Cardiovascular Physiology
1/73
Earn XP
Description and Tags
zool 463 cardiovascular physiology
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
74 Terms
Cardiovascular system
The system responsible for moving fluids around the body, including blood and hemolymph.
What is circulation? What is the circulatory system?
Pressure-driven bulk flow of body fluids through a system of tubular vessels to all parts of the body.
The system of blood vessels that body fluids travel through.
Convective transport
Transport of substances by means of bulk flow in the circulatory system.
Volumetric flow Rate (Q) (what is the formula)
Volume passing through a cross-sectional area per unit time, expressed as m³/s or L/min.
A: cross sectional area (m²)
V: velocity (m/s)
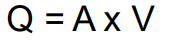
What is one of the properties of Q?
Q is conserved in closed systems. This means if a vessel narrows in diameter, then the velocity will increase to maintain a consistent Q. If the vessel splits into 2 vessels, the Q of the two vessels sum to be equivalent to the Q of the initial vessel.
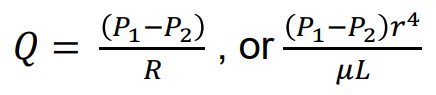
Hagen-Poiseuille Law (what is the formula and what does each thing mean)
P1 – P2 = pressure drop in the pipe (Pa)
U = dynamic viscosity of the fluid (Pa X s)
L = length of the pipe (m)
Q = volumetric flow rate (m3 /s)
r = radius (m)
R = flow resistance
Aorta and Arteries
They deliver oxygenated blood throughout the body and smooth out pressure changes from the pulsatile nature of the heart.
Arterioles
Small blood vessels that regulate blood into capillaries flow by constricting or dilating to alter the resistance.
Systole (how do arteries smooth it out?)
The contraction phase of a heart chamber. Arteries stretch to accomodate increased blood volume.
Diastole (how do arteries smooth it out?)
The relaxation phase of a heart chamber. The arterial wall recoils to maintain flow.
Capillaries
Smallest blood vessels that allow for gas and nutrient exchange.
Precapillary sphincters
Rings of smooth muscle at the entrance of capillary beds that regulate blood flow.
What are the three kinds of capillary walls? Describe them.
continuous: tightly joined walls (usually in skin/muscle)
sinusoidal: have large gaps to allow large protein and cell movement (liver, spleen, bone marrow)
fenestrated: small pores for large molecules to pass (kidney + intestine)
Veins
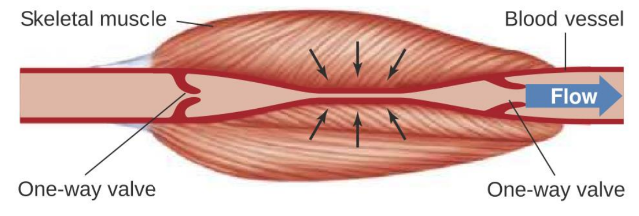
They contain lots of one way valves that prevent backflow and have basically no pressure (since blood loses pressure upon return from the capillaries)
If veins have no blood pressure, how do they return blood to the heart?
Either pumped back through contraction and relaxation of skeletal muscle (ie. in calves) or by smooth muscle constriction.
Which vessels have the most TOTAL cross sectional area? What does this mean about the linear velocity of blood in that vessel? Why is this?
Capillaries have the most total cross sectional area, which means that they have the least linear velocity of all blood vessels.
This is because the larger total area allows for more exchange of gases and nutrients, resulting in slower blood flow.
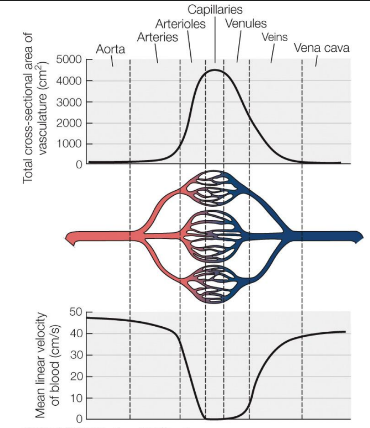
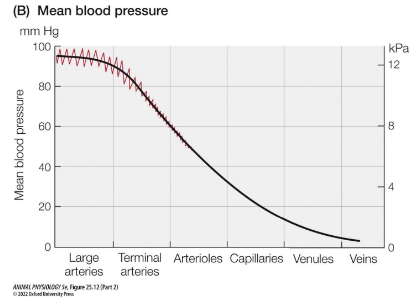
How does blood pressure change as it travels from the heart (arteries) to the tissues (capillaries) back to the heart (veins)?
Blood pressure decreases as it travels from arteries to capillaries due to increased resistance and the total cross-sectional area of capillaries, then continues to decrease in veins as the blood returns to the heart.
