skinner
1/132
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
133 Terms
what is the #1 cause of death for animals?
cancer
what does distal metastasis indicate?
systemic neoplasia
what is a common location for metastasis to occur from the primary site of a tumor?
the draining lymph node
what is the burden of neoplasia on a patient?
can impact how a patient feels based on the substances produced by the mass
if a mass rapidly changes from small → large, what are we more concerned about?
that this mass is a malignant form
what is key information from the PE that can help narrow down the dx of a mass?
tissues involved
movable or adhered
painful to touch?
pt BCS
location
are skin or SQ masses “actually” encapsulated?
no, a pseudocapsule tends to form, therefore they are not actually limited to a local area
why is it so important to ID what type of tumor it is?
so we can understand prognosis and extent that the tumor is present to make a plan of action
what is the reactive zone of a mass?
the zone around the tumor where the immune system is interacting with it
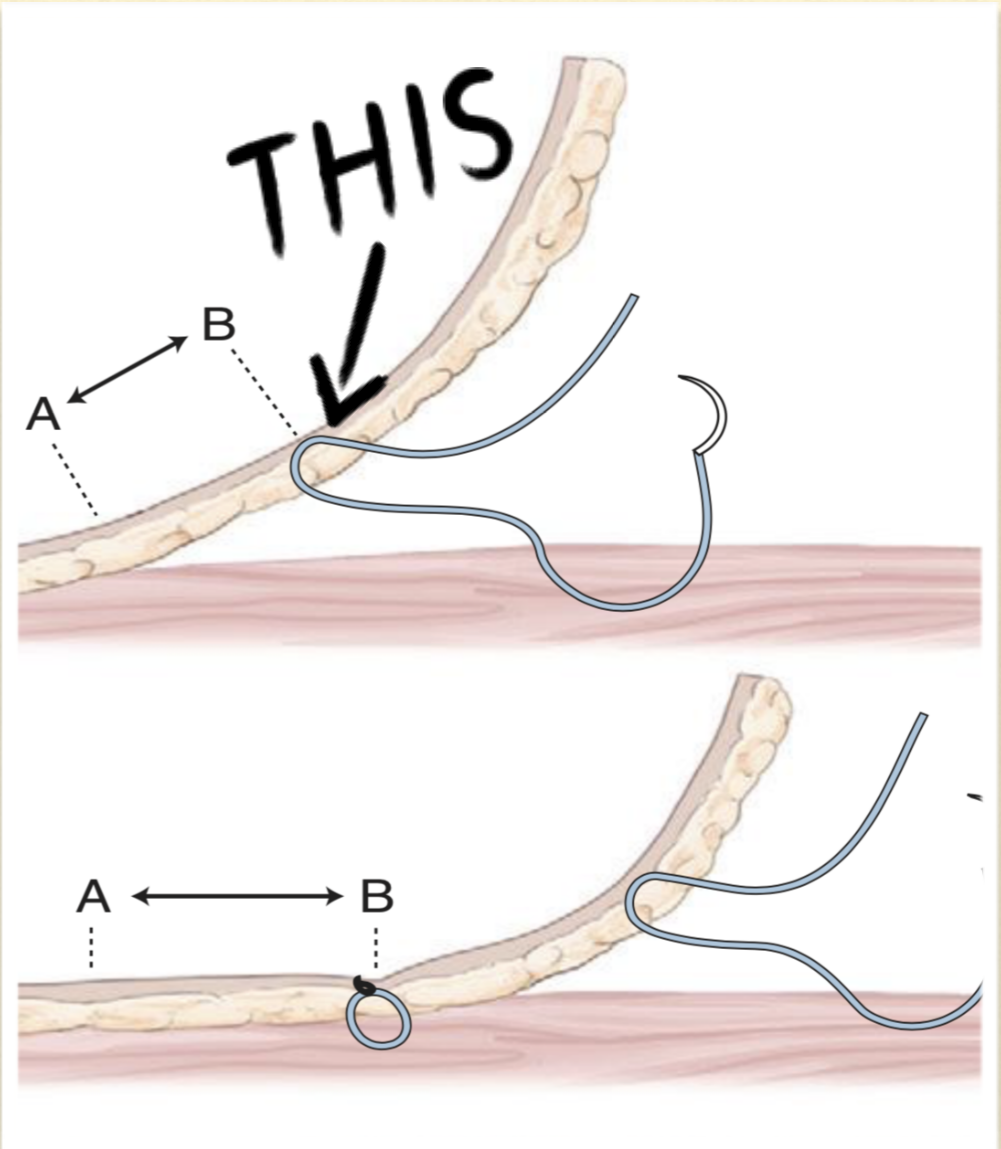
is this mobile or fixed?
mobile
is this mobile or fixed?
fixed
what is the major concern when a tumor is presenting as fixed?
we don’t know how far the tumor goes inward in the body and how many structures it is actually interacting with
what are the techniques we use to dx a mass?
aspirate → poke with a stick
body map
ultrasound guidance → for deeper aspirations
biopsy → will given definitive dx
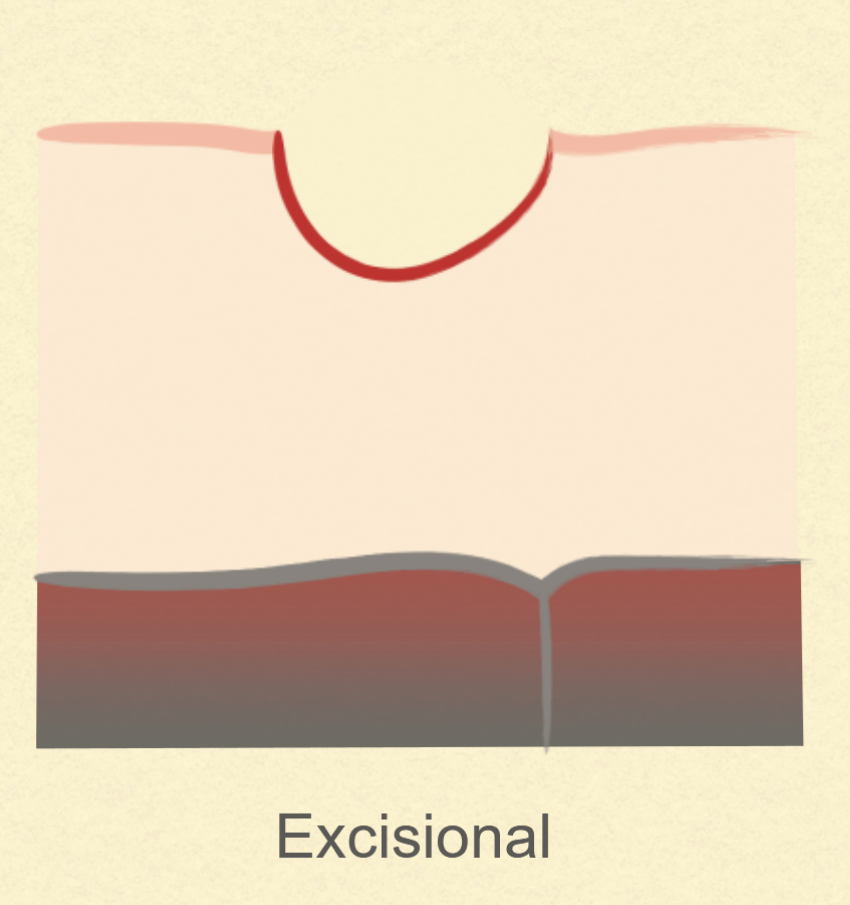
what are the two biopsy techniques?
incisional
excisional
what is incisional biopsy?
taking out a chunk of the mass to send out
get more reliable info without disturbing the margins of the tumor
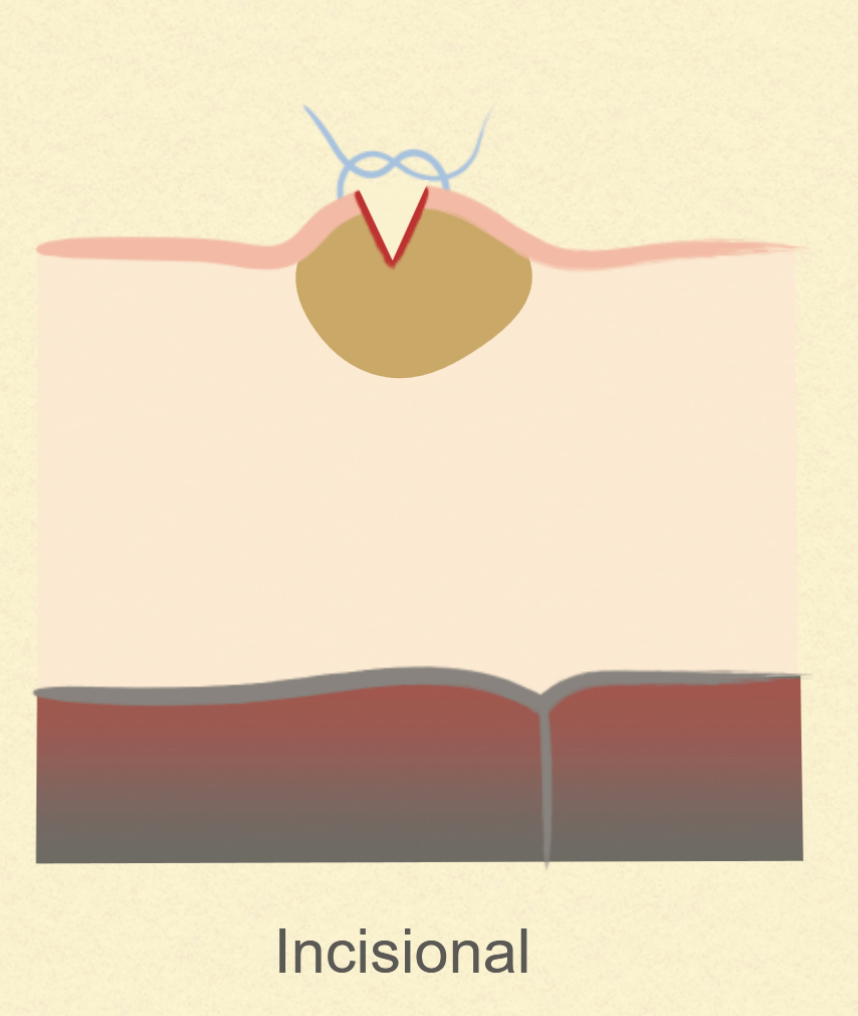
what is excisional biopsy?
