Muscular dystropies
1/5
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
6 Terms
Duchenne Muscular Dystrophy
• Most common and most severe muscular dystrophy
• Rapidly progressive muscle weakness
Onset
• Early childhood
Main Muscles Affected
• Skeletal muscles
• Cardiac muscle
Key Clinical Features
Most patient w wheelchair than die in 25-30years of age(respiratory insufficincy,heart failure)
• Delayed sitting, standing(Gower sign), walking
• Progressive muscle weakness(proximal more than distal)
• Calf pseudo atrophy
• Cardiomyopathy
• Learning difficulties may occur
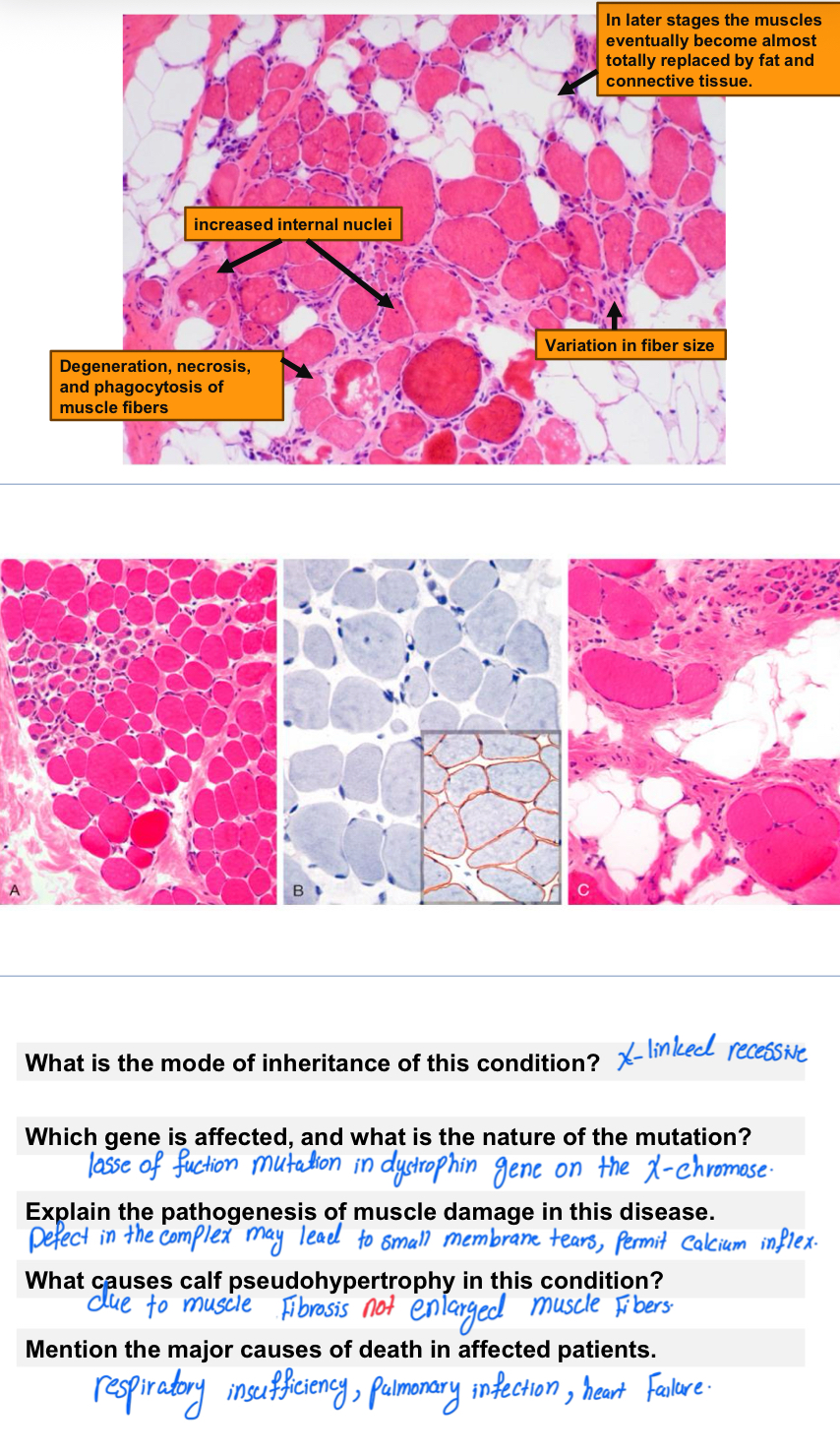
Morphology:
1-Variation in fiber size
2-Increased numbers of internalized nuclei
3- Degeneration, necrosis, and phagocytosis of muscle fibers
4-Regeneration of muscle fibers
5-Proliferation of endomysial connective tissue
Cause (Gene / Protein)
• Mutation in DMD gene
• Deficiency of dystrophin
• Dystrophin stabilizes muscle fibers and aids cell signaling
Inheritance Pattern
• X-linked recessive
• affects males,Female are carrier and they are asymoptomatic but have ⬆creatine kinase and show minimal histologic abnormalities on biopsy
Both of them at risk for dilated cardiomypathy
• Mothers are typically carriers
• Can occur due to new (de novo) mutations
Diagnostic Tests
• ↑ Creatine kinase (CK)
• Genetic testing for DMD mutation
Becker Muscular Dystrophy (BMD)
• Milder form related to Duchenne MD
• Progressive muscle weakness
Onset
• Later childhood or adolescence
Main Muscles Affected
• Legs and pelvis first
• Then shoulders, arms, neck
• Cardiac and respiratory muscles may be involved
Severity
• Less severe than DMD
• Slower progression
Cause
• Mutation in DMD gene (partial dystrophin function preserved)
Inheritance Pattern
• X-linked recessive
Important Note
• Genetic counseling recommended if family history is present
Myotonic Dystrophy f
• Most common adult-onset muscular dystrophy
• Progressive muscle weakness and wasting
• Presence of myotonia (delayed muscle relaxation/involuntary muscle contraction)
Clincal features:
Stifness and difficulty in relaxing their grip
Weakness of footdorsiflexors and intrinsic muscles of hand and wris extonsors
Atrophy of the facial muscles and ptosis
