Chapter 28: Cardiovascular Diagnostic and Therapeutic Procedures
1/28
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
29 Terms
Chapter 28: Cardiovascular Diagnostic and Therapeutic Procedures
Evaluate heart function by:
Measuring cardiac enzymes in blood
Using ultrasound to visualize heart structure and motion
Assessing cardiac response to exercise
Using catheters to assess blood volume, perfusion, fluid status, pumping ability, and degree of arterial blockage
Common procedures nurses should know:
Cardiac enzymes and lipid profile
Echocardiography
Stress testing
Hemodynamic monitoring
Angiography
Therapeutic procedures:
Central vascular access placement
Percutaneous coronary interventions
Cardiac Enzymes and Lipid Profile
Cardiac enzymes are released into the bloodstream when myocardial injury occurs
Lipid profile evaluates cholesterol levels and risk for heart disease
Cardiac enzymes are specific markers for diagnosing myocardial infarction (MI)
Indications
Angina
Myocardial infarction
Heart disease
Hyperlipidemia
Cardiac Enzymes and Lipid Profile Considerations
Preprocedure Considerations
Fast for 12 to 14 hours before lipid profile sampling
Interpretation of Findings: Cardiac Enzymes
Creatine kinase MB isoenzyme
Reference range: 0 percent of total CK (20 to 200 units/L)
Detectable after MI: 3 to 6 hours
Duration of elevation: 2 to 3 days
More sensitive to myocardium
Troponin T
Reference range: less than 0.1 ng/mL
Detectable after MI: 2 to 3 hours
Duration of elevation: 10 to 14 days
Troponin I
Reference range: less than 0.03 ng/mL
Detectable after MI: 2 to 3 hours
Duration of elevation: 7 to 10 days
Myoglobin
Reference range: less than 90 mcg/L
Detectable after MI: 2 to 3 hours
Duration of elevation: 24 hours
Interpretation of Findings: Lipid Profile
Total cholesterol
Less than 200 mg/dL
Screens for heart disease
LDL
Less than 130 mg/dL
“Bad” cholesterol
Transports cholesterol from liver to body cells
Triglycerides
Males: 40 to 160 mg/dL
Females: 35 to 135 mg/dL
Evaluates risk for heart disease
HDL
Females: greater than 55 mg/dL
Males: greater than 45 mg/dL
“Good” cholesterol
Protects coronary arteries by transporting cholesterol back to the liver
The nurse at the provider’s office is reviewing the laboratory test results for the client. The nurse should identify that which of the following results indicates the client is at risk for heart disease?
Select all that apply.
a
Cholesterol (total) 245 mg/dL
b
HDL 90 mg/dL
c
LDL 140 mg/dL
d
Triglycerides 125 mg/dL
e
Troponin I 0.02 ng/mL
a
Cholesterol (total) 245 mg/dL
c
LDL 140 mg/dL
Transthoracic Echocardiography (TTE)
Noninvasive ultrasound test
Diagnoses valve disorders and cardiomyopathy
Evaluates heart size, shape, motion, and ejection fraction
Indications
Cardiomyopathy
Heart failure
Angina
Myocardial infarction
Transthoracic Echocardiography (TTE) Considerations
Preprocedure
Explain test is noninvasive and lasts up to 1 hour
Intraprocedure
Client lies on left side and remains still
Postprocedure
Review results and discuss follow up plan
Transesophageal Echocardiography (TEE)
Provides clearer images than TTE due to less tissue interference
Transducer passed through mouth into esophagus
Indications
Heart failure
Valvular heart disease
Atrial or ventricular thrombi
Monitoring during valve replacement or CABG surgery
Transesophageal Echocardiography (TEE) Considerations
Preprocedure
Obtain informed consent
NPO for 4 to 6 hours
Establish IV access
Intraprocedure
Monitor level of consciousness, ECG, blood pressure, heart rate, respiratory rate, and oxygenation
Moderate sedation required
Postprocedure
Monitor vital signs, oxygenation, and return of gag reflex
Maintain head of bed at 45 degrees
Stress Testing
Exercise stress test involves walking on a treadmill
Evaluates cardiac workload and response to stress
Test stopped when target heart rate is achieved
Pharmacologic stress testing used if exercise not tolerated
Indications
Angina
Heart failure
Myocardial infarction
Dysrhythmias
Stress Testing Considerations