removing the entirety of the mass and sending it
this can be therapeutic → however commits to an approach of dealing with the mass before knowing exactly what it is
this method messes with the margins of the mass → letching potential cancer cells into neighboring tissues
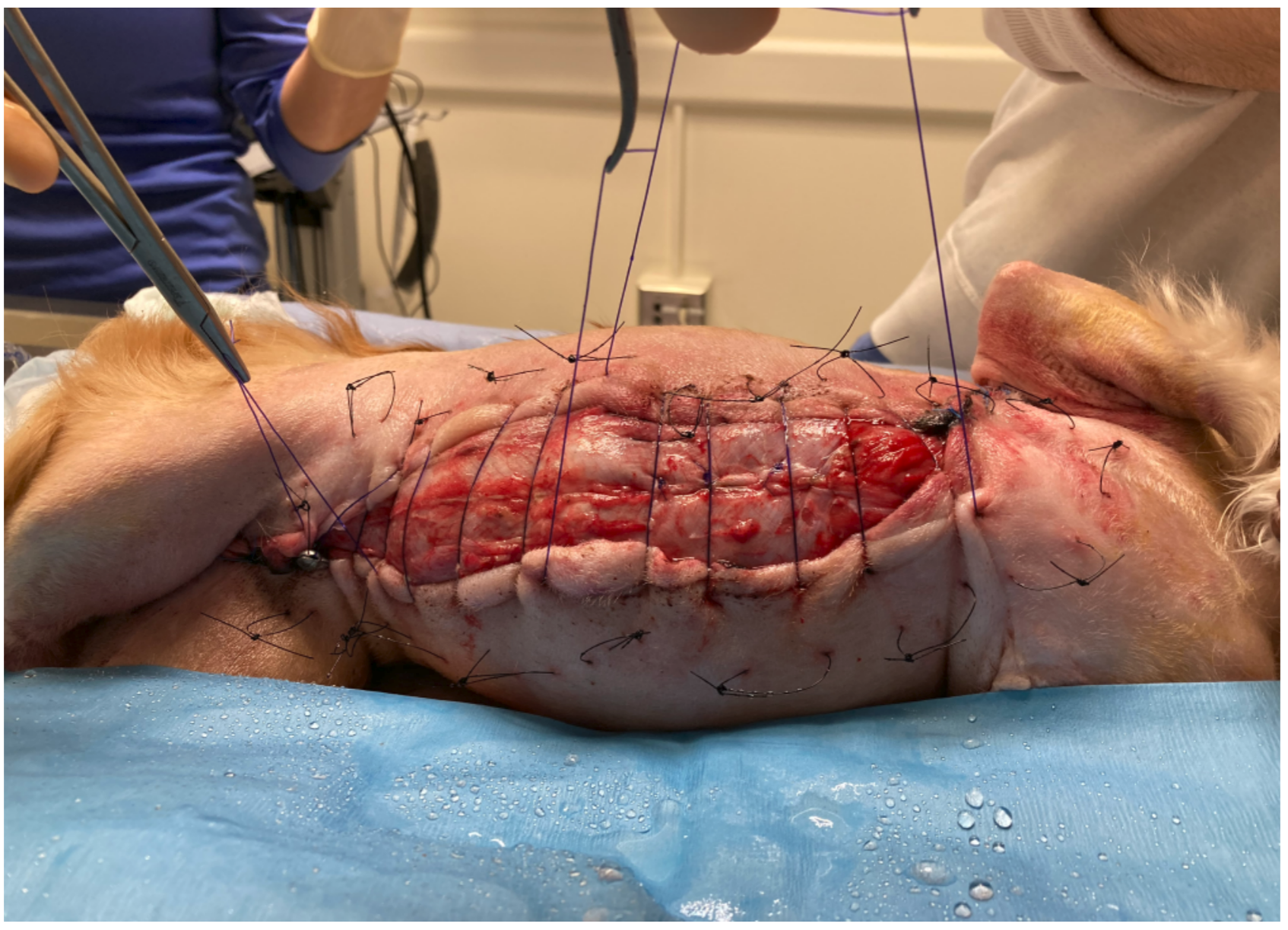
if you suspect feline injection site sarcoma, how should you biopsy it?
you should ONLY ever use incision because it is super aggressive and excisional can make it far worse condition
what are the pros and cons of biopsy?
pros
allows more definitive dx
better planning
cons
two procedures will need to be done = 1 for biopsy + 1 for removal once dx comes back
may increase risk of recurrence → seeding the biopsy track with cancer cells
what are the two types of incisional biopsy methods?
punch biopsy → great for skin/SQ masses
wedge biopsy →
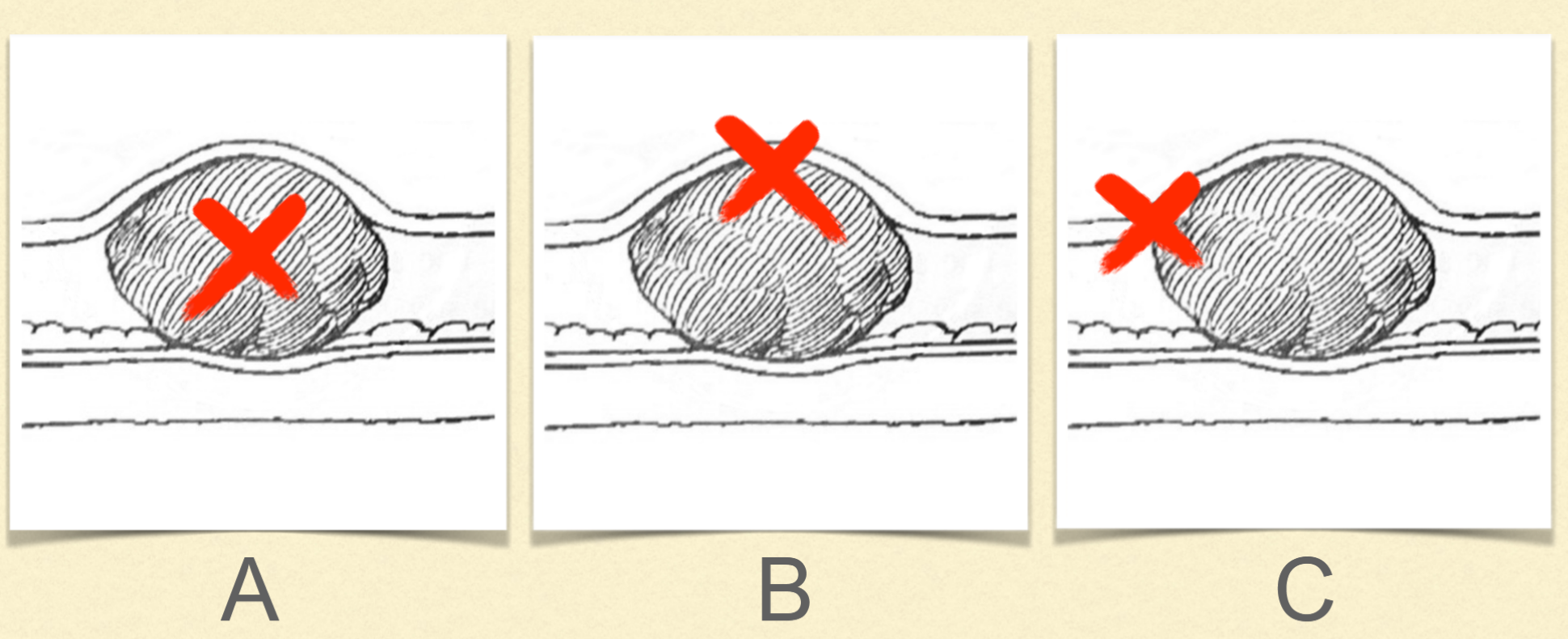
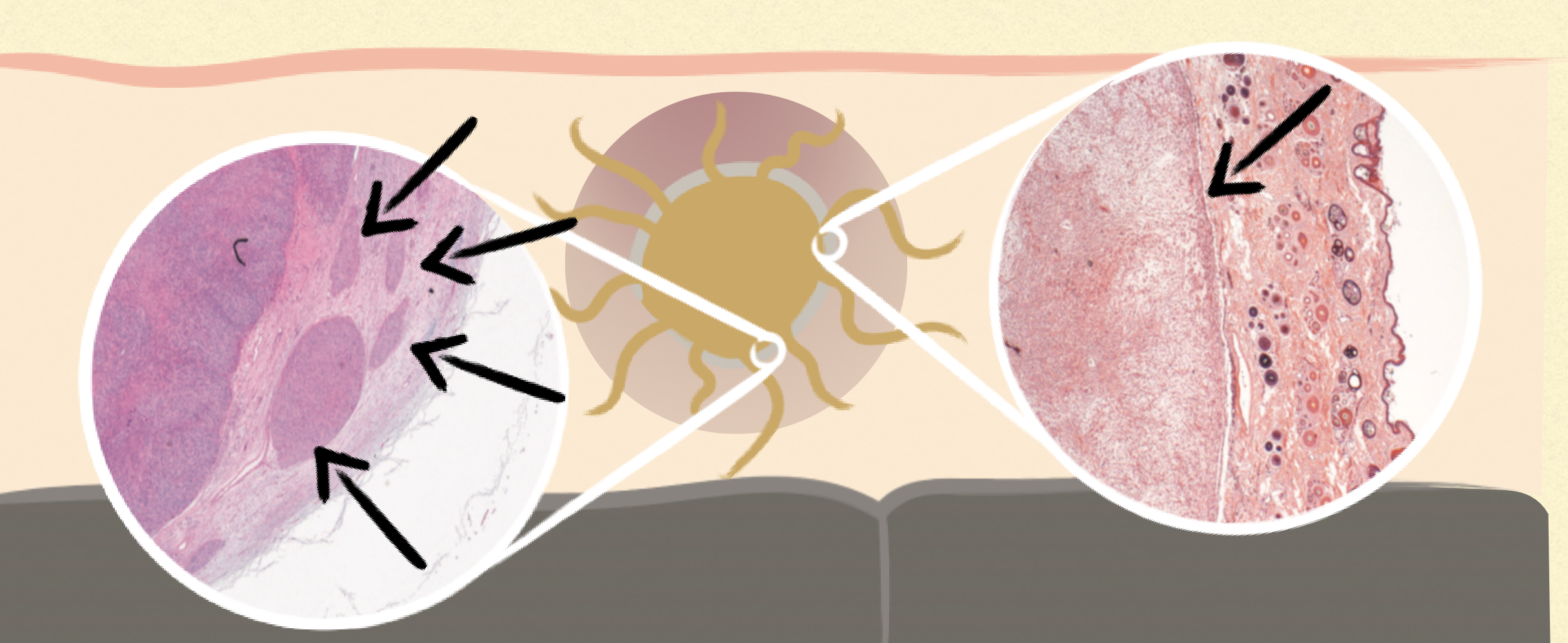
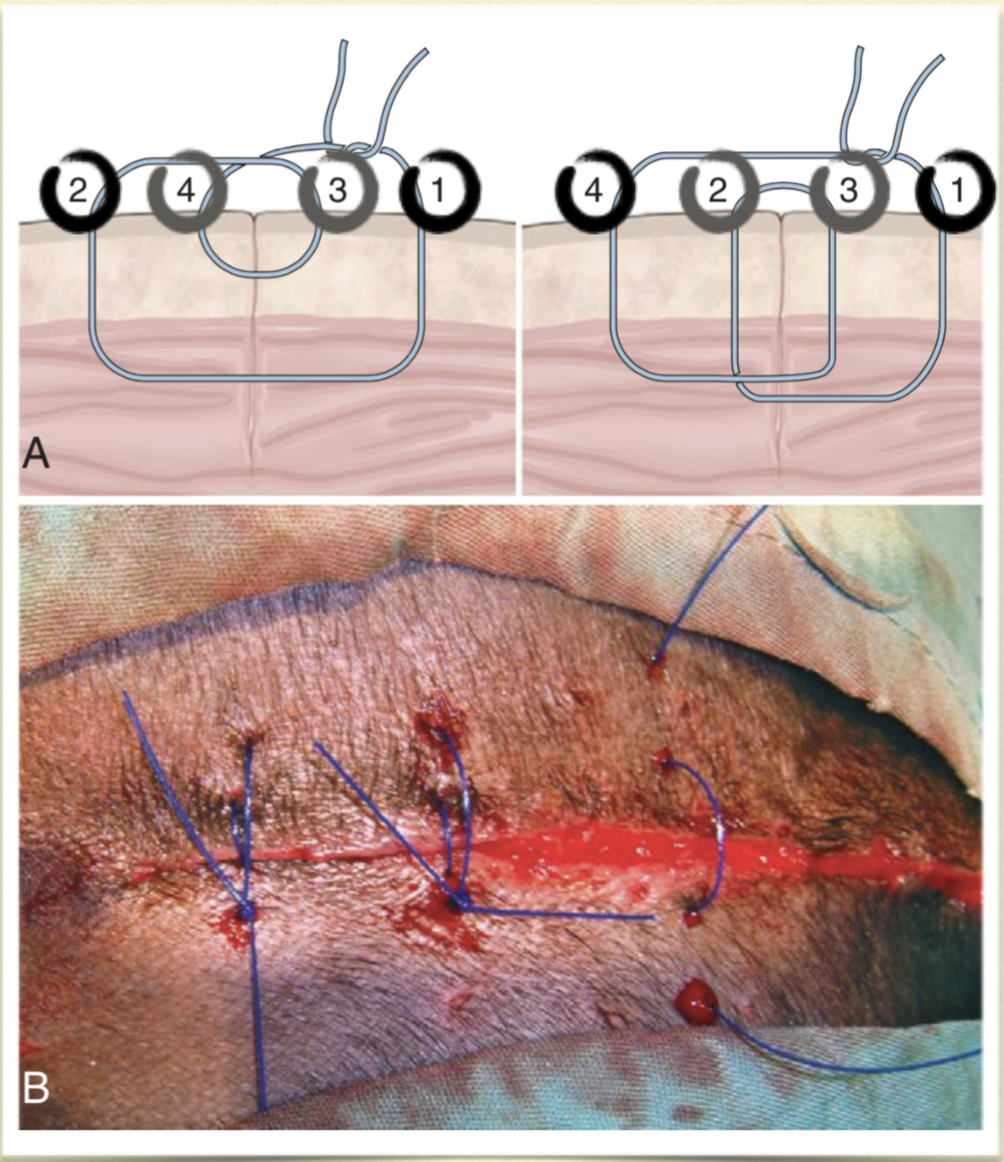
pick the best area to biopsy from?