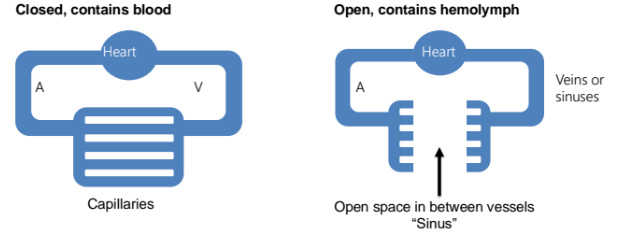
Closed vs Open system
closed system means blood is confined only to vessels and doesn’t fill open space.
has higher pressure
mostly vertebrates
open system contains hemolymph, which enters the sinus (open space)
lower pressure but less efficient
arthropods and mollusks
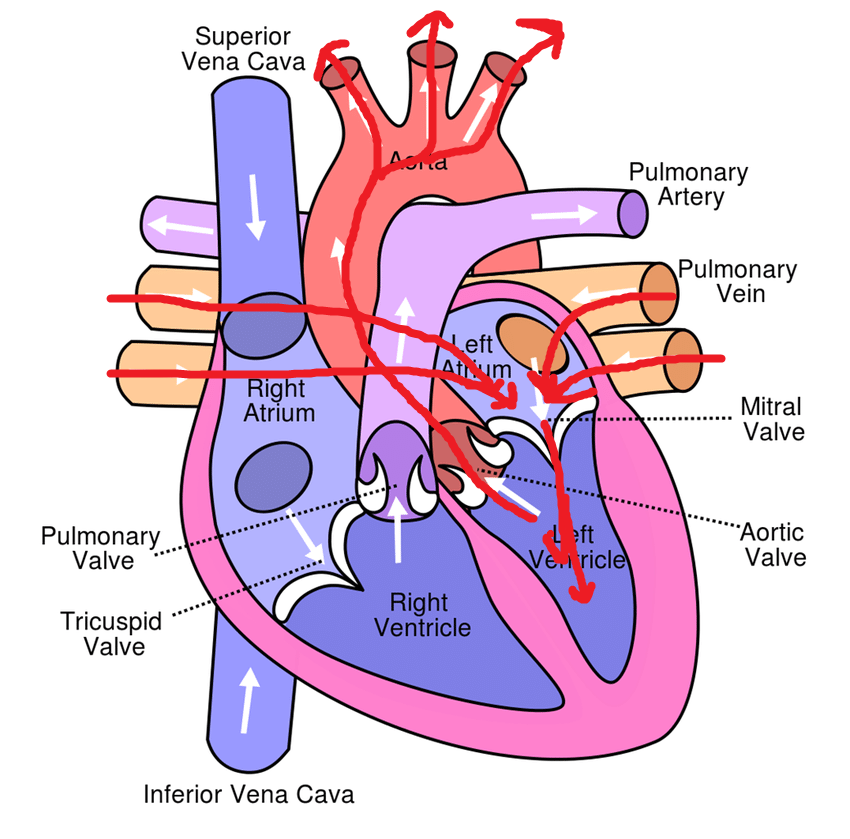
Atria or Atrium
Upper chambers of the heart that receive blood. There is a right and left atrium.
Ventricles
Lower chambers of the heart that pump blood out. There is a left and right ventricle.
How does deoxygenated blood from tissues enter the heart and go to the lungs?
It enters from the inferior and superior vena cava, which fills the right atrium. This blood is then pumped into the right ventricle (passing the tricuspid valve). It then passes through the semilunar pulmonary valve to enter the pumonary artery.
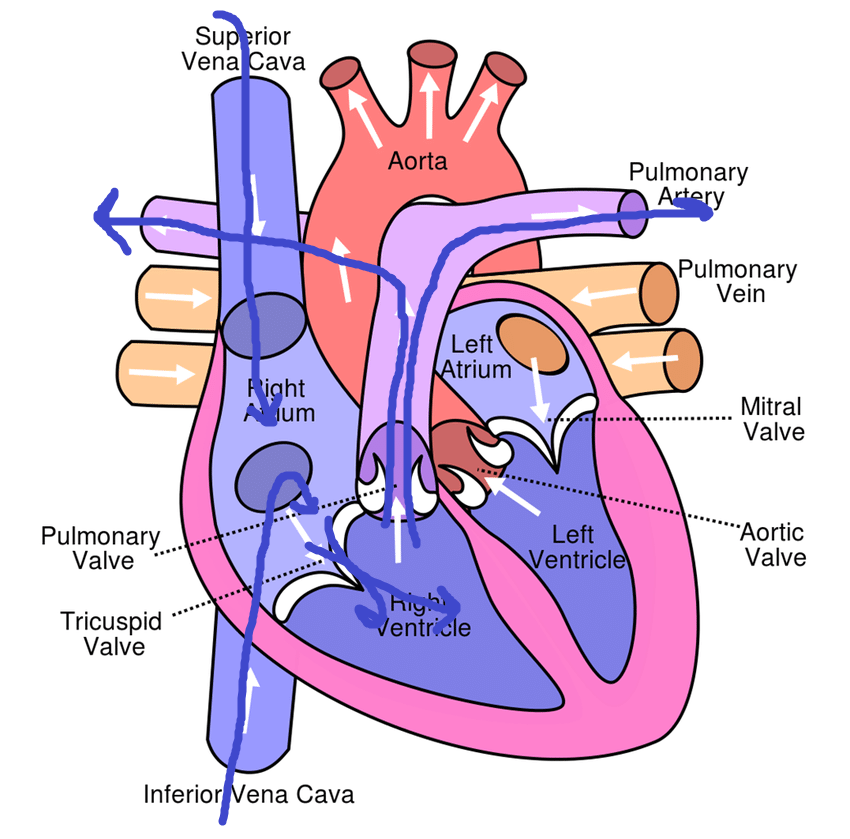
How does oxygenated blood from the lungs get distributed to the bodily tissues from the heart?
