PSYC 385 Classification and Assessment of Mental Disorders
1/41
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
42 Terms
Why classify?
1. To make sense of things ('nosology precedes
etiology' Raymond Cattell)
2.To assist in treatment decisions
3. To organize the search for new knowledge
Classification Systems:
DSM-5 (Diagnostic and Statistical Manual of Mental Disorders) and ICD (International Classification of Diseases) are the primary classification systems.
Features of the DSM-5:
- Based description rather than theory
- Divided into three sections:
- section i: introduction and use of manual
- section ii: 22 broad categories of clinical disorders
- section iii: emerging measures and models
- Harmonization with ICD system
In addition to being a compendium of mental disorders and diagnostic codes, the DSM-5-TR is also a written resource (descriptive text) about each mental disorder covering
- Diagnostic features
- Prevalence of a mental disorder (when known)
- Development and course of each disorder
- Risk factors
- Sex- and gender-related and cultural-related diagnostic
issues
- Association with suicide
- Differential diagnosis
- Comorbidity with other disorders
Major Innovations of DSM-5 (2013):
Addition and Modification of Disorders:
Some disorders were added (e.g., hoarding disorder), while others were reclassified (e.g., schizophrenia spectrum disorders, OCD moved to its own category).
Innovations of DSM-5 (2013):
Greater Alignment with ICD System:
DSM-5 aligned more closely with the ICD, making cross-system diagnoses easier.
Innovations of DSM-5 (2013):
Recognition of Age, Gender, and Culture:
There was increased focus on how these factors influence mental health.
Innovations of DSM-5 (2013):
Spectrum Disorders:
50 disorders were grouped into spectrum categories (e.g., autism spectrum, non-REM sleep disorders).
Innovations of DSM-5 (2013):
Replacement of “Not Otherwise Specified”:
The term was replaced with "Other Specified" and "Unspecified Disorders" to clarify diagnostic categories.
Innovations in DSM-5-TR (2022):
Prolonged Grief Disorder:
Added as a new diagnostic category, along with codes for suicidal behavior and non-suicidal self-injury.
Comparison of DSM Editions:
DSM-I (1952): Had 130 pages and classified 106 disorders.
DSM-IV-TR (2000): Expanded to 943 pages and 297 disorders.
DSM-5-TR (2022): Includes 947 pages, 158 disorders, with 80 classified as "other specified" or "unspecified."
Structure of a DSM-5 Diagnosis:
The most severe disorder (medical or mental) is listed first.
In cases of multiple diagnoses, the others follow in order of severity or impact on quality of life.
Comments include psychosocial, cultural, and other relevant issues.
Example diagnosis format:
C02.9 T2 N0 M0 Stg III squamous cell carcinoma of the base of tongue
300.4 (F34.1) persistent depressive disorder (dysthymia)
303.90 (F10.20) alcohol use disorder, moderate
304.90 (F12.20) cannabis use disorder, moderate
other factors: V61.03 (Z63.5) disruption of family by divorce (two years ago); V62.5
(Z65.0) conviction in criminal proceedings without imprisonment: probation
includes medical conditions, mental disorders, and relevant psychosocial factors.
Syndromes:
Clusters of symptoms make up syndromes.
Polythetic Criteria:
A disorder is diagnosed by meeting a certain number of symptoms from a larger set (e.g., 5/9 symptoms for major depression).
Exclusion Criteria:
Must rule out symptoms due to other causes (e.g., substance use, medical conditions).
Duration:
Disorders are often diagnosed based on how long symptoms have been present.
Personal Distress:
Mental disorders often involve significant personal distress or impact on others.
Dysfunction:
Disorders cause dysfunction in daily life or significant distress to the person or others.
Diagnostic Criteria for Schizophrenia:
A: Requires two or more symptoms (delusions, hallucinations, disorganized speech, disorganized or catatonic behavior, negative symptoms) for at least one month.
B: Must impair one or more areas of functioning (e.g., work, relationships).
C: Continuous signs must persist for at least 6 months, including one month of active symptoms.
Exclusion Criteria: Other disorders like schizoaffective disorder, bipolar disorder, or conditions caused by substance use must be ruled out.