B
when would excisional biopsy be preferred to incisional?
no benefit of pre-op biopsy
potential for hemorrhage
easy curative resection
**potential for seeding**
what are examples of excisional over incisional?
thyroid
lung mass
intestine
splenic
what if we don’t get good margins with the first surgery?
must take HUGE margins to be safe if any spread occurred from aggravating the mass
what are the % of pre-op diagnosis of masses?
cytology = 17%
incisional biopsy = 4%
if we know what we are dealing with before committing to surgical removal, we can have better prognosis outcomes
what are the two forms of metastasis?
vascular spread
lymphatic spread
what is staging of neoplasia?
define extent of the disease
tumor-specific
BEFORE major intervention
generally, more involved = greater stage
how can lymph nodes be helpful in staging/dx of a cancer?
palpation not senstive
aspirates are 66% sensitive
CT is 12% sensitive
sites of drainage are variable
can use contrasts to see where draining may occur
in what 2 cancers can lymphadenectomy be beneficial?
AGASACA
MCT
what are the two forms of surgical intent with masses/tumors?
palliative or curative
what are the questions we should ask ourselves before surgical management of a mass/tumor?
can this disease be cured or managed with surgery?
can I manage this disease with surgery? = do I have the skills/equipment necessary
what effects will resection have if full removal can’t be achieved?
is (neo)adjuvant therapy helpful? → chemo
when planning surgery for onco, we need to?
make a plan for both resection and closure based on the margins we need to achieve
what are the enneking classificaiton of surgical margins?
intralesional
marginal
wide
radical
what are intralesional margins?
taking out bits of the tumor, not used much
more likely in neuro
what are marginal margins?
just taking out the tumor whole
not for infiltration
when is marginal margins considered?
benign/low-grade lesions → low risk of reccurrence
anatomically encapsulated masses
adjuvant therapy
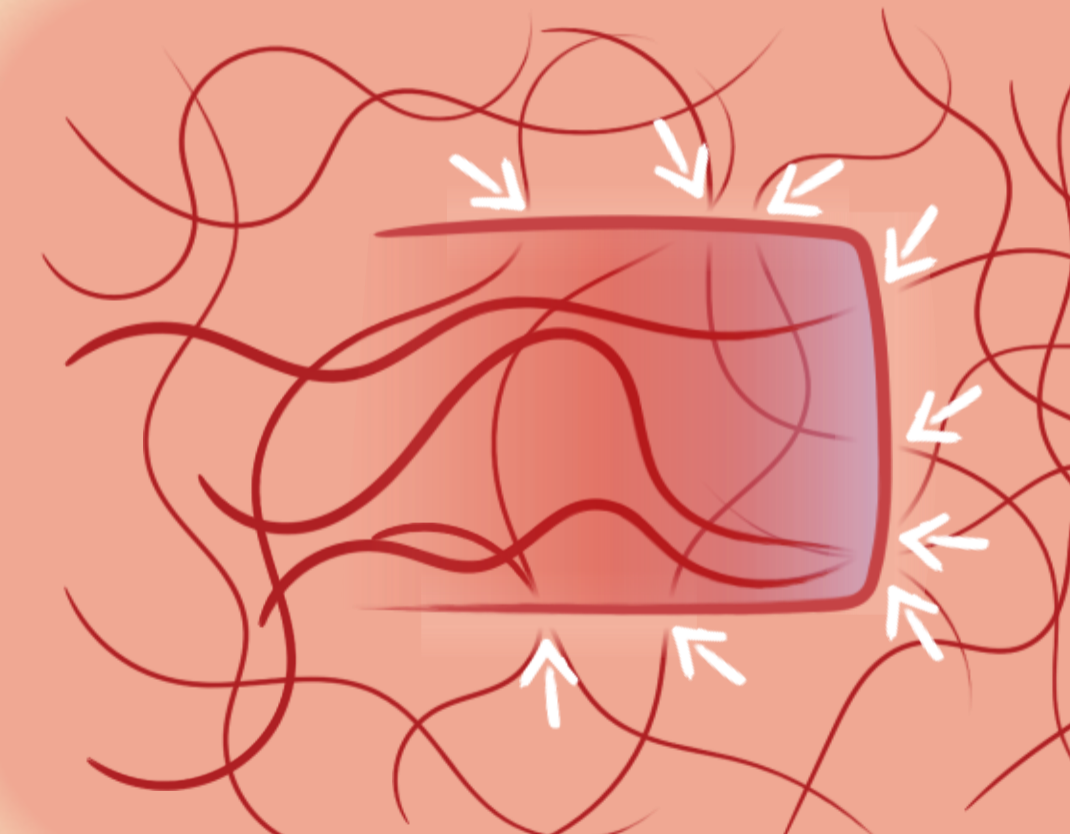
what are wide margins?
taking out disease and its possible extensions from the main tumor in the surrounding tissues
often 2-3 cm lateral margin
fascial plan deep
if you can’t go deep don’t go ____
wide
what are radical margins?
taking the entire body part that the tumor is involved with
5 cm lateral
2 fascial planes deep
what is considered a fascial plane?
fascial sheet
muscle
bone
body wall
when is a revision necessary?
when incomplete margins occur
what are surgical considerations that need to be addressed pre-op?
clip WIDE
plans for management of site
check availability of skin for closure
during surgery, what are the considerations that need to be made?
treat cancer like infection and DO NOT SPREAD IT
change gloves and instruments when working on multiple sites
take care with drains → close to main site
how do submit a sample of a mass?
leave ink margins if relevant → help to prove that all was removed
formalin = 10:1
framing notes that give details of patient and condition
after onco sx, what do you do?
follow up with client and patient
further treatment may be necessary based on what submission report says
what is primary wound closure?
surgical closure of a wound that has edges apposed and will heal by 1st intention healing
what are the main goals of wound closure?
closure
no complications
cosmesis
what are required to achieve the goals of wound closure?
planning and proper technique
primary wound closure
close a site right after it is damaged
delayed primary closure
delaying when to close a wound but closing before any granulation tissue forms
secondary closure
manage a wound open until it is clean and healthy with granulation tissue to then close
second intention healing
leaving a wound to close overtime on its own
what are Halsted’s 7 principles of surgery?
1) strict aseptic technique
2) gentle tissue handling
3) meticulous hemostasis
4) preservation of blood supply
5) obliteraction of dead space
6) accurate anatomic apposition
7) minimisation of tension
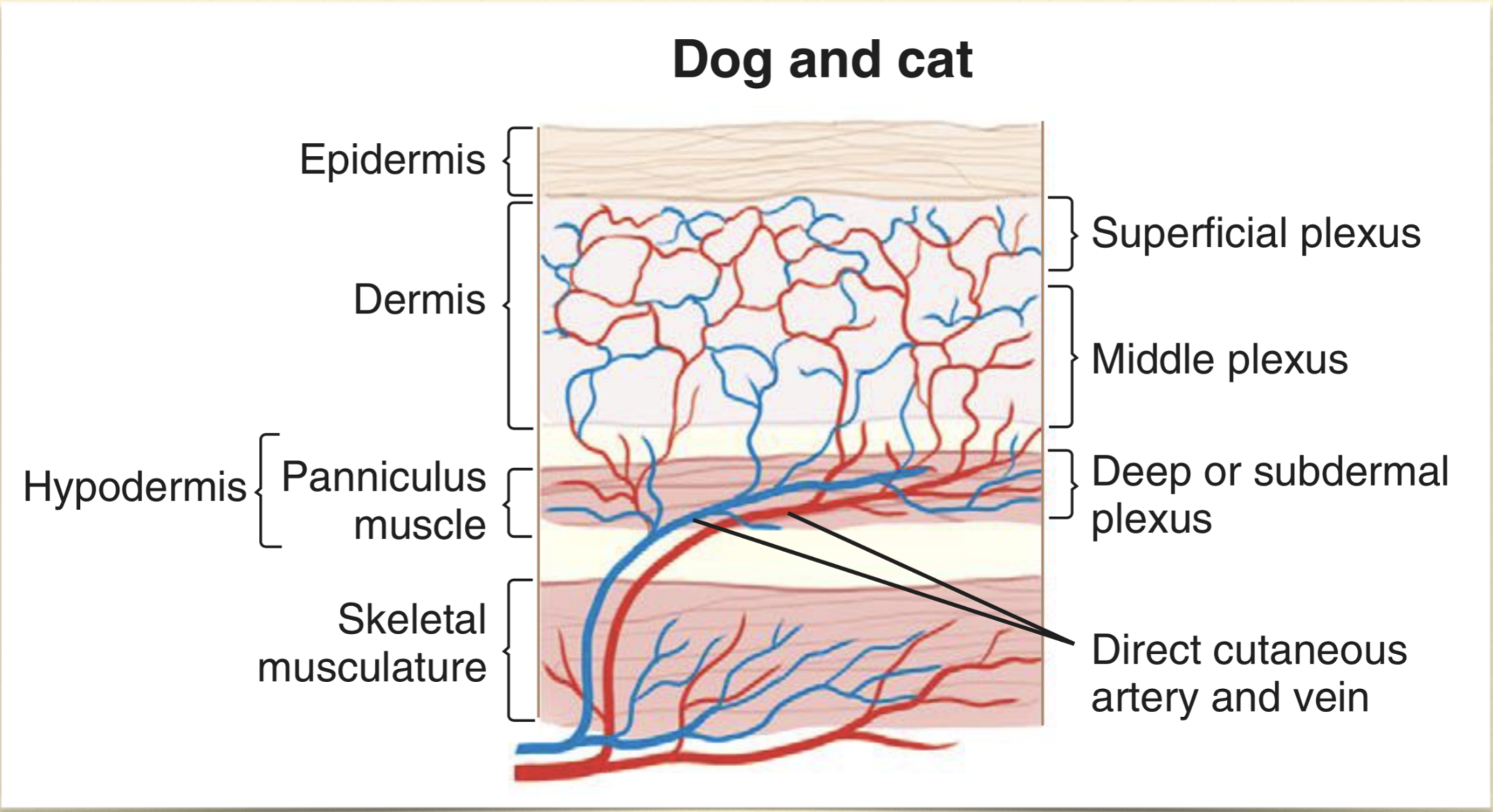
what area of tissue that supply blood to skin and SQ tissues?
deep or subdermal plexus
why to use primary closure?
simple
rapid wound healing
reduce pain
minimise scarring
protect underlying tissues
cosmesis?
cost? → may be less than second intention healing with visits and bandage changes
what are the patient characteristics that you must consider when deciding on how to close a wound?
systemic condition
immunosuppression → reduced wound healing, more prone to infection
metabolic disease → reduced wound healing = diabetes or cushings
cancer
radiation → causes delayed healing
temperament
species?
what are the wound factors that must be considered when deciding on how to close a wound?
location → higher area or contamination or highly mobile area?
configuration → is it even possible to close this?
tension
blood supply → a traumatic wound can have degloving that doesn’t declare itself for a number of days
what contamination levels are okay to close?
clean and clean-contaminated
what type of contamination is questionable to close?
contaminated wound → your judgement call/ on a case by case basis
how long does it roughly take for bacteria to grow enough in a wound to produce infeciton?
