Topic 4: Homeostasis
1/65
Earn XP
Description and Tags
Tested in Exam 1. the body's automatic process for maintaining a stable, balanced internal environment using feedback loops.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
66 Terms
Homeostasis
The body's dynamic automatic process for maintaining a stable, balanced internal environment using feedback loops. Internal adjustments are constant and counteract environmental changes to restore balance (stasis). This is so the body can function optimally, remaining energetically favorable and efficient.
Ex:
Enzymes function best when within a certain range of temperature and pH. Cells must maintain a balance between having too much or too little water in relation to their external environment.
Negative Feedback
A self-regulating process where a system's output reduces or counteracts changes to its input.
Internal Responses
The physiological processes of a body that execute homeostasis to return conditions to a set point.
Ex. water level controlled by ADH and kidneys.
Stimulus
Any internal or external change that disrupts the body's stable internal environment, necessitating a corrective response.
Sensor/Sensory Receptor
A specialized cell, tissue, or organ that detects stimuli in the internal or external environment and signals this information to the control center (often the nervous or endocrine system) through sensory transduction. Can sometimes be nerve fibers.
Sensory Transduction
Stimulus (or change) is converted into an action potential (AP) by a sensory receptor. Action potential is transmitted along axons towards the central nervous system (CNS) where it is integrated.
Ex: sensory cells (rods and cones) in the retina convert the physical energy of light signals into electrical impulses (APs) that travel to the brain.
Control
Chemical signals sent and coordinated by the nervous and endocrine systems to maintain stable internal conditions after receiving information from sensors/receptors. Can either be intrinsic or extrinsic.
Intrinsic Control
Self-regulation within an organ or system, driven by local needs.
Ex: oxygen levels in a specific tissue, heart controlling its own beat.
Extrinsic Control
Involves outside systems, such as the nervous or endocrine systems, regulating the organ for overall body needs.
Ex: maintaining blood pressure
Effector
A muscle or gland that carries out commands from the control center to reverse or enhance a stimulus, thereby maintaining homeostasis by coordinating the activities of organ systems. Can include many body systems, including: muscular, skeletal, integumentary, circulatory, lymphatic/immune, respiratory, digestive, excretory, and reproductive.
Hypokalemia
Low levels of potassium in the blood.
Hypochloaemia
Low levels of chloride in the blood.
Nephron
The functional unit of the kidney that filters your blood. Allows a person to reabsorb water or expel it as part of urine.
CO2 + H2O ↔ H2CO3 ↔ HCO3- + H+
Hydrogen ions and bicarbonate are excreted from renal tubular cells into the nephron lumen (removing them from extracellular fluid and increasing pH overall).
The absence of products shifts the buffer equation to the products side. Carbon dioxide combines with water inside the cells to form new bicarbonate and H+ (decreasing pH overall).
Kidneys reabsorb the bicarbonate and put it back into the blood to maintain homeostasis. H+ gets moved from the nephron lumen into urine for excretion.
When hydrogen ions are excreted, potassium and chloride are also lost.
Osmoreceptors
Specialized sensory neurons, primarily located in the hypothalamus of the brain, that detect changes in the osmotic pressure (solute concentration) of blood plasma. When the osmotic pressure of blood changes (i.e. dilution changes), water diffusion into and out of the osmoreceptor cells changes to expand when the blood plasma is more dilute and contract with higher concentration.
This causes an neural signal to be sent to the hypothalamus to increase or decrease ADH secretion from the posterior pituitary to return blood concentration to normal.
Is Osmolarity the Same as Tonicity?
No. Both terms describe solutions, but similarity ends there.
Osmolarity is concentration expressed in units of solute/volume. It can be measured on a machine called an osmometer, and it has units, usually osmoles or milliosmoles per liter.
Tonicity is a behavioral term. It describes what a solution would do to a cell's volume at equilibrium if the cell was placed in the solution. Tonicity cannot be measured on an osmometer, and it has no units. It tells what effect a solution has on a cell, and it depends both on the osmolarity of the solution and on whether or not solutes in the solution can enter the cell.
