11A- weight management and disordered eating
1/61
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
62 Terms
what is the source of fuel in food
macronutrients
carbohydrates, lipids (fatty acids), and amino acids
what do all 3 major macronutrients converge at
acetyl Co-A
feeds into TCA/Krebs cycle and oxidative phosphorylation in the mitochondria
order of events to create energy
glycolysis
beta-oxidation
deamination +
how is excess fuel stored
multistep process that requires energy itself
storing dietary fat is the most energy efficient
2-3% of the energy from fat is used to store it
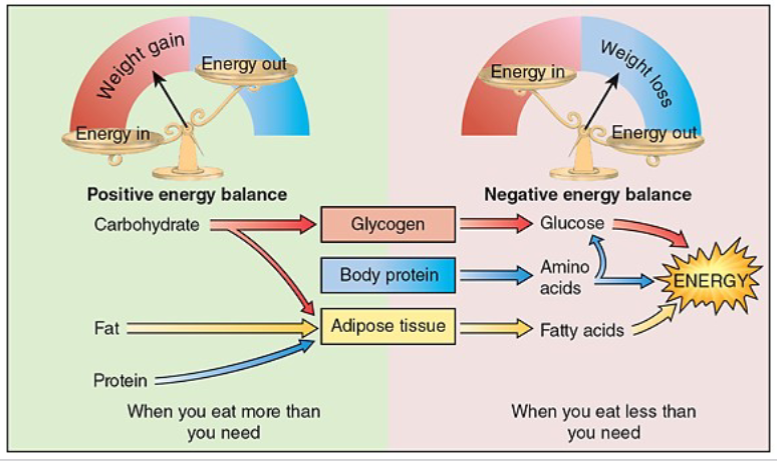
energy balance
energy intake- energy requirements
neutral energy balance
adequate energy= no net storage or depletion
positive energy balance
extra energy= energy storage
negative energy balance
insufficient energy= depletion
how is total energy balance determined
combination of factors
ex. food intake (including digestive efficiency), activity level
energy balance
consuming more energy than needed will result in energy storage
consuming less energy than needed will result in depletion of the energy reserves
energy needs directly impact energy balance
total energy expenditure formula
TEE= BMR + activity + TEF
TEE= total energy expenditure
BMR= basal metabolic rate
TEF= thermic effect of food
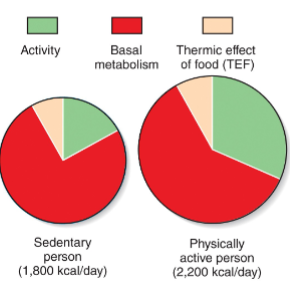
how does MBMR, activity and TEF variation determine TEE
BMR is largest proportion of TEE (75%)
activity is the most “straightforward: to modify voluntarily for healthy people (around 15%)
TEF is relatively stable compared to BMR and activity (around 10%)
how does TEF varie
meal size
meal composition (higher TEF for proteins and carbohydrates vs. lipids)
meal frequency, timing, duration…
factors that influence BMR may also influence TEF- body composition, age, etc.
