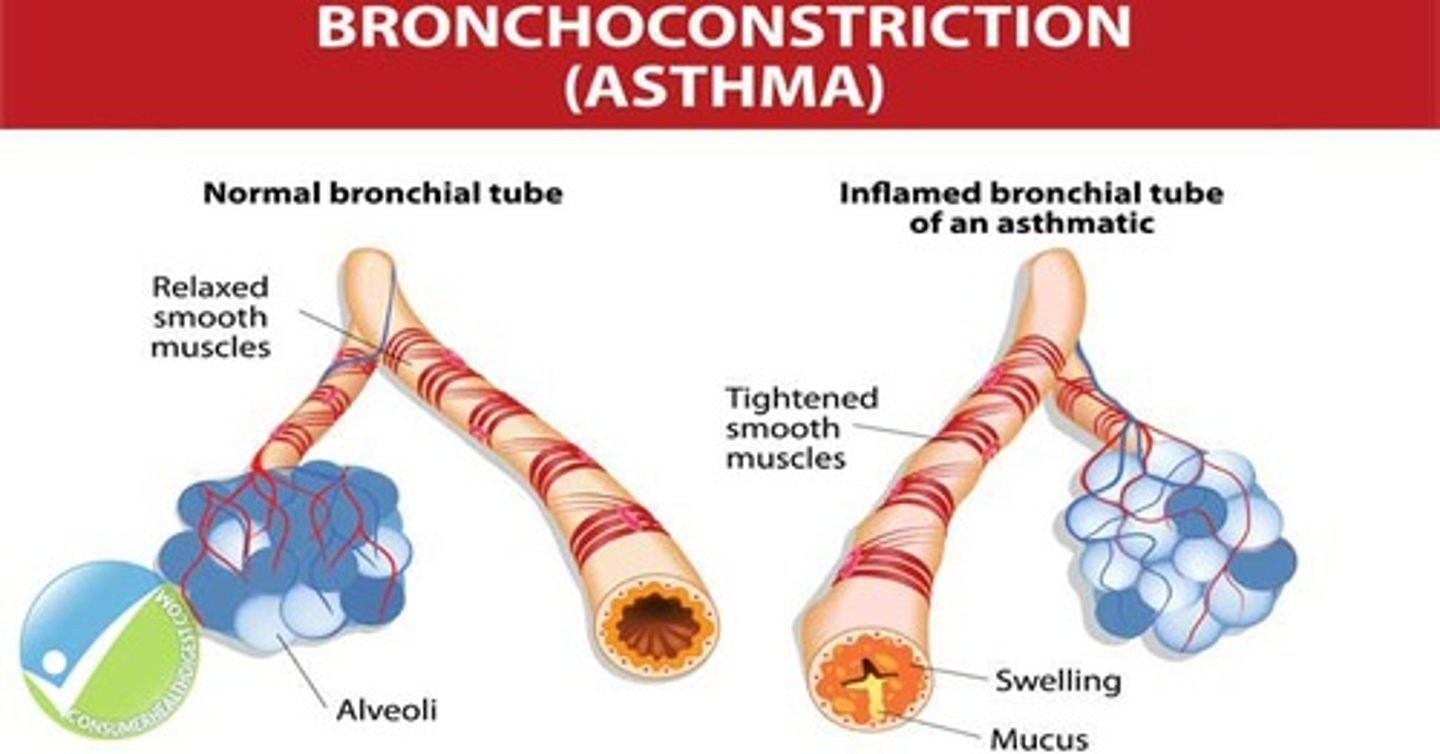
- low O2 (< 21%) availability due to eg. constriction/obstruction such as:
- bronchoconstriction (eg. asthma)
- thrombus/embolus (eg. PE)
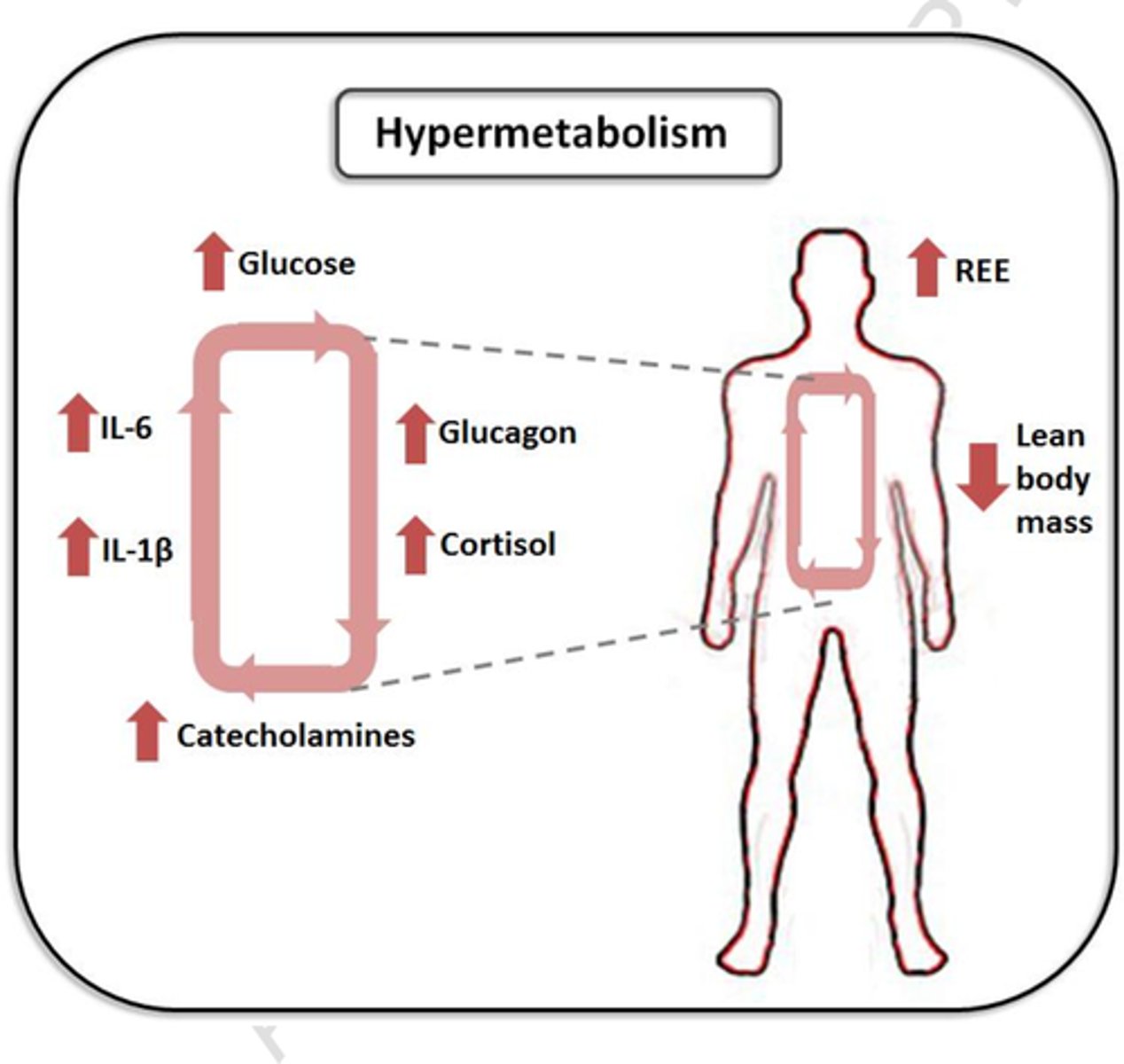
- hypermetabolic states (depleted resources and therefore increased demand) (eg. fever, burns)
How do hypermetabolic states occur within the body
- due to increased temperatures within the body, increasing resources needed to supply conditions
- results in depleted resources
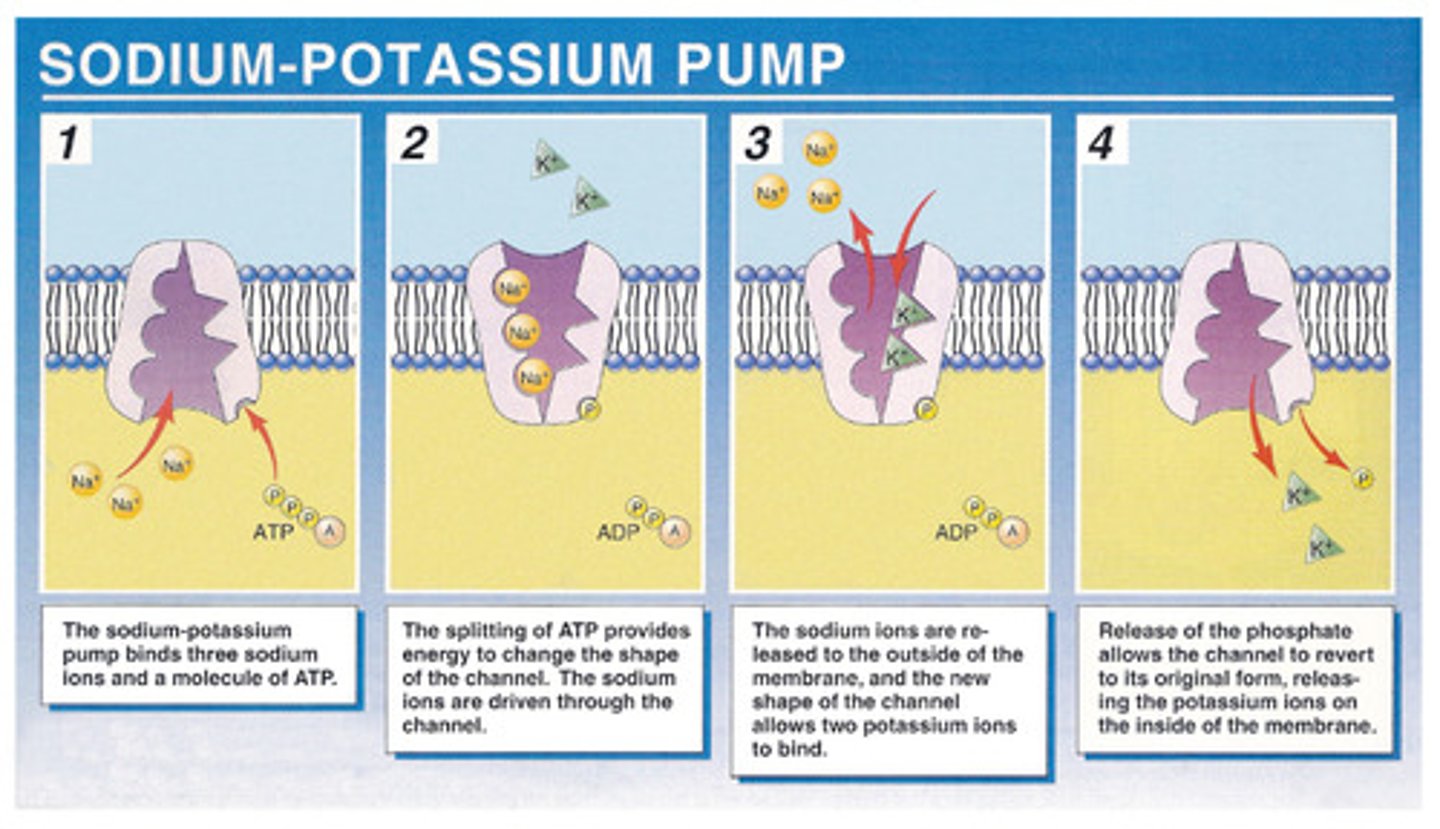
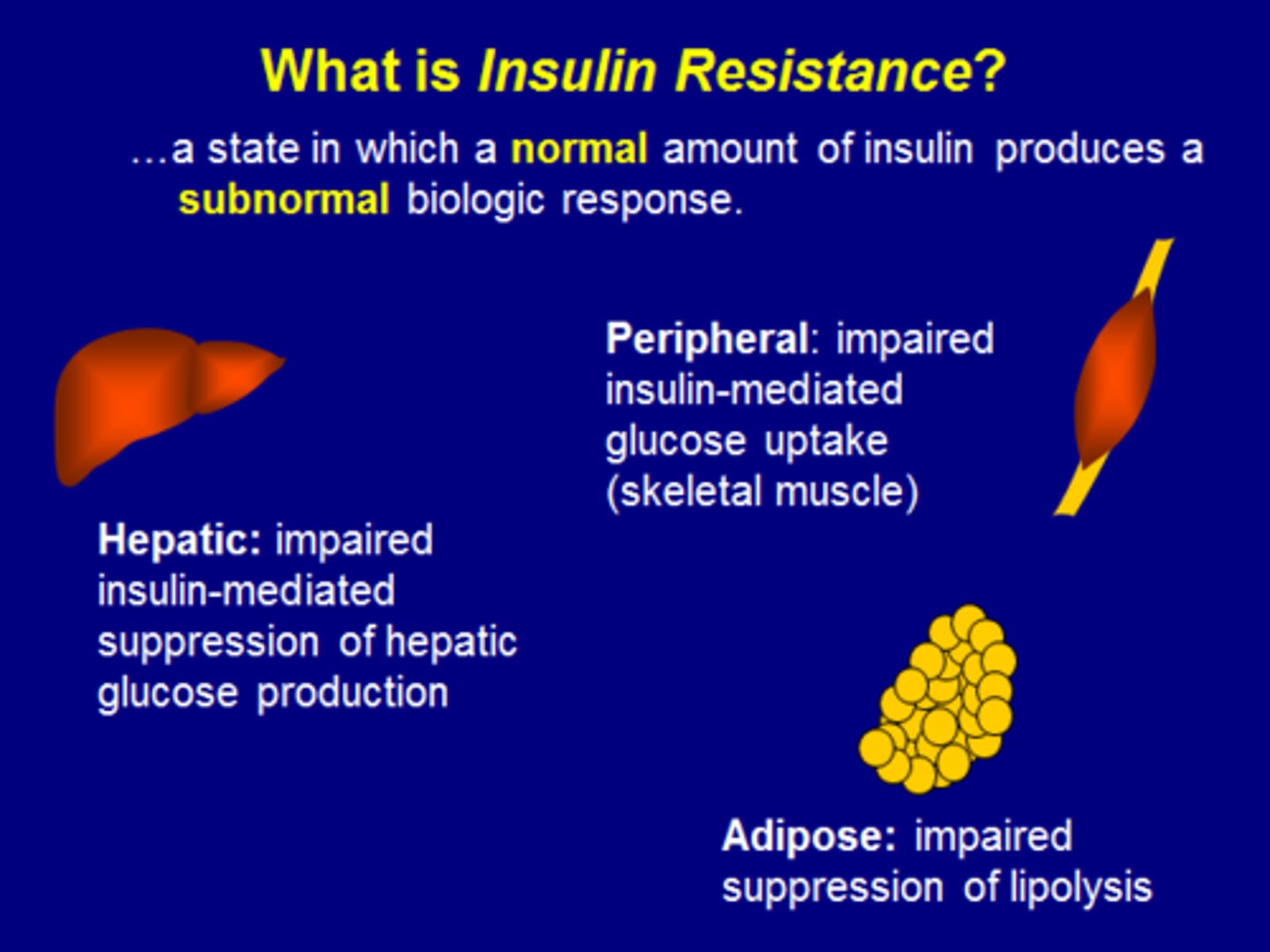
How does electrolyte dysfunction occur in cellular injury
- electrolyte pump dysfunction => high intracellular calcium/low intracellular K+ (& therefore low serum levels, decreasing electrolyte availability to cells)
=> mitochondrial dysfunction, low ATP, shift to anaerobic metabolism
= lactic acid production + loss of cellular fx (eg. insulin resistance (due to decreased pancreatic production), renal failure, low immunity)
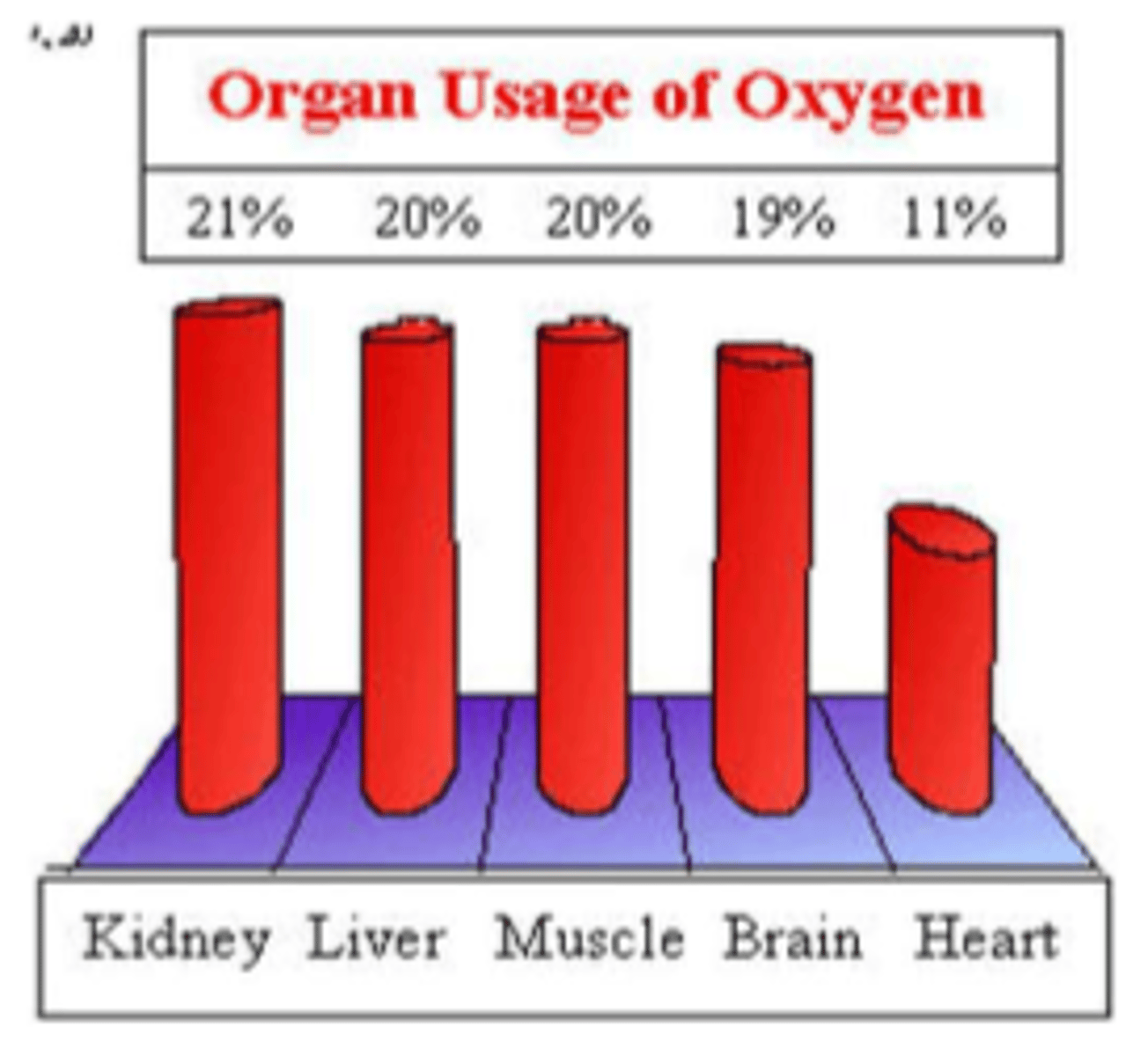
How much O2 does each organ use
- kidneys: 21%
- liver: 20%
- muscles: 20%
- brain: 19%
- heart: 11%
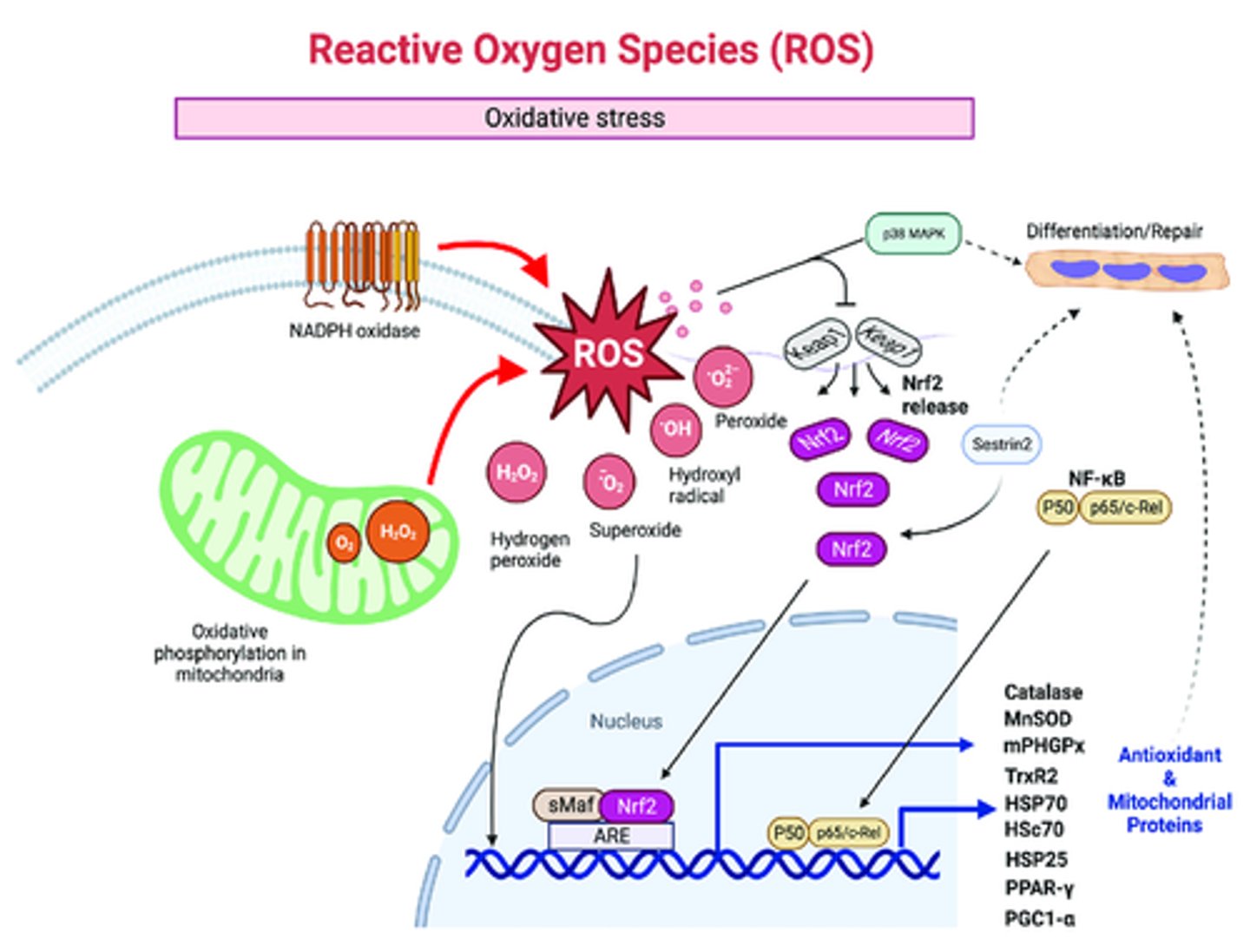
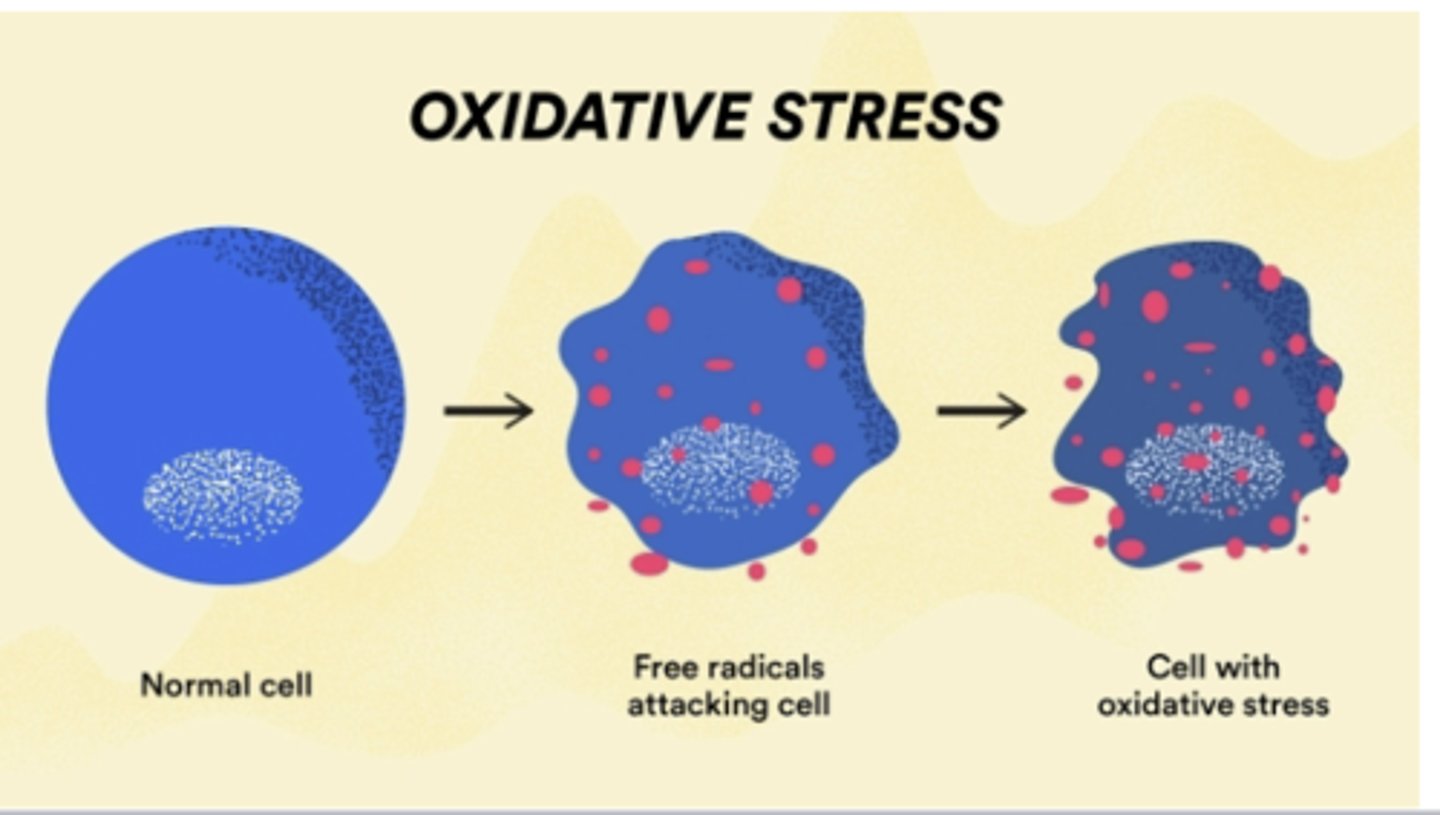
What are free radicals & how are they produced
- molecules containing an 'unpaired' electron" (essentially a healthy cell that is missing an electron) => therefore unstable & reactive => produces oxidative stress (eg: ROS, RNS)