6 hours
what is the level of growth in bacteria that can occur in 6 hours?
105 bacteria per g tissue
what other wound factors can cause you to question whether to close or not?
extent of tissue trauma
tissue loss
crushing/shearing/burn
lag time
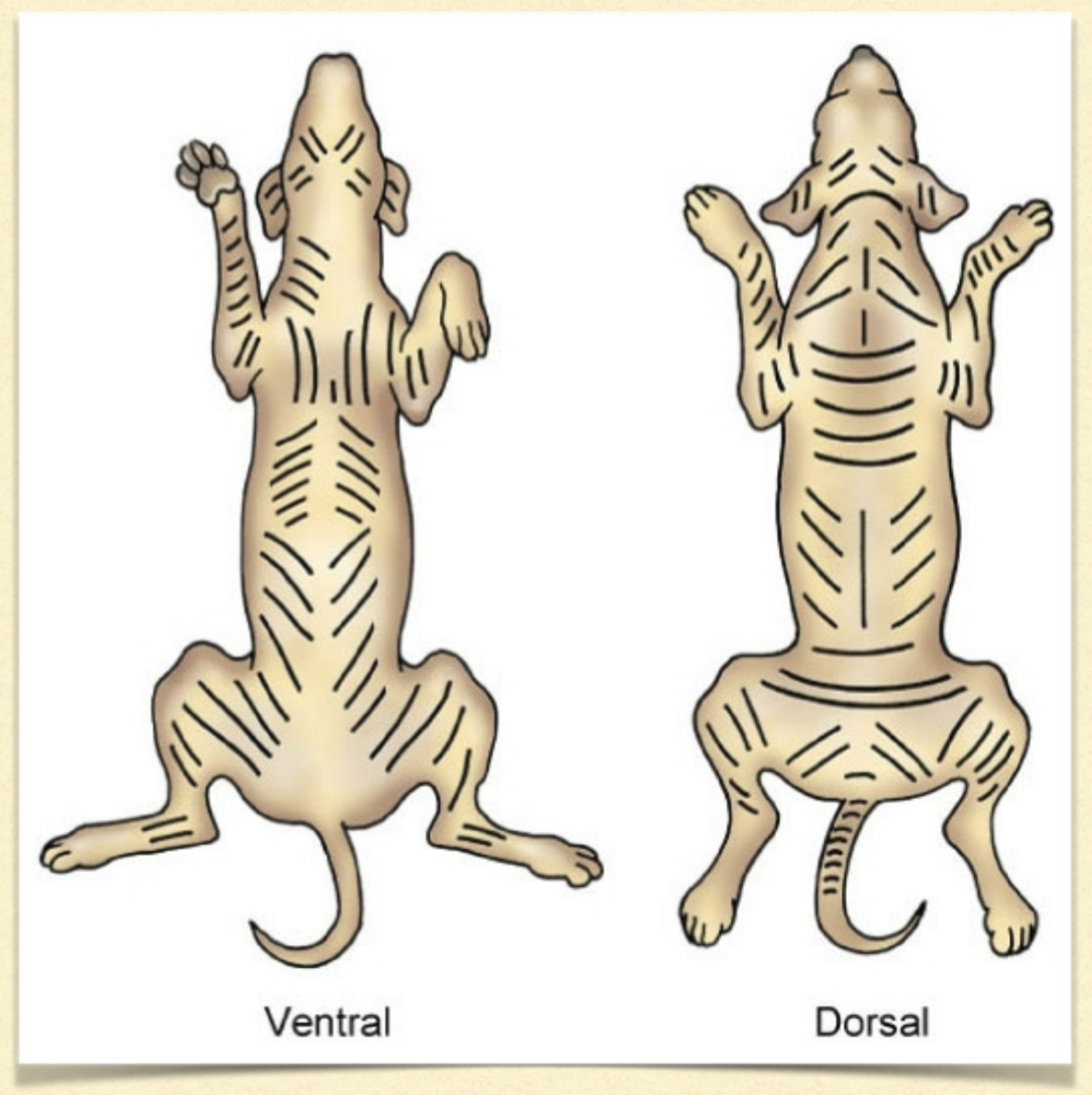
what is the general guidelines of skin tension lines?
on trunk = tension runs parallel
on limbs = perpendicular
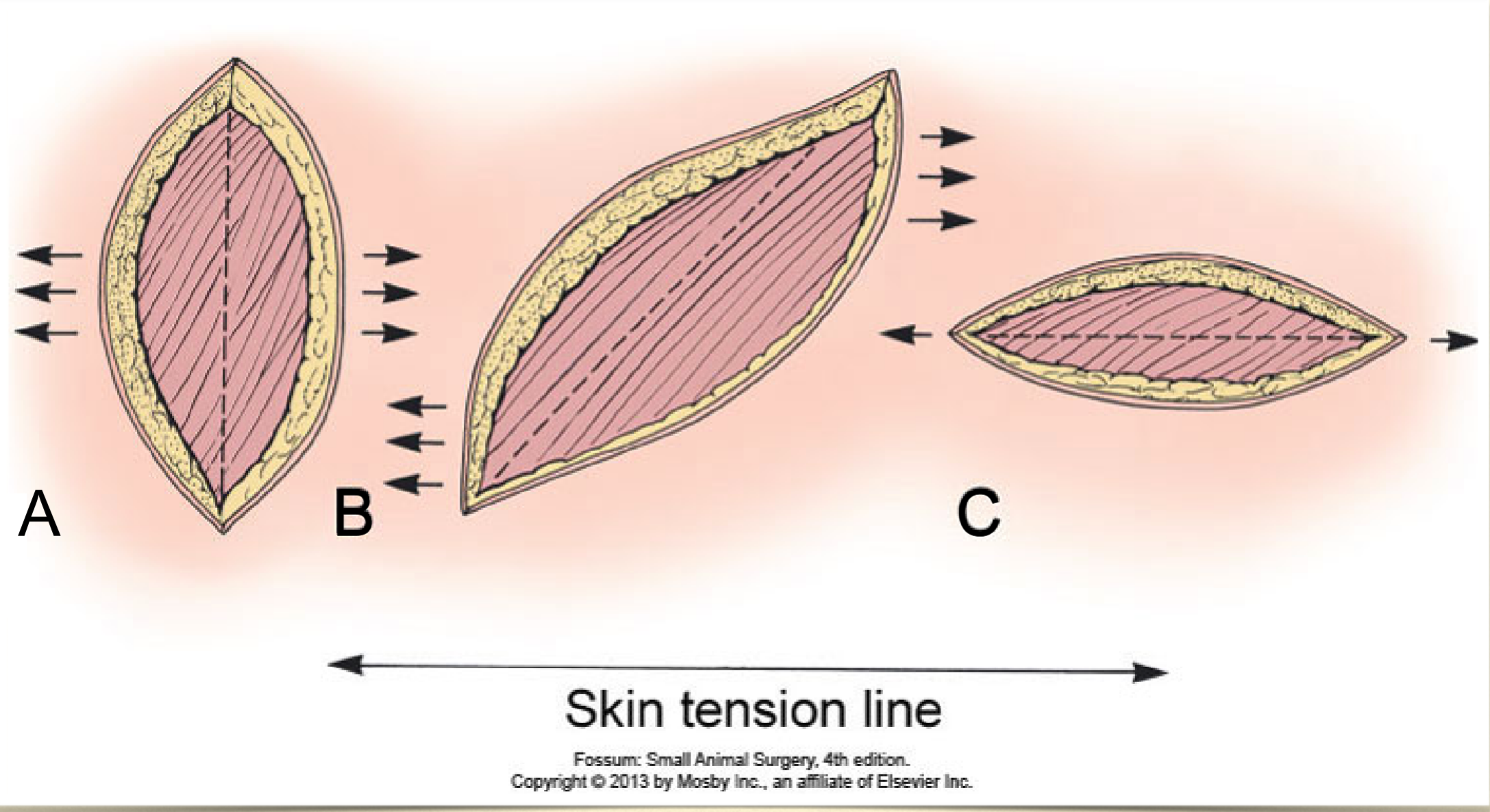
in what oriention to the tension lines do you want to close a wound?
parallel to tension lines
how to help to promote apposition with deep lesions?
multiple layer closures
muscle movement can be used to decrease space superficially
what do we want to use to create good apposition of the SQ?
distribute tension
decrease dead space
cruciate or mattress sutures
can also take wider bites that and into the fascial plane
can then add an additional suture in the skin to fully close - intradermal
continuous horizontal intradermal pattern
~50% overlap of bites
small bites
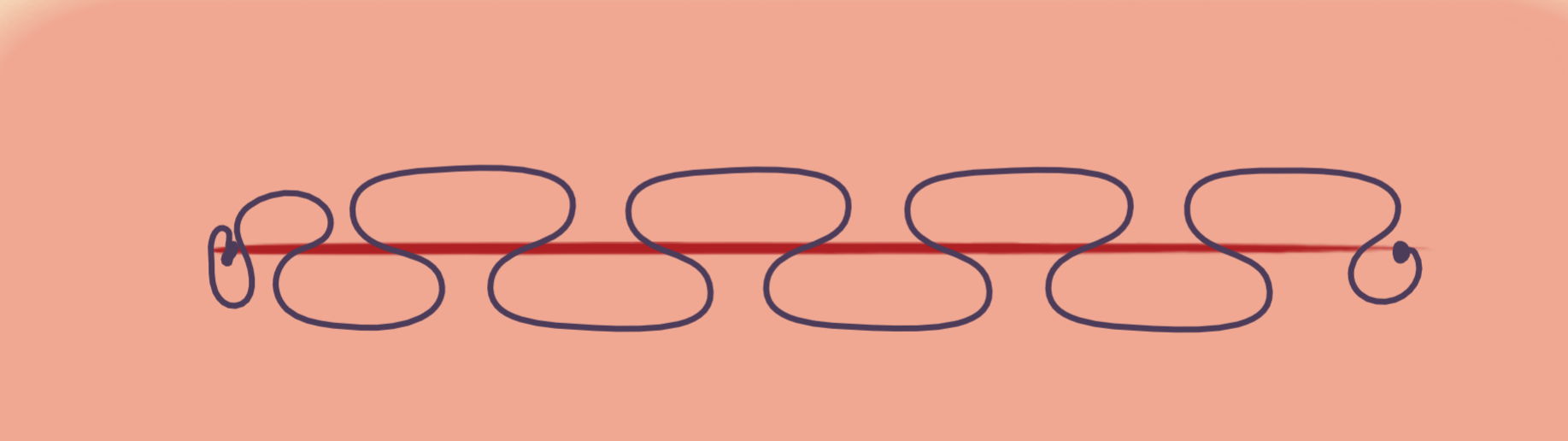
what happens with an intradermal pattern that has no overlap or larger bites?
