Lumbar Assessment and Treatments
1/17
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
18 Terms
Flexion PPIVM
Purpose: Determine pain and movement of a level
Patient: Side lying Therapist: Stand in front of at the level of the pelvis, cradling the patient’s knees on upper thigh/groin region.
Sensing Hand between the spinous processes of the motion segment being assessed
Technique Move pelvis towards the patient’s stomach so that the patient’s lumbar spine flexes. This is usually repeated 2-3 times at each segment in an oscillatory fashion.
Extension PPIVM
Purpose: Determine pain and movement of a level
Patient: Side lying Therapist: Stand in front of at the level of the pelvis, cradling the patient’s knees on upper thigh/groin region
Sensing Hand between the spinous processes of the motion segment being assessed
Technique Apply pressure through the legs and pelvis so that the patient’s lumbar spine extends. This is usually repeated 2-3 times at each segment in an oscillatory fashion.
Side Flexion PPIVM
Purpose: Determine pain and movement of a level
Patient: Side lying with hips approx. 90 degree
Therapist: Stand in front of at the level of the pelvis, cradling the patient’s knees on upper thigh
Sensing Hand between the spinous processes of the motion segment being assessed
Technique lean backwards and lift the patient’s ankles towards the ceiling so that the patient’s lumbar spine side flexes. This is usually repeated 2-3 times at each segment in an oscillatory fashion.
Rotation PPIVM
Similar set-up can be applied for lumbar rotation, which can be used as assessment or treatment
PAIVMs- Central PA
Purpose To determine resistance to movement and pain of motion segment
Patient Position Prone lying (pillow under stomach if prone position is uncomfortable)
Therapist Position Stand alongside the patient at the level of the thoracic spine
Hand Placement There are two different hand placements used commonly for this test: 1. Contact is made with the spinous process via the ulnar border or thenar eminence. 2. Contact is made over both transverse processes by the therapist using the index and middle fingers of one hand (so that the patient’s SP lies between the two fingers). These fingers are then covered by the ulnar border of the therapist’s other hand.
Technique The therapist leans their body weight (through extended elbows) so that a pure posterior to anterior motion is applied to the SP Load is progressively increased from a Grade I to a Grade III This is usually repeated 2-3 times at each segment in an oscillatory fashion The therapist notes resistance to movement and any pain response
PAIVMs- Unilateral PA (rotation)
As above for central PA, with therapist using either thumbs or ulnar border of the thenar eminence to apply force over the transverse process.
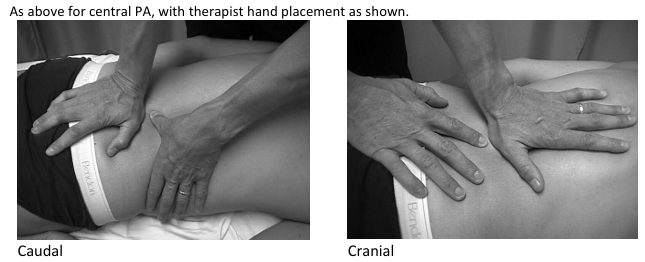
PAIVMa- Caudal / Cranial Glides
McKenzie Therapy- Postural Syndrome
Postural syndrome
Pain related to postures
Treat by correcting postures
McKenzie Therapy- Dysfunction Syndrome
Pain related to joint stiffness
Treat by improving range of stiff joints
McKenzie Therapy- Derangement Syndrome
Centralization / Peripheralization response to repeated movements
May present with flexion deformity or lateral shift
Treat with the movement direction that centralizes symptoms
Repeated Movement Assessment and Treatment:
Indication:
Suspected derangement syndrome (disc-related problem) To assist classification into correct McKenzie syndrome
Procedure:
Following usual active / passive movements -
Ensure you have a detailed baseline map of resting symptoms objective asterisk signs to re-assess (e.g., standing posture, flexion range and pain)
Guide repeated movement e.g., side-glide in standing X 10 e.g., extension in prone X 10 Re-assess resting symptoms (looking for centralization or peripheralization) and objective asterisk signs.