- produced by: noxious stimuli (drugs/drug metabolites eg. nicotine), pathogens (eg. bacterial toxins), excessive inflammatory mediators, radioactive substances/radiation, or cellular metabolism (eg. ageing)
What do free radicals cause direct damage to
- cell membranes (lipid bilayer)
- cellular structures (e.g. DNA)
- enzyme processes
What are ROS free radicals
- ROS = reactive oxygen species
- unstable 'O2' (eg. OH, H2O2)
- natural byproduct of normal respiration & cellular metabolism; chronic = ageing
- usually balanced by 'antioxidants', high amounts formed in altered cellular metabolism
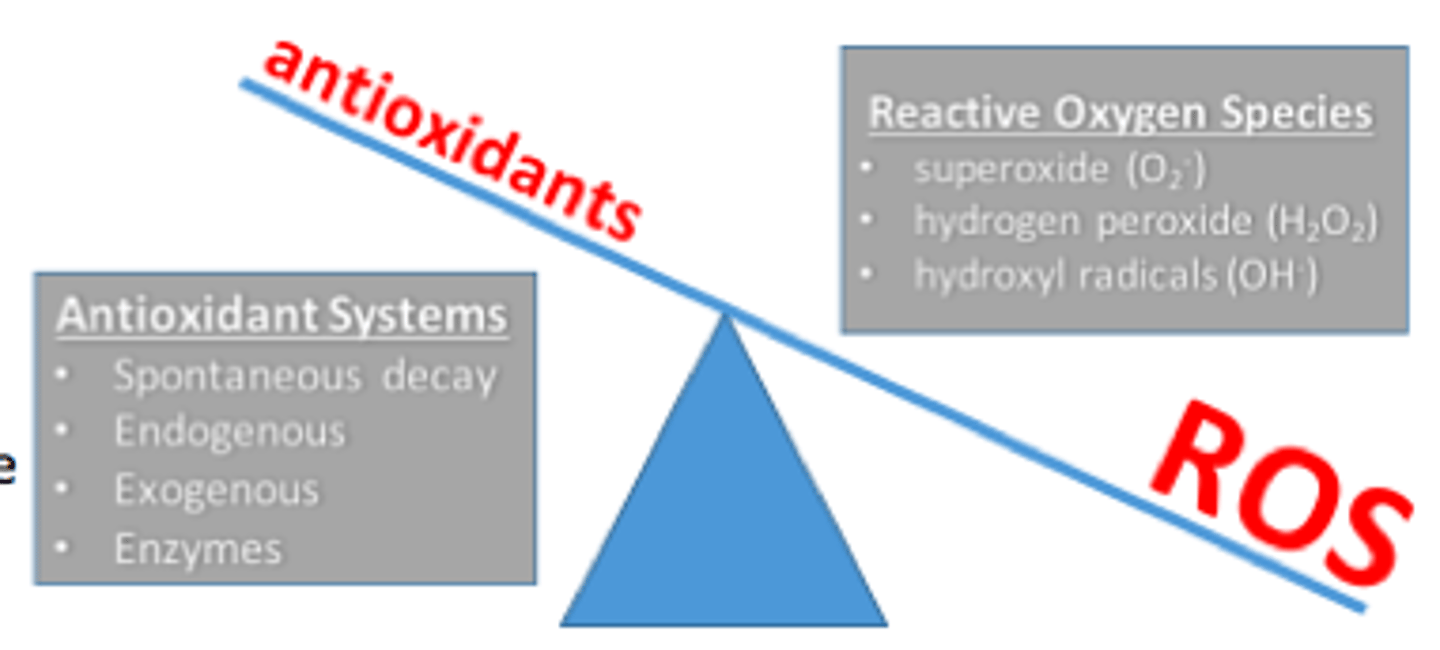
How are ROS usually balanced within the body
- balanced by 'antioxidants' & endogenous scavengers (eg. catalase)
- these antioxidants phagocytose & interrupt presence of ROS, decreasing damage that can be caused
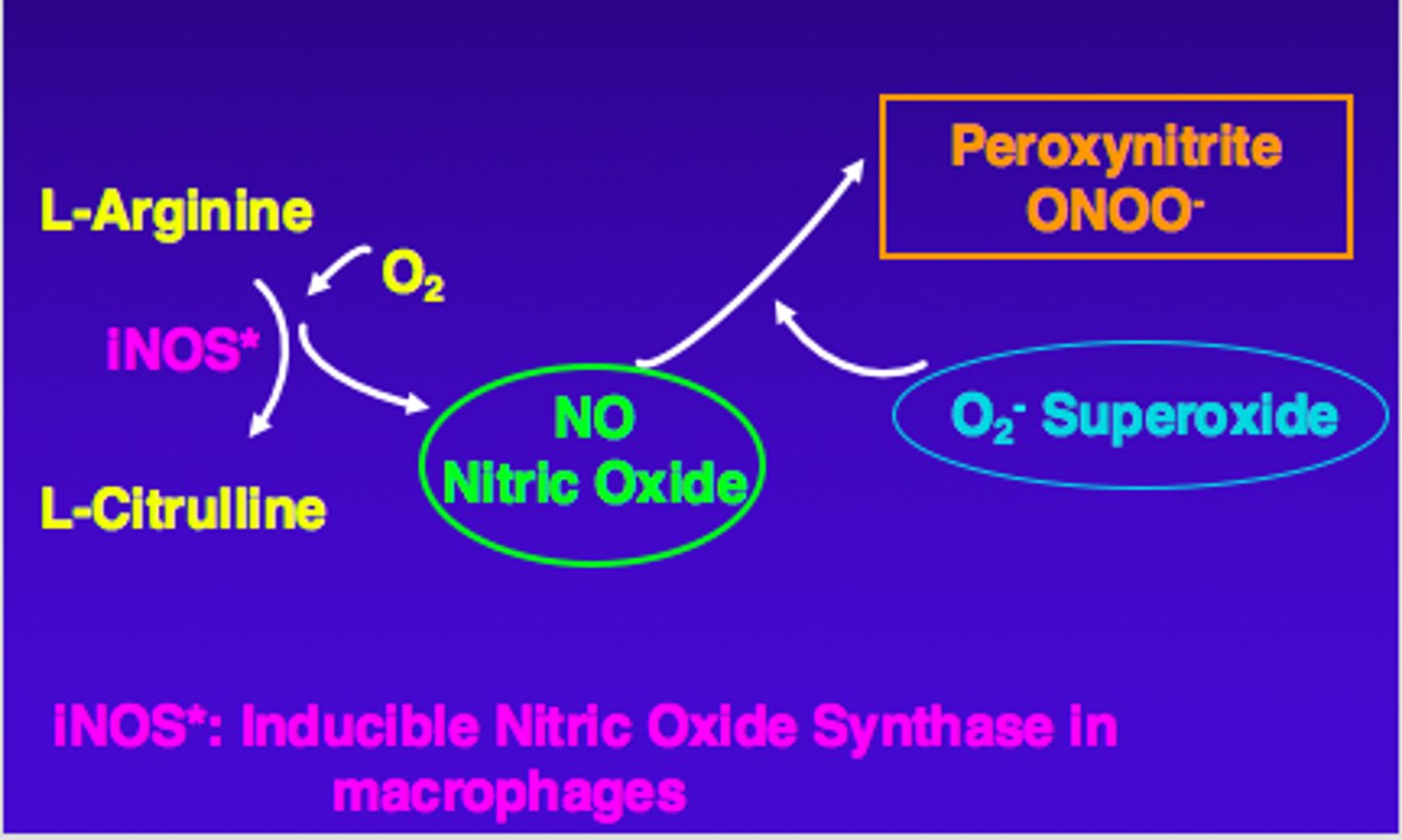
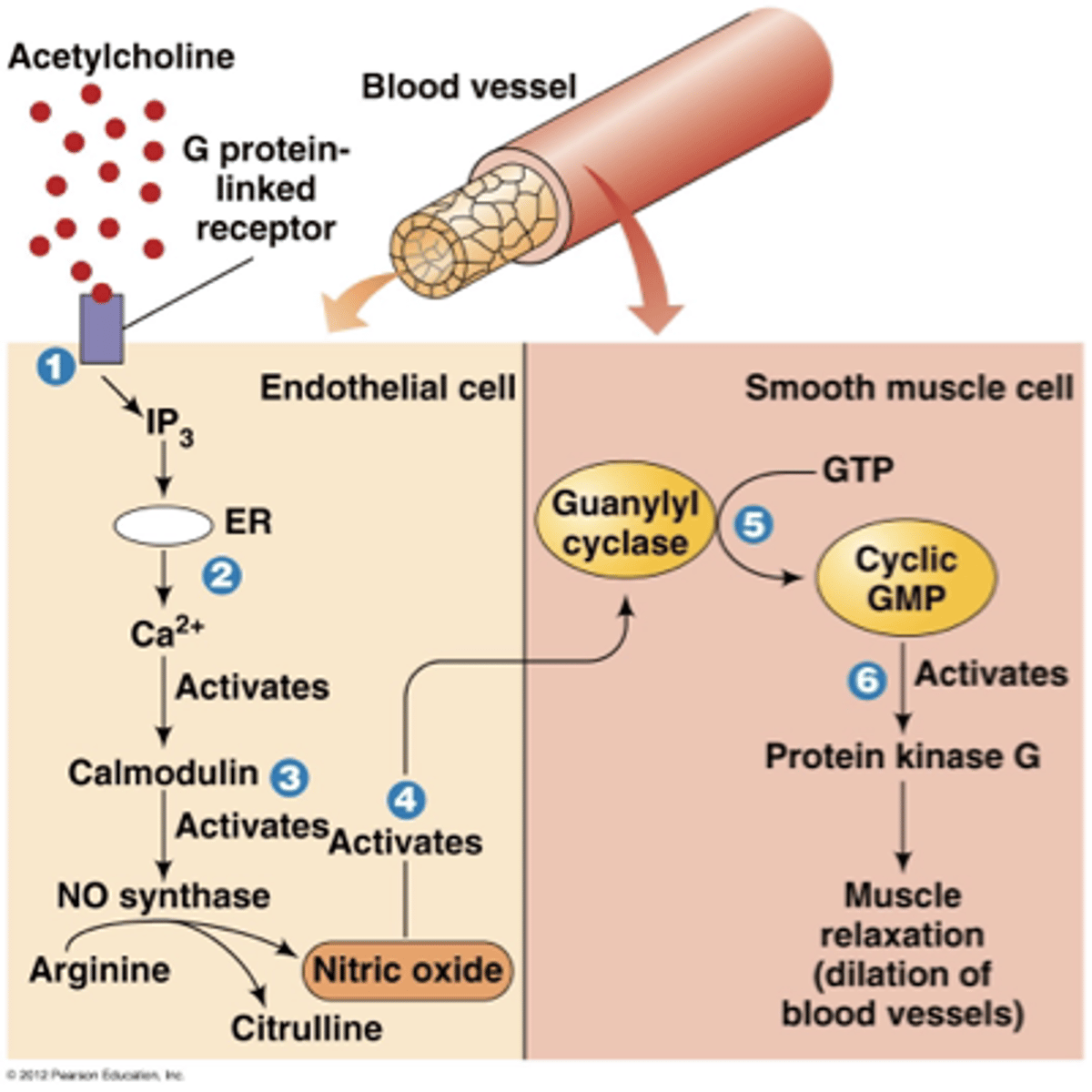
What are RNS free radicals
- RNS = reactive nitrogen species
- unstable nitric oxide
- NO released in high amounts during systemic vasodilation => RNS formed
What is an excess of free radicals called
'oxidative stress'
What is the fx of L-arginine and what happens if there is too much of it in the body
- makes nitric oxide
- excess levels increase risk of RNS presence and therefore oxidative stress
What is the fx of antioxidants and the main types
- decrease damaging effects of free radicals
- acquired in diet: Ascorbate (Vit C), Flavonoids, Carotenes (Vit A)
- endogenous enzyme: catalase

