MSK Exam and Interventions PQs
1/22
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
23 Terms
A patient comes to an outpatient clinic reporting of neck problems. Which of the following exercise combinations is MOST APPROPRIATE for a patient who has a forward head posture?
A. Strengthen the deep cervical flexors and stretch the sternocleidomastoids and upper cervical extensors
B. Strengthen the deep cervical flexors and sternocleidomastoids and stretch the upper cervical extensors
C. Strengthen the cervical extensors and stretch the sternocleidomastoids and deep cervical flexors
D. Strengthen the cervical extensors and sternocleidomastoids and stretch the deep cervical flexors
A. Strengthen the deep cervical flexors and stretch the sternocleidomastoids and upper cervical extensors
RATIONALE: Janda’s upper crossed syndrome describes forward head posture and includes tightness in the upper trapezius and levator scapulae, pectoralis major and minor, and sternocleidomastoid, and weakness in deep cervical flexors, lower trapezius, and serratus anterior. So, you need to strengthen deep cervical flexors and stretch sternocleidomastoid and upper cervical extensors.
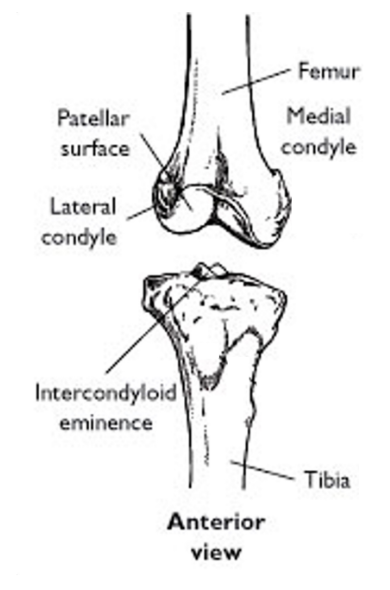
In the structure of the tibiofemoral joint, compare the lateral to medial femoral condyle.
What do these structural differences cause the tibia to do on the femur and at what range? What mechanism is this?
lateral femoral condyle is:
flatter
does not extend as far distally
projects further posteriorly
structural differences cause:
tibia to rotate laterally on femur at full extension
screw home mechanism

In regards to the knee joint, what is the FF tip of “TOLL” for the knee?
Tibia in Open chain goes Laterally for Locking
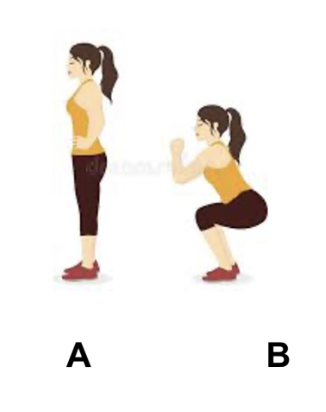
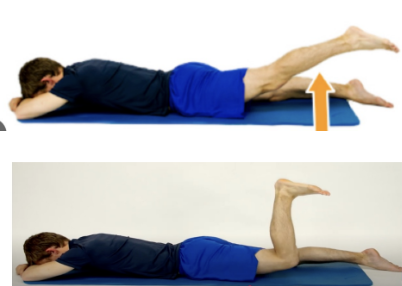
To unlock the knee, when going from position A to position B as shown in the image, which of the following motions is MOST LIKELY to occur?
A. Lateral rotation of the femur on the tibia
B. Medial rotation of the femur on the tibia
C. Lateral rotation of the tibia on the femur
D. Medial rotation of the tibia on the femur
A. Lateral rotation of the femur on the tibia
RATIONALE: During knee flexion ( From A to B) in a closed-chain movement, the femur undergoes lateral rotation on the tibia. This rotation allows the knee to unlock and flex into the squat position.
Which type of contraction do the biceps undergo as the shoulder
moves from 180° toward 90° of flexion?
Stand to Sit?
eccentric
eccentric
What are 3 upward rotators of the scapula?
3 downward rotators?