Preprocedure
Obtain informed consent
Explain treadmill exercise and recommend athletic clothing
Pharmacologic agents may include dipyridamole, adenosine, regadenoson, or dobutamine
Fast 2 to 4 hours prior per facility policy
Avoid tobacco, alcohol, and caffeine
Encourage adequate rest the night before
Intraprocedure
Apply 12 lead ECG
Monitor for dysrhythmias
Instruct client to report chest pain, shortness of breath, or dizziness
Postprocedure
Continue ECG monitoring
Check blood pressure until stable
Provider reviews results with client
Hemodynamic Monitoring (Image)
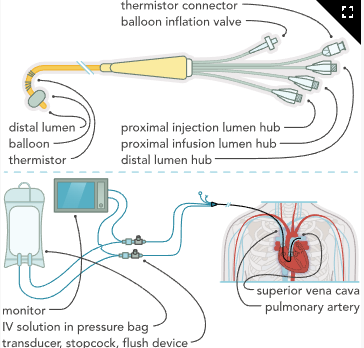
Hemodynamic Monitoring
Uses indwelling catheters to assess:
Blood volume
Perfusion
Fluid status
Cardiac pumping effectiveness
Key parameters:
Central venous pressure (CVP)
Pulmonary artery pressure (PAP)
Pulmonary artery wedge pressure (PAWP)
Cardiac output (CO)
Intra arterial blood pressure
Mixed venous oxygen saturation (SvO₂)
Indicates balance between oxygen supply and demand
Measured via pulmonary artery catheter with fiber optics
Monitoring System Components
Pressure transducer
Pressure tubing
Monitor
Pressure bag and flush device
Arterial Lines
Common insertion sites: radial, brachial, femoral
Provide continuous blood pressure monitoring
Allow arterial blood sampling
Pressures differ from cuff readings
Nursing care
Verify waveform accuracy
Monitor circulation distal to site
Assess for bleeding
Maintain secure connections
Not used for IV fluid administration
Pulmonary artery (PA) catheters
Inserted into large vein and threaded through right atrium and ventricle into pulmonary artery
Multiple lumens and ports allow measurement and sampling
Proximal lumen
Measures CVP
Infuses IV fluids
Obtains venous blood samples
Distal lumen
Measures PAP and PAWP
Not used for IV fluids
Balloon inflation port
Used intermittently for PAWP
Keep deflated and locked when not in use
Thermistor
Measures temperature differences to calculate CO
Additional infusion ports may be present
Indications for PA Catheter
Serious or critical illness
Heart failure
Post CABG
ARDS
Acute kidney injury
Burn injury
Trauma
CVP
PAP
PAWP
Hemodynamic Monitoring Considerations
Ensure client understanding and obtain informed consent
Assemble and purge monitoring system
Maintain sterile technique
Position client supine or Trendelenburg
Administer sedation and analgesia as prescribed
Level transducer at phlebostatic axis (4th intercostal space, midaxillary line)
Zero system to atmospheric pressure
Obtain baseline readings
Compare arterial and noninvasive blood pressure
Document client response
Intraprocedure Monitoring
Watch for signs of altered hemodynamics
Manifestations of Altered Hemodynamics
Preload indicators
Right heart: CVP
Left heart: PAWP
Elevated preload
Crackles
Jugular vein distention
Hepatomegaly
Peripheral edema
Taut skin turgor
Decreased preload
Poor skin turgor
Dry mucous membranes
Afterload indicators
Right heart: pulmonary vascular resistance
Left heart: systemic vascular resistance
Elevated afterload
Cool extremities
Weak peripheral pulses
Decreased afterload
Warm extremities
Bounding peripheral pulses
Postprocedure Nursing Actions
Obtain chest x ray to confirm placement
Continuous monitoring of vital signs, heart rhythm, and oxygenation
Compare arterial and noninvasive blood pressure
Maintain catheter integrity
Observe and document waveforms
Report waveform changes promptly
Document catheter placement each shift and after transport
Secure all connections
Obtain hemodynamic readings with client supine
Head of bed may be elevated 15 to 30 degrees
Level and zero transducer with position changes
Trend values over time
Correlate findings with physical assessment
Expected Hemodynamic Values
CVP: 8 to 12 mm Hg
Pulmonary artery systolic: 15 to 28 mm Hg
Pulmonary artery diastolic: 5 to 16 mm Hg
PAWP: 6 to 15 mm Hg
Cardiac output: 3 to 6 L/min
SvO₂: 60 to 80 percent
Older adults may have lower values due to reduced intravascular volume
Hemodynamic Monitoring Complications
