Overview of Eye Diseases and Related Conditions
1/423
Earn XP
Description and Tags
Medical condition: OT622
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
424 Terms
What percentage of all learning occurs through the visual channel?
80-90%
What percentage of sensory information supplied to the CNS is visual?
90%
What are the contributions of vision to occupational performance?
Anticipates/plans, drives decision making, interprets social interactions, supplies speed in info processing, dictates motor actions, and serves as an early warning system for postural control.
What are common causes of visual impairment?
Disease, trauma, aging, or a combination of any or all of the above.
What are the three jobs of the anterior visual system?
1. Focus the image on the retina, 2. Capture the image (encode it), 3. Transmit the image to the CNS.
What are common types of refractive disorders?
Myopia (near-sightedness), hyperopia (far-sightedness), astigmatism.
How can refractive disorders be corrected?
With lenses or surgery.
What percentage of the total refractive power of the eye is provided by the cornea?
Almost 70%.
What must the cornea maintain to contribute to refraction?
It must remain transparent and smooth.
What is the treatment for corneal disorders?
Corneal transplant and contact lenses.
What is the success rate of corneal transplants?
95% success rate as long as scar formation can be prevented.
What is a cataract?
Opacity in the lens that interferes with light transmission.
What is the most common cause of age-related vision loss in the world?
Cataracts.
What are the primary causes of cataracts?
Congenital, infection, severe malnutrition, diabetes, trauma, aging.
What percentage of people aged 64-74 have cataracts?
50%.
What percentage of people diagnosed over age 75 have cataracts?
70%.
What is the most common surgical procedure covered by Medicare?
Cataract surgery.
What percentage of persons undergoing cataract surgery have improved vision?
90%.
What is retinopathy of prematurity (ROP)?
Abnormal proliferation of blood vessels unique to pre-term infants.
What are the primary risk factors for ROP?
Prematurity and low birth weight.
What is the incidence of ROP in babies weighing 1.1-1.65 pounds?
Almost 100%.
What is retinitis pigmentosa?
A group of inherited diseases causing slow degenerative changes in receptor cells.
What is the pathogenesis of retinitis pigmentosa?
Rod cells are slowly destroyed, beginning mid-periphery and progressing both centrally and peripherally.
What is the rate of decline in vision for retinitis pigmentosa?
5% decline each year.
What are the two types of diabetic retinopathy?
Non-proliferative and proliferative.
What characterizes non-proliferative diabetic retinopathy?
Confined to the retina, may not cause significant visual impairment, characterized by dot and blot hemorrhages, macular edema, and scattered scotomas.
What is macular edema?
When fluid accumulates in the retina, usually the primary cause of visual impairment.
What is the pathogenesis of proliferative diabetic retinopathy?
New blood vessels grow along the retina's surface and into the vitreous, which can rupture and bleed, preventing light from passing and potentially causing retinal detachment.
What disease process attacks cone retinal cells in the macula?
Age-Related Macular Degeneration.
What are the two types of age-related macular degeneration?
Wet (exudative) and dry.
What are common symptoms of both dry and wet macular degeneration?
Macular scotomas, photophobia, fluctuating vision, and slow dark/light adaptation.
What lifestyle factors increase the risk of Age-related Macular Degeneration (AMD)?
Excessive smoking, vaping, alcohol consumption, high-fat diet, UV ray exposure, Caucasian race, fair skin, light-colored eyes, and heredity.
What is the pathogenesis of dry macular degeneration?
Gradual destruction of cone and rod cells.
How does the progression of dry macular degeneration compare to wet macular degeneration?
Dry macular degeneration progresses gradually and is not as severe as wet macular degeneration, often remaining unilateral for many years.
What is a potential precursor to wet macular degeneration?
Dry macular degeneration.
What characterizes wet macular degeneration?
It is an aggressive form of the disease that can cause vision loss overnight and is usually bilateral.
What is known about the cause or trigger of wet macular degeneration?
The cause or trigger is UNKNOWN.
What is glaucoma and where does it start?
Glaucoma is a disease of the optic nerve that starts in the anterior chamber of the eye.
How does glaucoma develop?
The notes do not provide specific details on how glaucoma develops.
What causes increases in intraocular pressure (IOP) in glaucoma?
A build-up of aqueous humor in the anterior chamber.
What is the only outlet for pressure in the eye?
The optic disc.
What happens to blood flow in the optic nerve due to increased IOP?
It decreases blood flow to the nerve.
What can permanent damage to the optic nerve lead to?
Blindness.
What are the risk factors for glaucoma?
Age 40 and older, family history, diabetes, myopia, race, and corticosteroid use in sensitive individuals.
Where does visual field loss begin in persons with glaucoma?
In the peripheral field.
What type of visual defect develops in the macula as glaucoma progresses?
A pie-shaped scotoma.
How aware are individuals of their glaucoma condition until significant damage occurs?
They are generally unaware until the macular scotoma develops.
What is a critical preventive measure for those at risk for glaucoma?
Routine eye exams after age 40.
What is the primary treatment for glaucoma?
Eye drops.
What is cortical visual impairment (CVI)?