We care because understanding tonicity is the basis for intravenous (iv) fluid therapy, and administering the wrong iv solution to patients can harm or even kill them.
Bicarbonate Buffering Reaction
CO2 + H2O ↔ H2CO3 ↔ HCO3- + H+
Where H2CO3 is carbonic acid, and HCO3- is bicarbonate.
Water dissociates in the body to hydrogen and hydroxyl ions. Overall, hydroxyl ions combine with carbon dioxide to form bicarbonate.
Abundance or build-up of CO2 will shift the buffering reaction to the right, according to the law of mass action. This will cause a build up of H+ will make blood more acidic, disrupting homeostasis.
Respiratory Acidosis
Decreased or obstructed respiration causes increased blood carbon dioxide and decreased pH. Carbon dioxide is produced constantly as the body burns energy and will accumulate rapidly if the lungs do not adequately dispel it.
Can be caused by a neuromuscular disease or chronic obstructive pulmonary disease (COPD).
Metabolic Acidosis
Can occur if the kidneys are not removing enough acid from the body.
Kidneys are unable to secrete the H+ into the filtrate. Thus, H+ cannot be excreted with urine and results in a drop in pH.
Ketoacidosis
Happens when the body fails to process glucose and switches over to burning fatty acid.
Inadequately regulates ketones (bi-products of fatty acid breakdown like acetone and acetoacetic acid). Accumulation of keto acids decreases blood pH and interferes with the body’s ability to excrete H+ into the urine.
Common ex:
Type 1 Diabetes. A lack of insulin means no glucose absorption, so the body switches to fatty acid metabolism, which causes ketones.
Alcoholic ketoacidosis. Alcohol blocks the first step of gluconeogenesis, meaning that body doesn’t synthesize enough glucose. Fatty acid metabolism kicks in and causes ketones.
Respiratory Alkalosis
Happens when blood pH is too high (too much bicarbonate concentration, making it alkaline). Can be caused by hyperventilation, which causes the body to lose carbon dioxide, since one is expiring more CO2 than what is being produced in the body.
When the CO2 concentration of the blood falls below its normal level, the blood's pH value is raised (making it more basic). To get CO2 levels back to normal, one can breathe into a bag. Rebreathing the air that is exhaled makes you inhale more CO2 and helps you to quickly add the CO2 back into your bloodstream.
Metabolic Alkalosis
Increase in plasma alkalinity (bicarbonate concentration). 4 main causes.
Excessive loss of hydrogen ions by the kidney or via the GI tract (vomiting). Loss of fluid decreases extracellular volume and arterial pressure, reducing glomerular filtration rate (GFR) so less water/urine is filtered out and lost.
Intracellular shift of hydrogen ions (reduces the extracellular concentration of hydrogen ions). Hyperaldosteronism: excess aldosterone production by the adrenal cortex impacts the RAAS system. RAAS system directs water secretion, leading to increasing renal hydrogen ion secretion and thus excess bicarbonate.
Retention of (exogenous) bicarbonate ions from loop and thiazide diuretics (increases urine output by making kidneys excrete more sodium, potassium, and water). Loosing sodium and water from taking diuretics indicates to kidneys to decrease GFR and reduce bicarbonate filtration by the kidney.
Volume contraction around a constant supply of extracellular bicarbonate. The body loses a proportionally significant amount of water and salt compared to bicarbonate, resulting in a higher concentration of bicarbonate in a reduced volume of plasma. Angiotensin and sympathetic activation increases bicarbonate reabsorption and generation in addition to sodium reabsorption in the tubule in response to low levels of fluid.
Diuretic
The process of forming or excreting urine (diuresis).
Antidiuretic Hormone (ADH)/Vasopressin
A hormone produced in the hypothalamus and released by the pituitary gland.