Oxygenated blood from the lungs enters the left atrium through the pulmonary veins, then it is pumped into the left ventricle (passing through the mitral valve) and leaves to be distributed through the aorta (passing the semilunar aortic valve) to the body's tissues.
Formula for cardiac output?
cardiac output = heart rate (bpm) * stroke volume (mL/beat)
Difference in pressure between right and left heart circuit
The difference in pressure between the right and left heart circuits is due to the varying levels of resistance in the pulmonary and systemic circulation, with the left side generating higher pressure to pump blood throughout the body.
Why does the left ventricle have thicker walls than the right ventricle?
The left ventricle has thicker walls than the right ventricle because it needs to generate higher pressure to pump oxygenated blood throughout the entire body, while the right ventricle only pumps blood to the lungs.
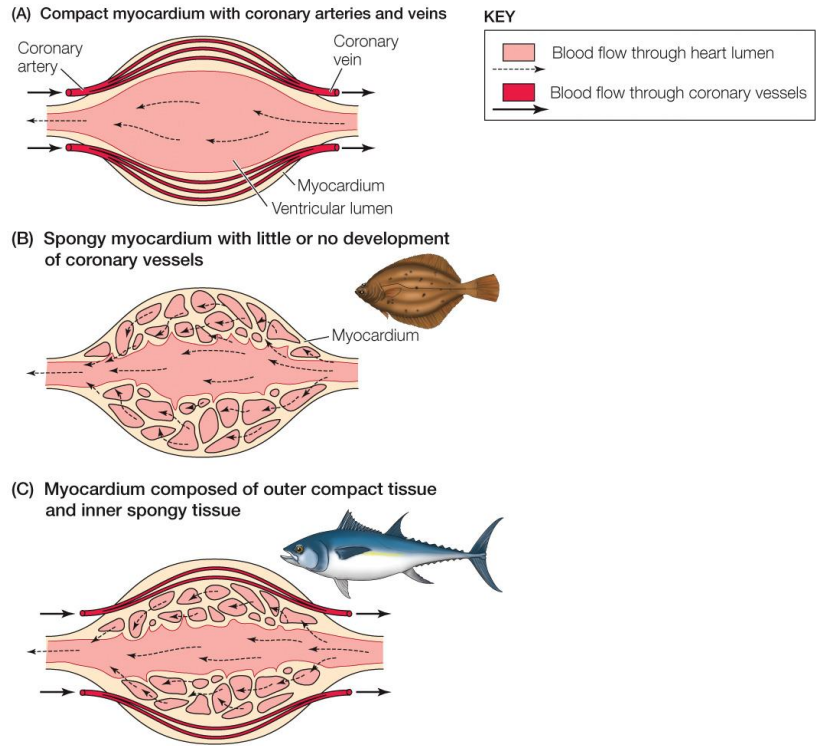
compact vs spongy myocardium (heart muscle)
Compact myocardium is densely arranged and is present in mammals who need high pressure.
Spongy myocardium is less dense, and have a rich capillary network. More common in low pressure circulatory systems and in animals with lower metabolic demand.
Describe the flow of blood in a fish's circulatory system. How is it different from mammals?
Fish have a single circulatory system, meaning blood passes through the heart only once during each full circuit.
Pathway:
Heart → Ventral Aorta → Gills → Dorsal Aorta → Body → Veins → Heart
What are the four chambers of a fish heart, and what is the role of the conus arteriosus in some species?
The fish heart has four sequential chambers:
Sinus venosus – receives venous (deoxygenated) blood
Atrium – pumps blood into the ventricle
Ventricle – muscular chamber, main force generator
Conus arteriosus – muscular outflow tract that contracts in sequence with the ventricle (found in species like sharks, lungfish)
🔄 The conus arteriosus helps even out pressure and maintain smoother blood flow into the delicate gill capillaries.