Infection or sepsis
Caused by poor aseptic technique
Nursing actions
Change dressings per protocol
Use surgical aseptic technique
Monitor WBC and temperature
Perform hand hygiene
Collect cultures as ordered
Administer antibiotics
Provide IV fluids
Administer vasopressors for sepsis related vasodilation
Embolism
Caused by clot or air entry
Nursing actions
Flush system with 0.9 percent sodium chloride per protocol
Can include heparin
Avoid air introduction
Monitor for pneumothorax
Monitor for dysrhythmias during insertion or movement
Angiography
Invasive diagnostic procedure to evaluate presence and degree of coronary artery blockage
Can also include arterial, venous, cerebral, liver, or extremity angiograms
Catheter inserted into femoral, brachial, or radial vessel and threaded to right or left heart
Contrast media injected and visualized under fluoroscopy to identify narrowing or occlusion
Indications
Unstable angina with ECG changes
T wave inversion
ST segment elevation or depression
Confirmation of location and extent of heart disease
Angiography Considerations
Preprocedure Nursing Actions
Maintain NPO for at least 4 hr (aspiration risk)
Obtain baseline vital signs
Auscultate heart and lung sounds
Assess and document peripheral pulses
Verify informed consent
Ensure client and family understand the procedure
Assess renal function prior to contrast administration
Contrast considerations
Iodine contrast is not automatically contraindicated with shellfish allergy
Further assessment required
Administer premedications if prescribed
Methylprednisolone
Diphenhydramine
Metformin management
Clarify provider orders
Often withheld before and up to 48 hr after procedure (risk of lactic acidosis)
Client Education (Preprocedure)
Mild sedative and local anesthetic will be used
Warmth or flushing may occur with dye injection
Groin is the most common access site
Pressure will be applied after procedure
If no vascular closure device, keep extremity straight for prescribed time
Intraprocedure Nursing Actions
Administer sedatives and analgesics as prescribed
Continuous monitoring
Vital signs
Heart rhythm
Chest pain
Be prepared to treat dysrhythmias
Ensure resuscitation equipment and emergency medications are available
Postprocedure Nursing Actions
Vital signs monitoring
Every 15 min x4
Every 30 min x2
Every hour x4
Then every 4 hr per protocol
Assess affected extremity at same intervals
Bleeding or hematoma
Thrombosis (pedal pulse, color, temperature)
Maintain bed rest
Supine position
Extremity straight for prescribed time
Vascular closure device may be used to promote hemostasis
Older adults may require pain management due to arthritis during prolonged bed rest
Continuous cardiac monitoring
Reperfusion after angioplasty can cause dysrhythmias
Administer medications as prescribed to prevent clot formation
Aspirin
Clopidogrel or other antiplatelets (ticagrelor, prasugrel, cangrelor)
Heparin
Enoxaparin
GP IIb/IIIa inhibitors (eptifibatide)
Monitor urine output and hydrate
Contrast acts as an osmotic diuretic
Assist with sheath removal
Apply pressure for prescribed time
Observe for vagal response (hypotension, bradycardia)
Withhold metformin for 48 hr after procedure
Client Education (Postprocedure)
Leave dressing in place for 24 hr
Avoid strenuous activity as instructed
Report immediately
Bleeding at insertion site
Chest pain
Shortness of breath
Color or temperature changes in extremity
Activity restrictions
No lifting over 10 lb if groin access
No lifting over 5 lb if arm or wrist access
Resume metformin only as prescribed
If Stent Placement Performed
Take antiplatelet therapy as prescribed (up to 12 months)
Take medications at the same time daily
Attend scheduled lab monitoring
Bleeding precautions
Soft toothbrush
Wear shoes out of bed
Lifestyle modifications
Weight management
Low fat, low sodium diet
Regular exercise
Smoking cessation
The nurse is teaching the client who is scheduled for a coronary angiography. Which of the following statements should the nurse make?