When water levels in the blood drop below normal range, the hypothalamus detects higher concentration of solutes in the blood. The pituitary releases this hormone, simulating kidneys to reabsorb more water to reach homeostasis.
When water level in the blood rise above the normal range, the hypothalamus detects lower concentration of solutes in the blood. The pituitary releases less of this hormone, simulating kidneys to reabsorb less water to reach homeostasis.
Interstitial Fluid
Extracellular fluid filling the spaces between cells, acting as a buffer, nutrient deliverer, and waste remover for tissues. Comprises main component of the extracellular fluid (ECF) including plasma. Contains ions for osmotic balance and complex molecules as energy. circulatory system and excretory system help remove waste.
Active Hyperemia
Increased blood flow through a tissue associated with increased metabolic activity.
Endothelial Cells
Thin layer of epithelial cells that line the interior surface of blood vessels. Serves 6 main functions:
Maintaining blood fluidity (forms a smooth, non-adhesive, and anticoagulant luminal surface).
Regulating the passage of molecules by controlling the movement of solutes and macromolecules between the blood and the surrounding tissues.
Responding to injury or infection by changing its processes to help with hemostasis and leukocyte recruitment.
Producing signaling molecules that regulate the contraction of smooth muscle cells and cardiac myocytes.
Creating new blood vessels
Participating in immunity by playing a role in both innate and acquired immunity.
Are Endothelial Cells in Blood Vessels the Same Thing as Smooth Muscle Cells in Blood Vessels?
No. Anatomically, endothelial cells line the blood vessel interior, with smooth muscle cells adjacent but further away from the lumen of the blood vessel.
They serve different purposes as well. Endothelial cells detect homeostasis levels and release chemical signals when needed, while smooth muscle cells execute what the signals direct them.
Acetylcholine
A neurotransmitter released by autonomic nerves in the walls of the blood vessel. Receptors in the endothelial cells of the blood vessel then activate nitric oxide synthase in response.
Nitric Oxide (NO)
When blood oxygen levels fall, endothelial cells in blood vessel walls synthesize and release nitric oxide. NO freely diffuses through the plasma membrane and affects nearby cells.
NO then activates the enzyme soluble guanylate cyclase sGC, which leads to the production of cyclic GMP (cGMP) and pyrophosphate from GTP, relaxing neighboring smooth muscle. This dilates blood vessels, increasing blood flow.
Nitric Oxide Synthase (NOS)
An enzyme in blood vessel endothelial cells that convert L-arginine into nitric oxide (NO) when activated by the presence of acetylcholine. Activated as a second message pathway after the release of acetylcholine.
Vasodilator
Chemical mediators that result in the dilation of blood vessels. If vasodilation happens in one area, vasoconstriction must happen in a different area at the same time as a compensatory mechanism (ex. blood draining from face to contribute to flight/fight response).
Ex: nitric oxide is a vasodilator (NO)
Adrenal Medulla
The inner portion of the adrenal gland (endocrine system) that functions as part of the sympathetic nervous system to manage short-term stress. Can increase blood pressure by releasing epinephrine and norepinephrine. Can also interact with cardiovascular and excretory systems when changing blood pressure.
Postural Hypotension
A sudden drop in blood pressure that occurs within less than 3 minutes of a person standing up. or sitting up When a person stands up, blood temporarily pools in the legs, particularly in the elderly due to varicose veins. Causes a drop in venous return to the heart: causes blood pressure to fall.
Baroreceptors
Specialized nerve endings that detect blood pressure changes by mechanically sensing vessel stretch. Generates action potentials (electrical impulses) when stretched. These receptors decrease their rate of firing (APs) when blood pressure drops.
Located particularly the atria of the heart, aortic arch, and carotid sinuses.
Relays signals (APs) to the medulla oblongata in the brainstem to elicit the appropriate response to restore homeostasis. The brainstem then sends signals via autonomic (involuntary) nervous system (ex: heart rate, digestion, respiration rate, etc) to elicit changes.