What are two main challenges fish face with their circulatory system?
Challenge 1:
After passing through the gills, blood pressure drops significantly, so when it reaches the body, the driving force is weak.
Challenge 2:
The heart itself receives deoxygenated blood, and its muscle (spongy myocardium) relies on this poorly oxygenated blood for fuel.
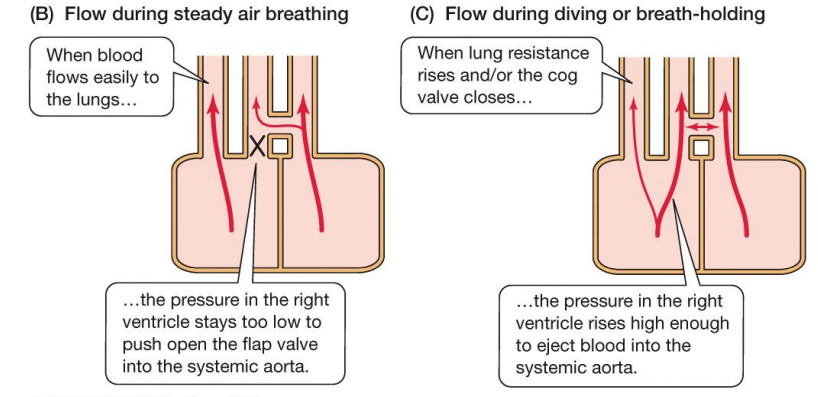
What is shunting? What is the tradeoff and why can’t mammals do it?
Some animals are able to redirect their blood flow away from certain areas by altering the resistance of different vessels. This allows (usually low metabolic demand) animals to skip the heart or lungs when blood is needed elsewhere.
Shunting can often involve skipping the pulmonary circuit, meaning that blood will not be reoxygenated. This means only animals with lower metabolic demands can afford to do it, as mammals and birds have too high metabolic demands.
Key anatomical features of an amphibian heart
The amphibian heart typically has three chambers: two atria and one ventricle.
It also has a central conus arteriosus, seperated by a fold to direct some blood into either the pulmonary artery or into the systemic circulation.
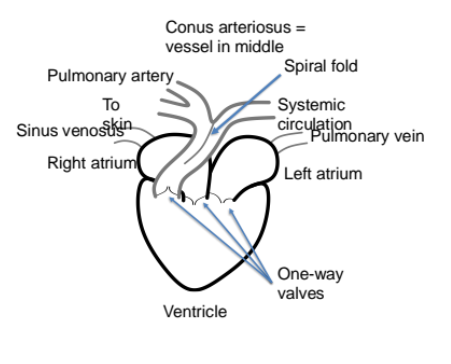
Explain the amphibian heart pumping pathway
Oxygenated blood (R) and deoxygenated blood (L) pool into the ventricle, but don’t mix much. Upon contraction, thr deoxygenated blood leaved through the conus arteriosus into the pulmonary artery. After, the oxygenated bloof flows through the conus arteriosus into the systemic circulation.
Amphibian shunting
Air breathing: directs O2 blood and low O2 blood do different parts of body
Breath holding: consrtivt pulmonary vessel, bypasses lungs.
Reptilian heart, how does it shunt?
Similar to mammalian heart, but has a right and left aorta connected by the fomaen of Panizza.
Air breathing: deoxygenated blood doesnt enter the systemic aorta as its closed by a valve
Breath holding: deoxygenated blood enters systemic aorta
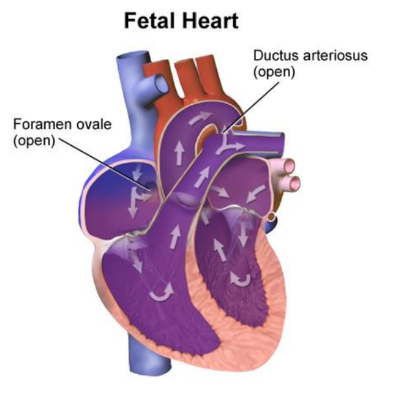
How does the mammalian fetus bypass the lungs? (2 pathways)
The mammalian fetus bypasses the lungs through the foramen ovale and ductus arteriosus. The foramen ovale allows blood to flow from the right atrium to the left atrium, while the ductus arteriosus connects the pulmonary artery to the aorta, directing blood away from the non-functioning lungs. These two ducts close upon birth.
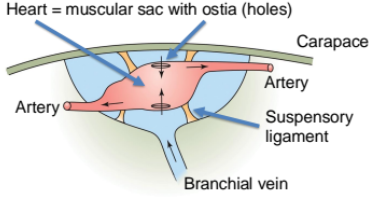
How does the heart work in a lobster’s open circulatory system?