TEF seems to be reduced in obese vs. lean individuals (may be related to insulin resistance.sensitivity)
how does BMR vary across individuals
varies between individuals and different points in life
height and weight (=BMI)
sex (% fat vs muscle mass, hormones)
age/development/lifestage (pregnancy, lactation, infancy, childhood, adolescence, adulthood, senior…)
hormone levels (ex. thyroid hormone)
stress, fever, illness
other genetic factors
effects of medications and other compounds (ex. caffeine)
fed, fasted, or starved energetic state
external cues that modulated energy intake
time of day
food availability
food quality
social norms and influences
internal cues for energy intake
hunger and satiety
emotions (ex. stress, boredom)
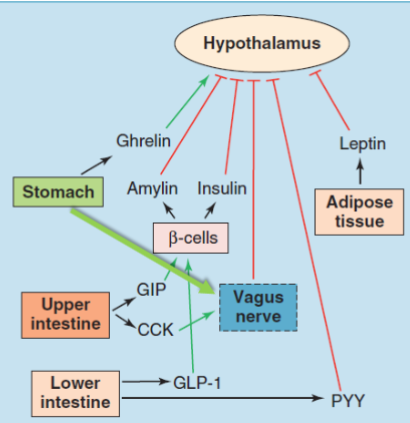
ghrelin
“hunger hormone”
produced by stomach
increases drive to eat
vagus nerve in hunger
connects brain and digestive system (PSNS)
vagal stimulation be stretch receptors in the stomach decrease appetite
leptin
“energy expenditure hormone”
protein hormone
made by adipocytes
levels correlate with energy reserves (stored triglycerides)
leptin inhibits hunger to stimulate satiety
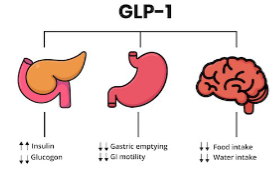
GLP-1
glucagon-like peptide-1
peptide hormone produced by large intestine and ileum
decreases blood glucose levels (+insulin and -glucagon)
decreases appetite by slowing gastric emptying
CCK
cholecystokinin
peptide hormone that stimulates the digestion of fat and protein
secreted by duodenum in the small intestine
insulin
peptide hormone
secreted by b=cells in the pancreas
induces uptake of glucose into body cells (+other function)
reduces hunger
overall overview of factors impacting appetite control
*missing vagal innervation of the stomach
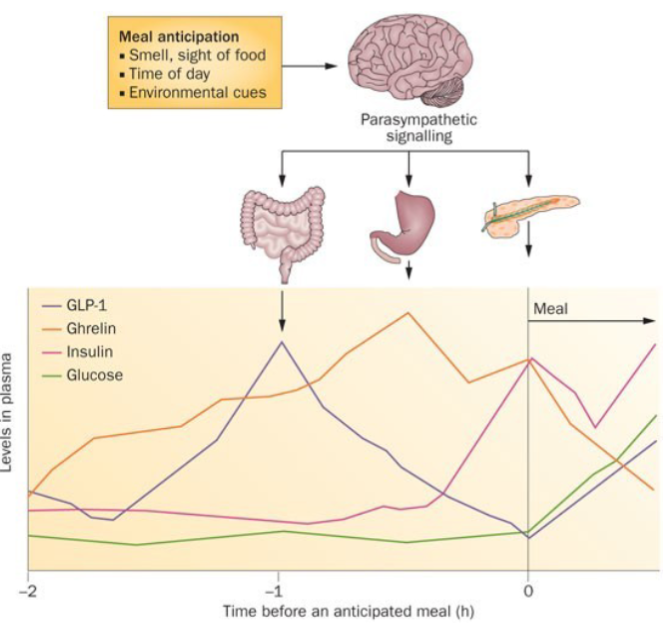
anticipatory signaling
regulation of food intake begins before a meal due to anticipatory signaling over 1h before feeding
what is anticipatory signaling triggered by
sensory and internal cues: smell/sight of food, time of day, other environmental cues
how does anticipatory signaling work
GLP-1 peaks around 1 h before a meal and return to baseline by meal start
