pneumonia drugs
1/44
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
45 Terms
uncommon non-infectious causes
lung infarction
common non-infectious causes
pulmonary edema
ARDS
lung cancer
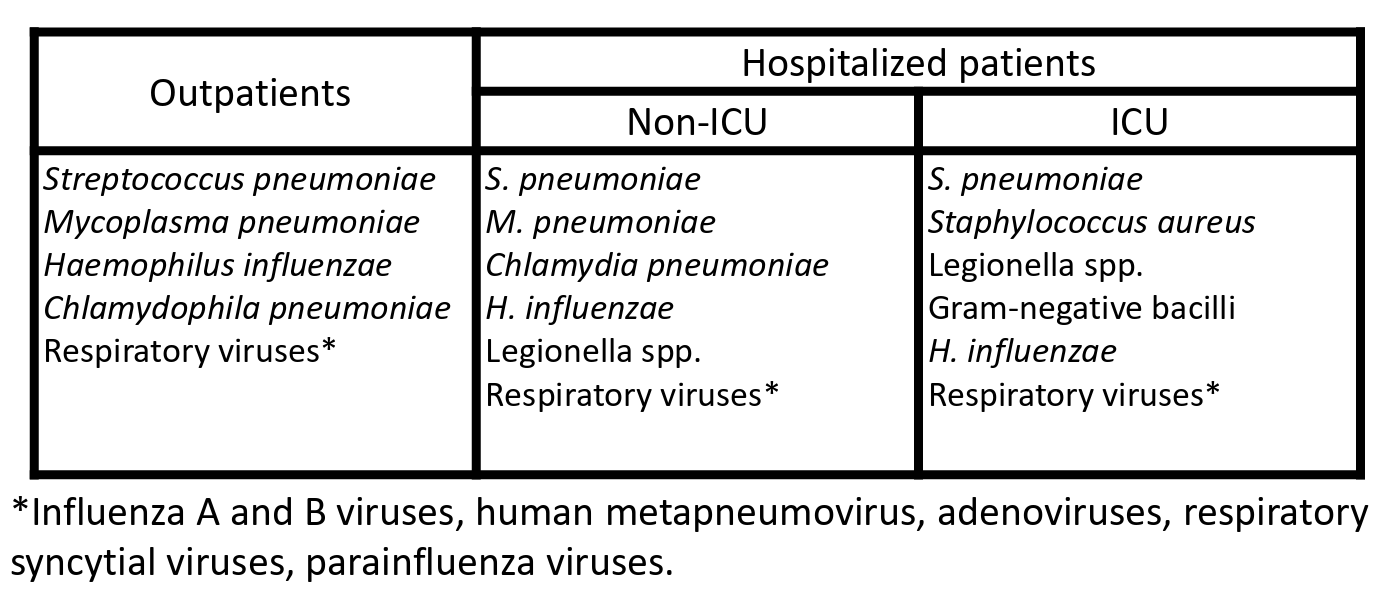
common infectious causes
streptococcus pneumoniae
Haemophilus influenzae
staphylococcus aureus
influenza and other viruses
uncommon infectious causes
pseudomonas aeruginosa
Pneumocystis jiroveci
Moraxella catarrhalis
typical CAP
Sudden onset of fever, chills, pleuritic chest pain, productive cough
typical CAP organisms
• Streptococcus pneumoniae
-Haemophilus influenzae
Atypical CAP
often preceded by mild respiratory illness
Atypical CAP caused by
• Legionella spp.
• Mycoplasma pneumoniae (walking pneumonia)
• Chlamydophila pneumoniae
Basics of pneumonia pharmacotherapy
• Start empiric therapy with a broad spectrum antibiotic
• Revise therapy once the causative organism is identified
• Revise therapy based on disease progression (and potential development of drug resistance)
• For hospitalized patients, once stabilized, move from IV to oral therapy prior to discharge
Streptococcus pneumoniae: CAP typical treatment
Usually susceptible to penicillin
give:
• Penicillin G (high doses)
• Aminopenicillins: Ampicillin (high doses)
Treatment of Penicillin-resistant Streptococcus pneumoniae
• Second Generation Cephalosoporins: Cefuroxime
• Third Generation Cephalosporins: Cefotaxime, Ceftriaxone
• Quinolones: Moxifloxacin, Levofloxacin
• Vancomycin
• Macrolides/ketolines: Telithromycin
what cephalosporin can treat MRSA
5th generation cephalosporins differ from ALL other betalactam antibiotics by being active against Methicillin-resistant Staphylococcus aureus (MRSA)
H.infleunzae treatment
Quinolone
macrolide
Legionella treatment
macrolide
quinolone
mycoplasma pneumoniae treatment
quinolone
macrolide
aerobic gram neg bacteria treatment
quinolone
chlamydophilia pneumoniae
quinolone
macrolide
staphylococcus aureus
quinolone
macrolide
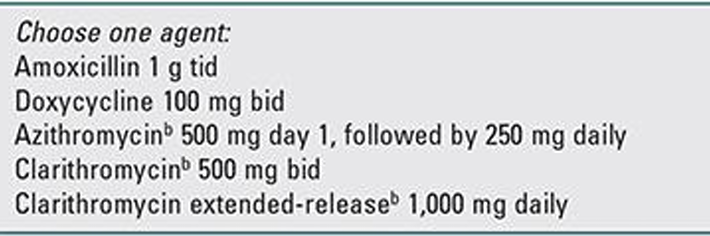
outpatient with no comorbidities or MRSA risk in community more than 25%
either:
-amoxicillin
-doxycycline
outpatient with no comorbidities or MRSA risk in community less than 25%
either:
-amoxicillin
-doxycycline
-Clarithromycin
-Azithromycin
outpatient with co-morbidities
either:
-monotherapy of fluoroquinolone (levifloxacin/moxifloxacin/gemifloxacin)
-beta-lactam + macrolide
-beta-lactam + doxycycline