What is ionizing radiation
- a type of radiation therapy (eg. gamma knife, proton, x-ray) => target carefully calculated
- in excess: causes direct DNA damage + generates free radicals in excess => will cause organ damage (eg. skin, internal organs)

What happens if ionizing radiation causes direct cellular damage
- highest cellular damage to fast multiplying cells
- eg. systemic exposure => damage to bone marrow, hair, GI tract => s&s

What are the main types of radiation we see outside of the hospital
- UV radiation (UVR): UVB
- cytotoxic drugs emitting radiation (eg. Polonium => never used therapeutically due to toxicity)
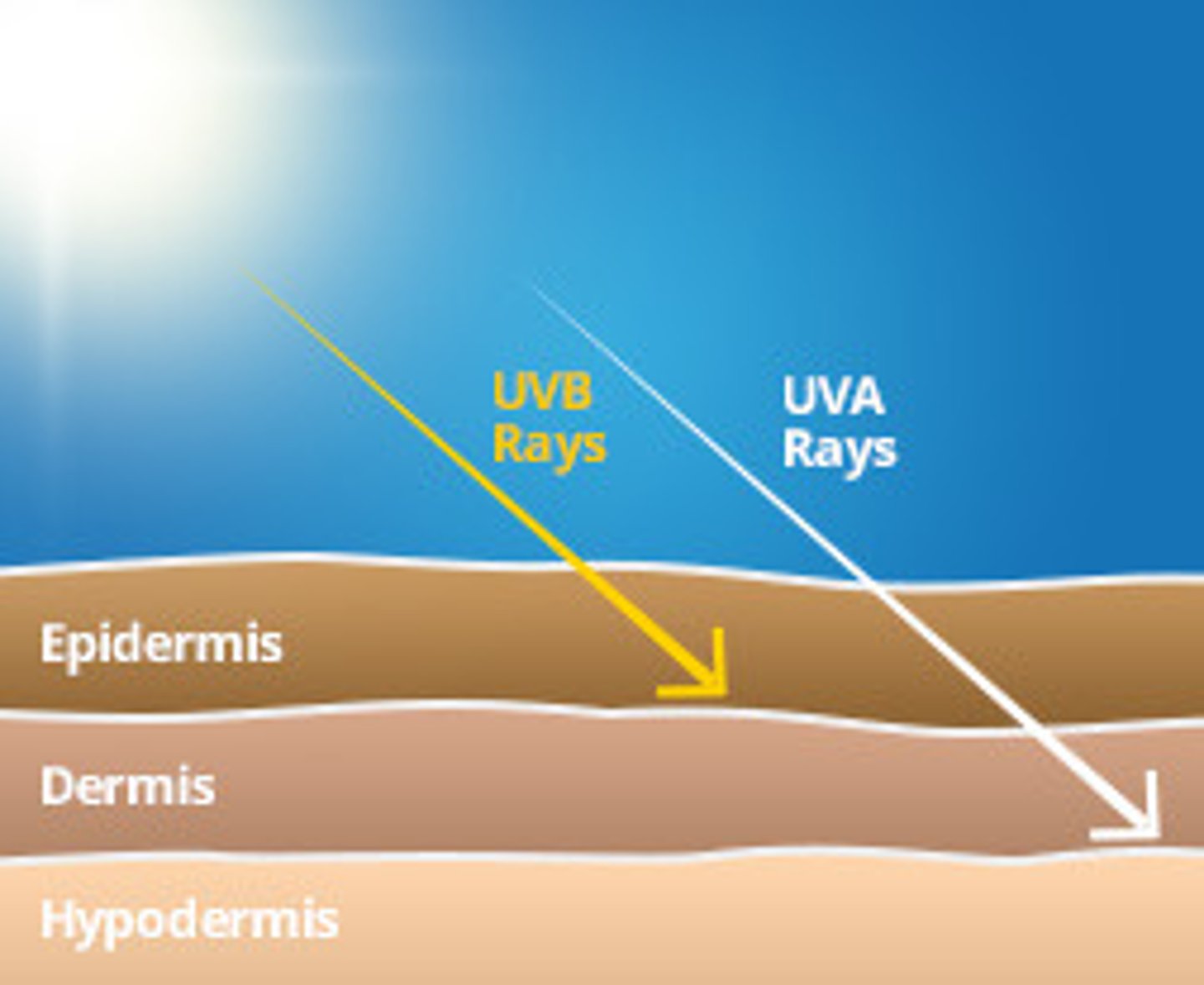
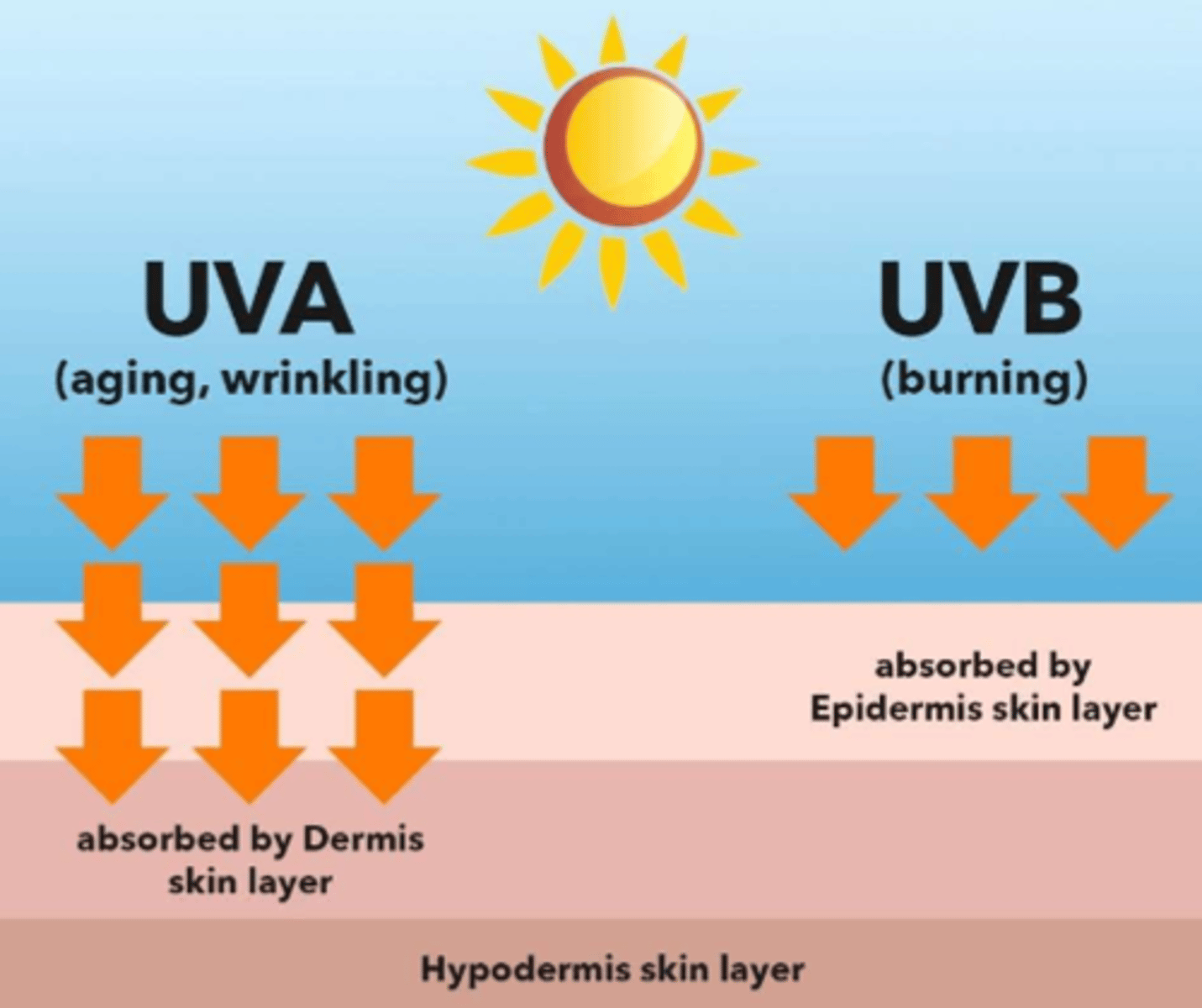
What are the different type of UV rays emitted by the sun
- UVB = sunburn (absorbed by epidermis)
- UVA = do not cause burns (low potency, low presence) (seen in ageing & wrinkling, absorbed by dermis)
- UVC = do not cause burns (low potency, low presence)
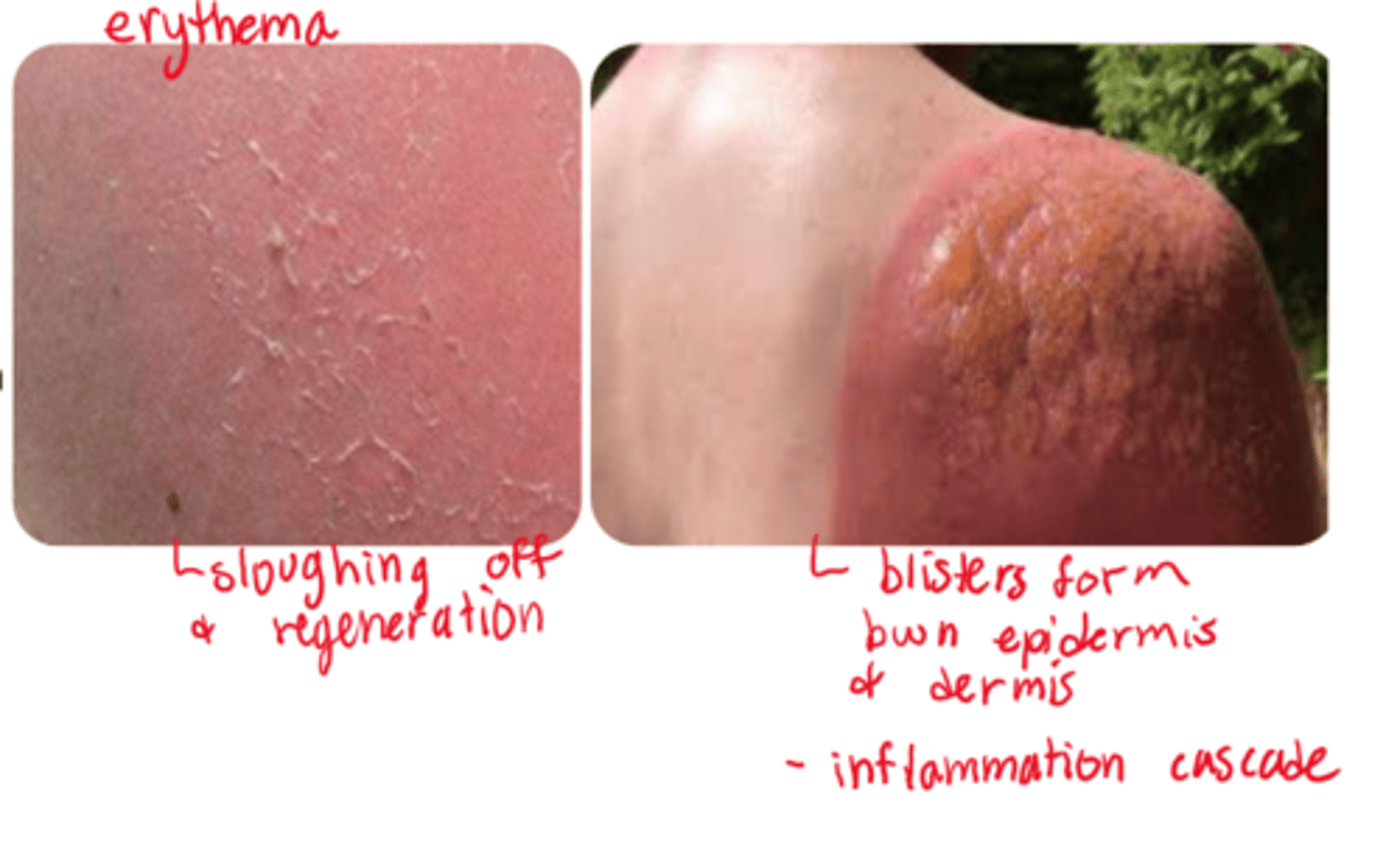
What is a UVB sunburn
- direct cell membrane disruption (skin tissue cells: melanocytes, Langerhans cells, immune cells)
- reactive oxygen &/or nitrogen formed => oxidative stress epidermal &/or dermal layers affected
- degree of damage varies per duration & intensity of exposure
- superficial effects (eg. erythema) vs systemic effects (eg. fever, chills, malaise, dehydration)
What are our UVB prevention choices