gapping of the incision
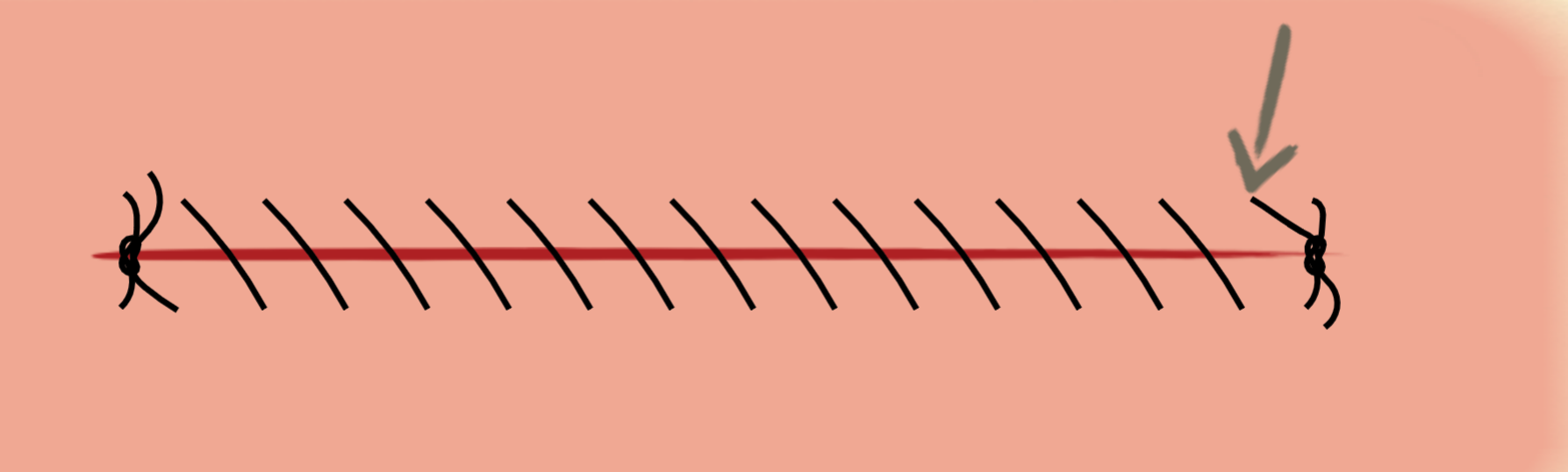
simple interrupted
poor tension relief
slow to do
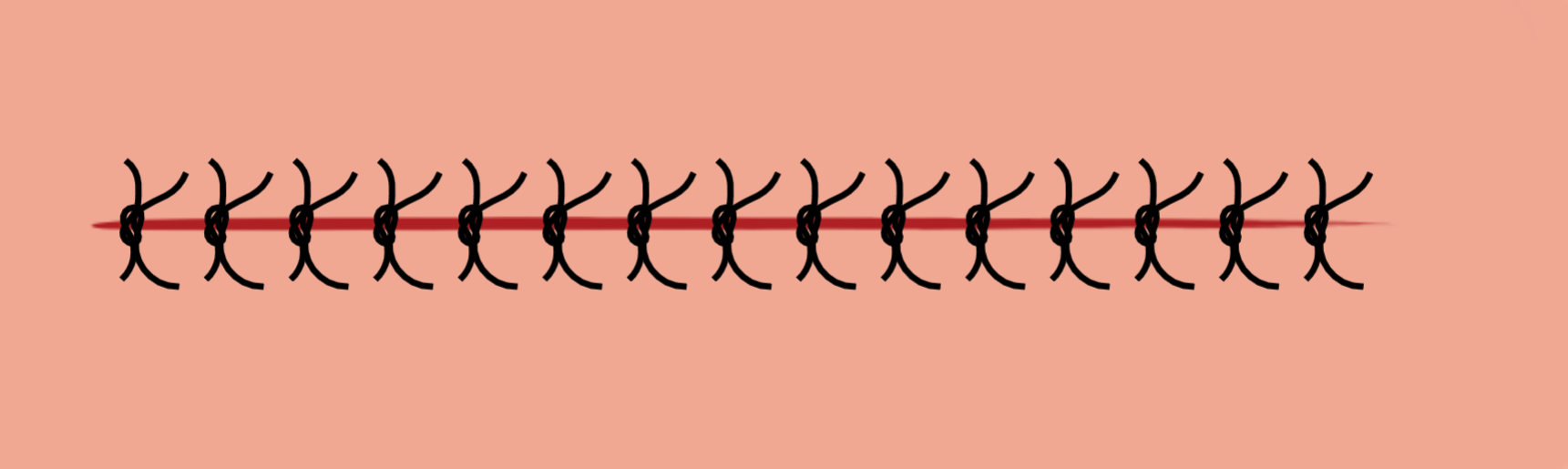
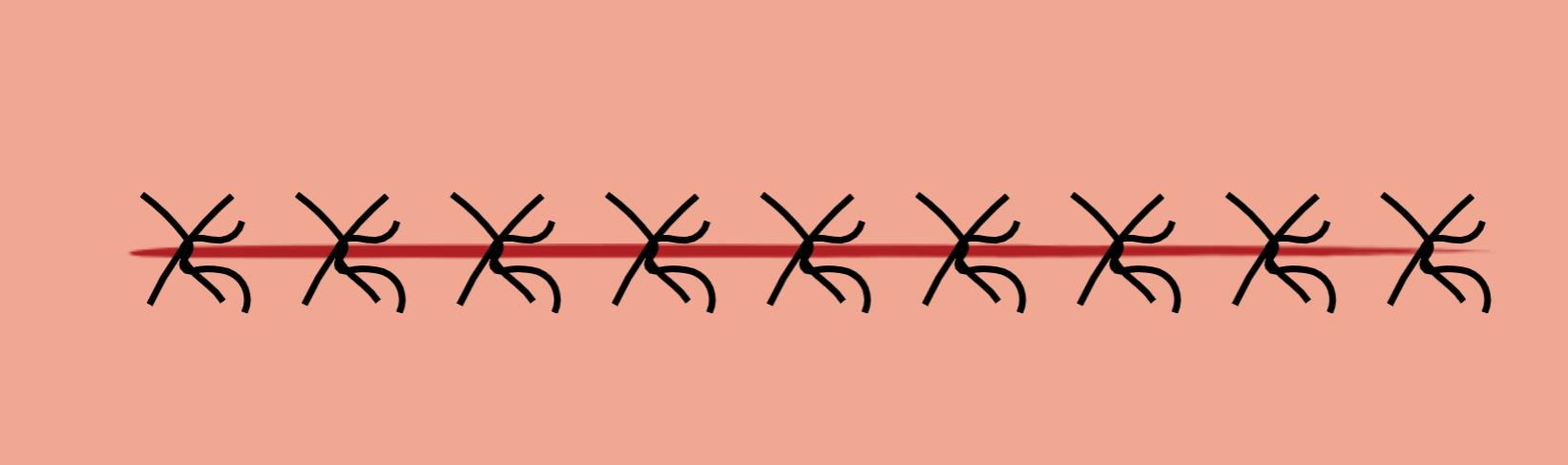
cruciate mattress
some tension relief
faster to put in
simple continuous
fast
not for high tension/motion
ford interlocking
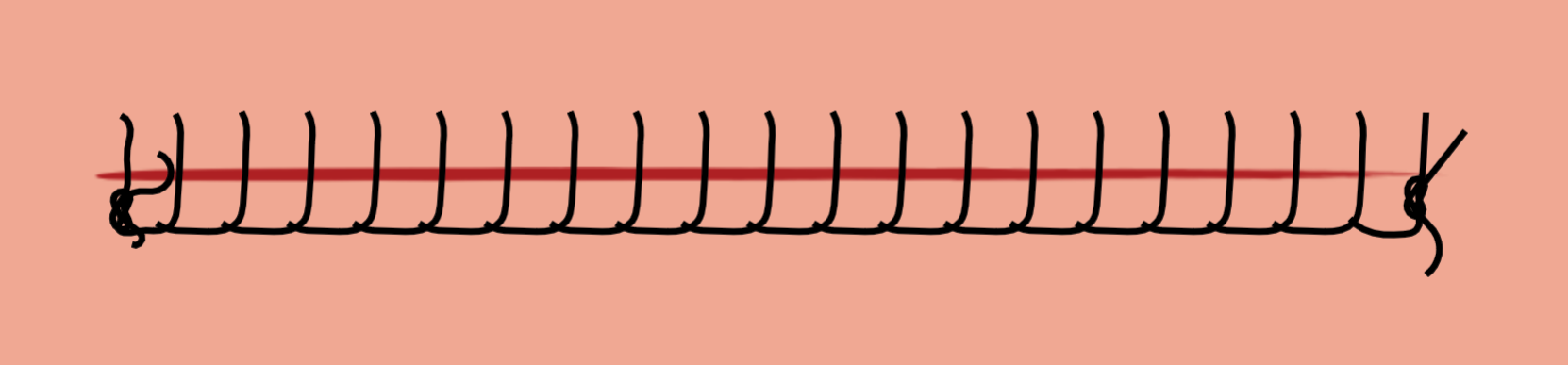
fast
more secure if broken compared to simple continuous as it grabs onto itself
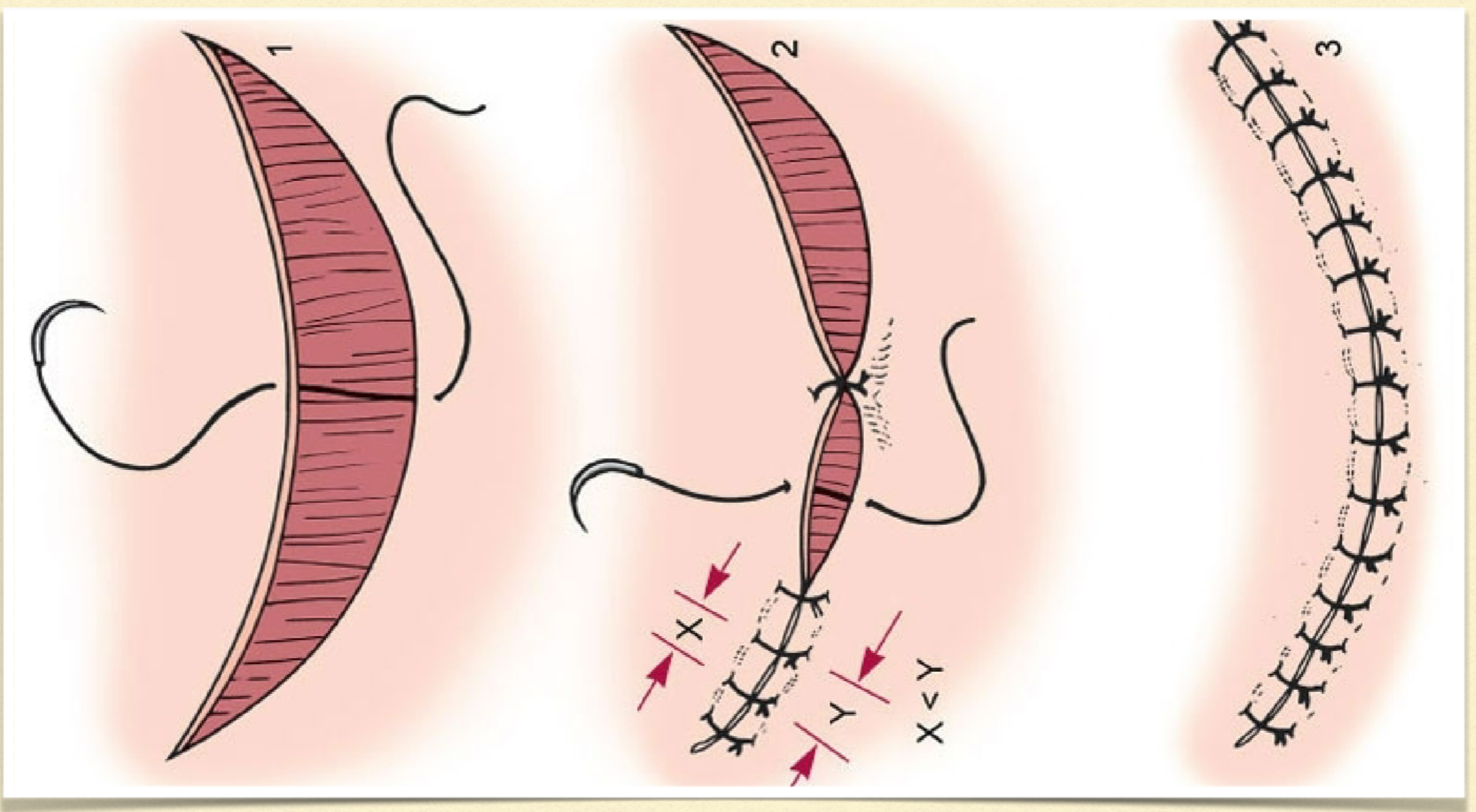
what are dog ears created by suturing a wound close?
