Ocular pharmacology
1/78
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
79 Terms
Describe the structure of the eye
The eye consists of three complete layers surrounding a central space.
It is covered by 3 membranes. The outermost layer is the sclera.
The choroid is dark and helps attract light to the back of the eyes.
Ciliary muscles are important to attach and change shape of the lens.
The iris is where the colour of the eyes. The retina is in the centres of the choroid. The receptors in the retina allows us to detect light.
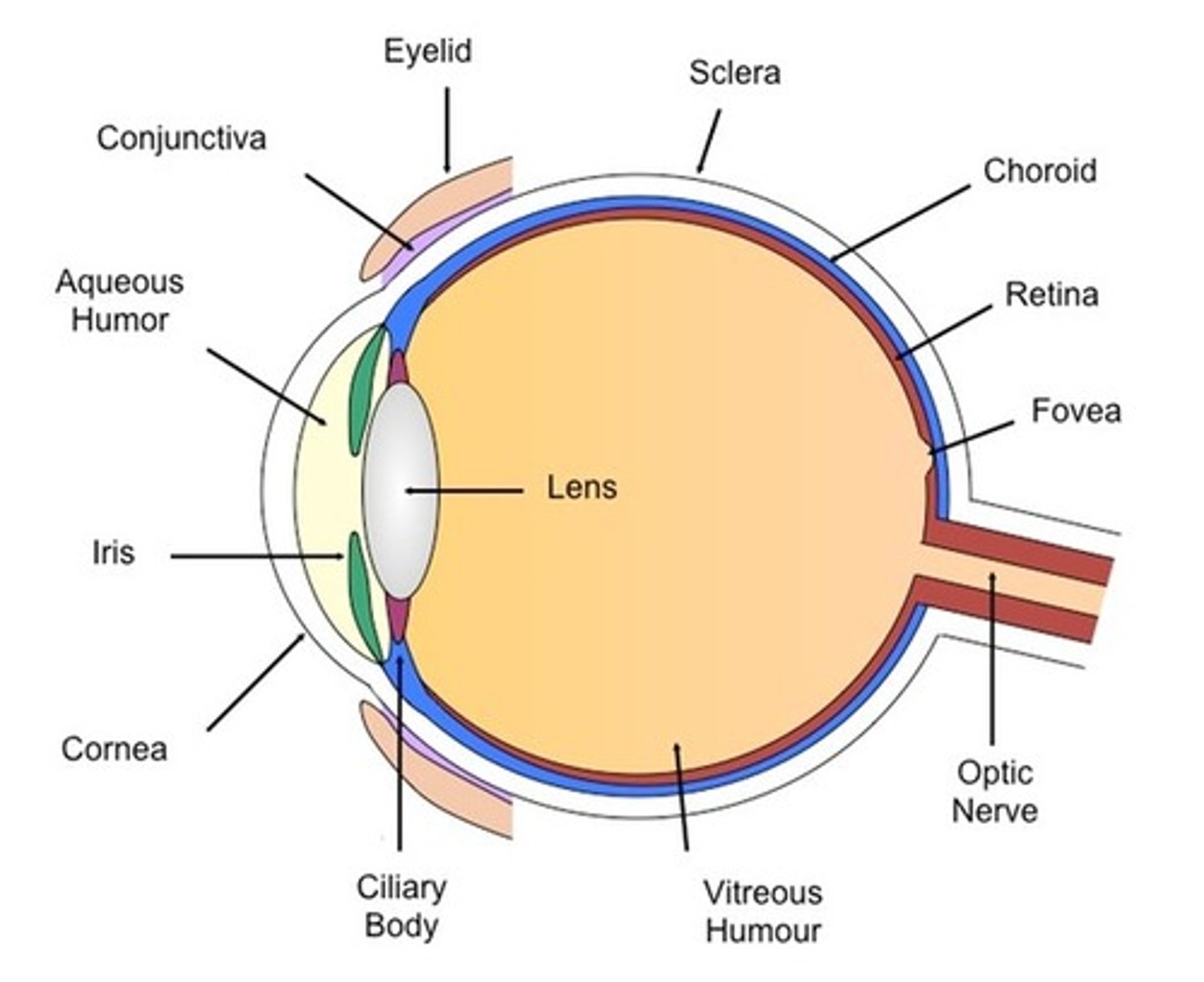
What are the two fluid chambers in the eye?