- sunscreens!! => can either absorb or reflect (usually about 20% of sunscreen component)
- non-sunscreen: clothing, behind glass (stay inside)
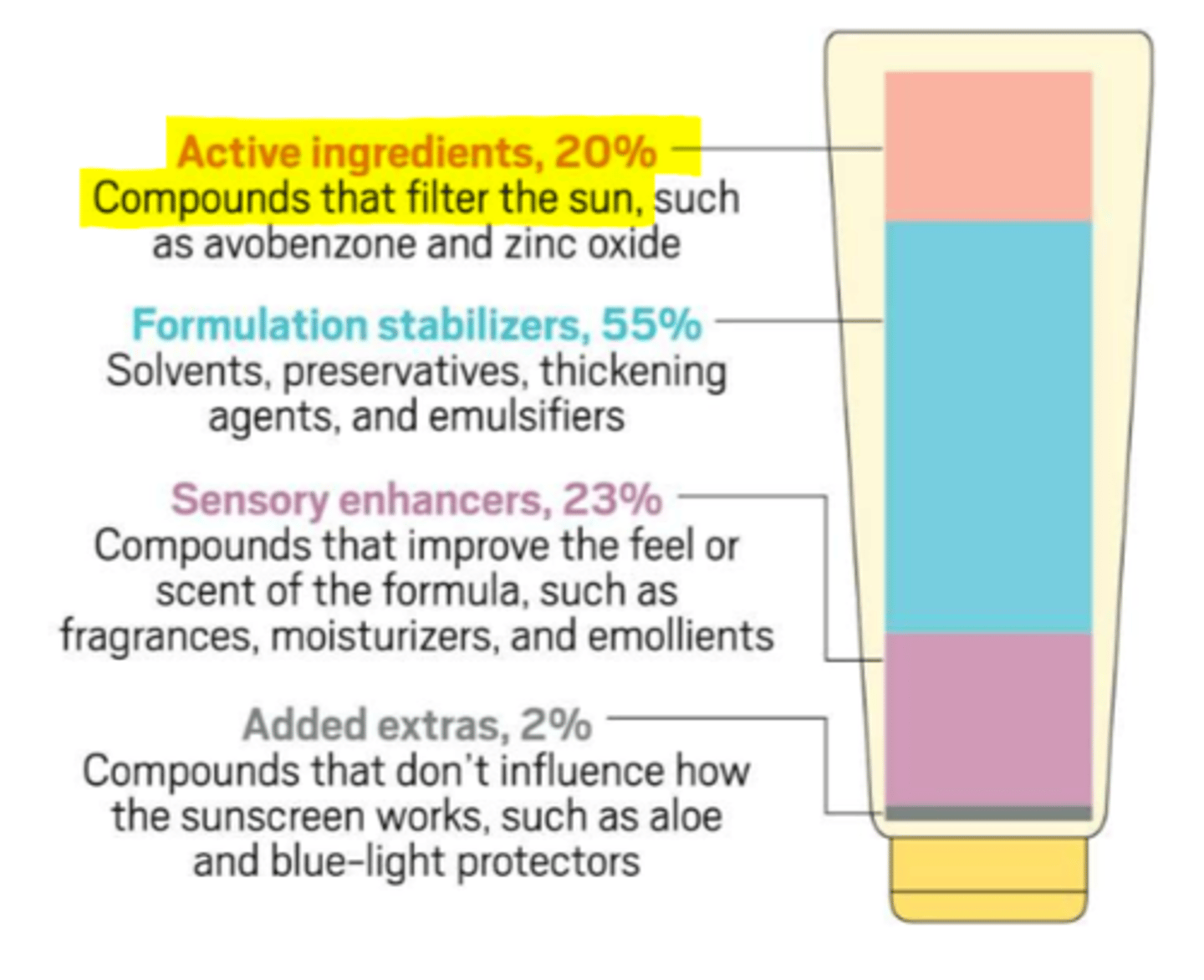
What drugs ABSORB UVR (topical => in sunscreen)
- drug class: benzones
- drugs: avobenzone, oxybenzone
- MOA: distributive shift of electrons => absorption & release (open up and expel the UVB)
What drugs REFLECT UVR (topical => in sunscreen)
- zinc or zinc-like
- MOA: physical protective layer
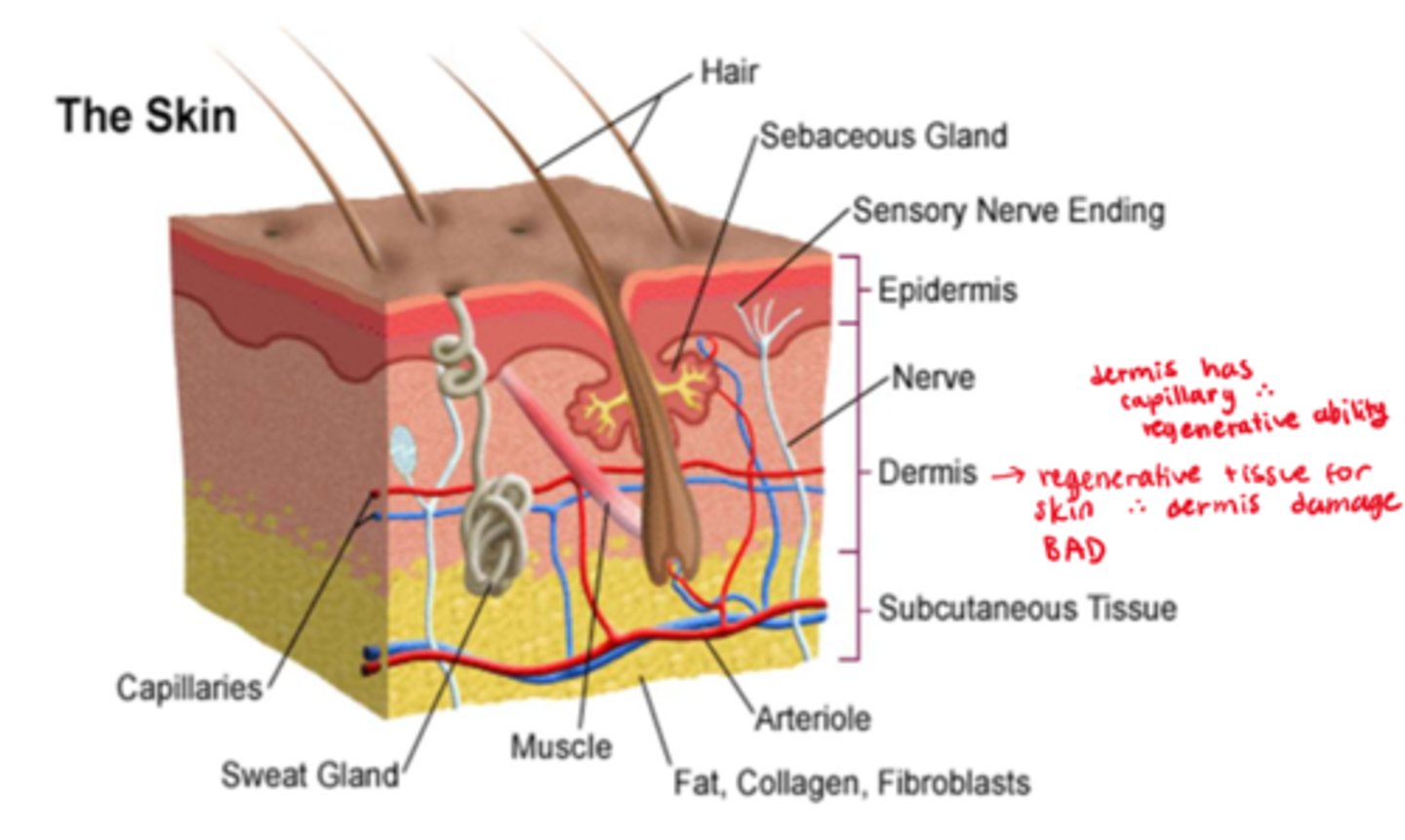
What are thermal burns overall
- associated with: flames, hot liquids, hot solid objects, steam
- not usually uniform in depth, many have a mixture of deep and superficial components
- burn wounds are dynamic => can progress to deeper wounds (may require several days for a final classification)
- regeneration is dependent on presence of dermal tissue, no dermal tissue means grafting is needed
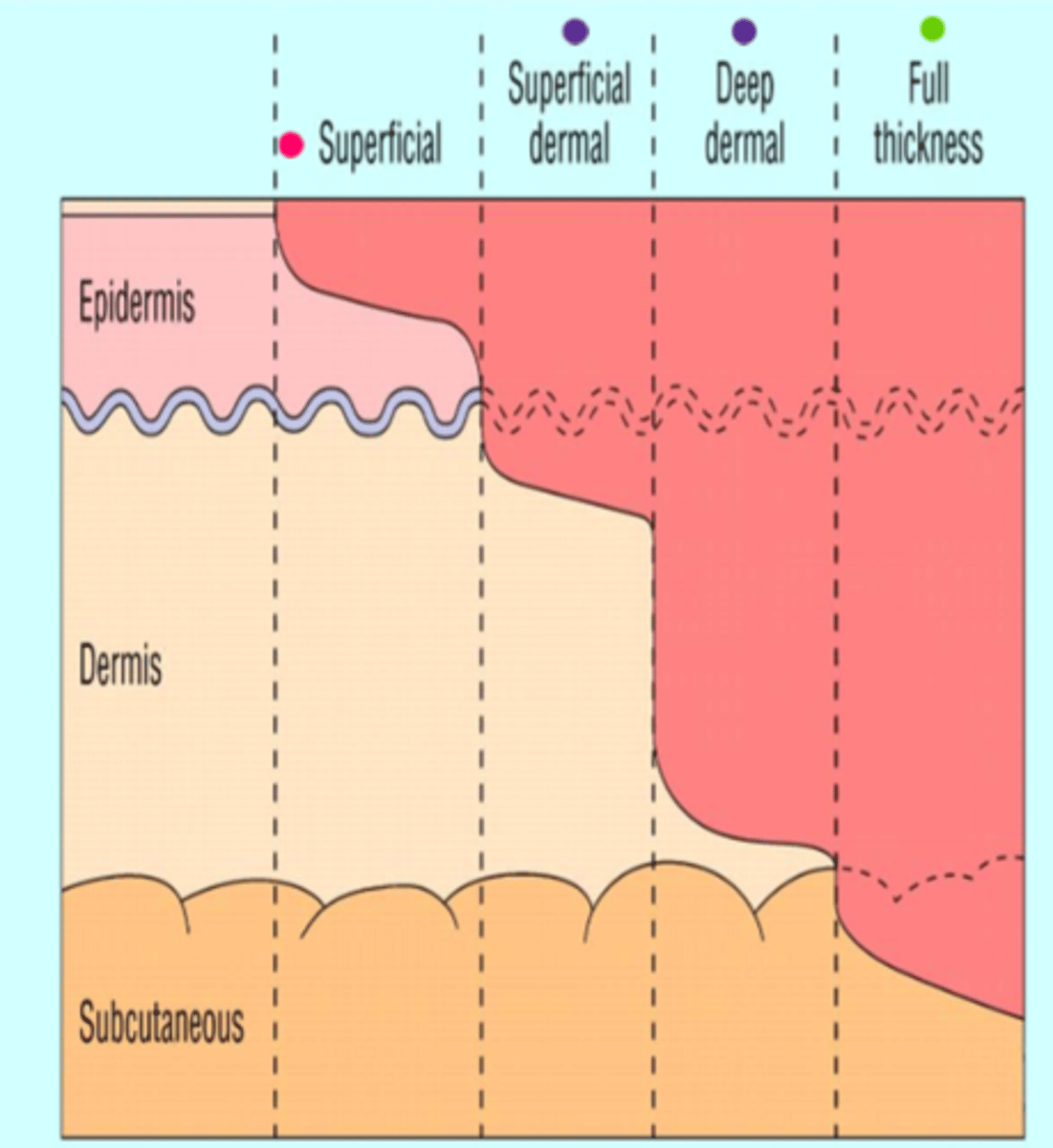
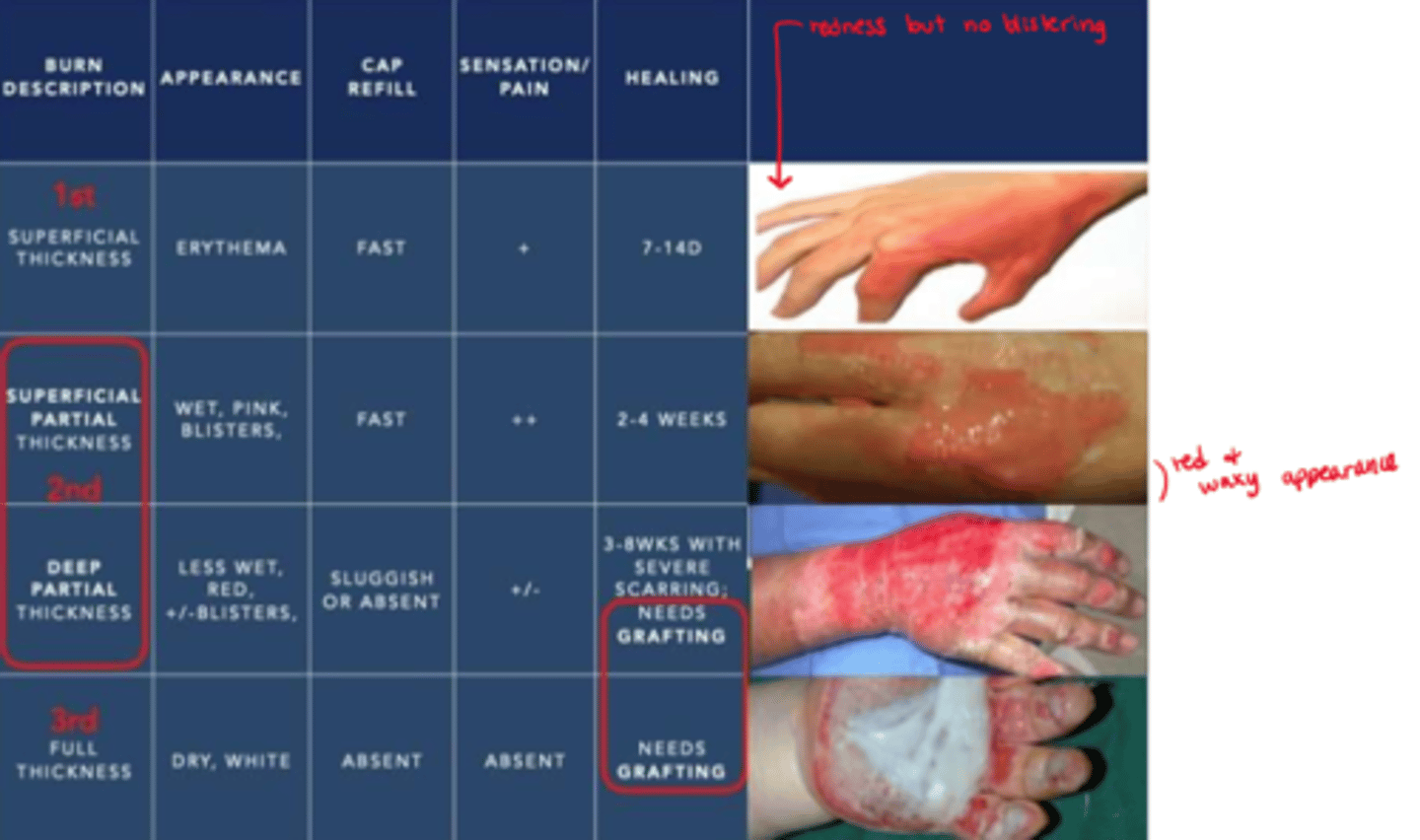
What are the 4 classifications of burns
1. Superficial ('epidermal')
2. Partial thickness (could be either 'superficial dermal' or 'deep dermal' involvement)
3. Full thickness
4. 4th degree
* not measured in degrees anymore except 4th degree
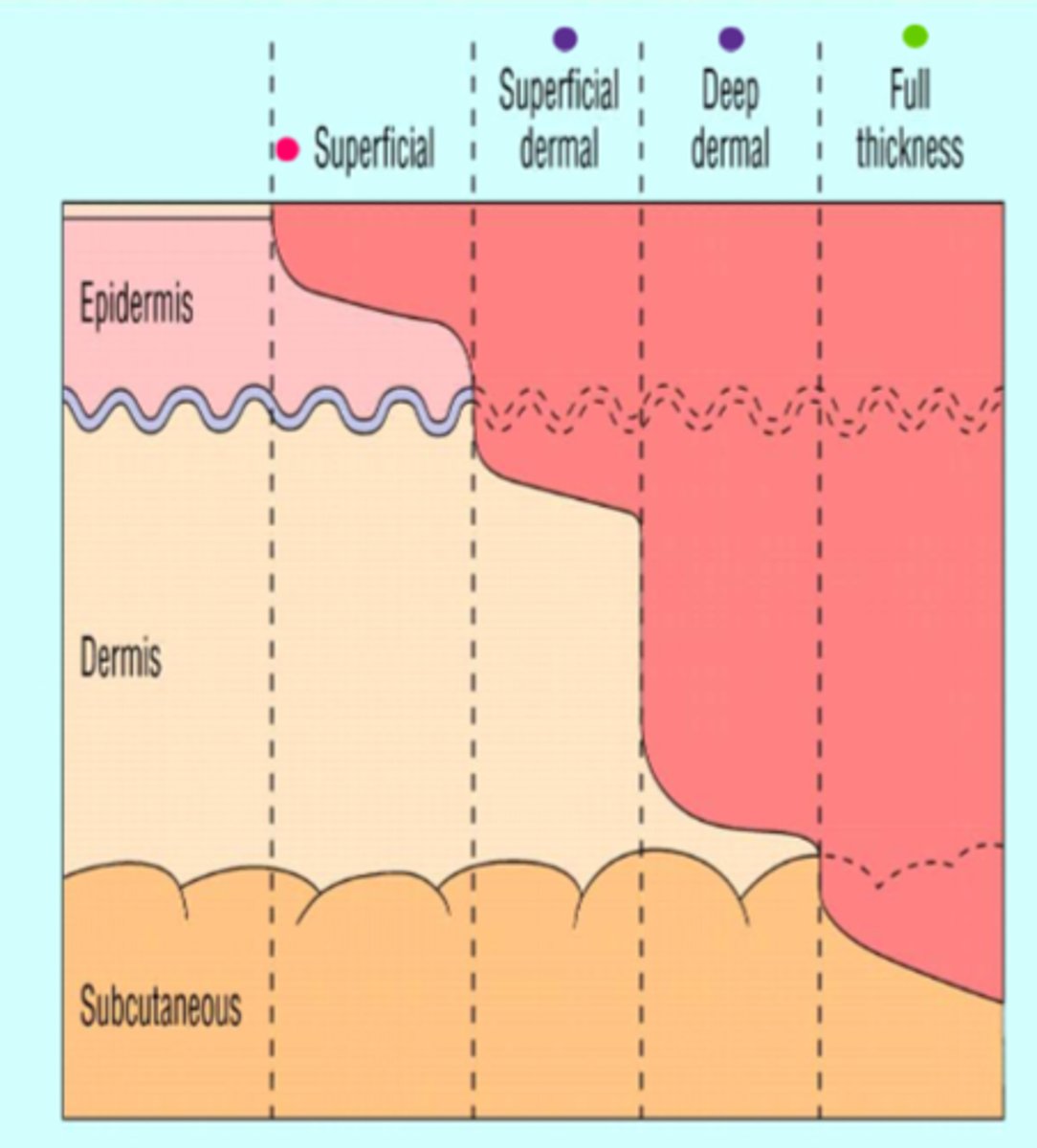
What is a 'superficial' ('epidermal') burn (1st)
- involves only the epidermis
- does not blister
- painful, dry, red (erythema) => cap refill normal
- healing time: 1 week