If improves with the chosen direction of repeated movement, consider repeating as treatment.
Generally treat a lateral component before a sagittal component
Lumbar Instability
Remember that joint instability can be:
Structural: Reduced passive stabilization of a joint (bony / ligamentous), e.g., spondylolysthesis
Functional: Reduced active (neuromotor) ability to control joint mobility
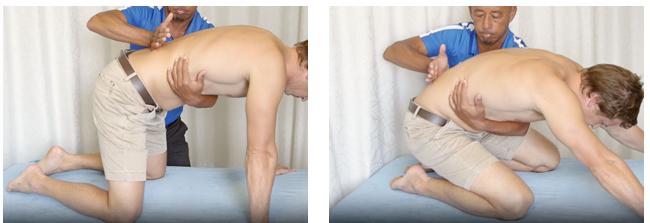
SNAG flexion in four-point kneeling
Apply glide cephalad at the spinous process (or unilaterally) using the hypothenar eminence
Traction
Purpose:
A ‘trial treatment’ to increase ROM and decrease pain associated with movement but also to help determine irritability
Technique:
The therapist gently leans backwards to apply a traction force to the patient’s lumbar spine via the legs. Load should be applied gently and progressively while monitoring pain response. Initially apply a small load, the release slowly and ask how the patient feels. If the patient is comfortable, reapply the load and add a little more. Hold for a few seconds, release slowly and re-evaluate
Beware:
Many patients get relief from the application of traction but have a significant increase in pain on its release. For this reason, you must apply and release load progressively as described above. If the patient reports pain with gentle traction... do not apply stronger forces.
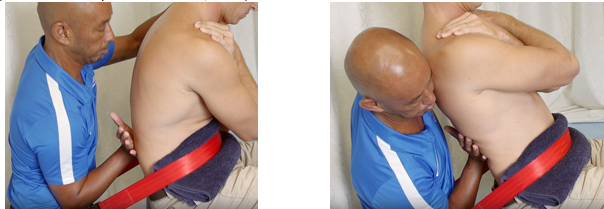
SNAG extension (flexion) in sitting
Seatbelt over ASIS
Apply glide cephalad at the spinous process (or unilaterally) using the hypothenar eminence.
Mobility Exercise Examples
Rotation: supine leg rotation progressions to sideling
Flexion: side lying / supine curling, 4pt kneel pelvic rocking
Lateral flexion: standing ITB/ Thoracolumbar fascia stretch
Extension: prone / standing
Isolation Exercise
Transversus Abdominis
Patient position: Crook lying with fingertips placed medial to the Anterior Superior Iliac Spine (ASIS) for tactile cueing and feedback. 4pt kneel, pone, standing positions can also be used
Gently draw the lower part of the abdomen away from top seam of the pants
Co-contraction with the pelvic floor can be used for facilitation. Instruct the patient to activate the pelvic floor, then gently also draw in the lower stomach. Use caution and avoid stopping urine flow, as it can lead to dysfunctional sphincter control
The therapist should feel gentle tone medial to the ASIS and breathing should not be disrupted. Dosage: Typically, 10 X 10 seconds is used for training, but prescription is based on the individual’s specific needs and progression ability
Integration exercise examples
Bird-Dog
Four-Point Kneeling on hand and knees
Modify by using higher surface or by performing it in standing if 4pt kneel is not tolerated
Patient extends the opposite arm and leg (the arm in front and the leg behind) whilst maintaining control of the lumbopelvic, head and scapula
This exercise can be progressed by having different surface for balance. Lumbar sitting posture correction
4pt kneel differentiation of F/E in different spinal regions
Alternating arm pulls with theraband
Hydrotherapy - arm movements maintaining thoracic neutral