Lecture 4: Principles of Adaptive Immunity
1/71
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
72 Terms
adaptive immunity
the response of antigen-specific lymphocytes (T cells and B cells) to antigen, including the development of immunological memory
features of adaptive immunity
acquired
highly specific and efficent
long lasting memory cells
increases recognition of pathogens by innate immune system
innate vs adaptive: speed of response
innate: immediate response
adaptive: gradual response
innate vs adaptive: specificity
innate: targets a group of pathogens with common patterns
adaptive: targets specific pathogens
innate vs adaptive: memory
innate: no memory
adaptive: has memory
innate vs adaptive: maximum response
innate: immediate maximum response
adaptive: lag between exposure and the maximum response
advantages of adaptive immunity
precise: targets small differences in pathogens
memory: B & T cells are retained for a quicker response in case of recurrent infection
adapts: keeps pace with rapidly evolving organisms
cell mediated immunity (CMI) pathogen
targets intracellular pathogens (viruses)
cell mediated immunity (CMI) mediator
mediated by cytotoxic C cells
cell mediated immunity (CMI) transferability
not transferable
humoral immunity (HI) pathogen
targets extracellular pathogens (bacteria)
humoral immunity (HI) mediator
antibody mediated
humoral immunity (HI) transferability
transferable
antigen