UPWARD ROTATORS:
upper trap
serratus anterior
lower trap
DOWNWARD ROTATORS:
rhomboids
levator scapulae
pectoralis minor
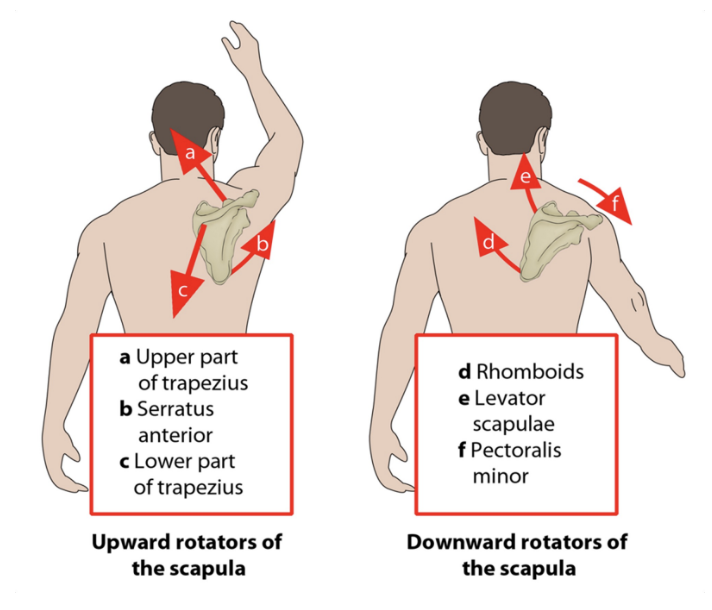
Excessive upward rotation of the left scapula is noted as the patient attempts shoulder abduction. Which of the following muscles is MOST LIKELY to contribute to excessive scapular rotation?
A. Weakness of serratus anterior
B. Weakness of lower trapezius
C. Weakness of rhomboid major & minor
D. Weakness of pectoralis major
C. Weakness of rhomboid major & minor
RATIONALE: Rhomboids is a downward rotator. If weak, it is not able to control the upward rotation, hence an excessive movement of upward rotation occurs. Strengthening the rhomboids would be the most appropriate intervention to improve downward rotation. Serratus anterior and lower trapezius are upwards rotators and they should have been tight to cause excessive upward rotation. Pec major does not cause rotation at the Scapula.
Training for daily activities will likely be geared towards what?
The focus of asking patients these types of questions is to always choose what type of interventions?
What is the first priority?
What is the second priority?
Questions addressing training will likely be geared towards the patient’s functional level
Pro tip: The focus of these questions is always to choose THE MOST APPROPRIATE interventions
• 1st priority should always be given to safety
• 2nd priority should always be placed on obeying the above while choosing the most relevant exercise to the desired task
A physical therapist is initiating passive and assisted movements for a patient who underwent surgical repair of a full-thickness rotator cuff tear six days ago. Which of the following positions is MOST APPROPRIATE for the patient?
A. Patient in sitting with arm abducted 70° with slight flexion
B. Patient is supine with arm abducted 45° with slight flexion
C. Patient in sitting with arm abducted 15° with slight flexion
D. Patient in supine with arm abducted 90° with slight flexion
B. Patient is supine with arm abducted 45° with slight flexion
RATIONALE: Patient is only 6 days post op so prefer supine over sitting for better stabilization. Arm abduction at 45 degrees is within safe limits and ROM. It is too soon to start with 90 degrees ROM less than a week post op. Thus B is appropriate to ensure the integrity of the repair.
For an achilles tendon repair, how long is it when using a conventional approach to weight-bear?
How about early remobilization approach?
Weight-bearing
• Conventional approach: 6 weeks immobilization and non-weight-bearing
• Early remobilization approach: Immediately after surgery or after 1 or 2 weeks
For an achilles tendon repair, how long is phase I?
Can you do active ROM?
At 2 weeks, what muscles do you focus on for setting?
Can you do weight-shifting activities? What positions?
What is permitted and why?