ghrelin builds over time adn declines with feeding
insulin increases just before mealtime and in response to blood glucose
how does obesity vary across subpopulations
increases with age
economics:
lower with increasing education
lower in landed immigrants vs. non immigrants
dietary patterns
5+ fruits or vegetables per day reduces the risk of obesity
many other factors
what chronic diseases is obesity associated with
diabetes (T2)
gallstones and gallbladder disease
high BP
arthritis
CV disease
colon cancer
breast cancer
joint disorders
sleep apnea
mechanisms obesity increases risk of type 2 DM
chronic inflammation contributes to development of insulin resistance in tissues
increased use of FFA= increased toxic byproducts; damage to beta cells of pancreas and insulin deficiency
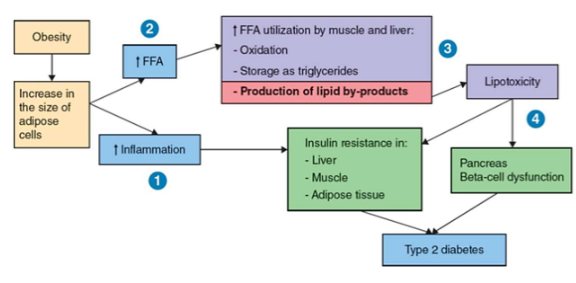
how do larger adipocytes contribute to chronic inflammation
enlarged adipocytes attract macrophages by secreting macrophage chemotaxis protein (MCP-1)
macrophages produce pro-inflammatory TNF-a
TNF-a induces export of FFA into the blood
how does inflammation cause insulin resistance
muscle imports the excess FFA from the blood, which build up as ectopic lipid droplets
ectopic lipid droplets interfere with GLUT-4 translocation= insulin resistance
exact mechanism unknown, but may be due to premature signaling pathway
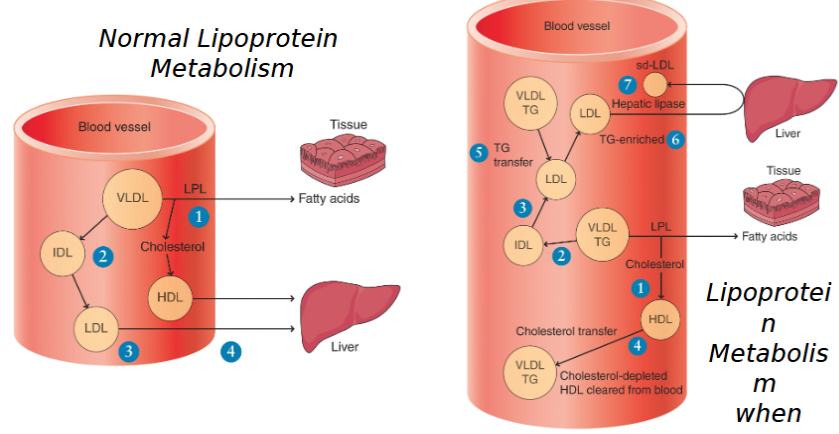
obesity and CVD
obesity promotes appearance of unusual lipoproteins that further increase the risk of CVD beyond “just” high LDL
how does obesity cause CVD
high levels of VLDL in obesity prevent normal metabolism of lipoproteins, leading to abnormal transfer of cholesterol and triglycerides between lipoproteins
production of “new” lipoproteins enriched with triglycerides (VLDL-TG and LDL-TG)
enriched lipoproteins can be converted into small dense-LDL (sd-LDL) by hepatic lipase
sd-LDL is like “norma;” LDL but worse- better at penetrating artery walls, longer residence time in the blood, more susceptible to oxidation
normal lipoprotein metabolism vs lipoprotein metabolism when VLDL is high diagram
BMI classifications (KNOW THIS)
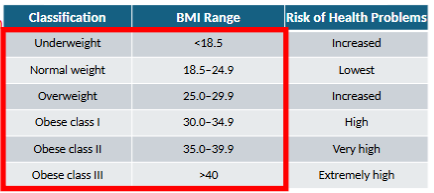