What is a 'partial-thickness' ('superficial dermal') burn (2nd)
- both epidermis & dermis involved
- very painful, red, weeping, blisters seen in 24 hours (between the epidermis and dermis) => cap refill normal
- healing time: up to 3 weeks

What is a 'partial-thickness' ('deep dermal') burn (2nd)
- same as superficial dermal but with more dermis involvement
- damages hair follicles & glandular tissue
- less painful, more waxy => cap refill is sluggish/absent
- healing time: up to 9 weeks (severe scarring needs grafting)
What is eschar
dead (necrotic) tissue that forms over healthy skin and then over time falls off (sheds)

What is a 'full thickness' burn (3rd)
- involves full dermis (& epidermis) + subcutaneous tissue
- no blisters; waxy to black; eschar formation ("charred surface")
- no pain, no tactile sensation, loss of function & no cap refill (needs grafting)
- no regeneration => dead tissue (eschar) needs to be debrided most likely (make sure they can maintain ABCs still post debridement!)
What is a 4th degree burn
- involves all layers of the skin + underlying structures involved => muscle, bone, joints

What do we first DO with superficial burns
- stop the burning: cool water for at least 20 minutes + cool compress (decrease vascular flow, decrease inflammation/pain)
- analgesia: NSAIDS, Tylenol, opioids; Lidocaine, Glucocorticoids or soothing lotions (eg. aloe vera)
- protect: loosely cover the burn area with a sterile bandage
- rehydration: fluids + electrolytes (eg. gatorade)