The heart is surrounded by a sinus connected to the branchial vein. Heart contracts, hemolymph flows out of the heart into the arteries. The heart expands and the ostia valves open to suck in hemolymph.
closed and open system examples of multiple hearts.
Closed: octopus
has a systemic heart and two branchial hearts since they have 3 gills.
Open: insect
hemolymoh moves through body cavity by hearts in multiple places
Cardiac muscle
Striated muscle tissue that makes up the heart. They are mononucleated and have a branched structure. They have troponin and tropomyosin (Ca2+ dependent) and cells are linked by intercalated discs containing gap junctions and desmosomes.
How is cardiac muscle activated?
Acetylcholine. Cardiac myocytes undergo excitation contraction coupling, where ACH binding triggers Na+ intake, causing an action potential. When the depolarization reaches the t-tubule, it activates DHPR’s (aka voltage gated L type Ca2+ channel) which activate ryanodine receptors on the sarcoplasmic reticulum, leading to Ca2+ release and muscle contraction.
How does the muscle cell remove excess Ca2+ after activation? (3 mechanisms)
Ca2+ enters the SR again via SERCA (sarco-endoplasmic reticulum ATPase)
Ca2+ can be removed from the cell by NCX (Na+/Ca2+ exchanger) or plasma membrane Ca2+ ATPase
Myogenic Excitation
Describes heart contraction initiated by muscle cells rather than nerve impulses. Found in vertebrates, molluscs and some other invertebrates.
Neurogenic
Describes heart contraction initiated by neurons, found in the rest of invertebrates. → neurons innervate the whole heart.
Pacemaker cells (myogenic vs neurogenic)
Specialized cardiac cells that generate electrical impulses for heartbeat.
myogenic: specialized muslce cells unable to contract
neurogenic: cardiac ganglion
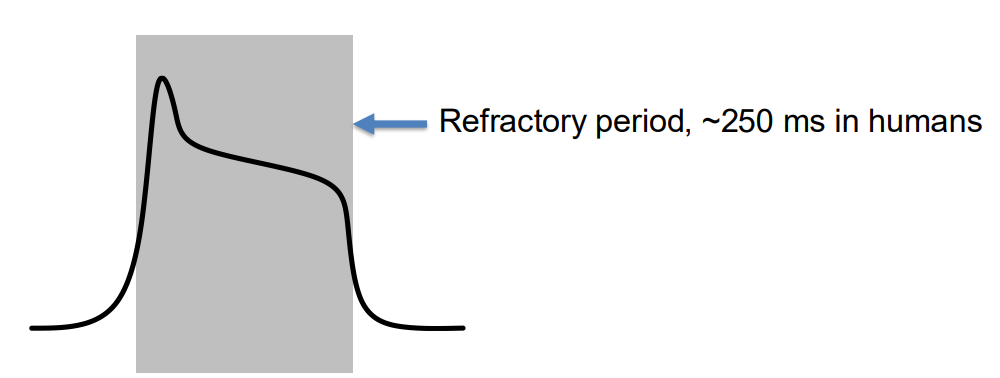
What shape does the cardiac action potential have? Why don’t cardiomyocytes undergo tetanus?
It is much wider than a normal action potential due to a long refractory period.
Cardiomyocytes need to contract and relax to allow the heart to refill with blood and continue pumping, otherwise it would be fatal.
What happens during early ventricular diastole, and how do pressures compare?
Ventricles are relaxed, atria are also relaxed.
Atrial pressure > Ventricular pressure, so AV valves open, allowing passive blood flow into ventricles.
Semilunar valves are closed (arterial pressure > ventricular pressure).
No heart sounds here.
What is the atrial kick, and what pressure changes cause it?
Atria contract, pushing extra blood into the ventricles (the "kick").
Atrial pressure briefly rises above ventricular pressure, aiding in ventricular filling.
Still AV valves open, semilunar valves closed.
No sound, but this boosts end-diastolic volume (EDV).
What causes the "Lub" sound and what happens to pressure here?
Ventricles contract, but all valves are closed initially.
Pressure in ventricles quickly rises above atrial pressure, closing the AV valves → makes the “Lub” (S1) sound.
Since semilunar valves are still closed, it's called isovolumetric (volume doesn’t change yet).
When and why do semilunar valves open?
Ventricular pressure > Arterial pressure, so semilunar valves open.
Blood is ejected into the aorta and pulmonary artery.
AV valves remain closed.
No new heart sounds here.
What causes the “Dub” sound and what are the pressure dynamics?
Ventricles relax, and ventricular pressure drops.
Once arterial pressure > ventricular pressure, semilunar valves close, making the “Dub” (S2) sound.