PHASE 1 (Up to 4-to-6 weeks )
• Active ROM of non-immobilized joints
• Muscle setting exercise of dorsiflexors, invertors, evertors and plantarflexors (at 2 weeks)
• Weight-shifting activities in bilateral stance while wearing the orthosis (when partial weight-bearing is permitted)
• No dorsiflexion permitted to prevent stretching of the tendon
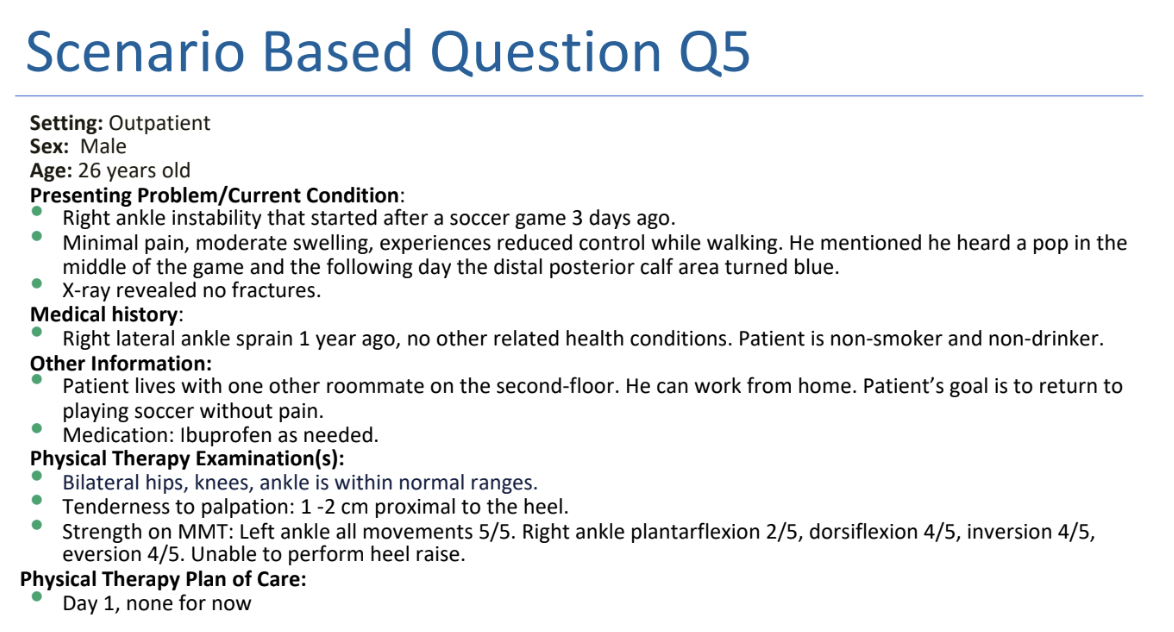
On examination, which special test is MOST LIKELY to be positive in this patient?
A. Anterior drawer test
B. Kleiger’s test
C. Thompson test
D. Talar tilt test
C. Thompson test
RATIONALE: The scenario describes, patient has an Achilles tendon rupture. The patient lies prone with his foot over the end of the table. contraction of the Achilles tendon, resulting in plantarflexion. If the Achilles tendon is completely ruptured, there will not be any apparent plantarflexion.
A- ATFL/ACL injury
B- Tibiofibular injury
C- Thompson’s is for Achilles tendon rupture
D- For CFL and deltoid sprain
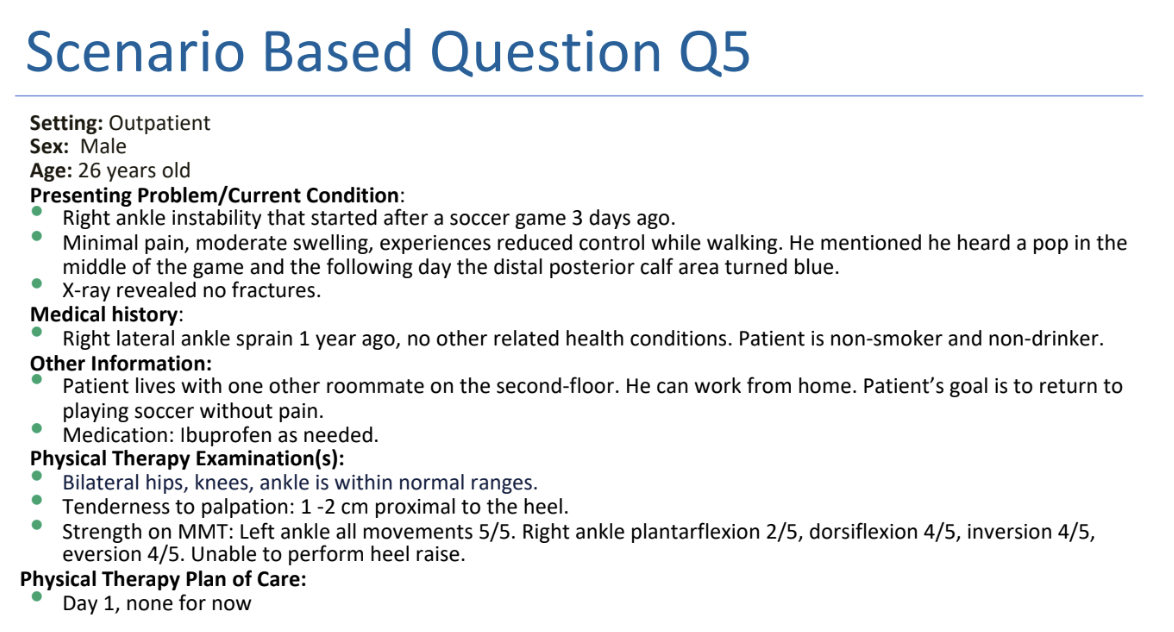
The patient underwent a right Achilles tendon repair and returned to the physical therapy clinic at 2 weeks wearing a controlled ankle motion (CAM) boot. Which of the following interventions would most likely be CONTRAINDICATED in the initial phase of rehab?