a
"You should have nothing to eat or drink for 2 hours prior to the procedure.”
b
“You will be given general anesthesia during the procedure.”
c
“You should not have this procedure done if you are allergic to eggs.”
d
“You will need to keep your affected leg straight following the procedure.”
d
“You will need to keep your affected leg straight following the procedure.”
The nurse is teaching the newly licensed nurse about caring for the client who is to have a CVP line placed. Which of the following statements by the newly licensed nurse indicates an understanding?
a
"Air should be instilled into the monitoring system prior to the procedure.”
b
“The client should be positioned on the left side during the procedure.”
c
“The transducer should be level with the second intercostal space after the line is placed.”
d
“A chest x-ray is needed to verify placement after the procedure.”
d
“A chest x-ray is needed to verify placement after the procedure.”
Angiography Complications
Artery Dissection
Perforation of artery by catheter
Can lead to cardiac tamponade or emergency CABG
Manifestations
Severe hypotension
Tachycardia
May require balloon occlusion and reversal of anticoagulation
Cardiac Tamponade
Fluid accumulation in pericardial sac
Manifestations
Hypotension
Jugular venous distention
Muffled heart sounds
Paradoxical pulse (≥10 mm Hg systolic drop with inspiration)
Hemodynamic findings
Equalized and elevated intracardiac and PAP pressures
Nursing Actions
Notify provider immediately
Administer IV fluids
Obtain chest x ray or echocardiogram
Prepare for pericardiocentesis
Monitor hemodynamics and heart rhythm
Monitor for dyspnea and provide oxygen
Hematoma Formation
Local clot formation at insertion site
Nursing Actions
Assess sensation, color, capillary refill, and pulses distal to site
Inspect groin at prescribed intervals
Apply pressure for bleeding
Notify provider
Allergic Reaction to Contrast Media
Manifestations
Chills
Fever
Rash
Wheezing
Tachycardia or bradycardia
Nursing Actions
Monitor closely
Maintain resuscitation readiness
Administer diphenhydramine or epinephrine if prescribed
External Bleeding
Nursing Actions
Monitor site for bleeding or swelling
Apply direct pressure
Keep extremity straight
Embolism
Dislodged plaque or clot
Nursing Actions
Monitor for chest pain
Monitor vital signs and SaO₂
Restenosis
Reocclusion of treated vessel
Can occur immediately or weeks later
Nursing Actions
Monitor ECG
Assess chest pain
Notify provider
Prepare for return to cath lab
Retroperitoneal Bleeding
Bleeding into retroperitoneal space from femoral puncture
Nursing Actions
Assess for flank pain and hypotension
Notify provider immediately
Apply firm pressure
Administer IV fluids and blood products
Client Education
Keep leg straight
Report chest pain or shortness of breath
Acute Kidney Injury
Caused by nephrotoxic contrast agent
Nursing Actions
Monitor urine output
Monitor BUN, creatinine, electrolytes
Promote hydration (oral or IV)
Cardiac Catheters (image)
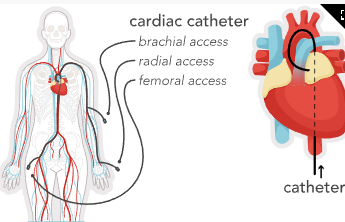
Vascular Access
Type and site depend on therapy characteristics
Medication type
pH and osmolarity
Duration of therapy
Goal
Minimize catheter insertions
Reduce complication risk
Central Intravenous Therapy
Used for rapid hemodilution in the superior vena cava
Confirm tip placement with x ray before use
Inserted using sterile technique
Locations include OR, bedside, or outpatient setting
Types