any molecule, macromolecule, viral particle or cell that contains a structure recognized and bound by an Ig or TCR
antibody determinant (epitope)
portion of the Ag recognized by the Ab
CD4T (AKA helper T cells)
triggers the immune system and picks the path of attack (HI vs CMI)
keystone cell
CD4T cell (aka helper T cell)
BCR
B cell receptor, binds native proteins on pathogen
soluble form of BCR
Antibody
TCR
T cell receptor, binds peptide fragments from degraded pathogen
soluble form of TCR
no soluble form
antibody
made by our bodies to bind a specific epitope and prevent re-infection
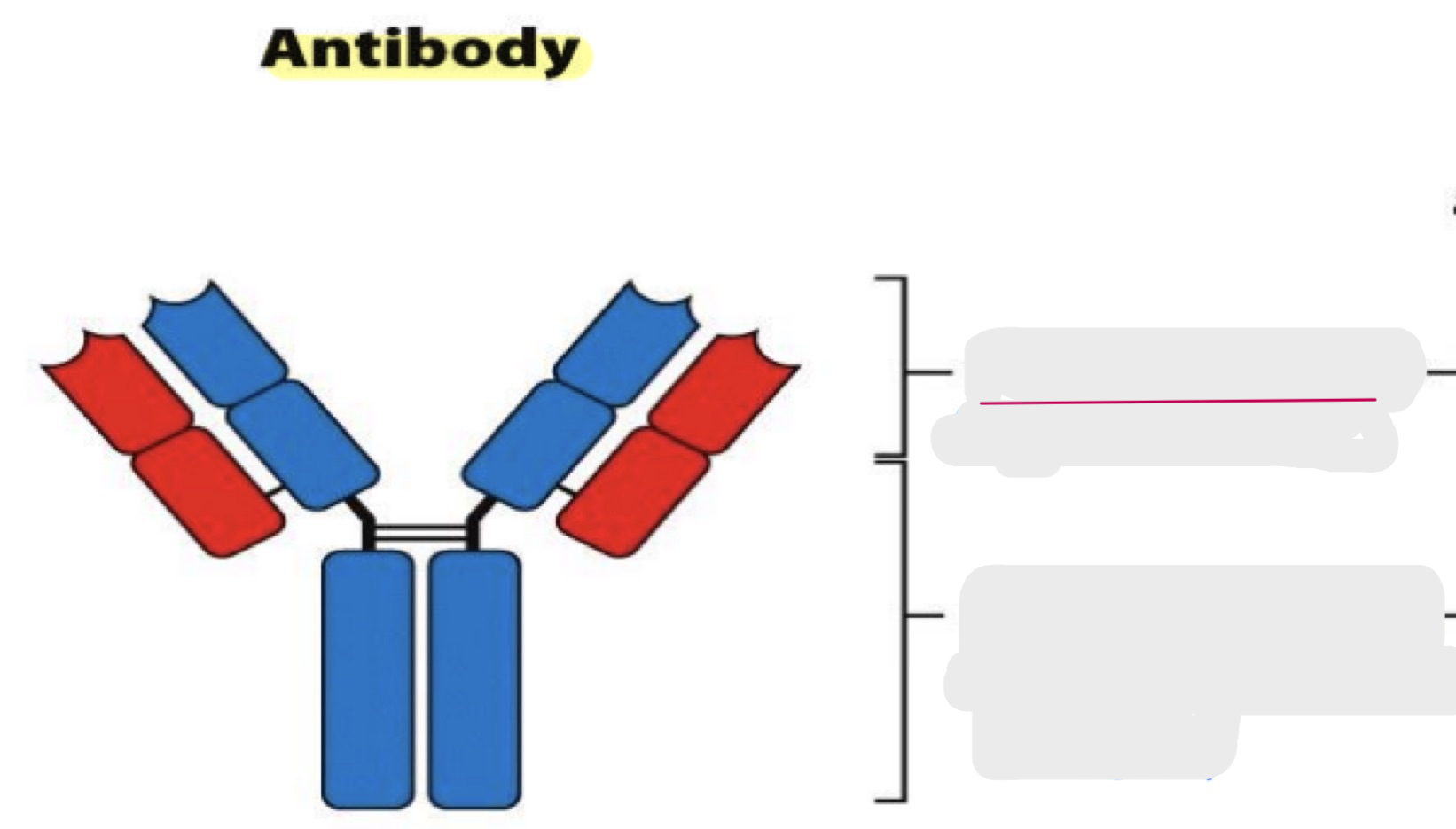
variable region
constant region
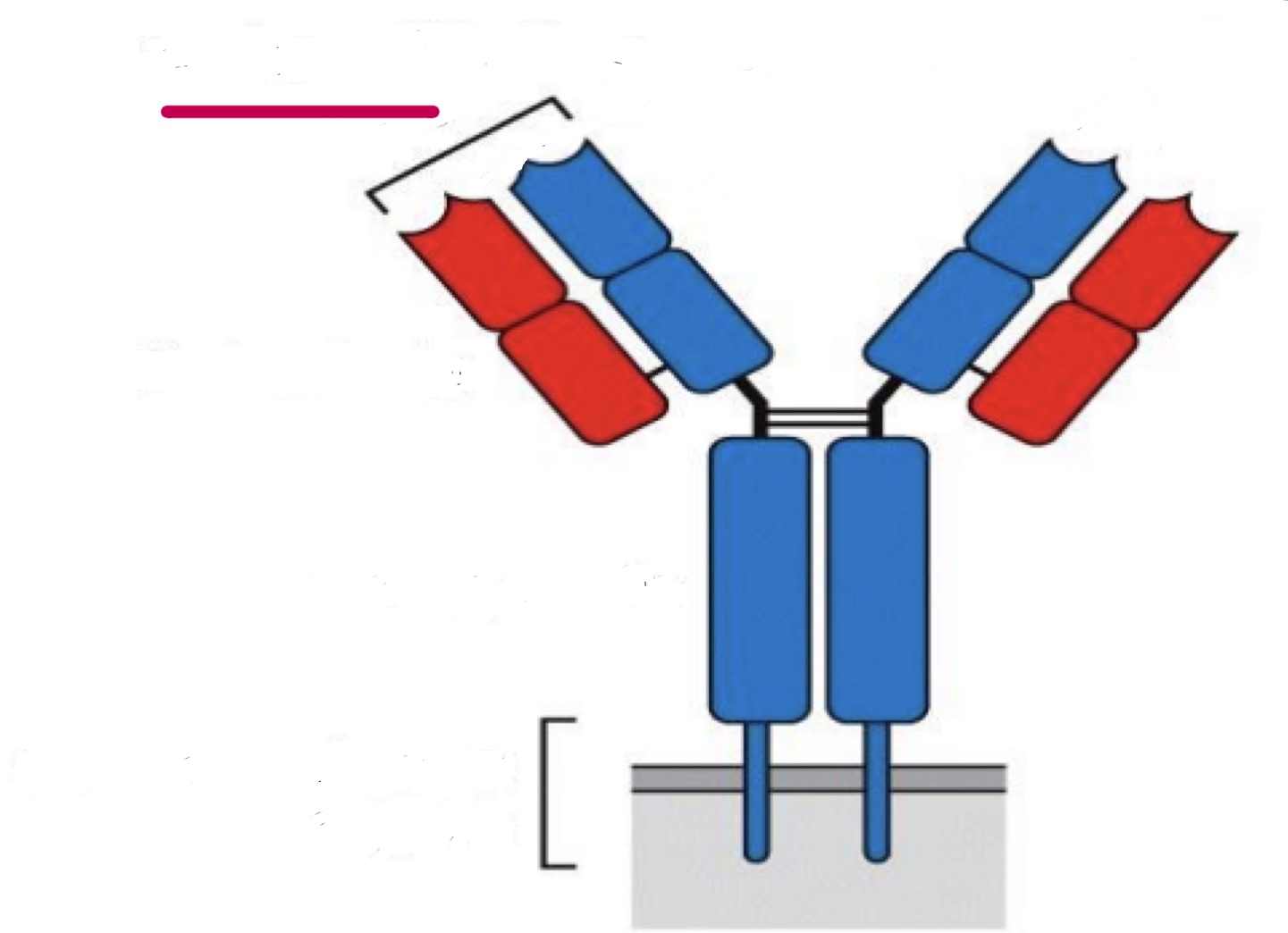
antigen-binding site
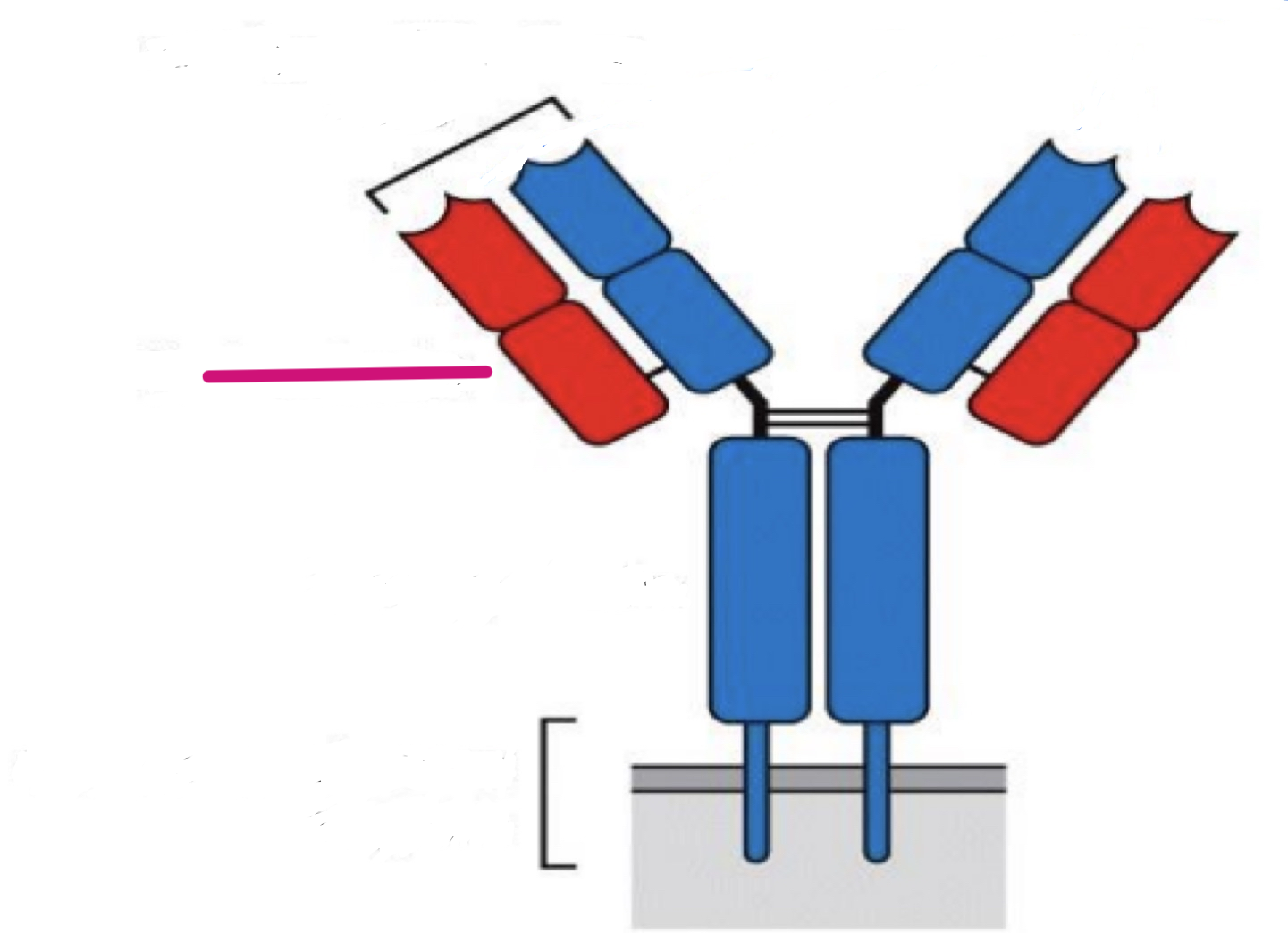
light chain
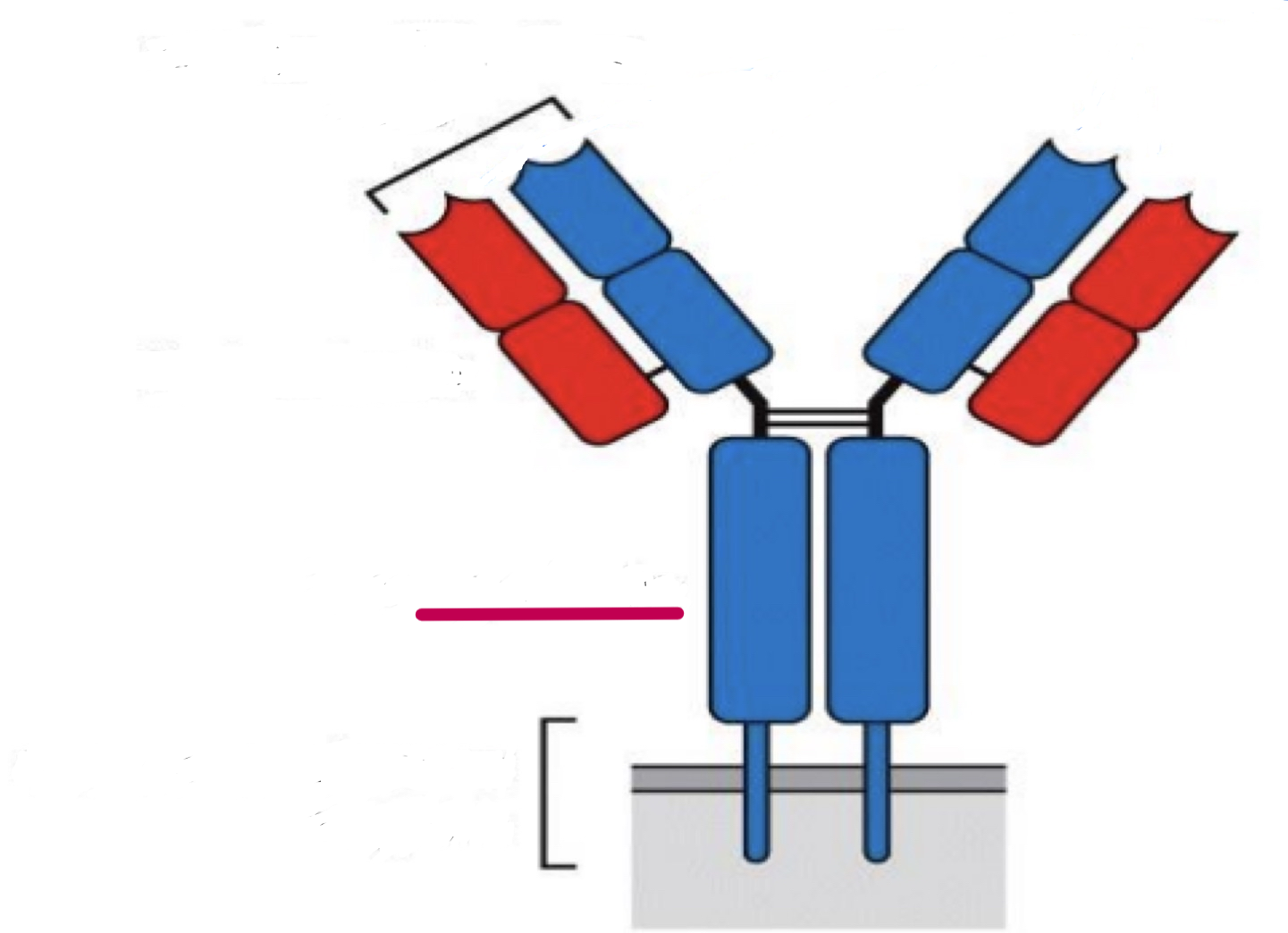
heavy chain
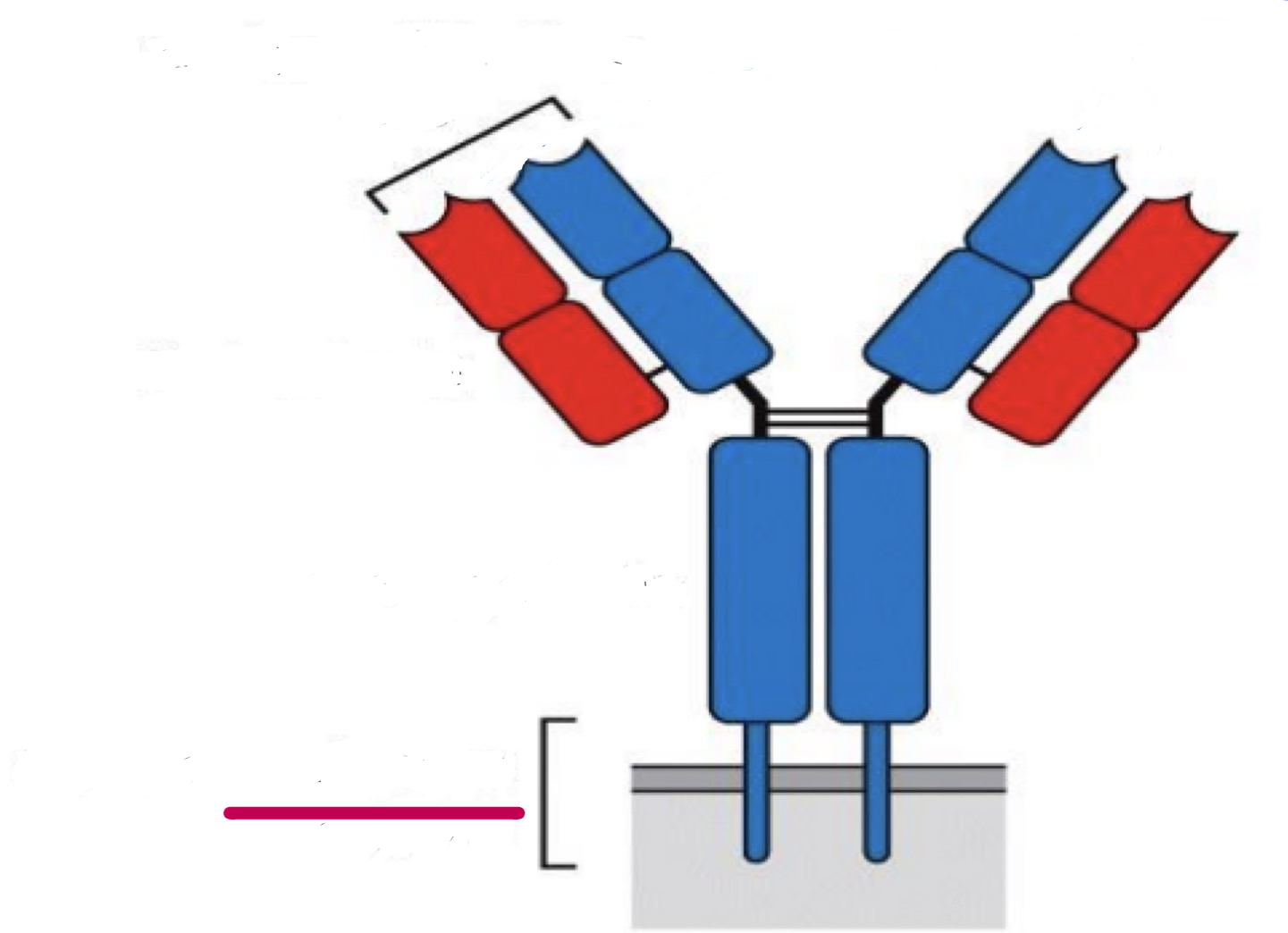
transmembrane region
antibody repertoire
the total number of antibody specificities in an individual (hundreds of billions!