What would we use for analgesia in peds burn pts
- (IN) intranasal route => non invasive
- usually fentanyl or ketamine

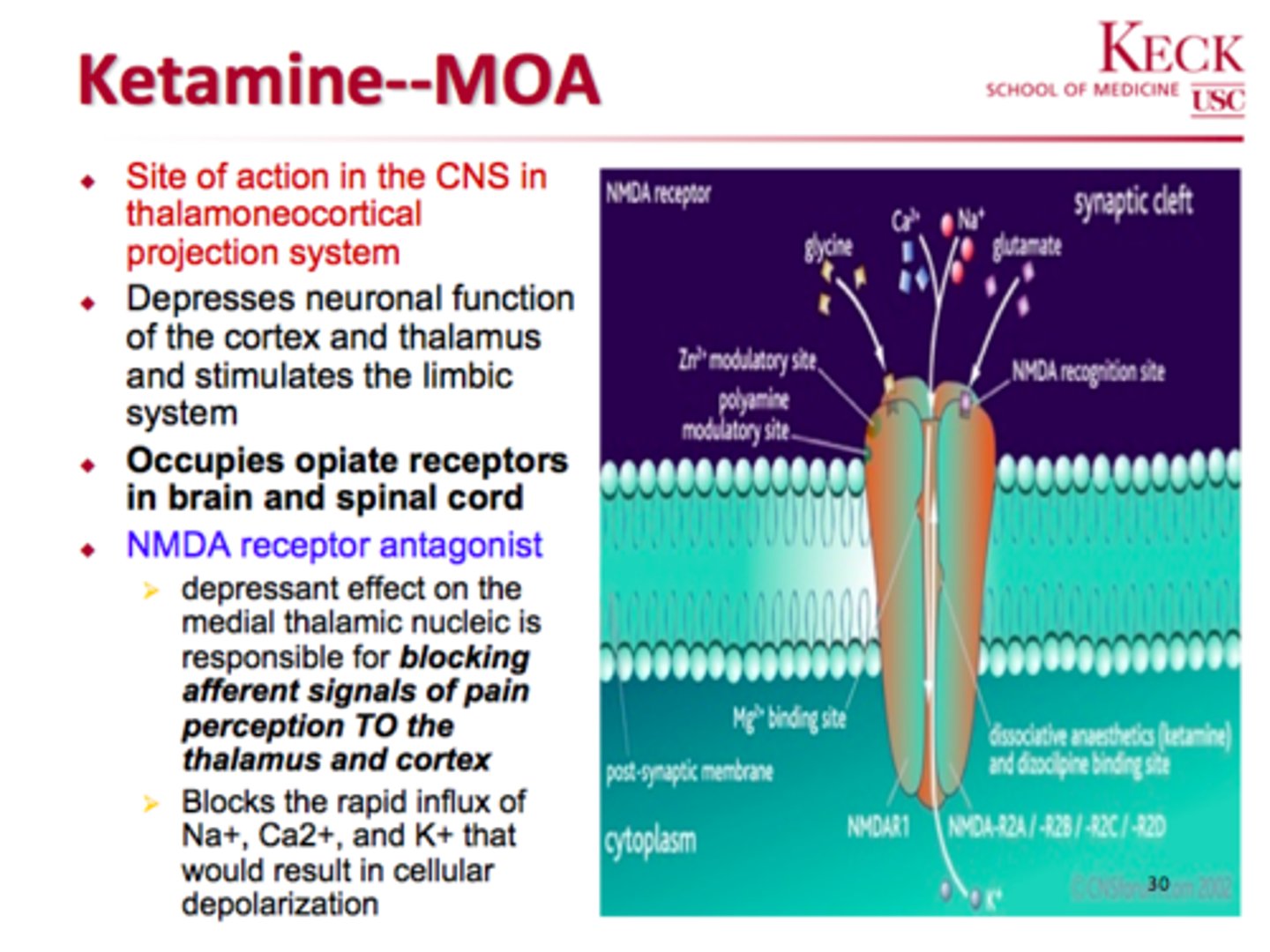
What is ketamine in regards to pain (burn tx)
- NMDA antagonist
- decreases glutamate & substance P, and therefore pain
What are the biggest DON'TS in superficial burn tx
- NO ice - further damage to the skin (causes severe vasoconstriction)
- NO butter, oils, toothpaste (fluoride) => trap heat & enhance burning

What are blisters and how do we know when to debride (pop) them
- inflated trapping of plasma (protective mechanism)
- form between the epidermis & dermis
- debridement if >6mm diameter => the bigger the blister the heavier/the more pressure on the healthy tissue (RvB)

What does white tissue indicate in a burn
- that it is WORSE, further into the dermis (will be drier/more waxy)

What are the main burn effects
- burn zone damage: direct cell membrane disruption => cell injury (necrosis of affected tissue) => inflammation, ischemia, electrolyte dysfunction, free radicals (oxidative stress)
- dehydration/hypovolemia - extent depends on severity of burn (d/t loss of plasma aka 'weeping wound (blisters), causes a loss of absolute vol & osmotic pressure)