Ex: Postural Hypertension
Postural Hypertension
Caused by standing up too fast cause less stretch in the baroreceptors, firing action potentials at a slower rate to the medulla oblongata. Less action potentials reach the cardiac inhibitory center of brainstem, increasing cardiac output to increase blood pressure.
Alternatively, the medulla oblongata can send the signal via the endocrine system and the Adrenal Medulla (adrenal gland) to release epinephrine and norepinephrine. This will also cause the heart to pump harder and faster.
Chemoreceptors
Specialized sensory cells that detect chemical stimuli such as oxygen, carbon dioxide, and pH levels to regulate internal homeostasis, specifically respiration and cardiovascular function.
Ex: if oxygen content falls below set point, these cells send AP signals to the brainstem. The brainstem integrates this information with the information from the baroreceptors. Sends the signal to increase the rate and force of the heartbeat and respiration.
Thermoregulation
Two types: physiological and behavioral.
Animal cells can survive in a temperature range of 0°C to 45°C (32°F -113°F).
Below freezing lipid bilayer changes from fluid to frozen gel, ice crystals form disrupting cell function and destroying organelles. At high temperatures, proteins and nucleic acids unfold due to an increase in kinetic energy of molecules.
Ectotherm
Animals that obtain heat from the environment. Must live in environment favorable to body temperature requirements, but typically have lower metabolic rate than endotherms which can conserve energy. Small surface to volume ratio enables them to retain more heat than endotherms.
Ex: some fish, reptiles, invertebrates, amphibians.
Endotherm
Animals that obtain heat from the environment and generate heat metabolically. Maintains body temperature over a narrow range. Balances internal heat production with heat loss from body surface. Metabolic rate rises at low environmental temperatures, generating body heat.
Ex: birds, mammals.
Altering Heat Conductance With Fur/Feathers
A form of thermoregulation via insulation. Animal with feathers or fur can fluff up as the temperature decreases to increase insulation by trapping a layer of air next to the skin; heat lost from the body gets trapped in that layer of air.
Air is a good insulator because its molecules are spread far apart, meaning heat transfer through conduction is difficult: minimal contact between molecules.
Alternatively, fur can be used to reflect sunlight away from the surface of the animal. Prevents (short wave radiation) absorption and conversion to heat (long wave radiation). Prevents dehydration. Ex: springboks.
Altering Heat Conductance With Blubber
A form of thermoregulation via insulation. Blubber (thick layer of fat under the skin) is common in many artic marine mammals, where living in water makes it difficult to retain heat. Blood circulation is restricted to deeper, warmer body tissues beneath the thick fat layer (blubber) rather than traveling to the cold skin surface.
Altering Heat Conductance With Vasodilation and Vasoconstriction
When cold: the body redirects blood flow to avoid the surface. Larger diameter of internal vessels than superficial vessels. Results in the body being more insulated because the blood is flowing beneath a fatty layer of skin.
If warm: the blood can be redirected to the surface and heat can flow out more easily. Larger diameter of superficial vessels than internal vessels. This increases conductance.
Counter-Current Flow
Where arteries and veins run parallel in opposite directions. Blood flowing out to the flipper is warm and warms the blood coming back to the body. This arrangement maintains a consistent concentration gradient along the entire vessel length.
Consequence: isolated body parts don’t change the temperature of the rest of the body.
Ex: limb of a bird that lives in the cold, veins surrounding the ulnar artery.
Thermoreceptors
Specialized sensory nerve endings in the skin (peripheral) and brain/body core (central) that detect temperature changes to maintain homeostasis. The signals created from these sensors are integrated by the hypothalamus and result in changes in blood flow to the body surface, sweating or panting, shivering, behavioral modifications.
Epithelial
A tissue that lines body structures and cavities and forms protective, secretory, and absorptive coverings. Serves in lining and exchange.
Three types:
Squamous epithelium. Layer of flattened cells to serve in diffusion. Located in the walls of blood vessels (ex. endothelial cells); air sacs or lungs.