antigenic processing
dendritic cells degrade pathogen, producing short peptides
clonal selection postulate 1
each cell has one receptor for one antigen
clonal selection postulate 2
activation occurs when a cell binds tightly to antigen
clonal selection postulate 3
differentiated effector cells are exact copies
clonal selection postulate 4
cells that bind tightly to self are destroyed
what links adaptive and innate immunity?
dendritic cells
two major steps linking adaptive and innate immunity
antigens carried to lymphoid tissue by dendritic cells
dendritic cells activate T cells
antigenic presentation
display of antigen as peptide fragments bound to MHC on cell surface
MHC
major histocompatibility complex, where peptides are presented
MHC class I
presents peptides from intracellular pathogens
MHC class I location
present on all nucleated cells
MHC class II
presents peptides from extracellular pathogens
MHC class II location
only on pAPCs
pAPC
professional antigen presenting cells
3 pAPCs
macrophages
dendritic cells
B-cells
co receptor for an intracellular infection
Tc TCR
co-stimulatory molecule for an intracellular infection
CD8
binding site of intracellular antigen recognition
APC MHC I
location of intracellular antigen recognition
AOC and cytotoxic T cells
co receptor for an extracellular infection
TH TCR
co-stimulatory molecule for an extracellular infection
CD4
location of extracellular antigen recognition
APC and helper T cell
binding site of extracellular antigen recognition
APC MHC II
APC
antigen presenting cell
to become activated, TCRs must bind to:
antigen and self protein on APC (with co-receptor)
co-stimulatory molecules
neutralization
prevents pathogen growth, replication or interaction with host cells
opsonization
aids in engulfment and destruction by phagocytosis
immunoglobulin
soluble form of antibody
clonal selection
selection of clones specific for Ag
clonal expansion
proliferation of selected clones
basic activation of B cells
surface Ig of B cells bind bacteria, the cell engulfs and degrades them, producing peptides
bacterial peptides are bound by MHC class II in vesicles
the bound peptides are transported by MHC class II to the surface of the cell
helper T cell recognizes the complex and activates the B cell
to become activated, a B cell must bind to:
free antigen
helper T cell (B cell acts as APC)
isotypes of antibodies
IgA
IgD
IgE
IgG
Igm
somatic recombination process
non-functional DNA is cut by enzymes to join the segments in the light chain or heavy chain, to be later transcribed and translated
segments in light chain
V (variable) and J (joining)
segments in heavy chain
V (variable), J (joining) and D (divsersity)
somatic recombination benefits
increases diversity and specificity of antibody response
junctional diversification process
random addition or subtraction of nculeotides at the junction between V, D and J segments
junctional diversification benefits
increases diversity and specificity of antibody response
isotype switching process
by altering the heavy chain the isotype is changed on the antibody
isotype switching benefirs
improves specialization of function and ability to recruit effectors
somatic hypermutation process
random mutation that selects for for antibodies that bind more tightly to pathogen
somatic hypermutation benefits
improves Ag binding by the Ab