A. Hip and knee strengthening
B. Ankle muscle setting exercises
C. Heel raises in standing
D. Ambulation training with CAM boot
C. Heel raises in standing
RATIONALE: Heel raises in standing is an advanced exercise for the patient. A, b and D are safe during initial rehab.
The patient is 6 weeks post operative status and is now able to fully weight-bear. Which of the following shoe modifications would be MOST APPROPRIATE for the patient?
A. Normal shoes
B. Shoes with 1-1.5 cm heel lift
C. Shoes with lower than the regular heel
D. Shoes with 5 cm heel lift
B. Shoes with 1-1.5 cm heel lift
RATIONALE: Since the patient is six weeks post-op and fully able to weight bear; shoes with 1-1.5cm heel lift will keep the foot in slight plantarflexion and prevent excessive dorsiflexion that will cause strain on the repaired Achilles tendon. Shoes with 2-3 cm heel lift will cause extra plantarflexion and not recommended at 6 weeks. Normal shoes and lower than regular heel will cause excessive dorsiflexion that can strain the repaired tendon.
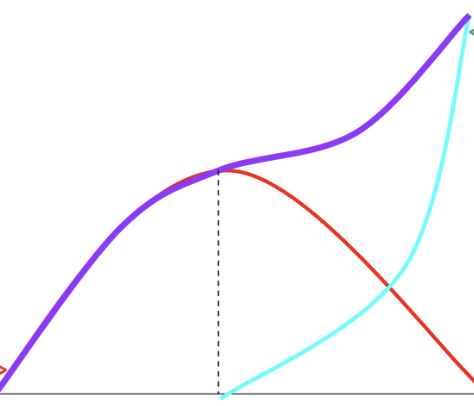
Understand this graph on active and passive insufficiency as a result of limitations in ROM due to the force-length relationship
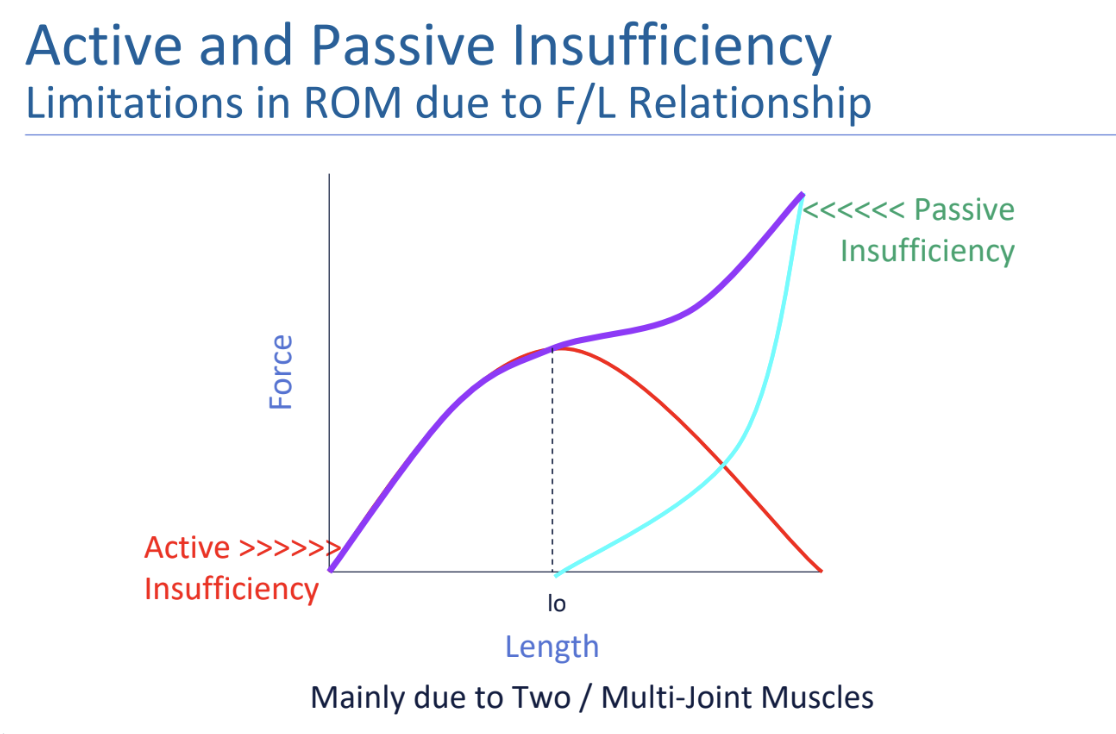
Differentiate active vs. passive insufficiency with what type muscle joint and what they can/cannot do.
Active Insufficiency
The inability of a two joint muscle to shorten simultaneously at
both joints
Passive Insufficiency
The inability of a two joint muscle to lengthen simultaneously at
both joints
When determining active and passive insufficiency, identify the 4 steps you should think about
Step 1: Name of the muscle
Step 2: Is it a two joint muscle?
Step 3: End range? Function of the muscle?
Step 4: Active or passive
A patient presents with reduced hip mobility, particularly during hip extension. The physical therapist notes that the patient experiences greater hip extension when the knee is extended compared to when the knee is flexed. What is the MOST LIKELY cause of the reduced hip extension with knee flexion?
A. Passive insufficiency of the hamstrings
B. Passive insufficiency of the gluteus maximus
C. Active insufficiency of the hamstrings