Cuboidal epithelium. Layer of cubelike cells; free surface may have microvilli and serves in secretion and absorption. Located in glands and tubular parts of nephrons in kidneys.
Columnar epithelium. Layer of tall, slender cells; free surface may have microvilli that serves secretion and absorption.
Connective
A tissue that connects, supports, binds, or separates other tissues or organs.
Types of Connective Tissue
Loose connective tissue, dense fibrous connective tissue, cartilage, adipose tissue, osseous tissue, and blood.
Fibroblasts
The primary, spindle-shaped cells of connective tissue that produce and maintain the extracellular matrix (like collagen, elastin, fibronectin).
Glycoprotein Matrix
The essential, carbohydrate-modified proteins that form a complex, fibrillar scaffold to support connective tissue.
Ex: fibronectin.
Loose Connective Tissue
Fibroblasts and other cells surrounded by collagen and elastin fibers forming a glycoprotein matrix. Loosely arranged in a mesh-like, airy network rather than being tightly packed together. Functions for support, elasticity, and diffusion. Located under the skin and most epithelia.
Fibrous Connective Tissue
Long rows of fibroblasts surrounded by collagen and elastin fibers in parallel bundles with a dense extracellular matrix. Functions for strength and elasticity. Located in tendons and ligaments.
Chondrocytes
A cell which secrets the matrix of cartilage and becomes embedded in it. Synthesizes chondroitin sulfate, a vital structural component of cartilage that helps maintain joint elasticity, shock absorption, and lubrication.
Cartilage
Chondrocytes embedded in a pliable, solid matrix of collagen and chondroitin sulfate. Functions for support, flexibility, and as a low-friction surface for joint movement. Located at the ends of long bones, the nose, parts of airways, and the skeleton of vertebrate embryos.
Hydroxyapatite
The main structural component of tooth enamel and bone mineral that provides hardness.
Fine Canals/Canaliculi
Microscopic channels radiating from lacunae (small spaces containing osteocytes) to connect them with each other and to central canals. They facilitate the transportation of nutrients, waste, and signaling molecules, allowing osteocytes to communicate and maintain bone matrix.
Bone Tissue
Osteocytes in a matrix of collagen and glycoproteins hardened with hydroxyapatite. Also contains fine canals and a central canal containing blood vessels. Functions for movement, support, and protection. Located in the skeleton of vertebrates.
Adipose Tissue/Fat
Large, tightly packed adipocytes with little extracellular matrix. Functions as energy reserves, insulation, and padding. Located under the skin, around the heart, and on the kidneys.
Blood
Leukocytes (white blood cells), erythrocytes (red blood cells), and platelets suspended in a plasma matrix. Functions to transport substances. Located in the circulatory system.
Types of Muscle Cells
Skeletal, Cardiac, and Smooth.
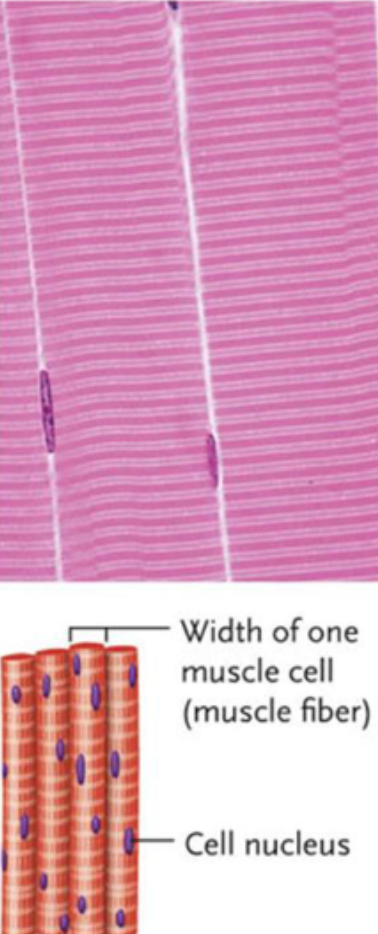
Skeletal Muscle
Bundles of long, cylindrical, striated, contractile cells called muscle fibers. Multiple cell nuclei. Functions as locomotion and movement of body parts. Attached to bones of the skeleton.