What are the SEVERE burn effects
- massive fluid shift (edema, hypovolemia, hypoproteinemia) + stimulation of clotting & coagulation (on a larger scale)
- hemodynamic instability & coagulation
- low cellular fx: eg. insulin resistance, low immune fx
- organ dysfunction
- immune dysfunction = risk of infection/sepsis
- hypermetabolic state
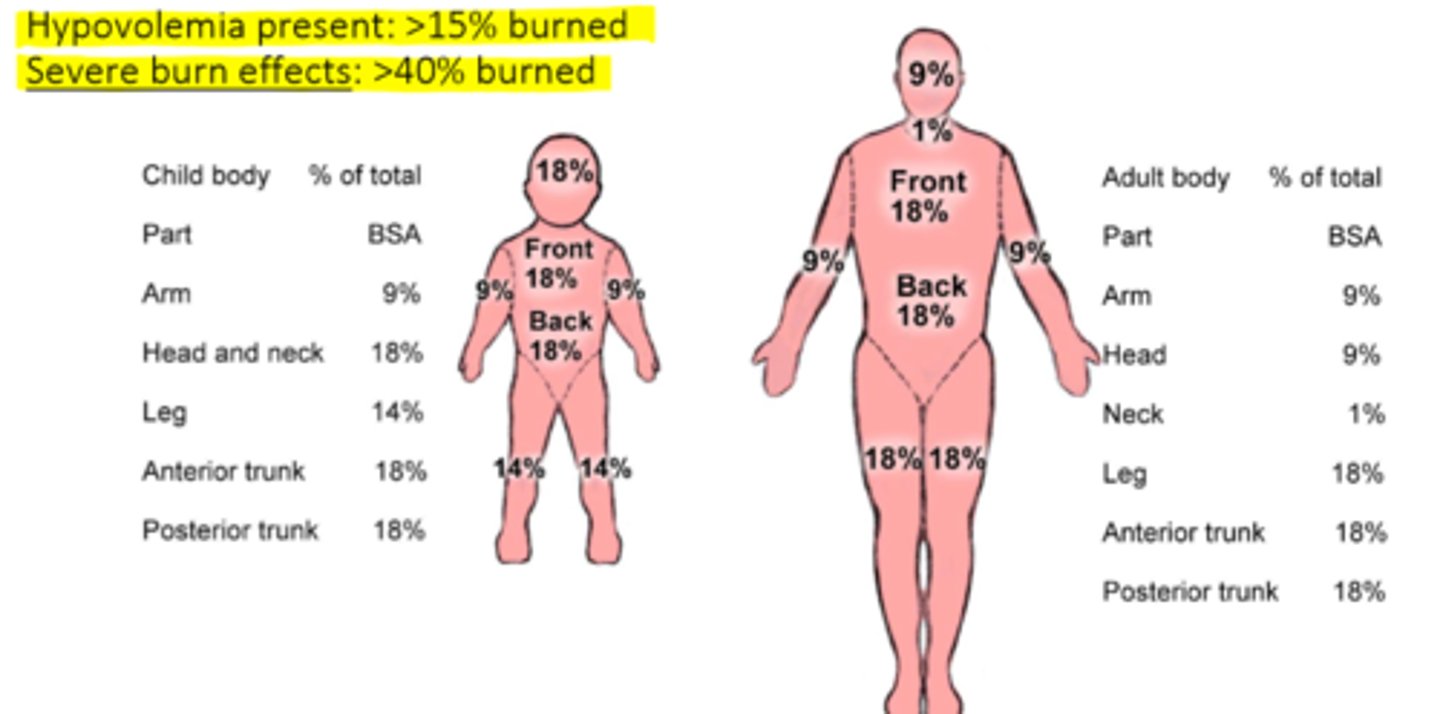
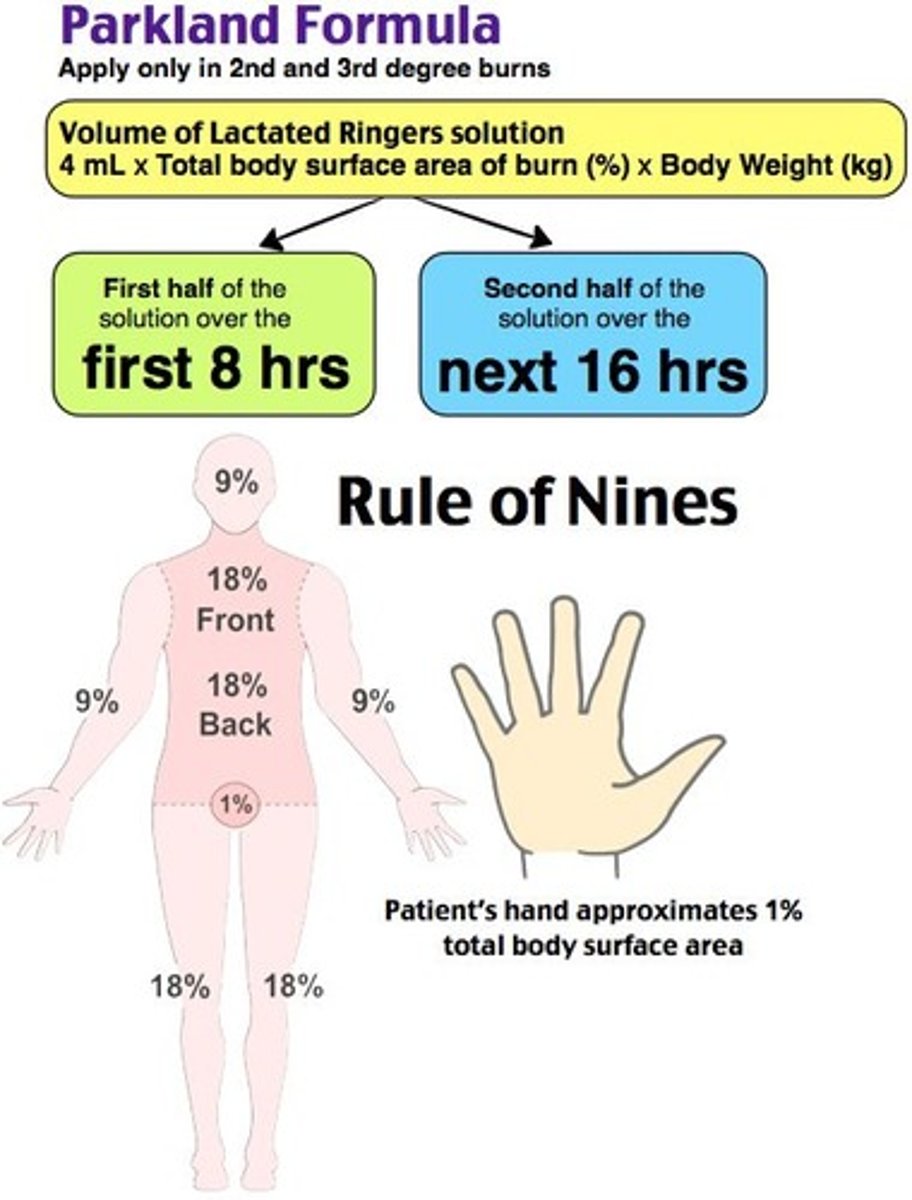
What is the 'rule of 9's'
- tells us the extent of injury in a burn (superficial burn not counted) => add up the % of burned areas on body surface and round up to determine needed fluid resuscitation (palm approximates 1%)
- hypovolemia present: >15% burned
- severe burn effects: >40% burned
When would we NOT give abx in burn pts
- PROPHYLACTICALLY without empirical evidence
- contraindicated as it can cause resistance of host flora & worsen pts condition
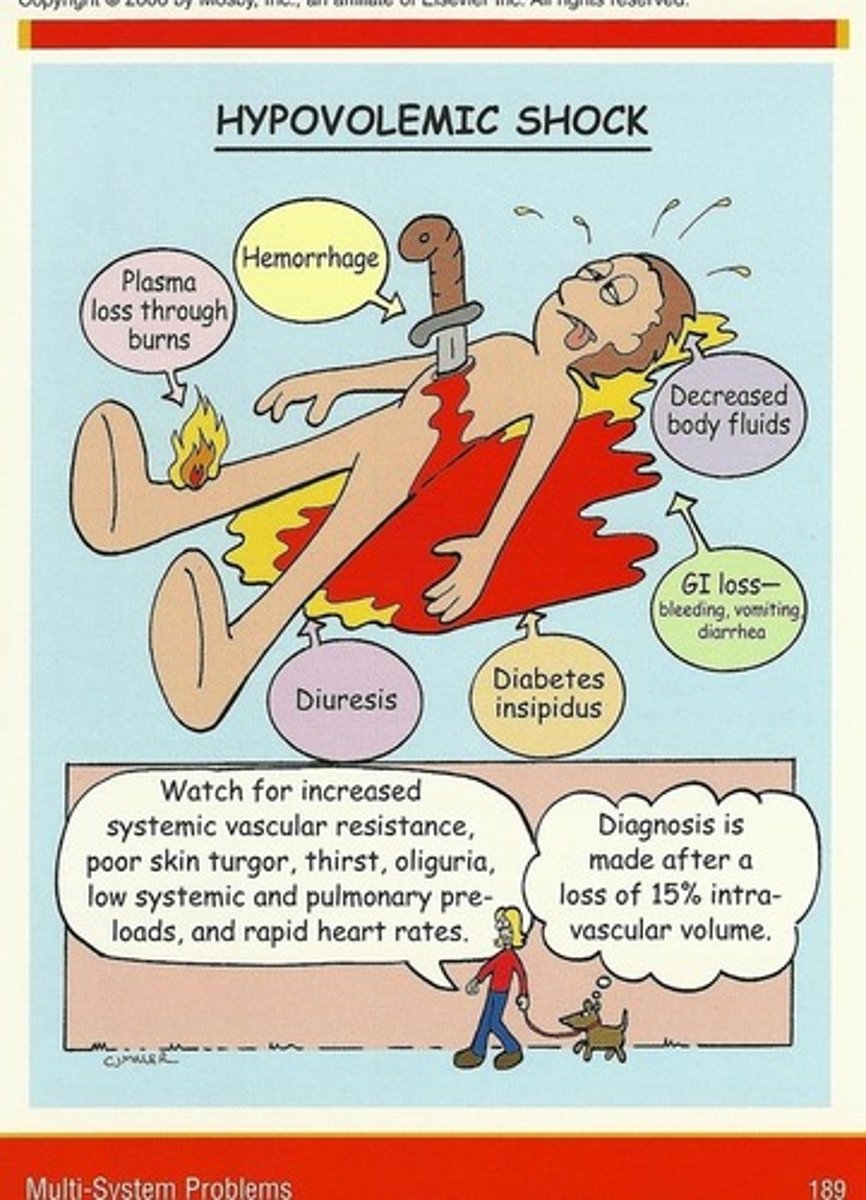
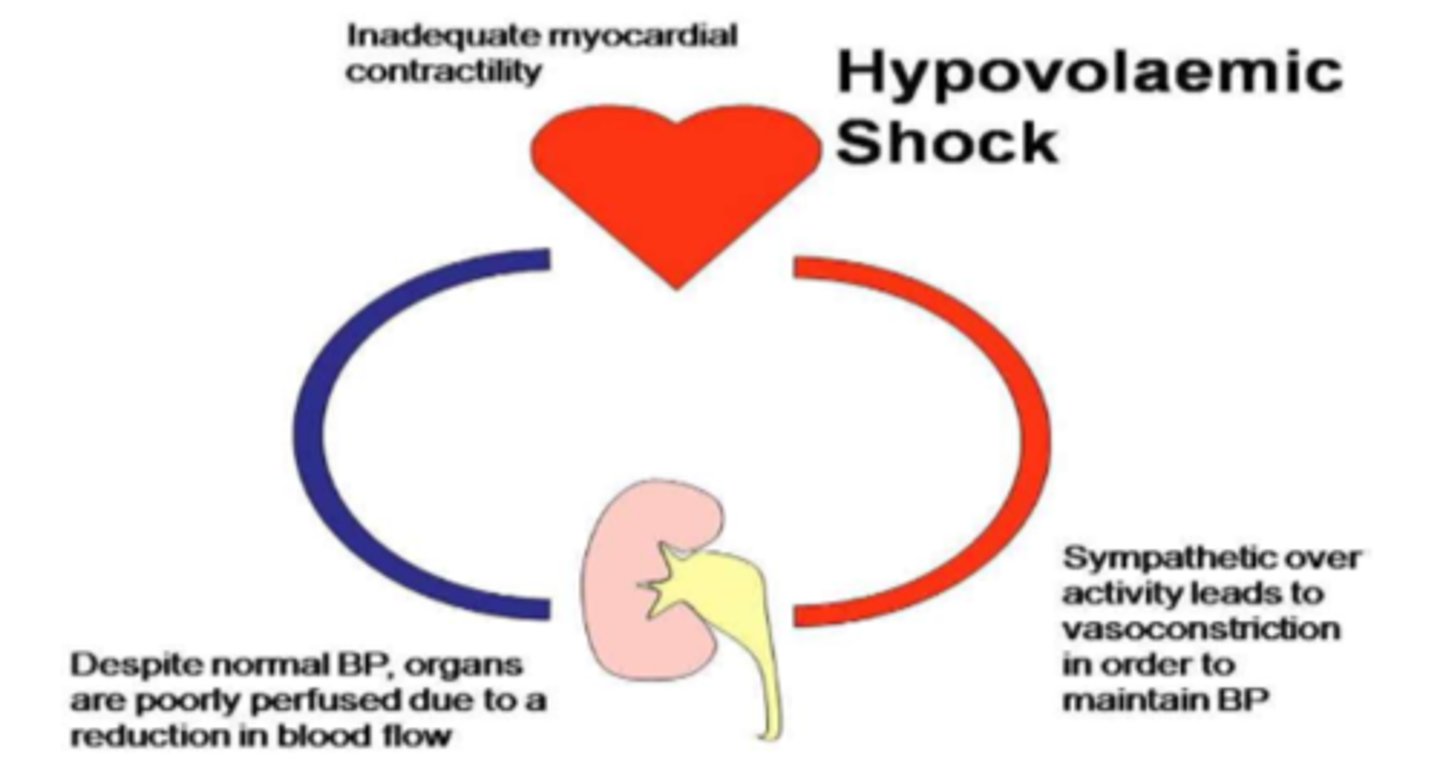
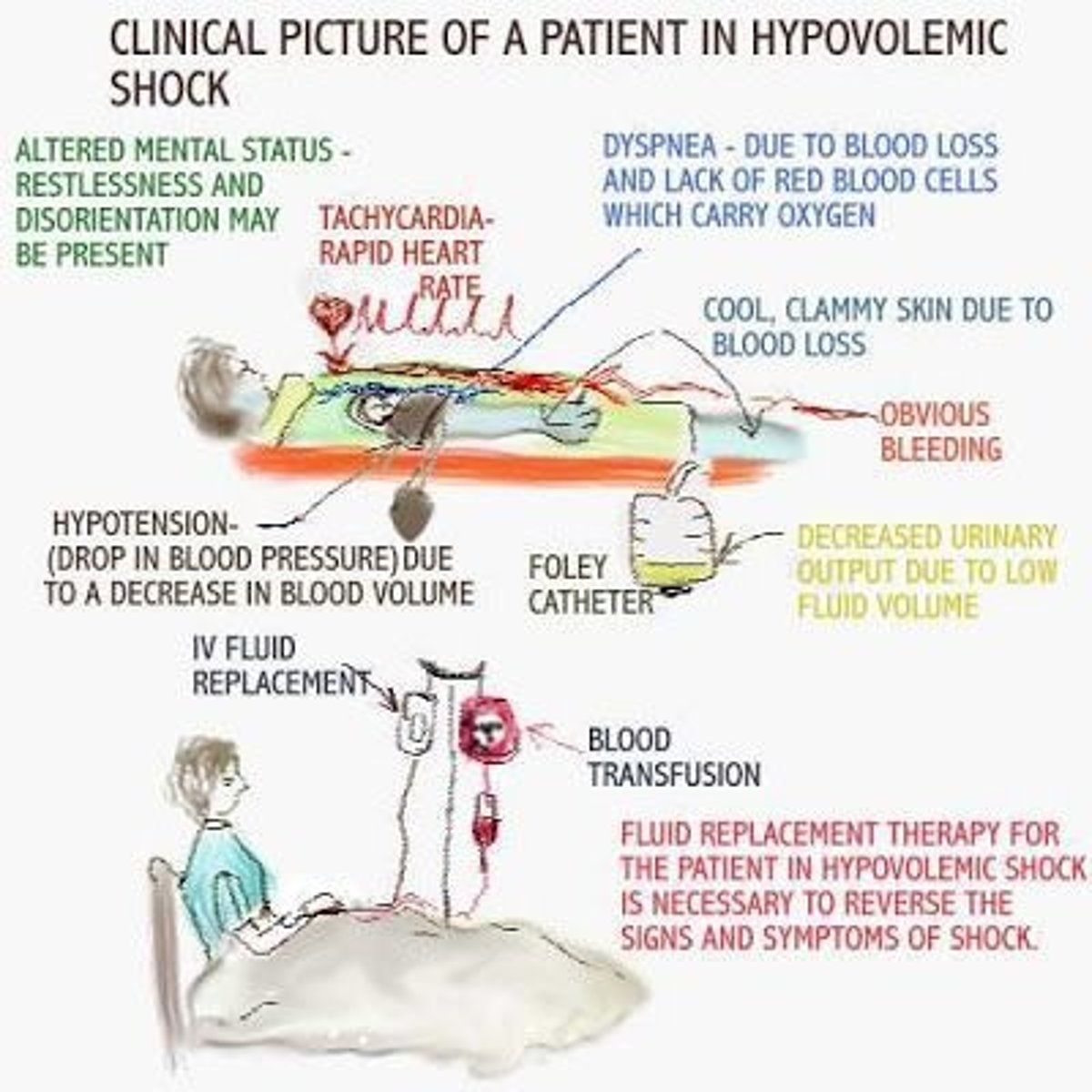
What happens the the heart & kidneys in hypovolemic shock (organ dysfunction => pt is getting worse)
- heart: inadequate myocardial contractility
- kidneys: low blood flow decreases perfusion despite normal BP => SNS over activity leads to vasoconstriction to maintain BP
What is the parkland formula
- only used in 2nd & 3rd degree burns
- vol of LR to be determined for fluid resuscitation in a burn pt
- calculation: 4 mL x total % of body surface burned (rule of 9's) x body weight in kgs
- give: 1st half of solution over the 1st 8 hours and the second half over the next 16 hours
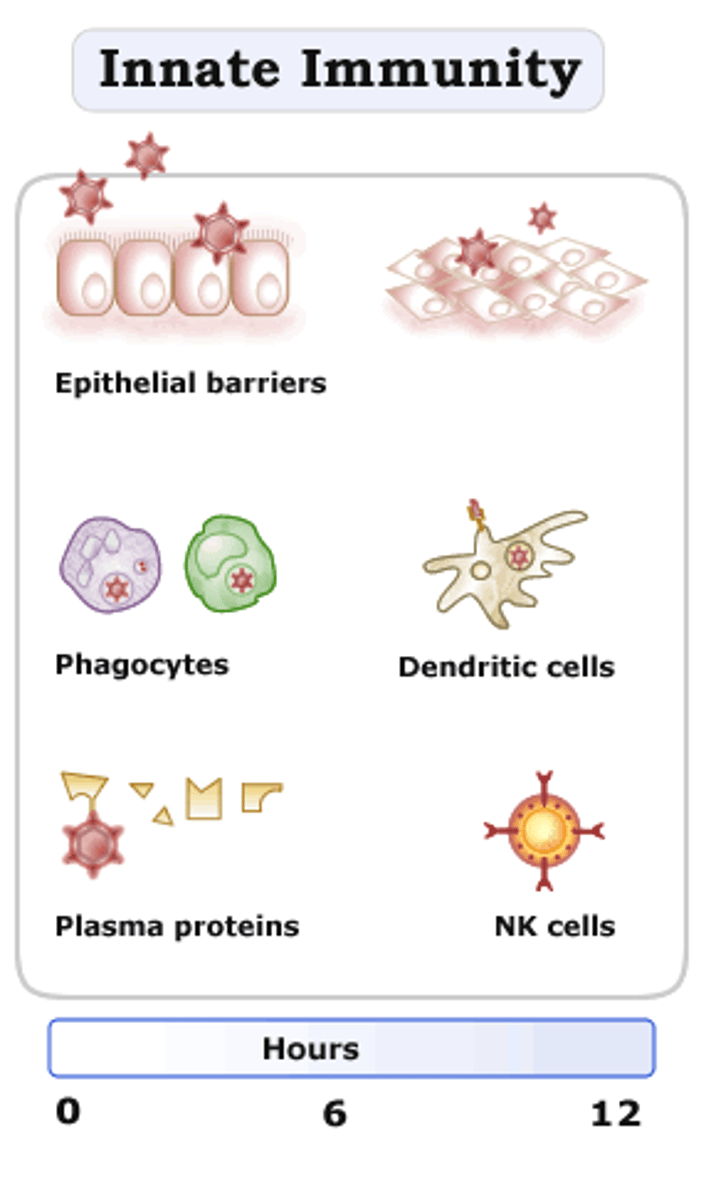
How does immune dysfunction occur in burns
- innate immunity losses: depletion & loss of WBCs & integument loss (protective layer)
=> infection risk up to 50%
What is hemodynamic instability (severe burn effect)
2 phases:
1. hypovolemic shock
2. hypermetabolic state (hypervolemic)
overall a metabolic crisis in the body!
What is the 1st phase of hemodynamic instability
hypovolemic shock:
- vascular permeability/tissue damage = loss of fluids & protein from cellular, interstitial, vascular compartments => total fluid loss
- low preload => decreased CO => organ dysfunction (eg. renals/CNS - d/t decreased organ perfusion)
***assess carefully, 2nd phase has HIGH CO!
What is the 2nd phase of hemodynamic instability
- hypermetabolic state (aka hypervolemic)
- massive overcompensation: high CO, high BMR, hyperthermia
- 24-72 hrs post-burn; lasts up to 2 years! (needing more demands for metabolic fx)
What cells are released in a hypermetabolic state (phase 2 hemodynamic instability) as an injury response
- catecholamines (NE/epi => SNS & adrenal medulla stim. causes compensation)
- cortisol (glucocorticoid from adrenal cortex => 50x higher levels than normal stress response)
- inflammatory mediators (cytokines, nitric oxide (NO), hydrogen sulfide (produced in liver in response to burn stress)
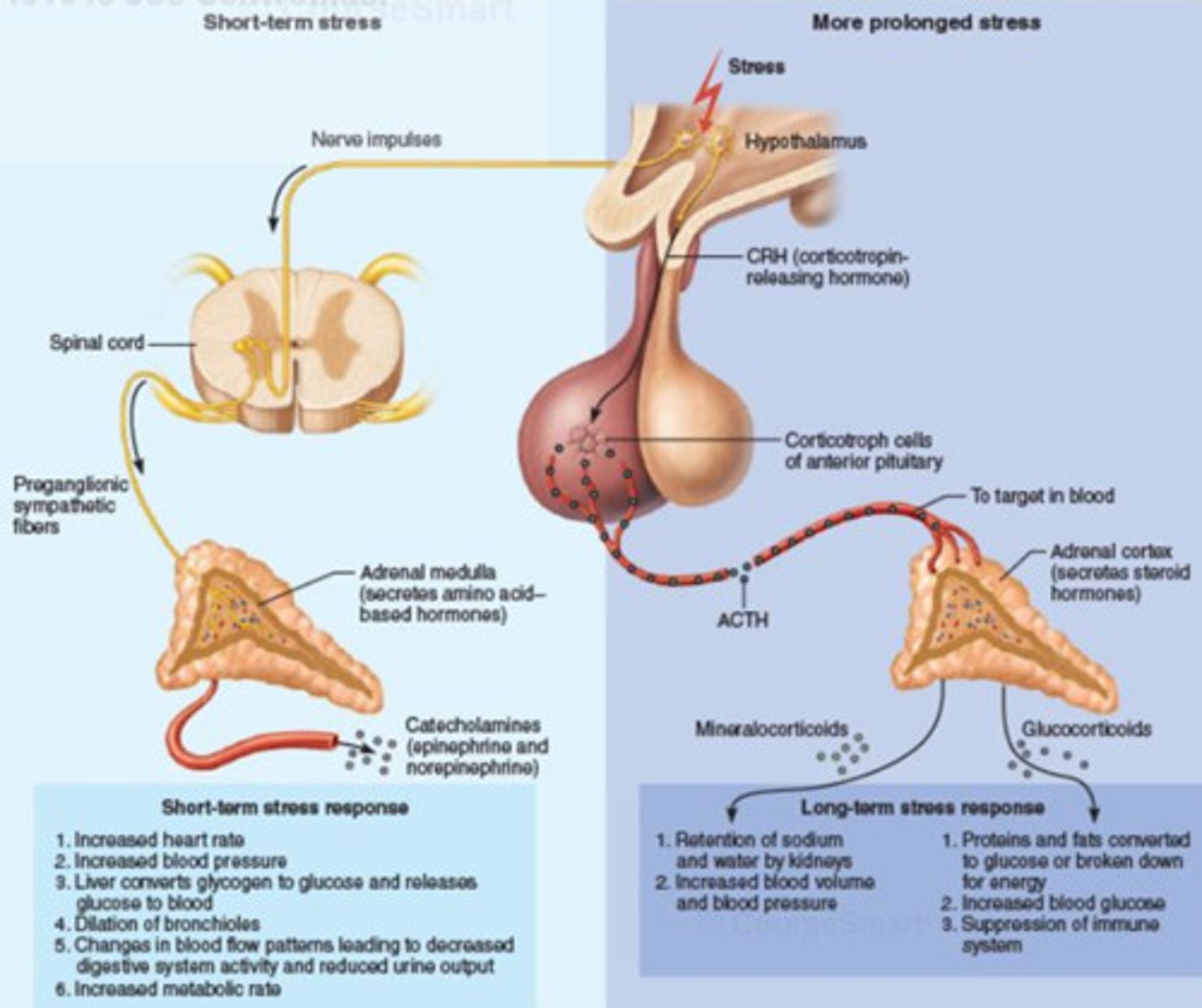
What is a 'metabolic crisis' (seen in phase 2 hemodynamic instability)
=> metabolic crisis: hyperglycemia but insulin resistance, protein catabolism; electrolyte imbalances (& therefore hypermetabolic demand)
- higher if more skeletal muscle damaged