1. Aqueous humour
2. Vitreous humour
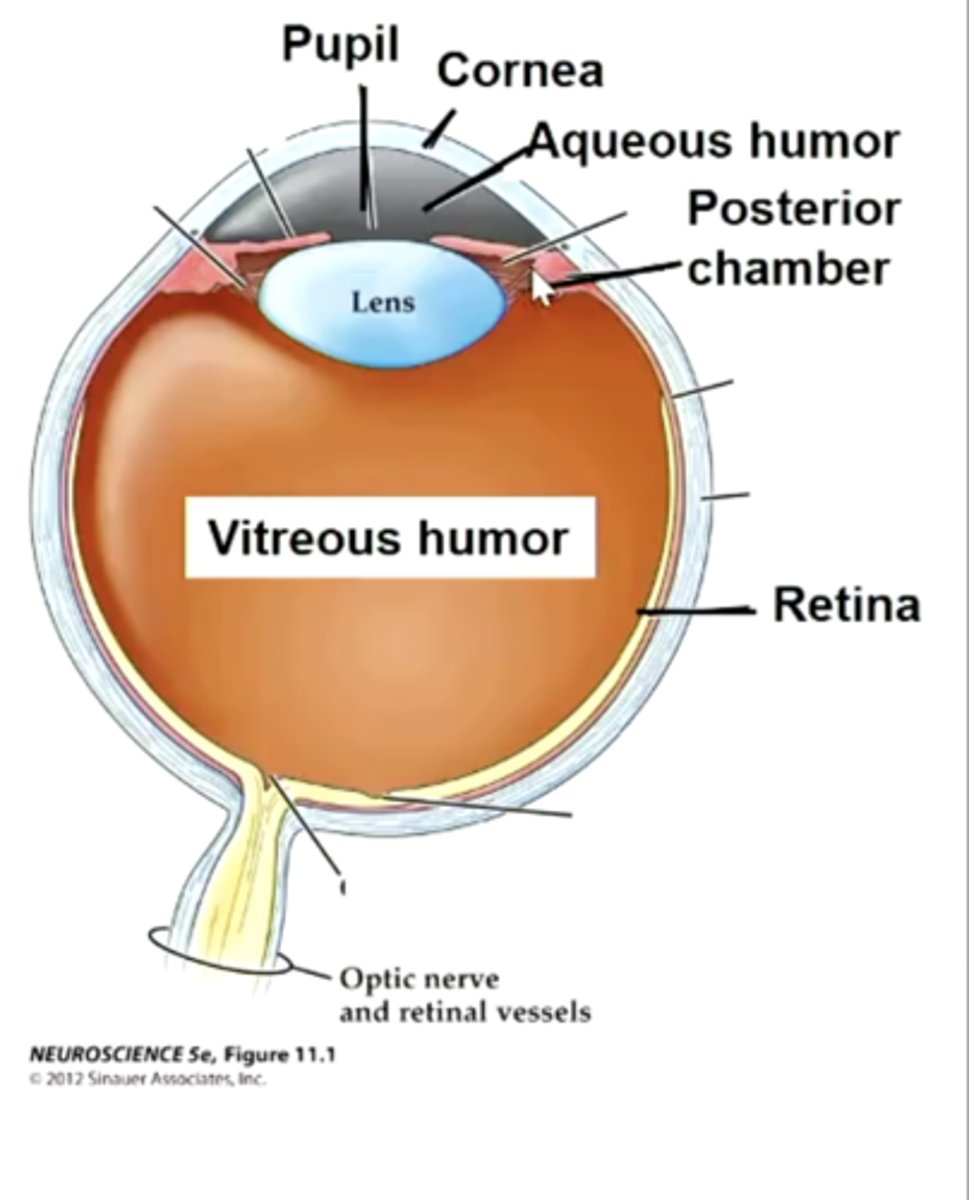
What is the role of the aqueous humour?
To maintain the shape of the front part of the eye and provide oxygen and nutrients to cells of the lens and cornea.
What is the role of the vitreous humour?
It maintains the shape of the rear part of the eye and supports the lens
What are the two smooth muscles in they eye?
1. Iris smooth muscle:
- dilator/ radial
- sphincter/ constrictor
2. Ciliary muscle
What is the role of the iris?
