Endocrine disorders - The Adrenal Gland: Hyperadrenocorticism 'Cushings'
1/24
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
25 Terms
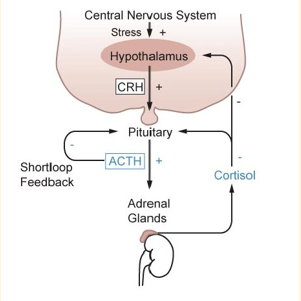
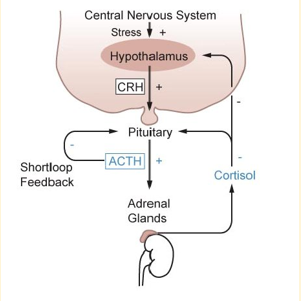
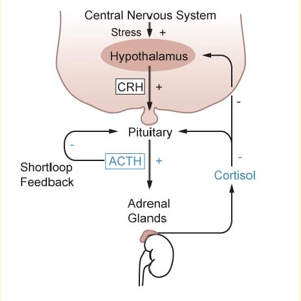
HPA axis
Hypothalamic-Pituitary-Adrenal
Cortisol goes around the body

Cushing’s Disease (HAC) (common in dogs > cats)
Can be:
Pituitary dependant hyperadrenocorticism (PDH)
Adrenal dependant hyperadrenocorticism (ADH)
Iatrogenic hyperadrenocorticism

Pituitary dependant hyperadrenocorticism (PDH) is often due to a tumour ..
This tumour releases ATCH → leads to increased cortisol
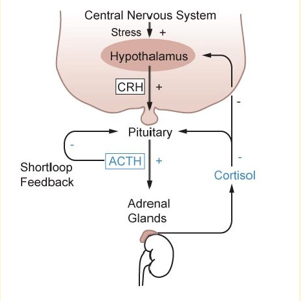
Adrenal dependant hyperadrenocorticism (ADH)
Patient has too much cortisol