when is BMI effective or not effective
useful for measuring risk in a population, but not as effective for an individual
muscle weighs much more than fat, so muscular individuals have a higher BMI than expected
BMI limitations
does not factor in lean muscle mass vs adipose tissue
location of adipose tissue (visceral vs SC) varies across subpopulations and better predicts some co-morbidities
ignores metabolic markers of disease risk and mental health component of obesity
SC vs visceral fat
SC: around belly and outside
visceral: around organs and more internal
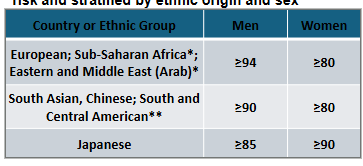
waist circumference cutoff’s associated with risk and stratified by ethnic origin and sex
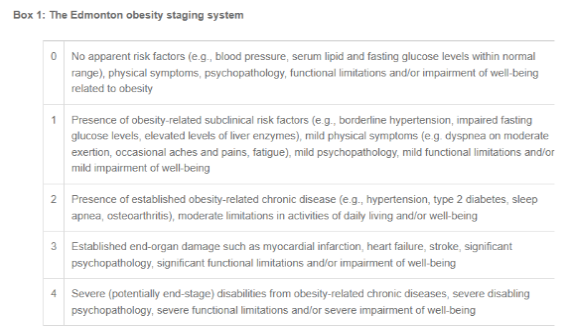
EOSS
edmonton obesity staging system
more comprehensive rating scale that includes physical adn psychological symptoms as well as functional limitations
focuses on associated health problem adn their severity vs weight
*be able to place someone on this scale
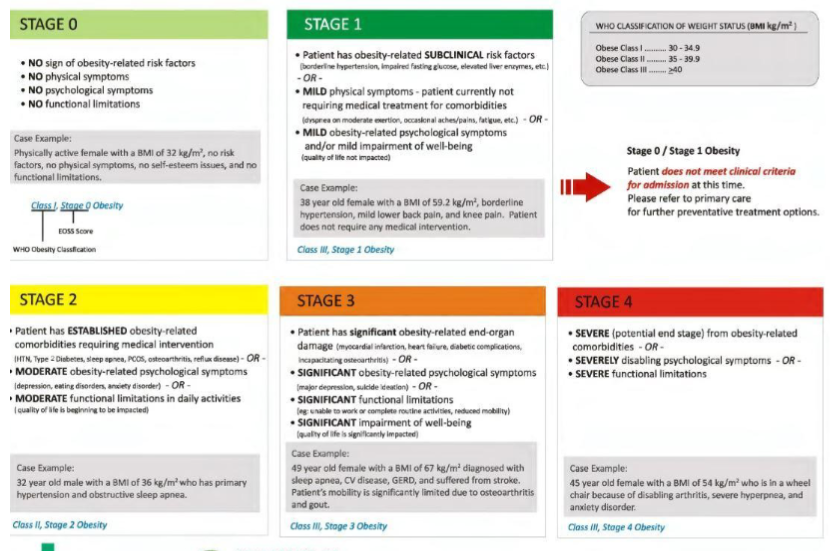
EOSS staging
0
obese but no risk factors present
no action or preventative options only
1
subclinical risk factor(s) present
preventative options only
2+
at least one established risk factor
specific nutritional, lifestyle, surgical, and/or pharmacological action needed
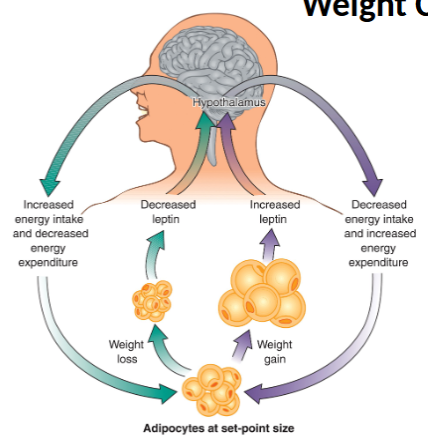
weight cycling
the human body has evolved to maintain survival when food was scarce and store energy efficiently in times of plenty
adipose cells have an average lifespan of around 9.5 years
leptin is a critical regulator of energy intake and expedenture
serves as an indicator of energy stores
however, leptin’s impact on energy intake can make weight management difficult
as energy stores are depleted, metabolic changes occur to stretch remaining stores as long as possible (“ecomode”)
BMR decreases
activity decreases
leptin decreases → increases hunger (increase food intake)
these factors make it easier to regain a positive energy balance, allowing adipose cells to refill
these factors also explain why calorie restriction alone is not a reliable weight management strategy
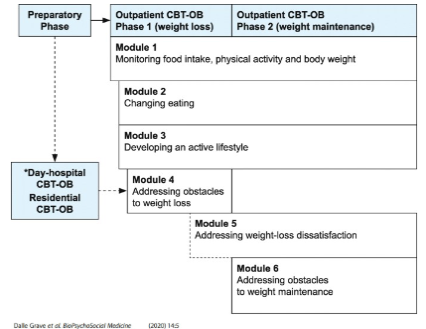