folding up of skin after suturing an awkward wound
what are the reasons for dog ear formation?
unequal suture spacing
non-linear wound
are dog ears really a problem?
no more a cosmetic problem and will diminish with time
what is a technique you can use to close a very large wound?
halving to help guide your suturing placement
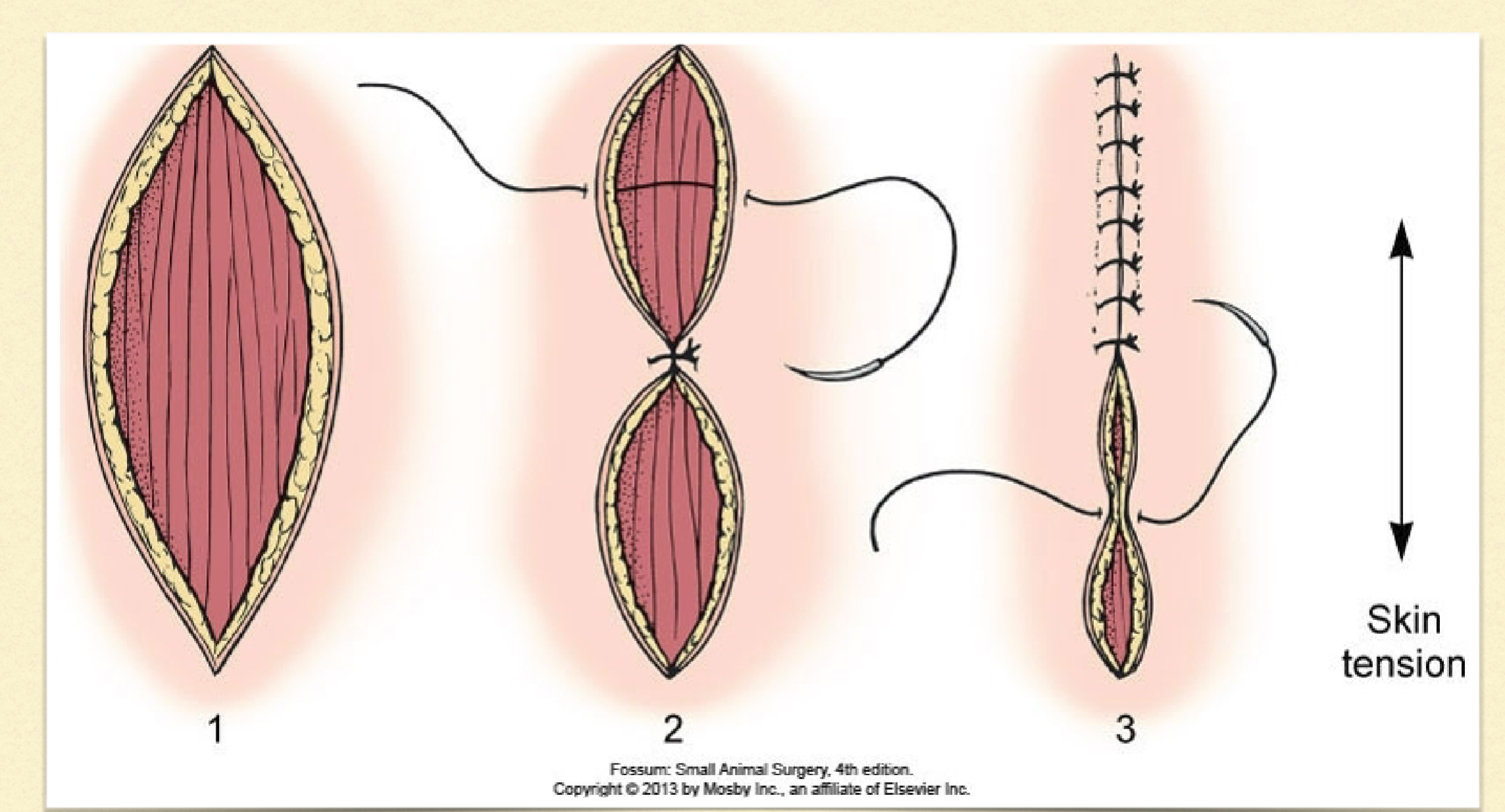
can halving work on a curved wound?
yes! suture bits need to be placed at different lengths across the curve so halving can help guide
how can you close a rectangular lesion?
close corners to bring middle closer together then
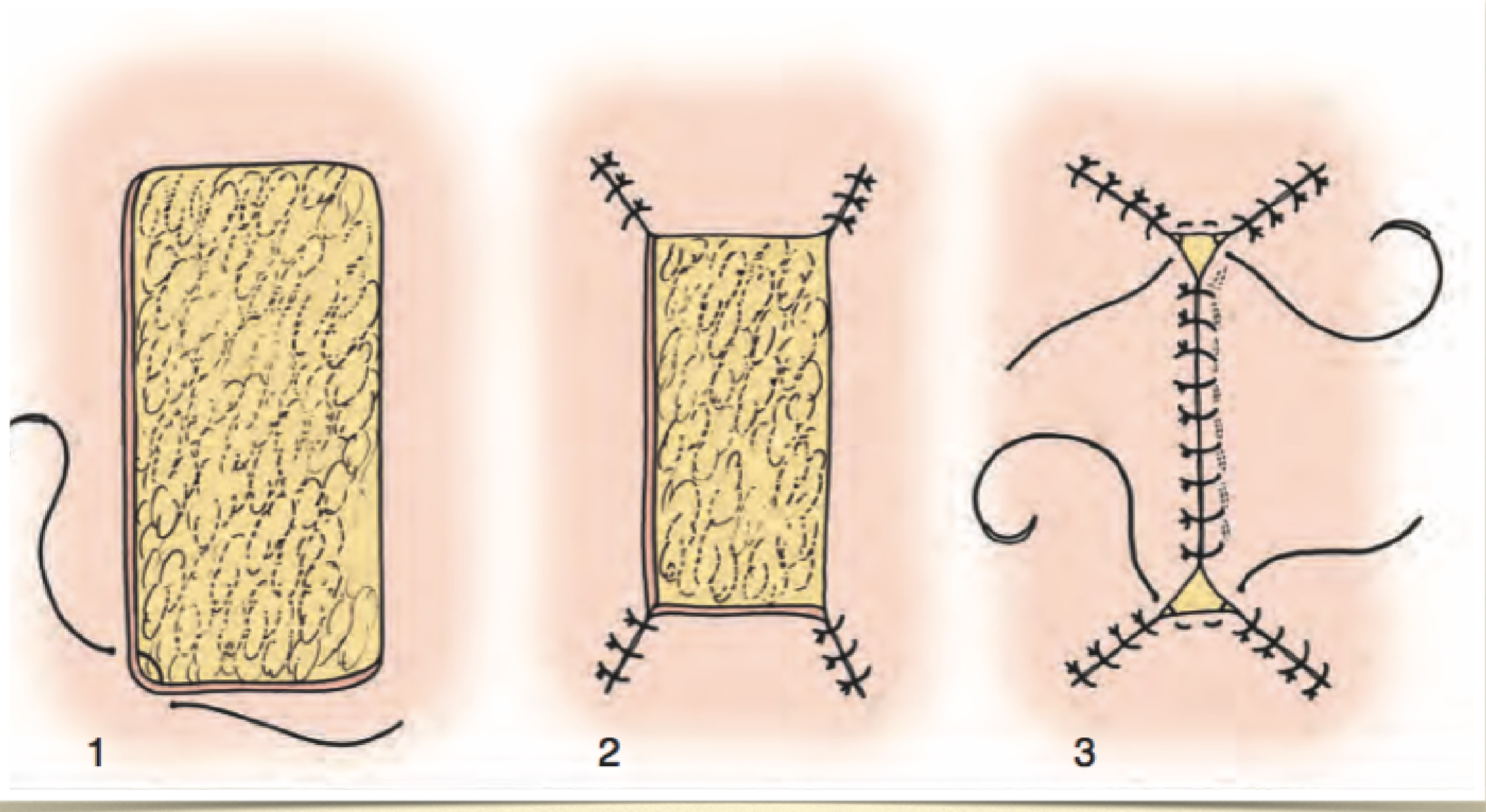
triangular closure
close up each side of triangle until meet in middle
what component of a primarily closed skin incision is most likely to fail with excess tension?
tissue
excessive tension of skin can lead to what?
dehiscence and tissue necrosis
what is another aspect that can cause dehiscence?
excessive activity that puts too much motion and tension on healing wound
what are the two methods of tension relief?
redistribution
creep
what are the two forms of creep?
mechanical
biological
what is mechanical creep?
stretching/breaking collagen and elastin
takes hours to days
common to use with larger defects
what is biological creep?
allowing new skin to grow
takes weeks
what is undermining?
mobilizing skin by separating it from deeper levels but going deep to the cutaneous trunci
why do keeping the cutaneous trunci with the tissue in undermining important?