All valves are closed during this brief phase.
Prepares for the cycle to start again with passive filling.
During atrial fibrillation, the contraction of the atria becomes disorganized. Why do you think this isn’t necessarily fatal (though it is serious)?
The majority of blood actually enters the ventricle from the atrium passively, due to the pressure difference after the atrium is filled. The atrial contraction is needed for the atrial kick, but that only expels the last bid of blood from the atrium.
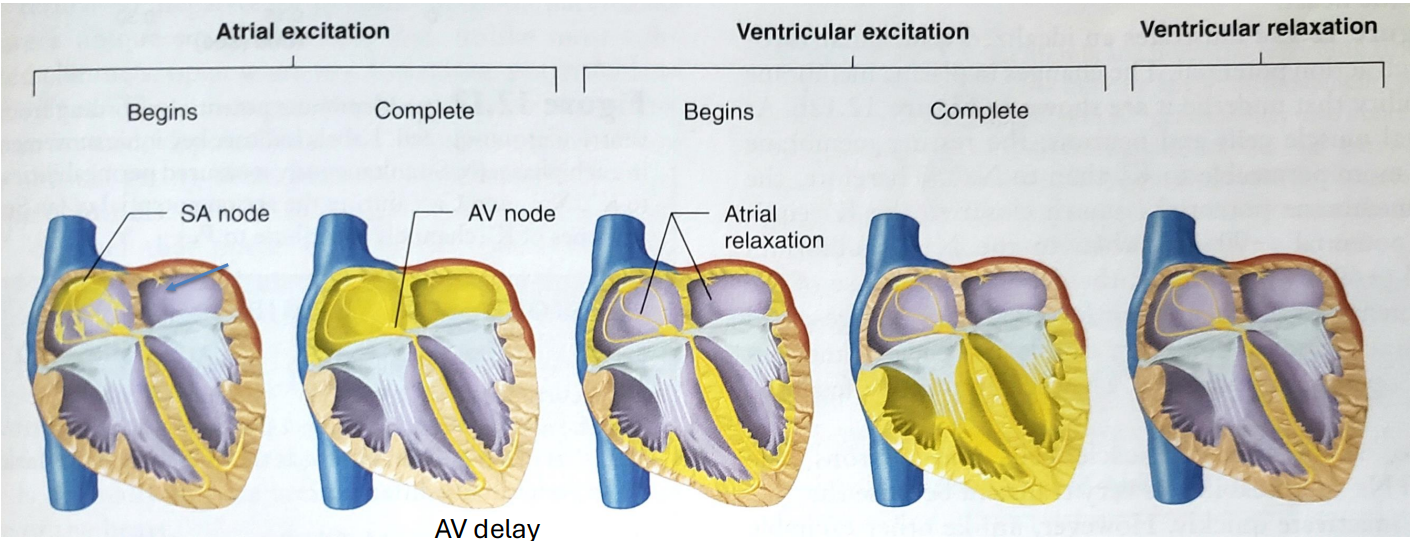
How does the myogenic contraction signal travel through the heart?
During atrial excitation
travels from SA node to AV node through internodal pathways. This moves the signal from the right to the left atrium.
During ventricular excitation
signal travels doen intraventricular septum, then fills whole ventricle. As the ventricle depolarizes, the atriums repolarize starting from the SA node, and by the time the whole ventricle is depolarized, the whole atriums are normal again.

Explain the ECG wave
atrial depolarization/contraction (P wave)
ventricular depolarization/contraction (QRS complex)
ventricular repolarization/recovery (T wave).
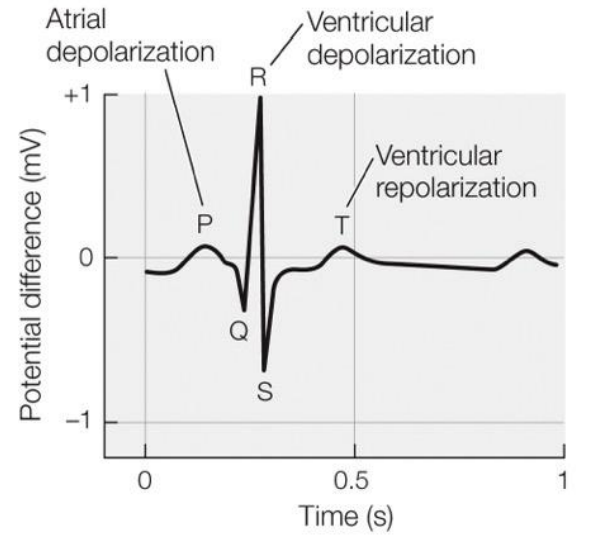
What makes ECG look different than an action potential?