D. Active insufficiency of the rectus femoris
C. Active insufficiency of the hamstrings
RATIONALE: Active Insufficiency occurs when a muscle that crosses two joints cannot shorten enough to produce full range of motion at both joints simultaneously. The hamstrings cross both the hip and knee joints. When the knee is flexed and the hip is extended, the hamstrings are shortening at both the knee and the hip. This dual action can lead to active insufficiency of the hamstrings because they are unable to generate sufficient force in this overly shortened state. In contrast, when the knee is extended, the hamstrings are lengthened over the knee, which allows them to contract more effectively at the hip, thus improving hip extension. Passive insufficiency of the hamstrings: This occurs when a muscle cannot lengthen enough to allow full range of motion at both joints it crosses.
A worker reports of difficulty gripping their tools tightly, and they repeatedly fall from their hand. On examination, the physical therapist notices that they can grip the tools tightly with their wrist in extension but struggles to do so with the wrist in flexion. What is the MOST LIKELY cause of this issue?
A. Passive insufficiency of both flexor digitorum profundus and extensor digitorum
B. Passive insufficiency of flexor digitorum and active insufficiency of extensor digitorum
C. Active insufficiency of flexor digitorum profundus and passive insufficiency of extensor digitorum
D. Active insufficiency of both flexor digitorum profundus and extensor digitorum
C. Active insufficiency of flexor digitorum profundus and passive insufficiency of extensor digitorum
RATIONALE: When the wrist is flexed, the flexor digitorum profundus becomes shortened, limiting its ability to generate force for gripping. This is active insufficiency, The extensor digitorum is in a stretched position when the wrist is flexed, reducing its ability to extend the fingers efficiently. This is passive insufficiency. The flexor digitorum profundus (finger flexors) becomes actively insufficient, and the extensor digitorum (finger extensors) becomes passively insufficient, both contributing to the worker's difficulty gripping with the wrist in flexion.