preserves subdermal plexus
preserve vessel
all this keeps the skin viable
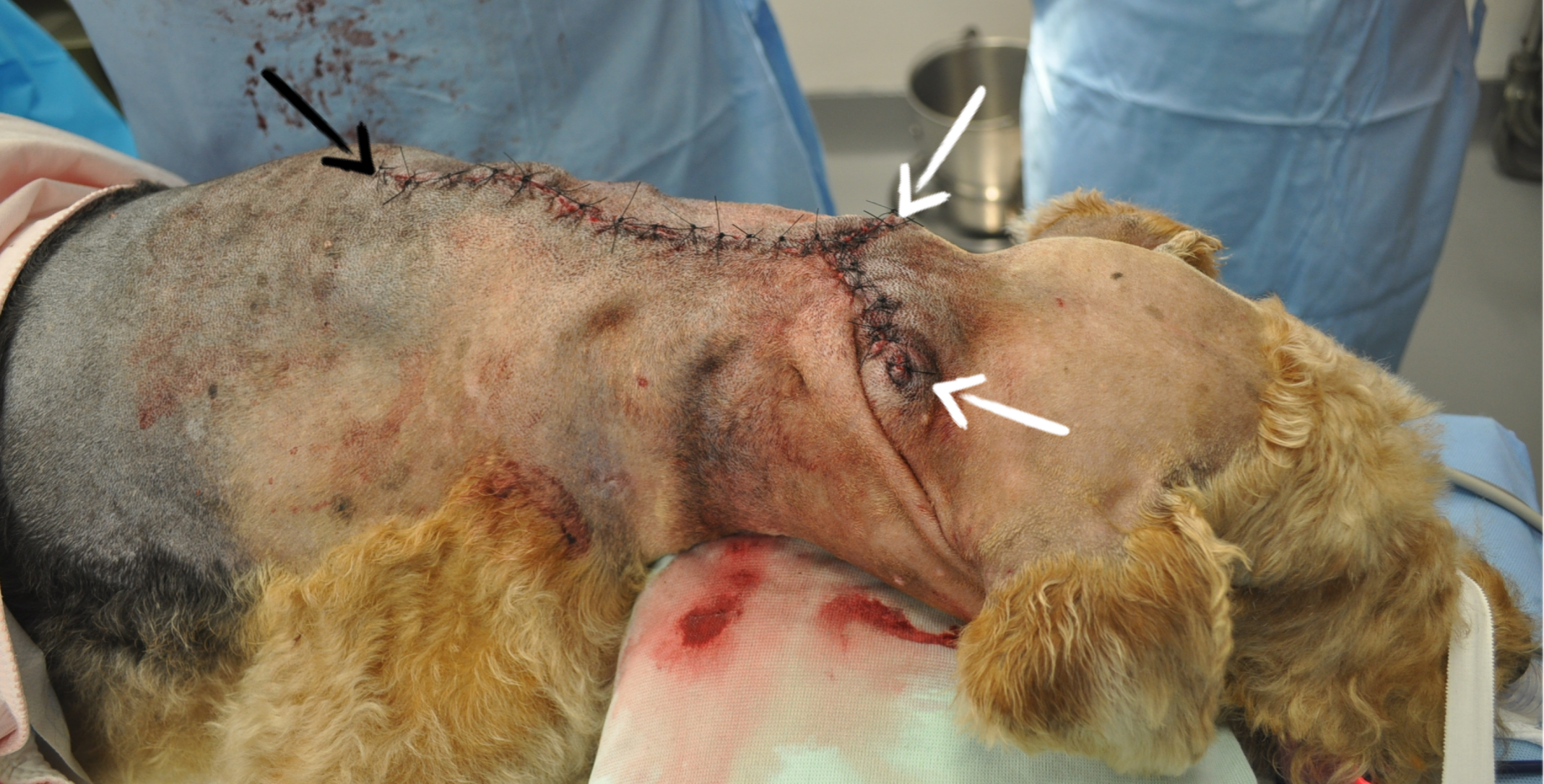
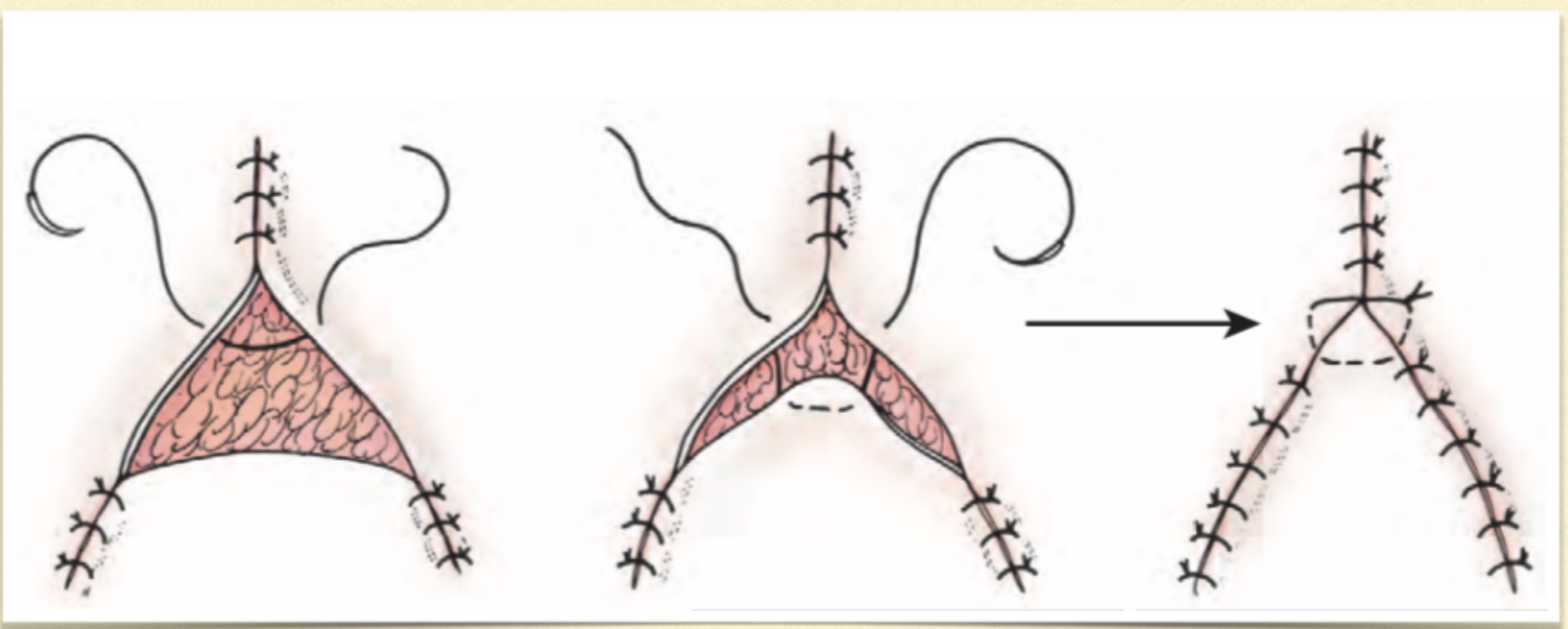
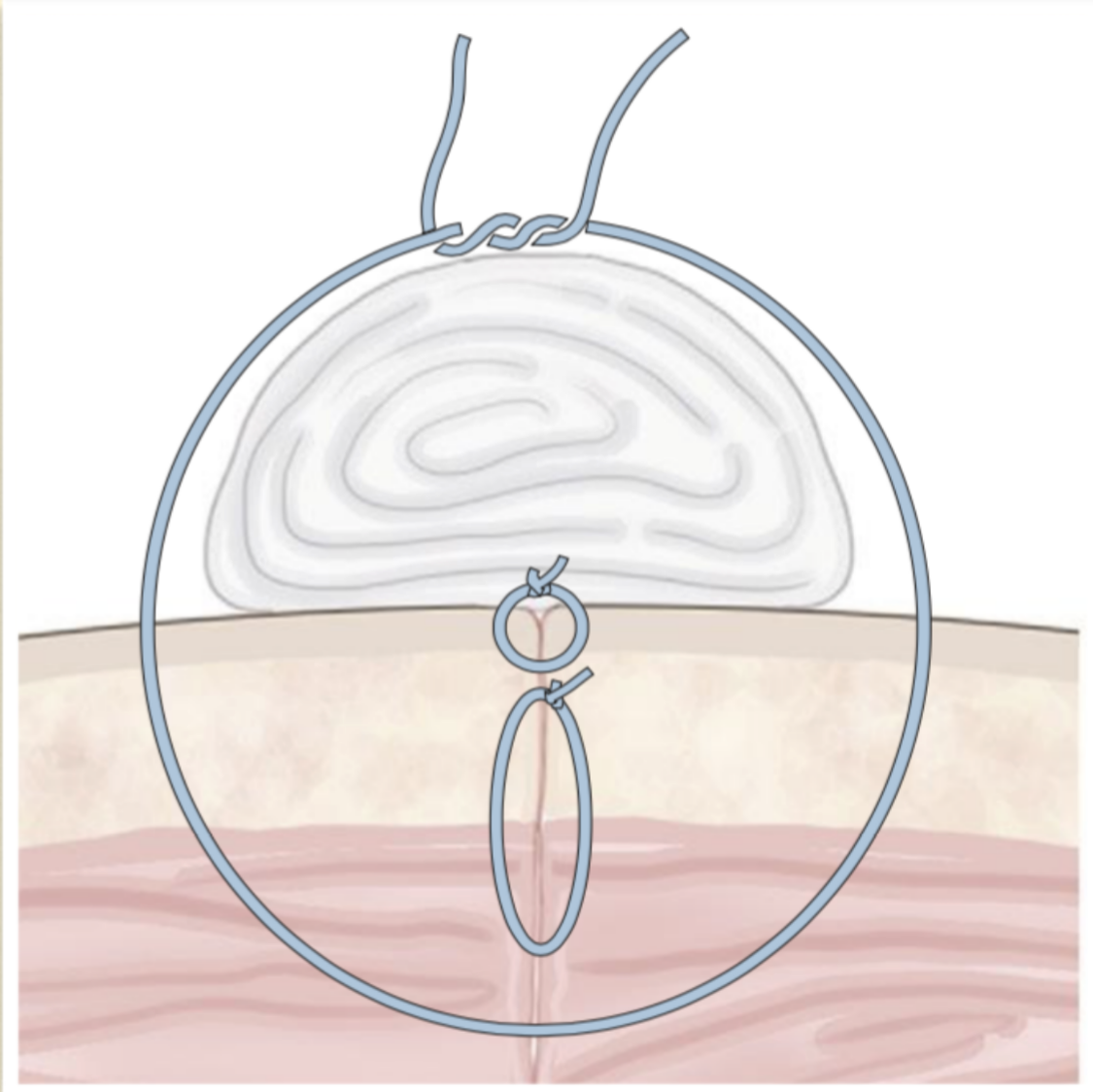
walking sutures
tension relieving
move skin across a defect → offset deep and superficial bites
stretching skin out
close dead space
what are the types of external sutures that help to relieve tension?
mattress sutures (horizontal, vertical, cruciate)
far-far-near-near/far-near-near-far
bolster/stent sutures
pre-place with wide bites
padding to distribute tension
what are releasing incisions?
incisions in healthy skin
heal by second intention
distal limbs is an optimal area to use this technique
mesh releasing incisions
~ 1 cm or less incisions parallel to the closure and staggered

what is another way to close a large defect?
skin stretching
what are the options of skin stretching?
commerical/homemade
velcro/suture
adjusting the tension over time
what are flaps used for?
to fill large defects
what are the options for flaps?
skin
mucosa
muscle
composite
when creating a flap, what will you inevitably do?
cut off some blood supply to the flap, making the tip slightly ischemic
what occurs at the base of the flap to blood vessels?