Nontunneled percutaneous CVC
Tunneled CVC (Hickman, Groshong)
PICC
Implanted port
Nontunneled Percutaneous CVC
Length: 18 to 25 cm
Lumens: 1 to 5
Short term use (<6 weeks)
Insertion sites
Subclavian
Jugular
Tip location: distal third of SVC
Indications
Emergent or trauma use
Blood administration
Chemotherapy
Antibiotics
Total parenteral nutrition
Tunneled Percutaneous CVC
Long term use
Catheter tunneled subcutaneously with cuff
Tissue growth anchors catheter
Reduces infection risk
No dressing required after healing
Groshong catheter
Pressure sensitive valve
Prevents blood reflux
No clamp required
Indications
Frequent or long term vascular access
Peripherally Inserted Central Catheter (PICC)
Length: 45 to 74 cm
Single or multiple lumens
Duration: up to 12 months
Insertion site
Basilic or cephalic vein
At least one fingerbreadth above or below antecubital fossa
Tip location: lower third of SVC
Indications
Long term antibiotics
Chemotherapy
TPN
Insert early to preserve peripheral veins
Vascular Access Considerations
Preprocedure
Verify informed consent
Cleanse site with chlorhexidine
Ensure sterile equipment
Restrict room traffic during insertion
Postprocedure
Confirm placement with x ray
Assess site for redness, swelling, drainage, tenderness
Clean port with alcohol for 15 seconds and allow to dry
Use transparent dressing
Change every 7 days or as needed
Do not immerse arm in water
Avoid BP measurements or venipuncture in PICC arm
Flushing Guidelines (INS)
Use 10 mL syringe
Flush with 10 mL normal saline
Before, between, and after medications
Flush with 20 mL normal saline after blood draws
Flush with 5 mL heparin (10 units/mL) when not in use
Do not flush if resistance is met
Implanted Port
Description
Small reservoir with thick septum
Placement
Implanted in chest wall pocket
Catheter tip in SVC
Indications
Long term therapy (≥1 year)
Common for chemotherapy
Accessing the Port
Only trained personnel
Use mask and aseptic technique
Use noncoring (Huber) needle
Confirm blood return before infusion
Maintenance
Flush with heparin or saline after each use
Flush at least monthly when not in use
Vascular Access Complications
Phlebitis
Causes
Chemical (pH, osmolarity)
Bacterial
Mechanical
Manifestations
Erythema
Pain or burning
Warmth
Edema
Induration or red streak
Slowed infusion
Fever
Prevention
Hand hygiene
Regular site assessment
Sterile dressing changes
Chlorhexidine skin prep
Occlusion
Blockage from thrombosis or emboli
Nursing Actions
Flush per policy
Do not force flush
Use 10 mL syringe to avoid catheter rupture
Mechanical Complications
Dislodgement of port or catheter tip
Nursing Actions
Use only noncoring needle for ports
Client Education
Report swelling, port movement, or inability to access port
Report gurgling sounds or neck or ear pain immediately
A nurse is teaching a newly licensed nurse about vascular access devices. Match the following vascular access devices with the associated characteristics.
Used for short-term access
Percutaneous inserted central catheter (PICC)
Nontunneled percutaneous central venous catheter
Percutaneous inserted central catheter (PICC)
Surgically inserted into the chest wall
Nontunneled percutaneous central venous catheter
Used for short-term access
Nontunneled percutaneous central venous catheter
Inserted above or below the antecubital fossa
Percutaneous inserted central catheter (PICC)
Surgically inserted into the chest wall
Implanted port