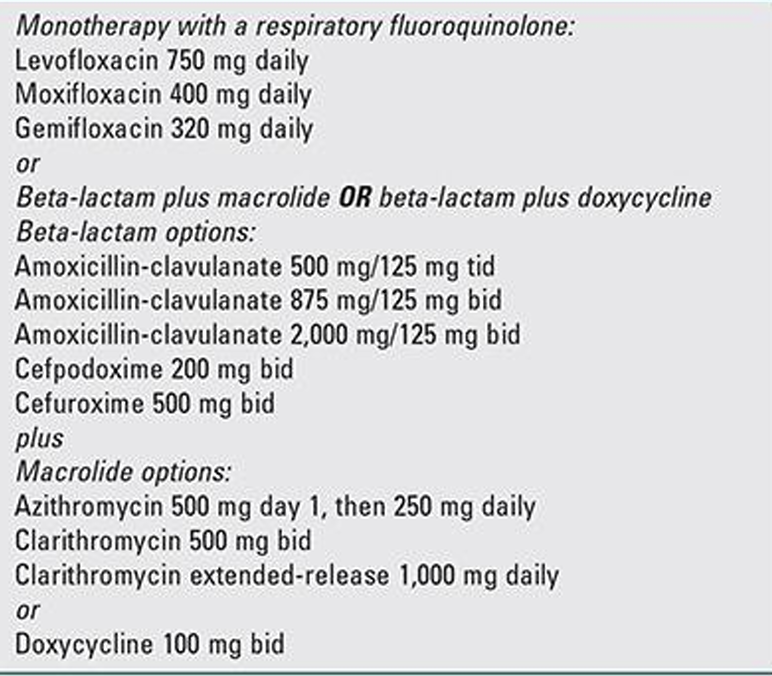
in-patient nonsevere
-monotherapy of fluoroquinolone (levifloxacin/moxifloxacin/gemifloxacin)
-beta-lactam + doxycyline
-beta-lactam + macrolide
MRSA in nonsevere and severe in patient
add vancomycin or linezolid
P.areguinosa consideration
switch the b-lactam to an antipsuedomonal beta lactam
antipseudomonal b-lactams
-piperacillin-tazobactam
-cefepime
-ceftazidime
-imipenem
-meropenem
-aztreonam
in-patient severe
-b lactam + macrolide
-b lactam + fluroquinolone
HAP is divided into two classes:
Early onset HAP
Late onset HAP
Early onset HAP
occurs within first five days of hospitalization
• Usually after 48 hrs from admission
Late onset HAP
occurs after 5 days of hospitalization
Bacterial Causes of Early Onset HAP
• Methicillin-sensitive Staphylococcus aureus (most)
• Haemophilus influenzae
• Enterobacteriaceae
• Streptococcus pneumoniae
Early Onset HAP treatment
ceftriaxone
Quinolone
ampicillin/sulbactam
Ertapenem
Bacterial Causes of Late Onset HAP
• Pseudomonas aeruginosa
• Acinetobacter spp.
• Enterobacteriaceae
• Methicillin-resistant S. aureus
Methicillin-resistant S. aureus treatment
either:
-antipsuedomonal b-lactam
-carbapenem
with:
quinolone
or
aminoglycoside (tobramycin/gentamycin)
if MRSA suspected:
add vancomycin or linezolid
b lactam adverse
diarrhea
nausea
vomiting
Doxycycline adverse
inhibits bone growth
teeth discoloration
Azithromycin and clarithromycin adverse
QT interval prolongation
fluoroquinolones adverse
Qt interval prolongation
torsades de pointes
vaginal candida
what should be separated from doxycycline and fluroquinolones
Calcium
Magnesium
Iron
-reduce drug absorption take several hours before or after
what drugs shouldnt be taken with QT interval prolonging drugs
azithromycin
clarithromycin
fluoroquinolones
what shouldnt be taken with hypoglycemic drugs
fluroquinolones
Clarithromycin inhibits
CYP3A4
dont give what with clarithromycin
CCB are metabolized by CYP3A4
-can lead to death, acute kidney injury, hypotension
pregnancy aviod
• Doxycycline: inhibition of bone growth.
• Clarithromycin: teratogenic in animals.
• Fluoroquinolones: arthropathy in animal studies, but observational data in pregnant women suggest that teratogenic effects are unlikely to occur at therapeutic doses.
pregnancy take
Amoxicillin or amoxicillin/clavulanate plus azithromycin can be used for outpatient treatment of pregnant women with CAP.