Chapter 15 Nursing care of the child with an infection
1/41
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No study sessions yet.
42 Terms
Infection
refers to invasive of body cells and tissues by microorganisms with the potential to cause illness or disease
infectious process
Infection occurs when an organism enters the body and multiplies, causing damage to the tissues and cells. The body’s response to this damage due to infection or injury is inflammation. The body delivers fluid, blood, and nutrients to the area of infection or injury and attempts to eliminate the pathogens and repair the tissues. The body does this through vascular and cellular reactions. The vascular response is an initial period of vasoconstriction followed by vasodilation. This vasodilation allows for the increase of fluids, blood, and nutrients to the area.
Granulocytes
Neutrophils (leukocytes or PMNs, segs), Eosinophils, Basophils
First line of defense upon invasion of bacteria, fungus, cell debris, and other foreign substances
Respond to allergic disorders, parasitic infections, and chronic immune responses
Respond to allergic disorders and hypersensitivity reactions; used to study chronic inflammation
Lymphocytes
Main source of producing an immune response; respond to viral infections (measles, rubella, chickenpox, infectious mononucleosis); tumors
Monocytes
Second line of defense; respond to larger and more severe infections than neutrophils by phagocytosis; leukemias and lymphomas; chronic inflammation
Phagocytosis
to ingest and destroy the pathogen.
Fever
Infection or inflammation caused by bacteria, viruses, or other pathogens stimulates the release of endogenous pyrogens (interleukins, tumor necrosis factor, and interferon)
fever measurements and routes
Oral: >37.8°C (100°F)
Rectal: >38°C (100.4°F)
Axillary: >37.2°C (99°F)
Tympanic: >38°C (100.4°F)
Temporal: >38°C (100.4°F)
1 Incubation
Time from entrance of pathogen into the body to appearance of first symptoms; during this time, pathogens grow and multiply.
2., Prodrome
Time from onset of nonspecific symptoms such as fever, malaise, and fatigue to more specific symptoms
Illness
Time during which child demonstrates signs and symptoms specific to an infection type
Convalescence
Time when acute symptoms of illness disappear
Infectious agents
Anything that cause infection ex: bacteria, viruses, rickettsiae, protozoa, and fungi
control and eliminate
Hand washing
Wearing gloves
Cleaning, disinfecting, or sterilizing equipment
Reservoir
A place where the pathogen can thrive and reproduce; examples: human body, animals, insects, food, water, inanimate objects (e.g., stethoscopes)
Portal of exit
A way for the pathogen to exit the reservoir; examples: skin and mucous membranes, respiratory tract, urinary tract, gastrointestinal tract, reproductive tract
Modes of transmission
Direct transmission: body-to-body contact
Indirect transmission: transferred by fomite or vector; spread by droplet or airborne transmission
Portal of entry
A way for the pathogen to enter the host; examples: skin and mucous membranes, respiratory tract, urinary tract, gastrointestinal tract, reproductive tract
Susceptible host
Any person who cannot resist the pathogen
Lab Complete blood count (CBC)
Evaluate white blood cell count (particularly the percentage of individual white cells)
ind: Detect the presence of inflammation, infection.
Erythrocyte sedimentation rate (ESR)
Nonspecific test used in conjunction with other tests to determine presence of infection or inflammation
ind: Detect the presence of inflammation, infection
Standard C-Reactive protein (CRP)
Nonspecific test that measures a type of protein produced in the liver that is present during episodes of acute inflammation or infection
Usually used to diagnose acute infections
Ind: To detect the presence of infection, CRP is a more sensitive and rapidly responding indicator than ESR.
Blood culture and sensitivity
Deliberate growing of microorganism in a solid or liquid medium. Once it has grown, it is tested against various antibiotics to determine which antibiotics will kill it.
Ind: Detect the presence of bacteria or yeast, which may have spread from a certain site in the body into the bloodstream.
Determine which antibiotics the bacteria or yeast is sensitive to.
Stool culture
To determine if bacteria or parasite have infected the intestines
Ind: Detect pathogens, including parasites or overgrowth of normal flora in the bowel. Indicated for children with diarrhea, fever, or abdominal pain
Urine Culture
Collection of urine to detect the presence of bacteria in the urine
Ind:Detect the presence of bacteria in the urinary tract. Indicated for children with fever of unknown origin, dysuria, frequency, or urgency, or if urinalysis suggests infection
Wound Culture
Allows for microbial growth and identification of specific organism
Ind: Identification of specific organism
Throat culture
Vigorous swabbing of the tonsillar area and posterior pharynx to detect the presence of invasive organisms
Ind:Most reliable method of detecting group A streptococcal pharyngitis
Will also detect Bordetella pertussis, Corynebacterium diphtheriae, viral infections
May be performed in those with fever of unknown origin
Nasal swabs (nasopharyngeal)
Insertion of swabs into the nose until reaching the nasopharynx to detect the presence of invasive organisms
Ind: Optimal method for detecting B. pertussis. Also used to detect Corynebacterium diphtheriae and viral illnesses such as respiratory syncytial virus (RSV), parainfluenza
sepsis
is a systemic overresponse to infection resulting from bacteria and viruses (most commonly), fungi, viruses, rickettsiae, or parasites. It can lead to septic shock, which results in hypotension, low blood flow, and multisystem organ failure.
sepsis patho
results in the systemic inflammatory response syndrome (SIRS) due to infection. It results from the effects of circulating bacterial products or toxins, mediated by cytokine release, occurring as a result of sustained bacteremia. The pathogens cause an overproduction of proinflammatory cytokines, previously termed endotoxins. These cytokines are responsible for the clinically observable effects of the sepsis. Impaired pulmonary, hepatic, or renal function may result from excessive cytokine release during the septic process.
scarlet fever
is an infection resulting from group A streptococci. It usually occurs with a group A streptococci throat infection (i.e., strep throat) or rarely streptococcal skin infection.
rash/ droplets and contact
Scarlet fever begins abruptly, strawberry tongue
Diphtheria
is caused by infection with Corynebacterium diphtheriae and may affect the nose, larynx, tonsils, or pharynx.
Pseudomembrane as it forms swallowing becomes difficult and signs of airway obstruction becomes apparent
Pertussis
is an acute respiratory disorder characterized by paroxysmal cough (whooping cough) and copious secretions.
The disease is caused by Bordetella pertussis. The incubation period is 6 to 20 days, usually 7 to 10 days. Pertussis usually starts with 7 to 10 days of cold symptoms. The paroxysmal coughing spells then begin and can last 1 to 4 weeks. Convalescence occurs over the course of several weeks to months.
Tetanus
is an acute, often fatal neurologic disease caused by the toxins produced by Clostridium tetani.
Botulism
is a disease that is caused by a toxin produced in the immature intestines of young children resulting from infection with the bacterium Clostridium botulinum.
Osteomyelitis
is a bacterial infection of the bone and soft tissue surrounding the bone. S. aureus is the most common infecting organism, with MRSA accounting for a third of these infections