behavioural modification to treat chronic disorders of energy balance
may include specific interventions like CBT
ex:
preparatory phase: assess the nature and severity of obesity and any medical or psychosocial comorbidities
phase 1: initial weight loss including changing eating pattern, activity
phase 2: long term weight maintenance phase focusing on “locking in” new habits, tapering off monitoring
behavioural modification- diet
general recommendations for dietary modifications to treat obesity reflect those in the Canada Food Guide:
high protein to promote satiety
water as drink of choice
nutrient dense as opposed to energy dense foods
reduce processed foods
substitutions as opposed to eliminations
weight loss diets
low calorie (ex. weight watchers- follow canada’s food guide but reduced calorie intake)
prepared meals/drinks
low fat
low carb (paleo, keto, atkins)
intermittent fasting
gluten-free
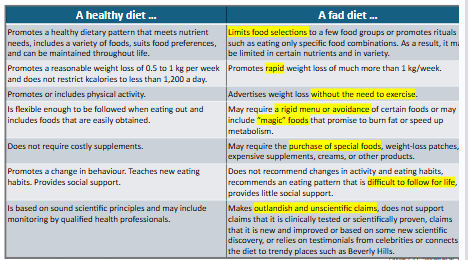
commercial weight loss programs are a spectrum from fat diet to healthy diet
considerations for weight loss diets
context and individual needs matter in diet choice
a gluten free diet for a person with gluten intolerance in good
fad diet
a plan that promotes results such as fast weight loss without robust scientific evidence to support its claims
client should be discouraged from using
healthy diet vs fad diet
weight loss pharmacotherapy approved in canada
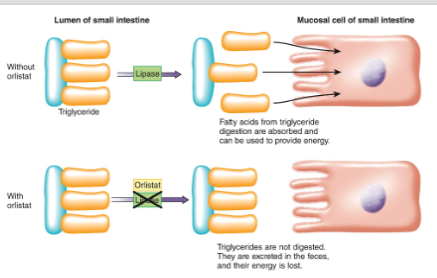
orlistat: pancreatic lipase inhibitors limits fat absorption
liraglutide and semaglutide: GLP-1 agonists reduce appetite
naltrexone and bupropion: hunger suppression
orlistat
GLP-1
once weight loss pharmacotherapy is stopped
often regained
side effects of weight loss meds
headache, dizziness, fatigue
GI disruption (nausea, vomiting, abdo pain, diathermia)
hypoglycemia, gallbladder problems, pancreatitis
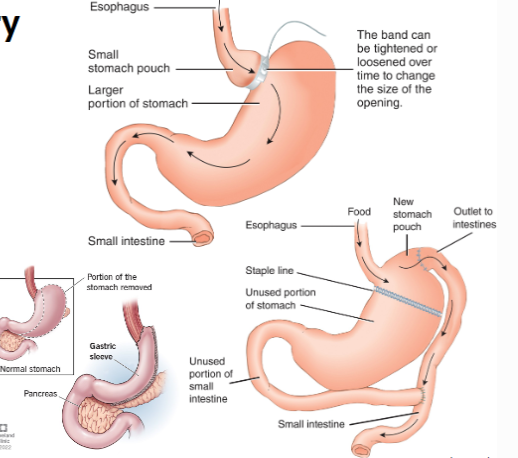
weight loss surgery
bariatric surgery: gastric banding, gastric bypass, sleeve gastrectomy
typically limited to higher obesity classes and obesity and established comorbidities
requires lifelong changes in diet adn lifestyle to accommodate permanent to GI physiology and absorption