Iatrogenic hyperadrenocorticism
Something we’re given to the patient, for example, steroids
Predisposing factors for HAC - Pituitary
Smaller breeds
Middle aged-older animals
more common (80-85%)
Predisposing factors for HAC - Adrenal
Larger breeds
Older animals
Females > males
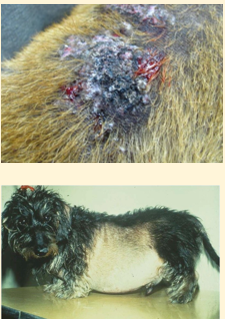
Clinical signs of HAC
PU/PD/PP
Pot-bellied appearance
Muscle wasting and weakness
Lethargy & panting
Dermatological changes (calcinosis cutis)
Alopecia - bilaterally symmetrical, normally on the trunk
Diagnosis of HAC - Haematology
Stress leucogram (SMILED)
Segmented neutrophils and Monocytes → Increased
Lymphocytes and Eosinophils → Decreased
Diagnosis of HAC - Biochemistry
Raised ALP/ALKP +/- cholesterol and glucose
Diagnosis of HAC - Urinalysis
SG <10.10 (low SG due to drinking lots)
Elevated urine cortisol:creatinine ratio (UCCR) - screening test
Diagnosis of HAC - Imaging
Ultrasonography - hepatomegaly, enlarged adrenal glands, neoplasia
CT - smaller neoplastic lesions
Urine cortisol:creatinine ratio
Penitents with cushings will have cortisol in their bloodstream and this is excreted in their urine
A negative (or low) UCCR rules out cushings
A positive (or high) results means the diagnosis remains a possibility
Stress should be minimised during sampling (free catch at home in the morning is best)
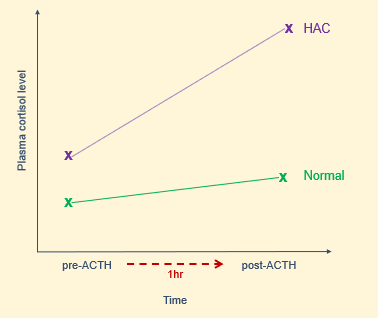
ACTH stimulation test - HAC
This test has high specificity but variable sensitivity. This means a low likelihood of false positives but potential for false negatives - especially ADH.
Fasted blood sample for baseline cortisol
Inject synthetic ACTH IV
Repeat cortisol blood sample 1hr later
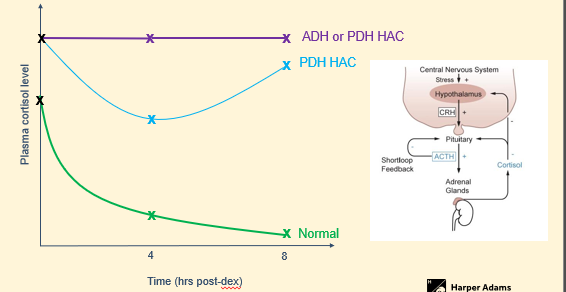
Low dose dexamethasone suppression test process
Blood sample for baseline cortisol
Inject 0.0mg/kg dex IV
Repeat cortisol blood sample 4hr and 8hr later
Low dose dexamethasone suppression test
High sensitivity (means false negatives are rare), but lower specificity (means false positives are common)
Given steroid will inhibit ADH and ACTH
Lost negative feedback loop (adrenal) or in pituitary (have a negative feedback loop) can be used to determine which one it is so a tumour could be removed
Diagnostic tests - screening tests
UCCR urine test
ACTH stimulation test
Low dose dexamethasone suppression test
Diagnostic tests - differentiating tests
Low dose dexamethasone suppression test
High dose dexamethasone suppression tests (rarely used)
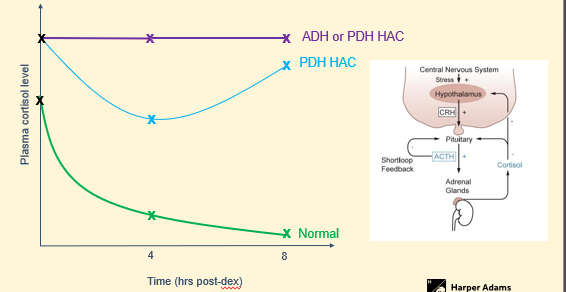
High dose dexamethasone suppression test
High-dose dexamethasone suppression (HDDS) is indicated for use in dogs already diagnosed as having hyperadrenocorticism where no suppression is seen on the LDDS at 4 and 8 hours.
Suppression during an HDDS test, in dogs already diagnosed as having hyperadrenocorticism, is consistent with pituitary-dependent hyperadrenocorticism.
Failure to suppress could occur with both pituitary-dependent or adrenal-dependent hyperadrenocorticism and further diagnostics would be necessary to differentiate (e.g. abdominal ultrasound).
High dose dexamethasone suppression test - protocol
Collect a baseline blood sample (1-2 ml in a plain/gel tube). o Inject 0.1 mg/kg of dexamethasone intravenously, via IV catheter.
Collect the second blood sample (1-2 ml in a plain/gel tube) 4 hrs post-injection.
Collect the third blood sample (1-2 ml in a plain/gel tube) 8 hrs post-injection.
Ensure the samples have clotted and centrifuge the samples 30-120 minutes after collection.
For samples collected in plain tubes, please separate the serum into another plain tube (this step is not necessary for samples collected in gel tubes).
Please label all tubes with the patient’s name and the time of sampling.
Please include the patient history, including drug history, on the request form.
Submit the separated serum samples and the request form to the reference laboratory (Test code DEXH).
Cortisol will be measured in all three samples.
Medical treatment of HAC
Tristan (vetoryl)
Regular ACTH stimulation/biochemistry/lytes at 10d/4w/12w
Can use pre-vetoryl cortisol
Can do a blood sample pre-administration to gain baseline
Surgical treatment of HAC
Adrenalectomy
Hypophysectomy
Triolstane
Antagonist of the enzymes involved in cortisol production - blocks the production
This lowers cortisol levels which resolves clinical signs in the patient - polyphagia, polyuria/polydipsia will be relatively quickly, coat changes will take months
Trolstane - pharmacology
Pharmacokinetics variable so dose needs to be tailored to the individual - based on weight
Administered orally and presence of food enhances bioavailability - should be given with food
Risk of iatrogenic hypoadrenocorticism if overdosed - can be more prevalent in smaller patients due to tablet sizes - cannot get smaller sizes or be split in half
Nursing care of the cushingoid patient
Minimise stress during procedures (increase cortisol)
Ensure water availability (PD) - can become dehydrated quicker than a normal patient would
Regular toileting opportunities (PU)
Care with venepuncture
Owner support and education