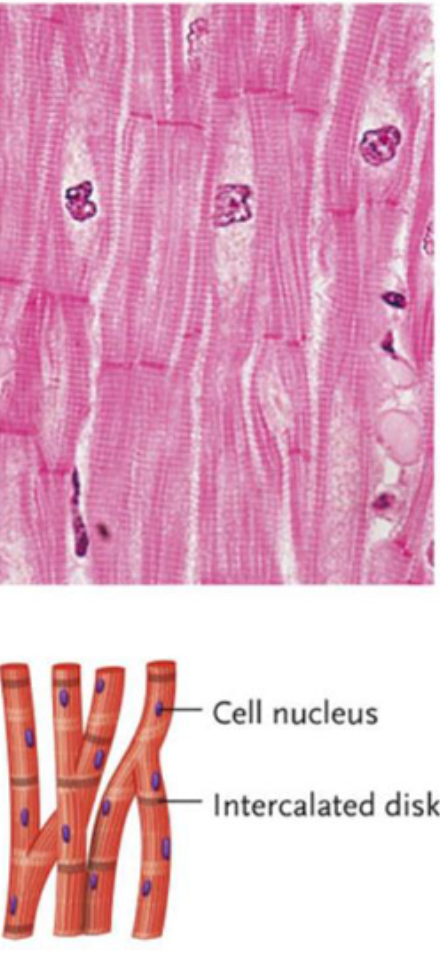
Cardiac Muscle
Cylindrical, striated cells that have specialized end junctions called intercalated disks. Functions to pump blood within the circulatory system. Located within the wall of the heart.
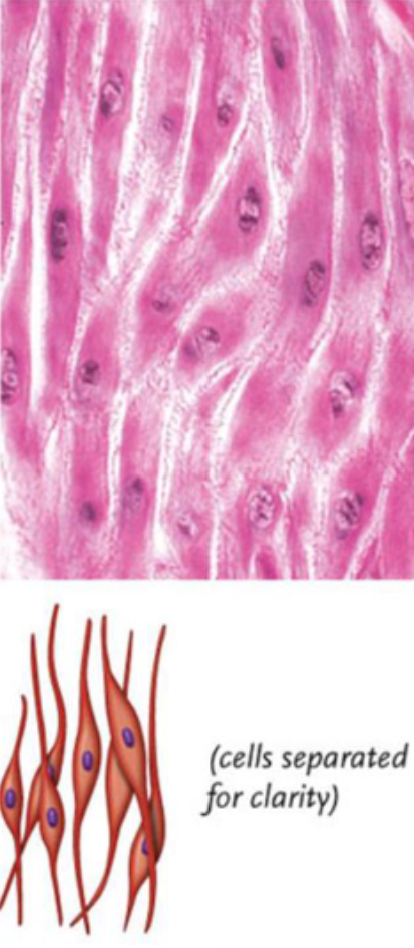
Smooth Muscle
Contractile cells with tapered ends. Functions for movement of internal organs. Located in the wall of internal organs, such as the stomach.
Dendrites
A short branched extension of a neuron with synapses. Impulses received from other cells at synapses are transmitted to the cell body.
Cell Body of a Nerve/Soma
The central part of a neuron containing the nucleus and vital organelles, acting as the cell's control center to process information and maintain life, integrating signals received by dendrites and transmitting them down the axon to communicate with other cells.
Axon and Axon Terminals
A long, slender projection of a neuron that conducts action potentials (electrical impulses) away from the cell body to other neurons, muscles, or glands. Terminals are the specialized ending of an axon that releases neurotransmitters to transmit signals across a synapse to another.
Why Must we Distinguish and Identify the Tissues that Make Up Organs?
Scientists must understand the basics and normal composition of organs before using them as comparison to tissues affected by disease.