ECG is taken as a recording from the body surface, as a difference between two electrical nodes.
amplitude depends on:
tissue mass
signal’s rate of change
(±) depends on
direction of signal travel
depolarization vs repolarization
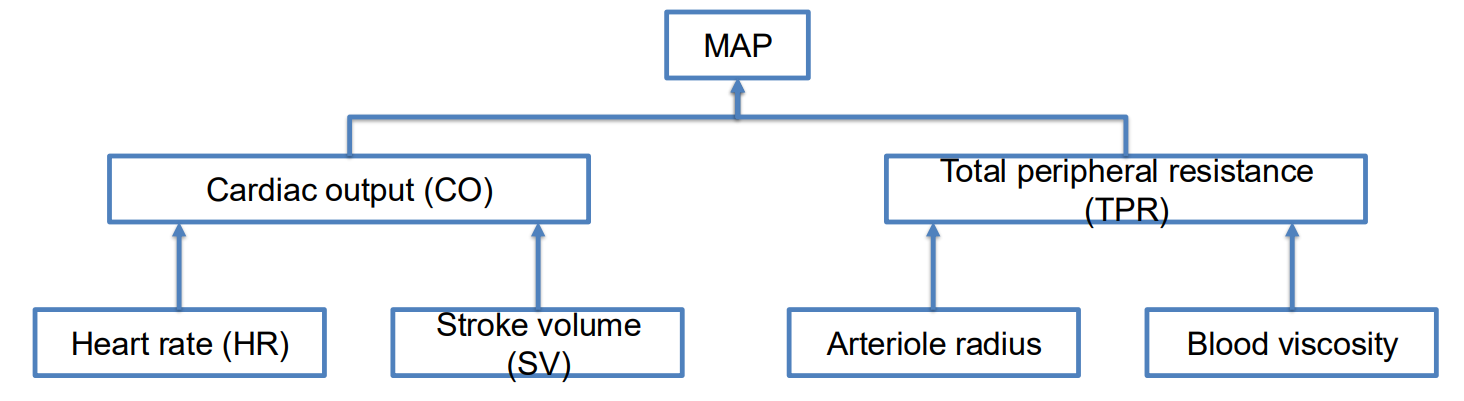
Mean Arterial Pressure (MAP)
is the average pressure in a patient's arteries during one cardiac cycle
Baroreceptors (where are they)
Sensors that detect blood pressure changes and regulate heart rate and vessel dilation.They are primarily located in the walls of the carotid arteries and aorta, sending signals to the central nervous system to maintain homeostasis.
What factors go into controlling MAP?
cardiac resistance
viscosity
arteriole radius
cardiac output
heart rate
stroke volume
Autonomic nervous system (ANS)
The part of the nervous system that controls involuntary bodily functions, including heart rate. Controls parasympathetic and sympathetic mechanisms.
End diastolic volume (EDV)
Volume of blood in the ventricles at the end of diastole, affecting stroke volume.
Stroke volume (SV)
The volume of blood pumped by the heart with each beat.
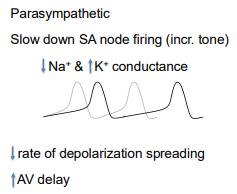
Parasympathetic tone
The influence of the parasympathetic nervous system to slow heart rate.
Paraympathetic Control (neurotransmitter, heart receptor and arteriole receptor)
neurotransmitter: ACh
heart receptor: Muscarinic
ateriole receptor: None
Parasympathetic control function
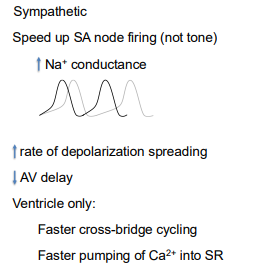
Sympathetic Control (neurotransmitter, heart receptor and arteriole receptor)
neurotransmitter: epinephrine + norepinephrine
heart receptor: beta adrinergic
ateriole receptor: alpha adrinergic
Sympathetic control function
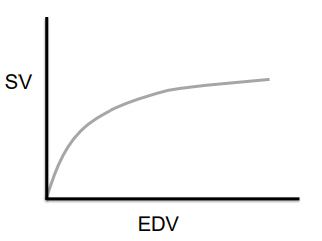
Frank-Starling mechanism
The principle that the stroke volume is directly proportional to the end diastolic volume. (the ascending limb of the force-length curve)
Indicates that cardiomyocyte stretch increases Ca2+ release from SR and increases troponin sensitivity.