A decreased visual response due to a neurological problem affecting the visual part of the brain.
What visual characteristics are common in children with CVI?
Preference for specific colors, movement or positional-based vision, visual latency, and difficulty with complex vision.
What is nystagmus?
Involuntary, rhythmical, repeated movement of one or both eyes.
What types of nystagmus can occur?
Horizontal, vertical, or torsional.
What visual issue does nystagmus cause?
Reduced visual acuity due to poor gaze stability.
What is the null point in relation to nystagmus?
An area of reduced eye movement and improved visual acuity.
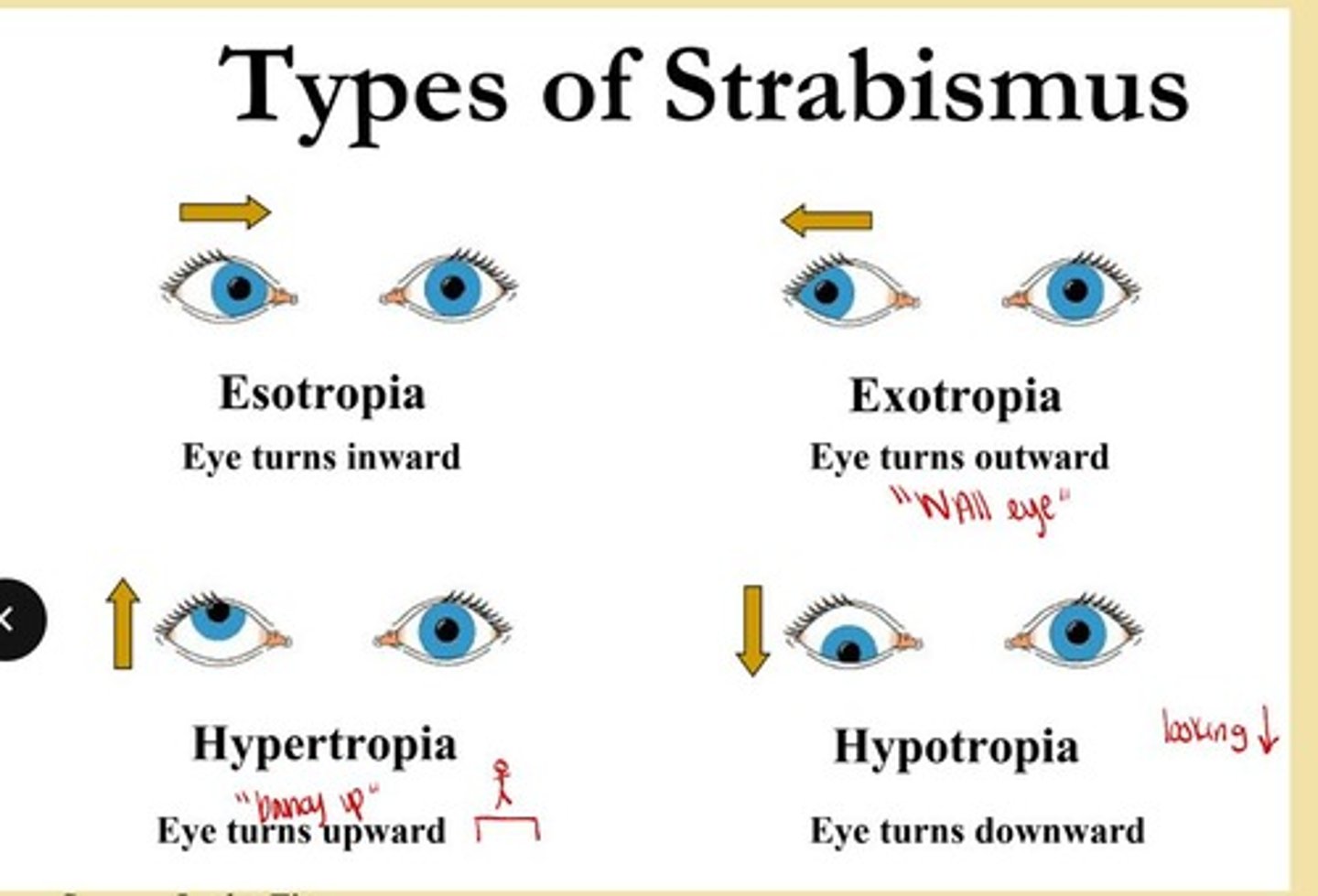
What is strabismus?
Unequal eye muscles leading to misalignment of the eyes.
What are two forms of strabismus?
Phoria and tropia.
What condition can strabismus lead to?
Amblyopia.
What is sensory suppression in children with amblyopia?
The CNS shuts down the image from one eye to eliminate double vision.
What is dysphagia?
Difficulty with swallowing or the inability to swallow.
What is the bolus in the context of swallowing?
A round mass of food prepared for swallowing by chewing.
What are some common etiologies of dysphagia?
Stroke, traumatic brain injury, progressive neurological diseases, high-level spinal cord injury, brain tumors, and cancer.
What cognitive issues can affect swallowing?
Decreased attention and self-monitoring.
What are the phases of swallowing?
Voluntary and involuntary actions involved in the process of swallowing.