Reliability: The consistency of a diagnosis (e.g., whether different clinicians reach the same diagnosis).
Inter-rater Reliability: Consistency across different raters.
Test-Retest Reliability: Consistency over time.
Validity: Whether the diagnosis measures what it’s supposed to measure.
Concurrent Validity: Diagnosis agrees with other relevant assessments.
Predictive Validity: Ability of the diagnosis to predict future outcomes or behavior.
Unresolved Issues in DSM-5:
Scientific Basis of DSM-5: The DSM-5’s definitions and criteria for mental disorders are not always scientifically sound.
Criticism of DSM-5 Research: The research behind the DSM-5 categories includes weak justifications for some disorders.
Symptom Count: The specific number of symptoms required to diagnose a disorder is sometimes arbitrary.
Time Periods for Diagnosis: The periods for which symptoms must last (e.g., 6 months) to meet diagnostic criteria are also seen as arbitrary.
Further Issues with DSM-5:
Inter-rater Reliability: There is often inconsistency in the diagnoses given.
Categorical vs. Dimensional Approaches: Some argue a dimensional approach based on how much an individual deviates from the norm (rather than whether they meet a fixed number of criteria) is better.
Comorbidity: The simultaneous occurrence of multiple disorders is another issue. Some question whether it is due to over-classification of similar conditions or if it reflects valid co-occurrences.
Historical Information: Poor use of longitudinal or historical information when diagnosing disorders.
Social and Political Issues:
Pathologizing Normal Behavior:
Behaviors that are culturally or personally acceptable can be pathologized under the DSM-5. This creates controversy, particularly around what society deems "normal."
Social and Political Issues:
Stigma:
Labeling someone with a mental disorder can contribute to significant stigma, both within society and for the individual.
Psychological Assessment
Process: The collection and interpretation of information to understand another person.
Goals:
1. Make predictions about behavior or outcomes.
2. Plan interventions to address issues.
3. Evaluate the success of interventions.
Major assumptions about behavior:
1. There is consistency in behavior
2. Different levels of analysis may be used depending on questions that need to be addressed
3. Assessment procedures vary in usefulness depending on cases
Six possible sources of information on an individual's personality:
- The psychological interview (unstructured, structured, semi-structured)
- Peer and 'significant others' reports
- Behavioral observation and ratings
- Cognitive and neuropsychological testing
- Personality tests and self report inventories (MMPI-3, MCMI-IV, PAI, symptom
specific questionnaires)
- Projective tests
Types of projective techniques
Association (Rorschach Test):
Identifying thoughts and feelings through the interpretation of inkblots.
Types of projective techniques:
Construction (Thematic Apperception Test):
The individual is asked to create stories based on ambiguous images, revealing underlying thoughts and feelings.
Types of projective techniques:
Sentence Completion Tests:
The person completes sentence stems, revealing thoughts, beliefs, and desires.
Types of projective techniques:
Artistic Expression:
Drawing or other creative tasks can provide insight into personality.
Assessment of social systems:
Assessing families/groups to understand the dynamics that influence individual behavior.
Assessment of biological systems:
Includes psychophysiological assessments, often utilizing brain imaging techniques such as CT scans, MRI, and PET scans.
Controlled Experimental Research:
This includes clinical trials and laboratory research to test hypotheses in a controlled setting.
Quasi-experimental Methods:
Studies where participants aren't randomly assigned to conditions, often due to practical or ethical constraints.
Non-experimental Methods:
These include correlational studies, case studies, and single-subject research.
Epidemiological Research:
Studies that investigate the prevalence and incidence of disorders in populations.
Heritability Studies:
Investigating the genetic basis of disorders through family, adoption, and twin studies.
Evaluating Research in Abnormal Psychology:
Statistical Significance: Determines whether the findings are likely to have occurred by chance.
Clinical Significance: Measures whether the findings have real-world, meaningful effects on individuals’ lives.
Normative Comparisons: How the findings compare to normal, healthy populations or accepted standards.