How does Sympathetic tone effect the Frank-Starling mechanism? [DIRECT]
Activation of beta-1 receptors activate kinases that phosphorylate:
L type Ca2+ channels
lets in more Ca2+
RyR
lets out more Ca2+ from SR
Troponin
more sensitive to Ca2+
What controls arteriole dilation?
local: low O2, high CO2, low pH, immune signals and temp
hormonal: epinephrine
neuronal: low sympathetic tone
What controls arteriole constriction?
local: temp
hormonal: epinephrine, vasopressin, angiotensin II
neuronal: high sympathetic tone
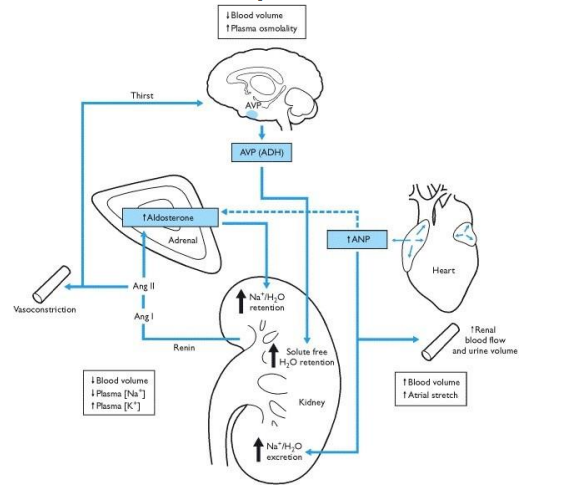
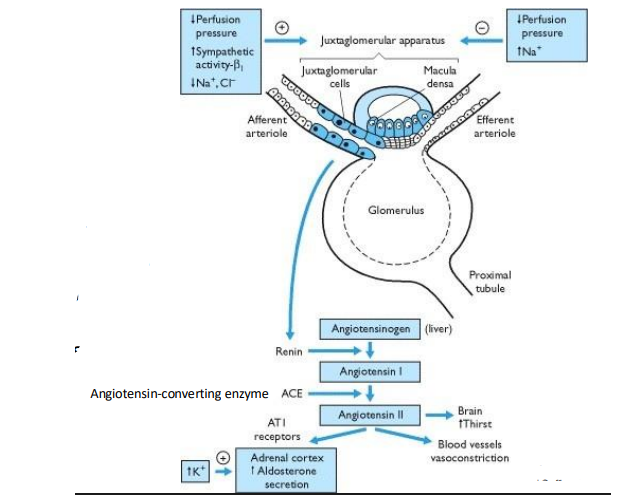
What does Angiotensin do?
Promotes vasoconstriction
Stimulates Aldosterone release
Stimulates ADH release
Increases sympathetic nervoud system activation
stimulates thirst
How is the Angiotensin II made?
Angiotensin II is produced from the conversion of angiotensin I by the enzyme angiotensin-converting enzyme (ACE), primarily in the lungs, in response to decreased blood flow or blood pressure detected by juxtaglomerular cells at the kidney.
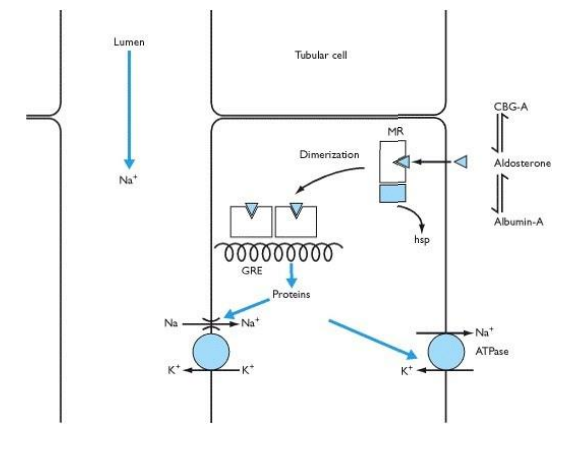
What does aldosterone do?
its a mineralocorticoide/steroid and binds an internal receptor in the kidneys tubular cells. The receptors dimerize, and promote transcription of proteins involved in sodium reabsorption and potassium secretion, leading to increased blood volume and blood pressure.
What is ANP (Atrial Natriuretic Peptide)
Atrial Natriuretic Peptide, a hormone produced by the heart that helps to reduce blood pressure by promoting sodium and water excretion in the kidneys, thus decreasing blood volume.
It also supresses RAAS (renin-angiotensin-aldosterone system) activity and inhibits ADH
Integrated Blood Pressure Control: What 4 hormones involved? Where are they produced?
AVP/ADH - hypothalamus
ANP - heart
Aldosterone - renal cortex
Angiotensin - Kidney
Integrated Blood Pressure Control: Explain how these 4 hormones affect blood pressure.
ADH triggers H2O retention in response to low bp, high plasma mOSM or thirst
ANP increases Na+/H2O secretion and increases Aldosterone secretion, it also increases urine volume an renal blood flow.
Aldosterone increases Na+/H2O retention
Renin is stimulated by low blood pressure or sympathetic nervous system activation, leading to increased angiotensin II formation, which constricts blood vessels and increases blood pressure, also increasing thirst