Involement of other organ systems(fatal cardiac arrhythmias,cataracts,frontal balding,endocrunopathies,and testicular atorphy)
Affect proximal musculature of the trunk and limbs
Onset
• Usually 20s–30s
• Can occur at any age
Major Types
🔹 Type 1 (DM1)
• Distal muscles (hands, feet, face)
• More severe
• Shows anticipation
Most common(95%)
🔹 Type 2 (DM2)
• Proximal muscles (neck, shoulders, hips)
• Milder form
• No clear anticipation
Causes
• DM1: Mutation in DMPK gene
• DM2: Mutation in CNBP gene
Inheritance Pattern
• Autosomal dominant w trinucleotide repeat expansion
• Anticipation occurs only in Type 1
Facioscapulohumeral Muscular Dystrophy (FSHD)
• Slowly progressive muscular dystrophy
• Not usually life-threatening
Caseud by overexpression of DUX4 target genes
Onset
• Adolescence most common
• Can appear in childhood or adulthood(20 years)
Majority have normal life
Prevalence
• ~1 in 20,000
• 95% FSHD1, 5% FSHD2
Key Molecular Mechanism
• Hypomethylation of D4Z4 region on chromosome 4
• Leads to abnormal gene activation
Types
🔹 FSHD1
• Autosomal dominant
• D4Z4 contraction (1–10 repeats instead of 11–100)
🔹 FSHD2
• Mutation in SMCHD1 gene (most cases)
• Some cases unknown cause
Inheritance
• Autosomal dominant
• Can be sporadic (de novo mutation)
Congenital Myasthenic Syndrome (CMS)
• Neuromuscular junction disorder
• Muscle weakness worsens with exertion
Onset
• Early childhood
• Can appear later
Main Muscles Affected
• Facial muscles
• Eyelids (ptosis)
• Chewing and swallowing muscles
• Limb muscles
Severe Features
• Breathing difficulties
• Apnea
• Cyanosis (in severe cases)
Major Causative Genes
• CHRNE (most common)
• RAPSN
• CHAT
• COLQ
• DOK7
Pathophysiology
• Defective acetylcholine receptor function
• Impaired neuromuscular transmission
Inheritance Pattern
• Usually autosomal recessive
• Rare autosomal dominant
• Can occur due to new mutations
Walker–Warburg Syndrome
• Rare congenital muscular dystrophy
• Associated with brain and eye abnormalities
Clinical Features
• Severe muscle weakness
• Neurological defects
• Ocular abnormalities
Cause
• Mutations in genes affecting α-dystroglycan glycosylation
• Important genes include:
– POMT1
– POMT2
– CRPPA
– FKTN
– FKRP
– LSRGE1
Pathophysiology
• Defective glycosylation → unstable muscle fibers
Inheritance Pattern
• Autosomal recessive