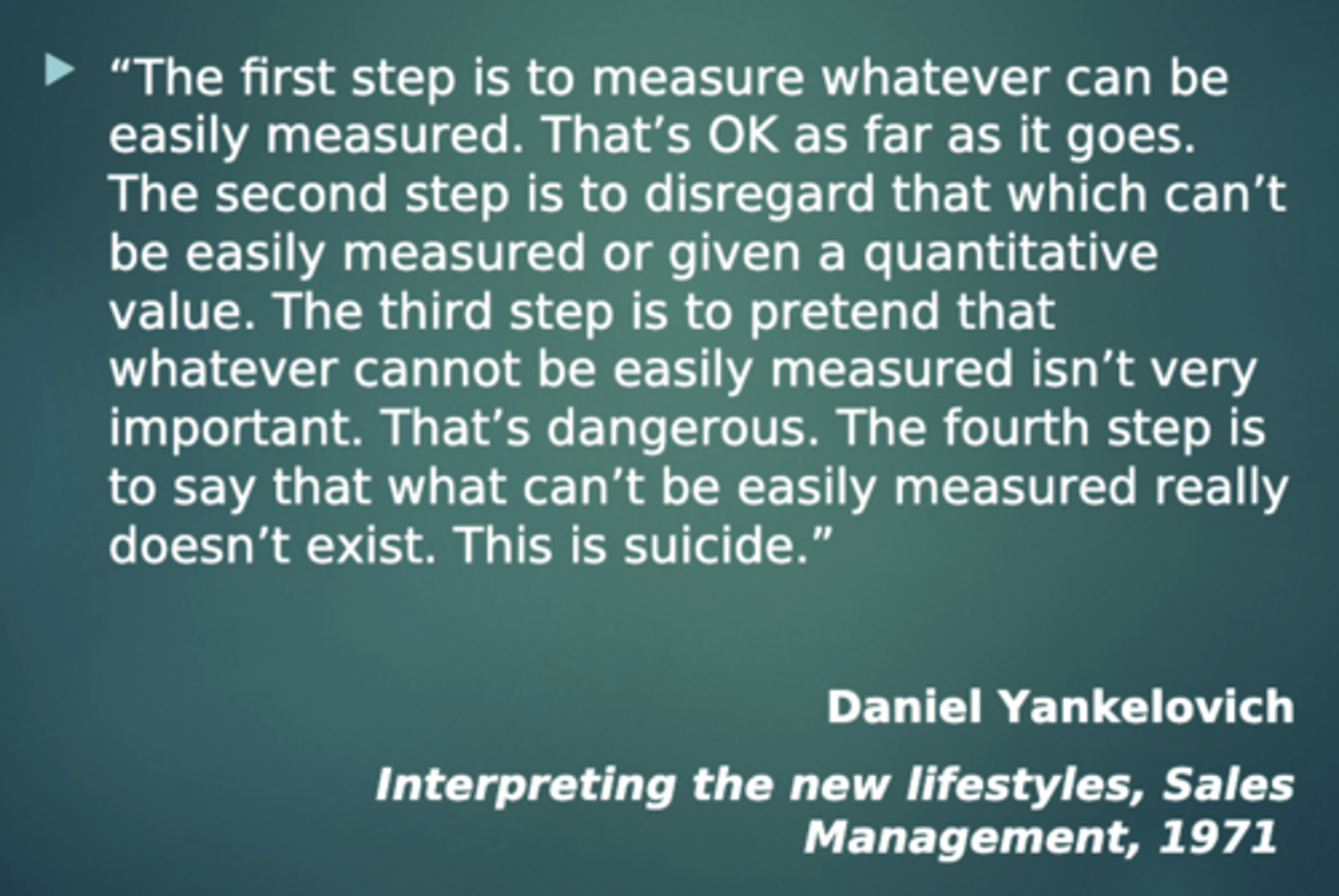
The McNamara fallacy (AKA the quantitative fallacy) highlights the danger of relying solely on measurable data. It progresses through four steps:
1. Measure what can be easily quantified.
2. Disregard what can't be easily measured.
3. Pretend what can't be measured isn't important.
4. Deny the existence of things that can't be measured.