What happens when new blood vessels rupture in the eye?
They bleed into the vitreous, collecting blood and preventing light from passing.
What condition can result from degenerating blood products in the eye?
It can cause contraction of the vitreous and formation of fibrous tissue, leading to retinal detachment.
What does age-related macular degeneration (AMD) primarily affect?
It attacks cone retinal cells in the macula.
What are the two types of age-related macular degeneration?
Wet (exudative) and Dry (atrophic or senile).
What common symptoms do both types of age-related macular degeneration cause?
Macular scotomas, photophobia, fluctuating vision, and slow dark/light adaptation.
What are some risk factors for age-related macular degeneration?
Excessive smoking, high-fat diet, UV ray exposure, Caucasian race, fair skin, light-colored eyes, and heredity.
What characterizes dry macular degeneration?
Gradual destruction of cone and rod cells, often unilateral for many years, and may be a precursor to wet macular degeneration.
What is a significant risk of wet macular degeneration?
It can cause vision loss overnight and is usually bilateral.
How does glaucoma develop?
It develops from increases in intraocular pressure (IOP) due to a build-up of aqueous humor in the anterior chamber.
What is the consequence of increased pressure in glaucoma?
It causes permanent damage to the optic nerve.
What are some risk factors for glaucoma?
Being 40 years or older, family history, diabetes, myopia, race, and corticosteroid use.
What visual field loss occurs in glaucoma?
Visual field loss starts in the peripheral field, developing into a pie-shaped scotoma.
How do individuals with glaucoma typically perceive their condition?
They are generally unaware until significant damage has occurred.
What are some characteristics of children with CVI?
Preference for specific colors, movement-based vision, visual latency, and difficulty with complex vision.
What is nystagmus?
Involuntary, rhythmical movement of one or both eyes, which can be horizontal, vertical, or torsional.
What is the impact of nystagmus on vision?
It reduces visual acuity due to poor gaze stability, causing blurry vision.
What is strabismus?
A condition characterized by unequal eye muscles, leading to misalignment of the eyes.
What are the two forms of strabismus?
Phoria (deviation held in check by fusion) and tropia (observable constant deviation).
What is amblyopia?
Functional blindness in the central field created by sensory suppression, often seen in children with reading issues.
What is dysphagia?
Difficulty with swallowing or the inability to swallow, affecting the safe passage of food from the oral cavity to the stomach.
What is the role of cognition in swallowing?
Cognition affects attention, self-monitoring, and the ability to take appropriate bolus sizes and speeds during mealtime.
What are the phases of swallowing?
The phases include oral preparation, oral transit, pharyngeal phase, and esophageal phase.
What is a bolus in the context of swallowing?
A round mass of food prepared for swallowing by chewing.
What is the sulcus in relation to swallowing?
A groove or furrow between the jaw and cheek that aids in the swallowing process.
What is the first phase of swallowing and what occurs during it?
The first phase is the anticipatory phase, which begins before the client enters the dining area and includes the client's expectations of the eating experience, appetite or hunger level, sensory qualities of food, motivation to eat, and cognitive awareness.
What happens during the oral preparatory phase of swallowing?
Food is masticated by the lips, cheeks, and tongue, forming a bolus, while visual and olfactory information stimulates the salivary glands.
What initiates the swallowing process in the oral phase?
The tongue initiates the movement of the bolus toward the pharynx, marking the beginning of swallowing.
What are the key components of the pharyngeal phase of swallowing?
This phase involves both voluntary and involuntary components and marks the beginning of the involuntary portion of the swallowing process as the bolus moves past the base of the tongue.
What occurs during the esophageal phase of swallowing?
When the bolus enters the esophagus, esophageal muscles contract and move the bolus through peristaltic wave contractions, taking 8-20 seconds.
What are some indicators of eating and swallowing dysfunction?
Indicators include difficulty bringing food to the mouth, forming a bolus, keeping food/liquid in the mouth, coughing before, during, or after swallowing, a wet/gurgling voice after eating, loss of appetite, pain when swallowing, difficulty breathing while eating, and a weak cough.
What should be included in a medical chart review for eating and swallowing assessment?
Medical diagnosis, history, previous aspiration or pneumonia, medications, hydration and nutrition, nasogastric tube (NG tube), and gastrostomy (G tube).
Why is understanding a client's occupational profile important in swallowing assessment?
Knowing prior habits and routines and the importance of eating to the client and family helps in determining interventions that will meet the client's needs while considering cultural values and beliefs.
What does the outer oral status assessment evaluate?
It evaluates sensation (drooling, food on lips), musculature (strength, movement, tone), and oral reflexes (absence or impairment that can interfere with safe swallowing).
What is assessed in the intraoral status during an oral assessment?
Condition and quality of teeth/gums (dentition) and the strength, range of motion, control, and tone of the tongue.
What is the role of the epiglottis during swallowing?
The epiglottis acts as a movable lid that covers the windpipe to prevent food from entering it.
What happens to the bolus during phase two of swallowing?
The bolus stimulates receptors at the back of the throat, the tongue prevents it from going back into the mouth, and the back of the throat moves to block the airway from the nose.