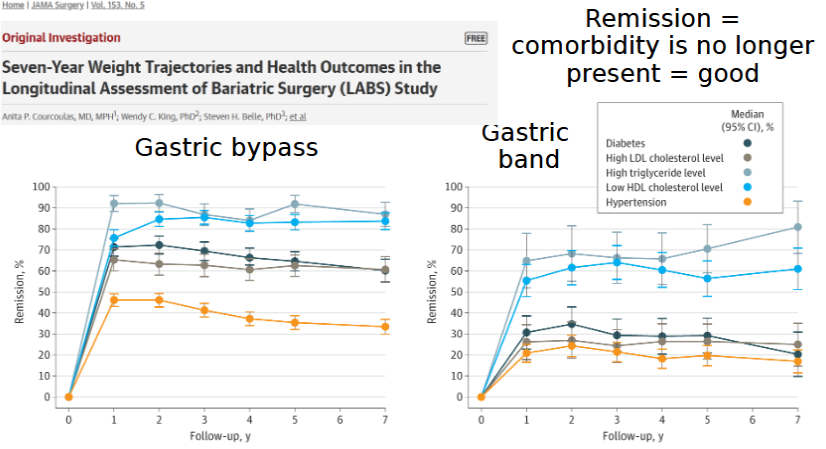
good outcomes
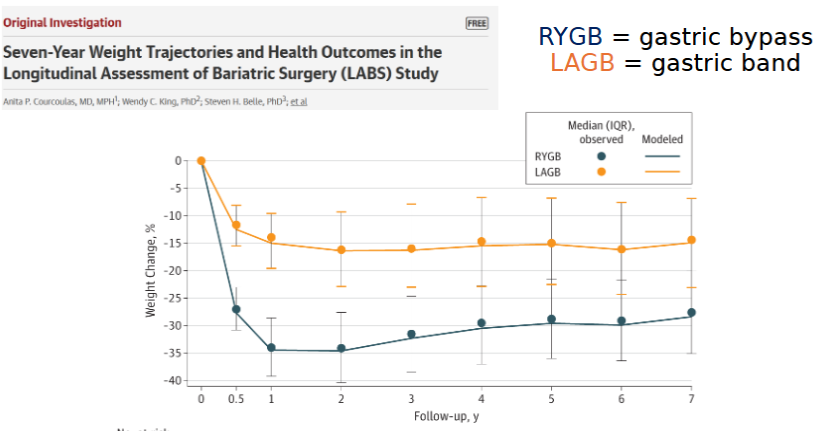
trajectory for bariatric surgery pt.1
trajectory for bariatric surgery pt.2
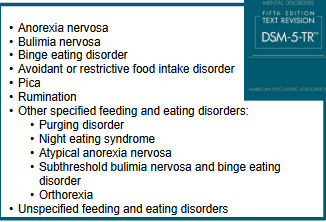
DSM description of feeding and eating disorders
a disorder characterized by a persistent disturbance of eating or eating-related behaviour that results in the altered consumption or absorption of food and that significantly impairs physical health or psychological functioning
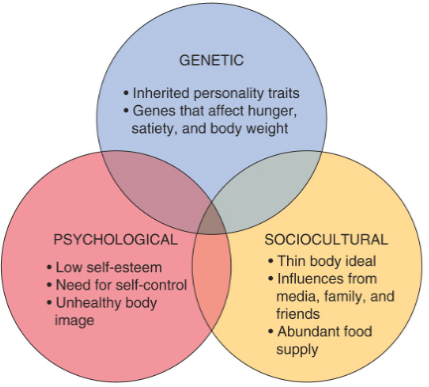
causes of feeding and eating disorders
psychosocial and sociocultural combine to develop a distorted body image
genetics can play a factor- ex personality traits (perfectionism, rigidity, narcissism…) “baseline” body type, hunger/satiety
often first appear in adolescence
physical, social and mental changes
desire for control during changes can manifest in control of food intake and weight
feeding and eating disorders in canada
PHAC: 3% of women will be affected by eating disorders in their lifetime (~1.7 million total)
CCHS: 3.8% of Canadian girls and women (aged 15-24) were at risk of an eating disorder
30% of grade 9-10 girls (~14 to 16 years old) report trying to lose weight in the last year
Incidence of eating disorders among boys and men is increasing (up to 1/3 of patients)
Early detection is important to refer for treatment – highest mortality of any mental illness (10 to 15%)
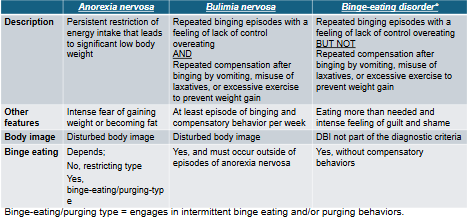
major feeding and eating disorders similarities and differences
anorexia athletica
“sport anorexia”
eating disorder characterized by excessive and compulsive exercise
not officially recognized by DSM-5 (patients likely classed as anorexia nervosa, R-type)
typically rooted in performance vs. body image concerns
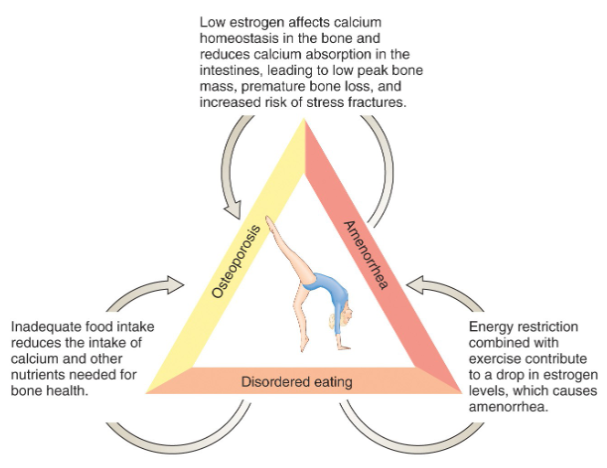
female athlete triad
disordered eating due to pressures to maintain lean, thin, and athletic bodies
energy restriction paired with excessive exercise can upset hormonal imbalance
low estrogen levels can lead to amenorrhea (stopping of menstruation)
low food intake and low estrogen can impact nutrient intake, especially calcium