What are the main treatment focuses in burns
- ABC's
- oxygenation: O2, intubate PRN
- analgesia: Tylenol, NSAIDs, opioids
- anxiolytics: benzodiazepines
- hemodynamic stability (need 2 IV lines)
- thermoregulation: cool the burn area
- post-acute phase: keep room warm to prevent hypothermia
- manage lactic acidosis & hyperglycemia (insulin PRN)

What IV fluids may we need for hemodynamic stability tx in burns
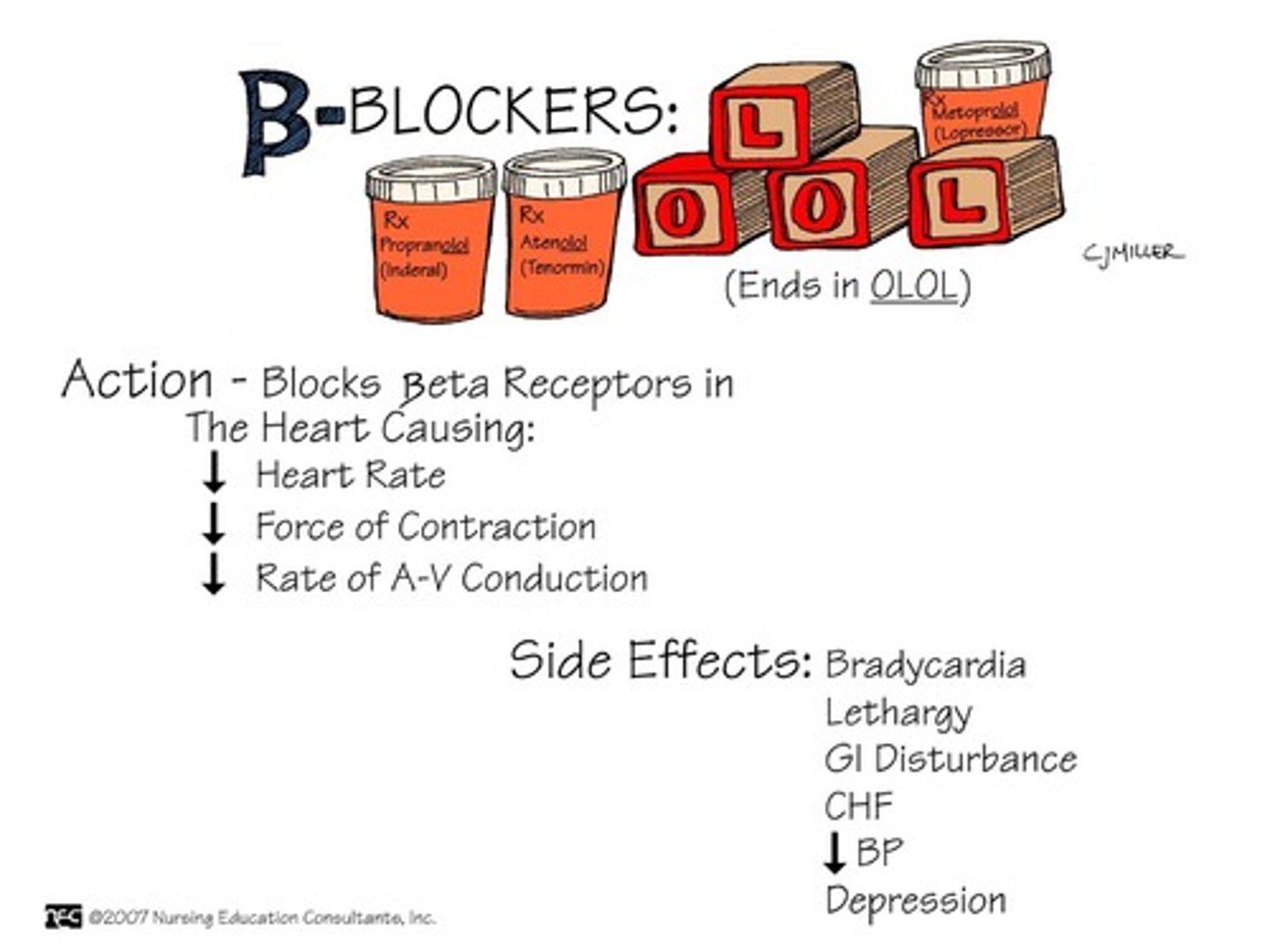
- 1st IV fluid resuscitation, cautious approach
- may need albumin replacement
- may need beta blockers (to decrease the catecholamine responses that are causing hypermetabolic fx)
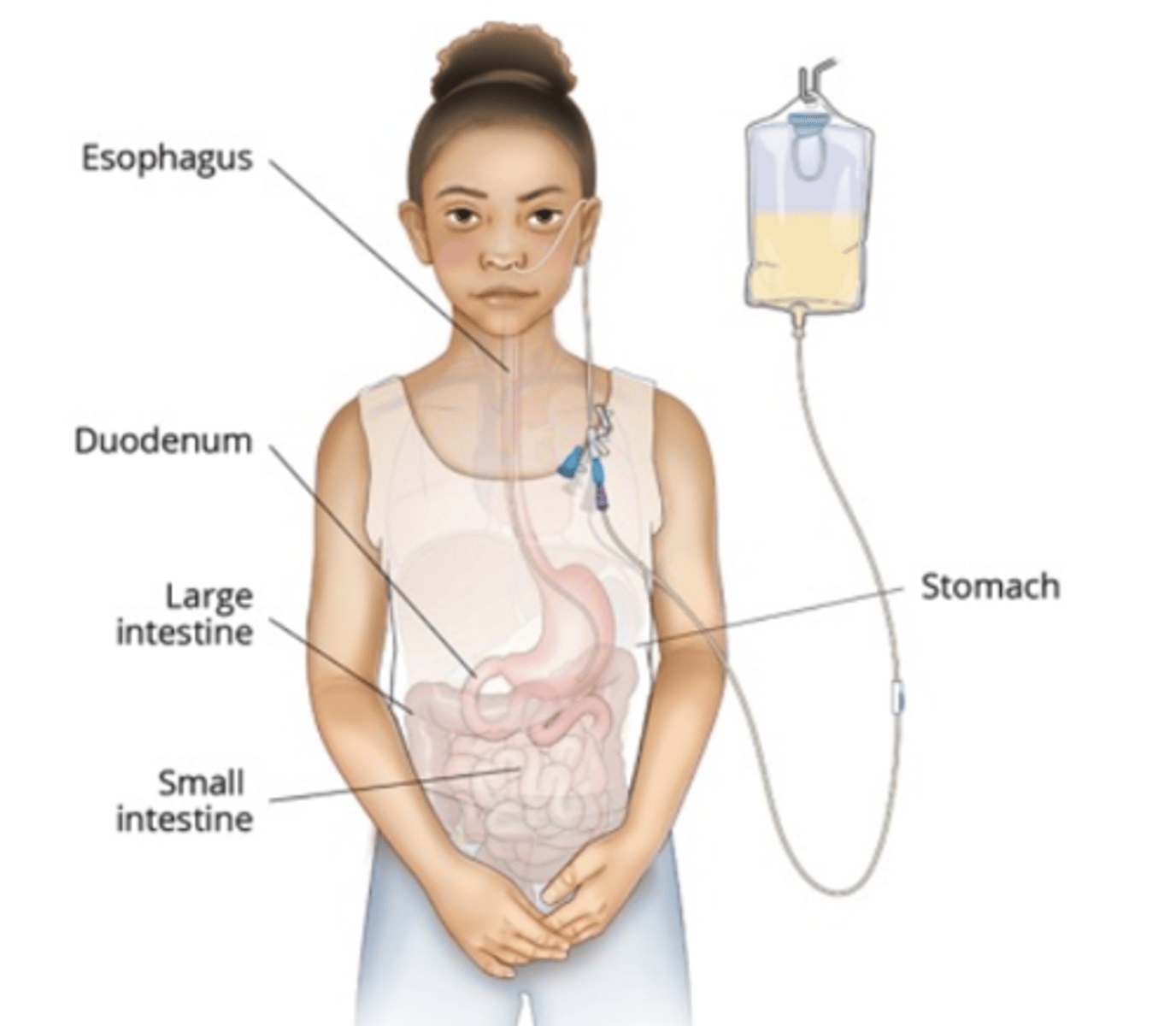
What are our adjunct treatment focuses in burn pts (alongside meds)
- nutrition: enteral feeds (protein demands at 50% above normal (normal: 1g/kg))
- prevent infection (sterile dressings, isolation)
- eschar removal (excision, escharotomy) => excision decreases hypermetabolic state; wound grafting ASAP
- manage long term hormonal imbalance (exhausted by hypermetabolic response) (eg. growth hormone, testosterone)
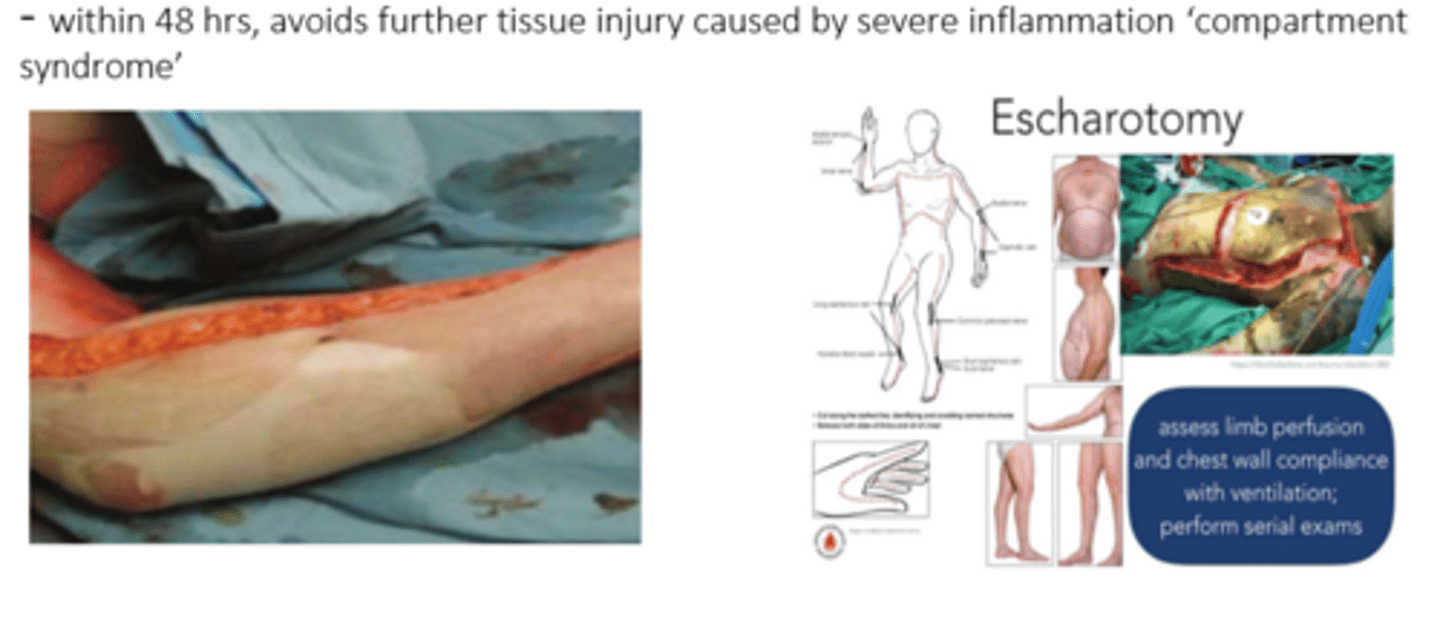
What is an escharotomy
- incision into eschar/necrotic tissue, opening it up to alleviate pressure caused by inflammation
- helps pt still maintain fx
- done within 48 hrs of onset, avoids further tissue injury caused by severe inflammation aka 'compartment syndrome' (painful condition d/t high pressure)
How can a burn occur in an inhalation injury
- direct burn = poisoning
- cyanide: high incidence of cyanide toxicity in house fires => formed by incomplete combustion of nitrogen in burning plastics, vinyl
- cytotoxic = blocks cellular respiration

What do we look for in an electrical burn
- exit wound treatment & address electrical abnormalities within the pts body to tx eg:
- arrhythmia tx (eg. Vfib) or seizure tx (put pt on an ECG)