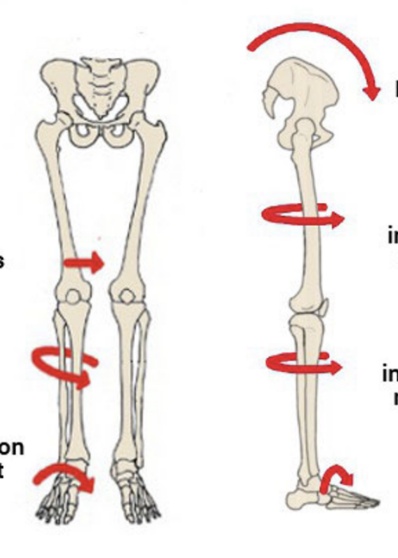
Understand this graphic of the kinematic chain
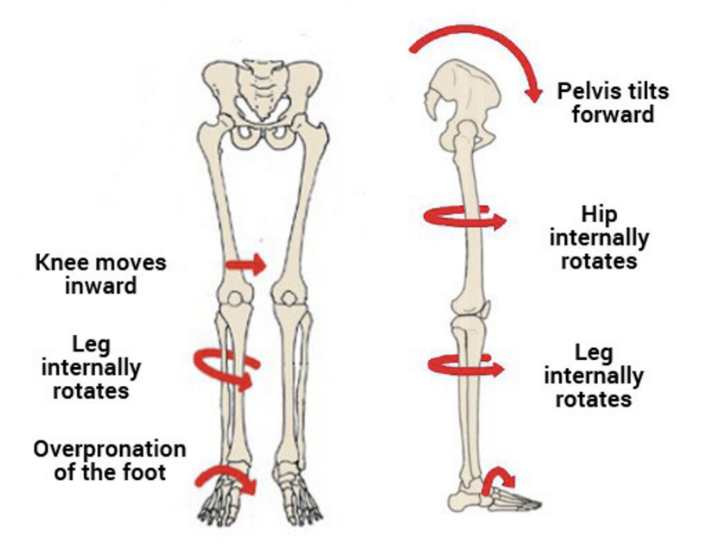
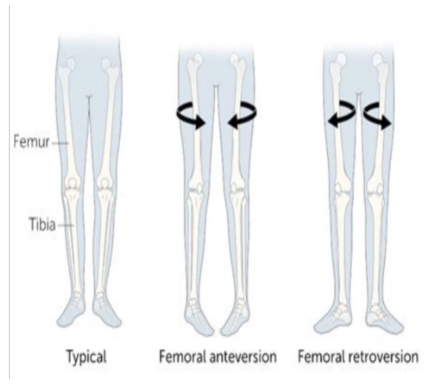
In a femoral anteversion posture, know the position of the:
hip
tibia
subtalar
toe
patellae
● Hip internal rotation
● Tibial internal torsion
● Subtalar pronation
● Toe in
● Squinting patellae
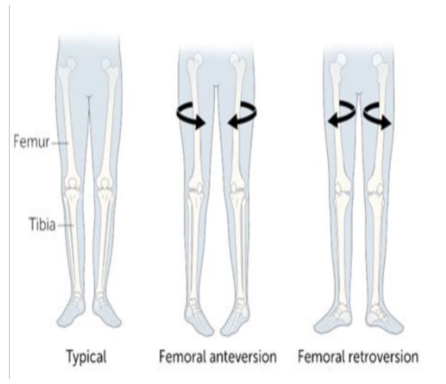
In a femoral retroversion posture, know the position of the:
hip
tibia
subtalar
toe
patellae
● Hip external rotation
● Tibial external torsion
● Subtalar supination
● Toe out
● Frog-eyed patellae
A patient reports of foot pain during running, and the physical therapist observes excessive foot pronation. Which of the following orthotic interventions would MOST LIKELY benefit this patient?
A. Medial post under first metatarsal head
B. Cushion heel
C. Lateral post under fifth metatarsal head
D. Posterior leaf spring
A. Medial post under first metatarsal head
RATIONALE: Correction of the overpronation can be done by a medial post placed just proximal to the first metatarsal head. This approach involves bringing the ground up to meet the foot. A post under the fifth metatarsal head would accentuate the problem. Cushion heel can be used for plantar fasciitis and a posterior leaf spring is used for a foot drop. Posterior leaf spring is used in weak dorsiflexors conditions.