Rubella (Measles)
Caused by rubella virus
Transmission: by direct or indirect contact with droplets, primarily by nasopharyngeal secretions, but also in blood, stool, and urine. Also transmitted from birthing parent to fetus
Peak incidence: late winter and early spring
Incubation period: 12–23 days (usually 14 days)
Communicable: 7 days before to 7 days after onset of rash
Rubeola (Measles)
Caused by measles virus
Transmission: direct or indirect contact with droplets, primarily by nasopharyngeal secretions and airborne (virus can stay in air for up to 2 hours after infected person leaves the area); highly contagious
Peak incidence: late winter and spring
Incubation period: 6–21 days, usually 13 days
Communicable 1–2 days before the onset of symptoms (4 days before onset of rash) until 4 days after rash has appeared

Varicella Zoster (Chickenpox)
Caused by varicella zoster virus, human herpes virus 3
Transmission: direct contact with infected people’s nasopharyngeal secretions or via airborne spread, to a lesser degree by contact with unscabbed lesions. Highly contagious. Also transmitted from birthing parent to fetus
Peak incidence: winter and early spring
Incubation period: 10–21 days, usually 14–16 days
Communicable 1–2 days before the onset of rash until all vesicles have crusted over (about 3–7 days after the onset of rash)

Exanthem Subitum (Roseola Infantum or Sixth Disease
Caused by B variant of human herpes virus 6 (HHV-6); (less frequently human herpes virus 7 [HHV-7], adenoviruses, enteroviruses, parainfluenza virus)
Transmission: little is known and depends on causative virus but HHV-6 suspected to be from saliva of infected person and enters the host through the oral, nasal, or conjunctival mucosa
Peak incidence: ages 7–13 months, spring and fall
Incubation period: 5–15 days, average of 10 days
Communicability is unknown, but most likely contagious before symptoms appear

Erythema Infectiosum (Fifth Disease)
Caused by human parvovirus B19
Transmitted by large droplet spread from nasopharyngeal viral shedding or percutaneous exposure to blood and blood products. Also transmitted from birthing parent to fetus
Peak incidence late winter and spring
Incubation period: 4–28 days, average 16–17 days
Communicability is uncertain, but most children are no longer infectious by the time the rash appears and diagnosis is made, so isolation or exclusion from school, once the child is diagnosed, is unnecessary (those with aplastic crisis may be communicable up to 1 week after the onset of symptoms and those who are immunosuppressed with chronic infection and severe anemia may be communicable for months to years).
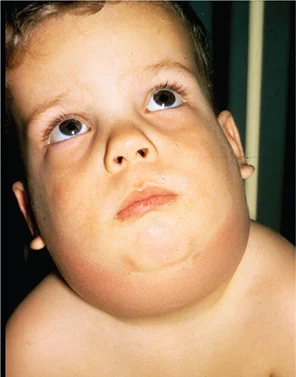
Mumps
a contagious disease caused by Paramyxovirus, is characterized by fever and parotitis (inflammation and swelling of the parotid gland). Mumps is spread via airborne droplets or contact with infected droplets.