those vessels in line with the flap will become engorged to supply the area
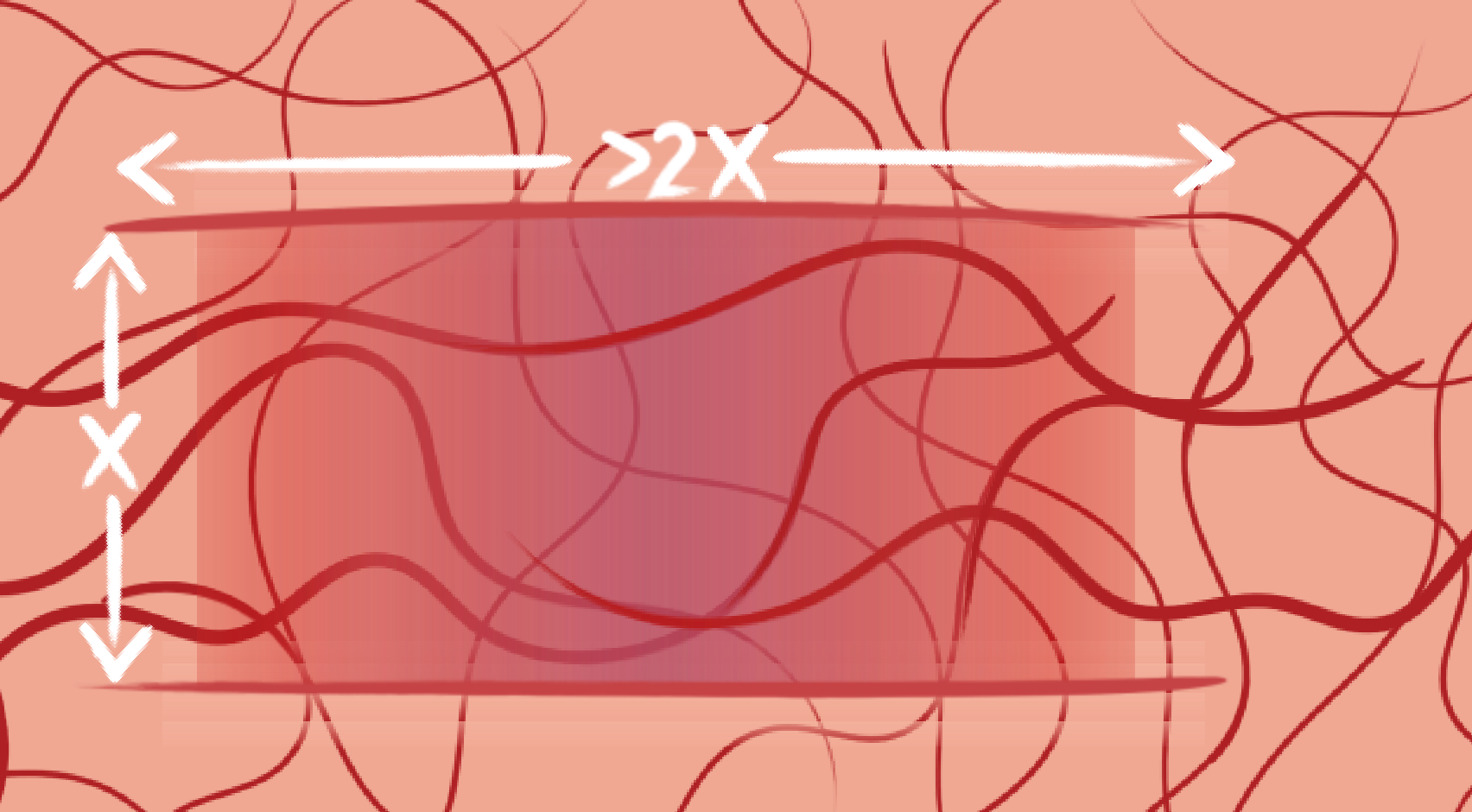
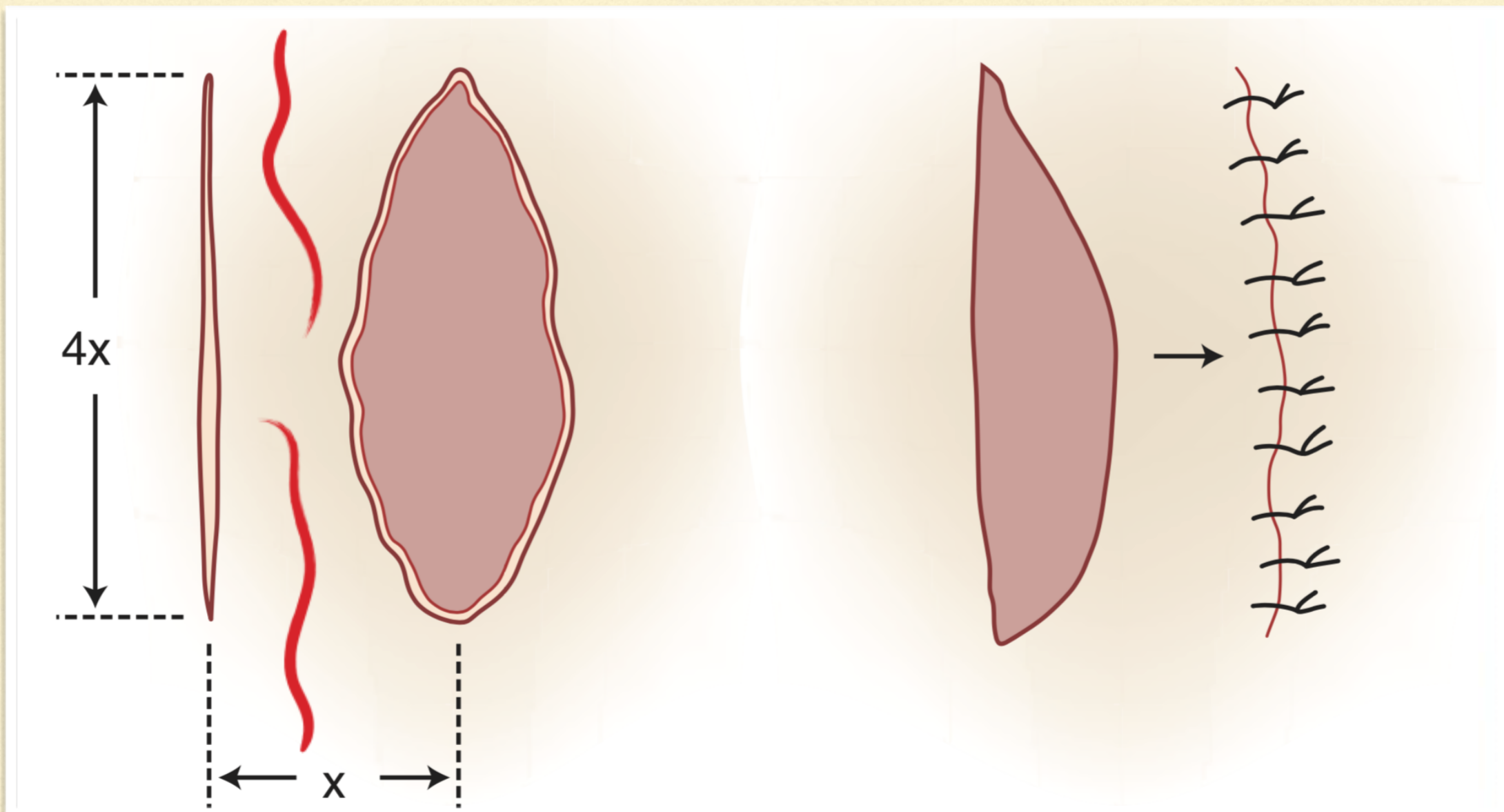
what are the dimensional limitations of creating a skin flap?
the length should not be 2x greater than the width
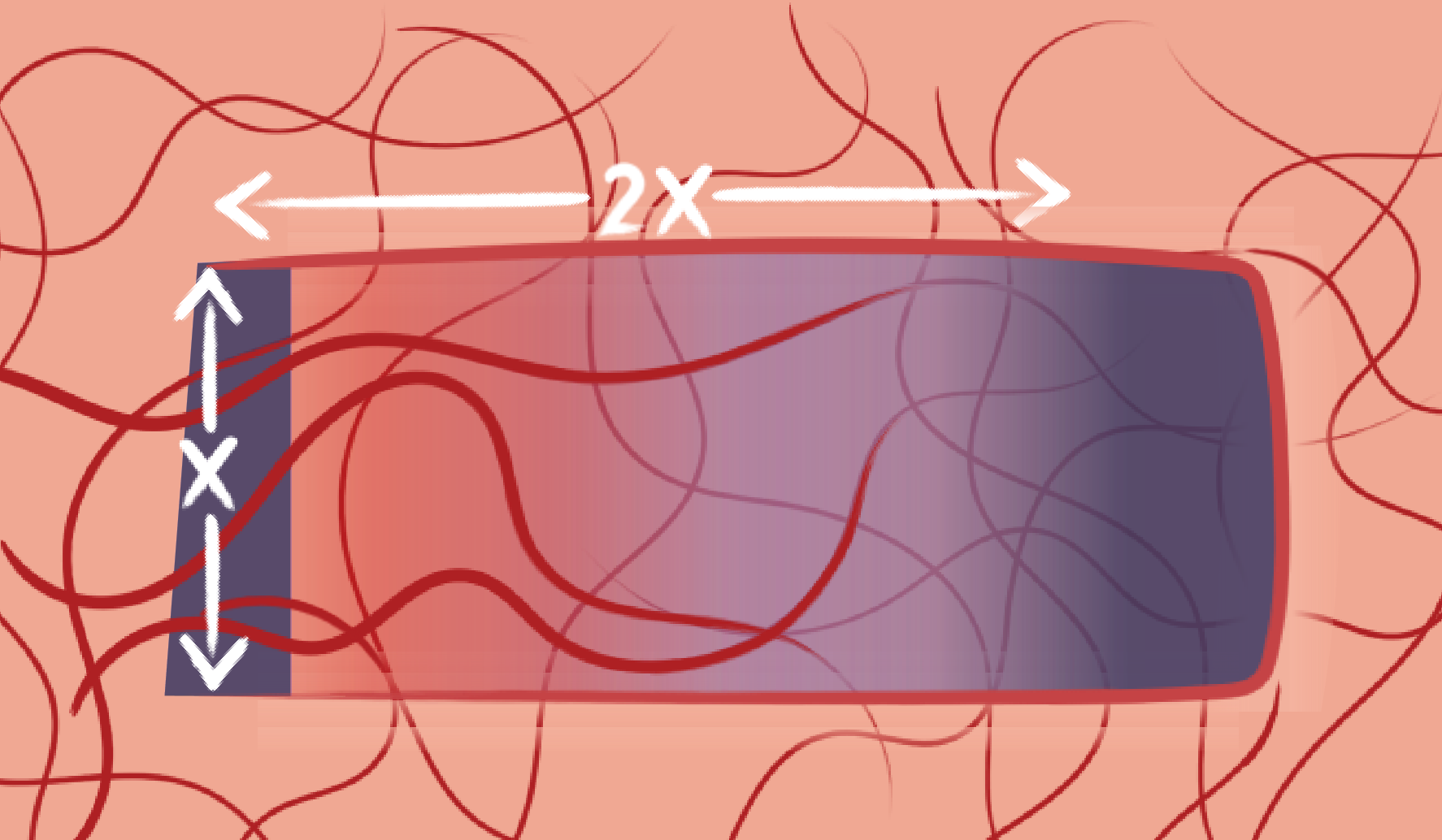
how can you make a flap longer than 2x the width?
by making a delayed flap that is where you cut the lengths (2 parallel incisions) you want but wait to cut the width part