To regulate pupil size & hence the amount of light reaching retina
What is the role of the ciliary muscle?
To change the refractive index of lens accommodation.
This means they:
- Attach the lens
- Change the shape of the lens to see clear imaging.
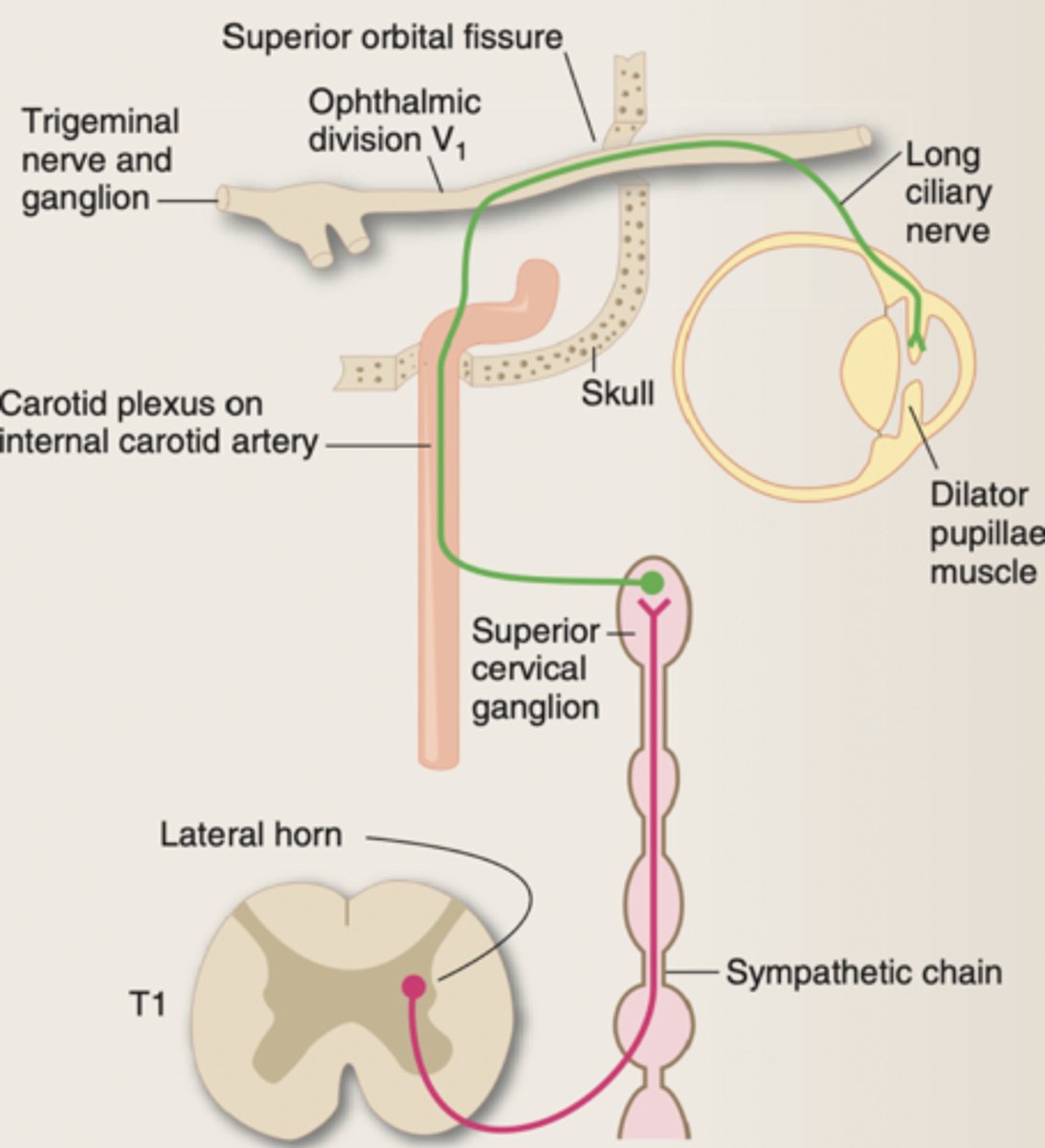
Describe innervation of the eye
It is controlled by the autonomic nervous system (involuntary).
It is innervated by both the sympathetic and parasympathetic NS.
The parasympathetic NS dominates and maintains iris tone.
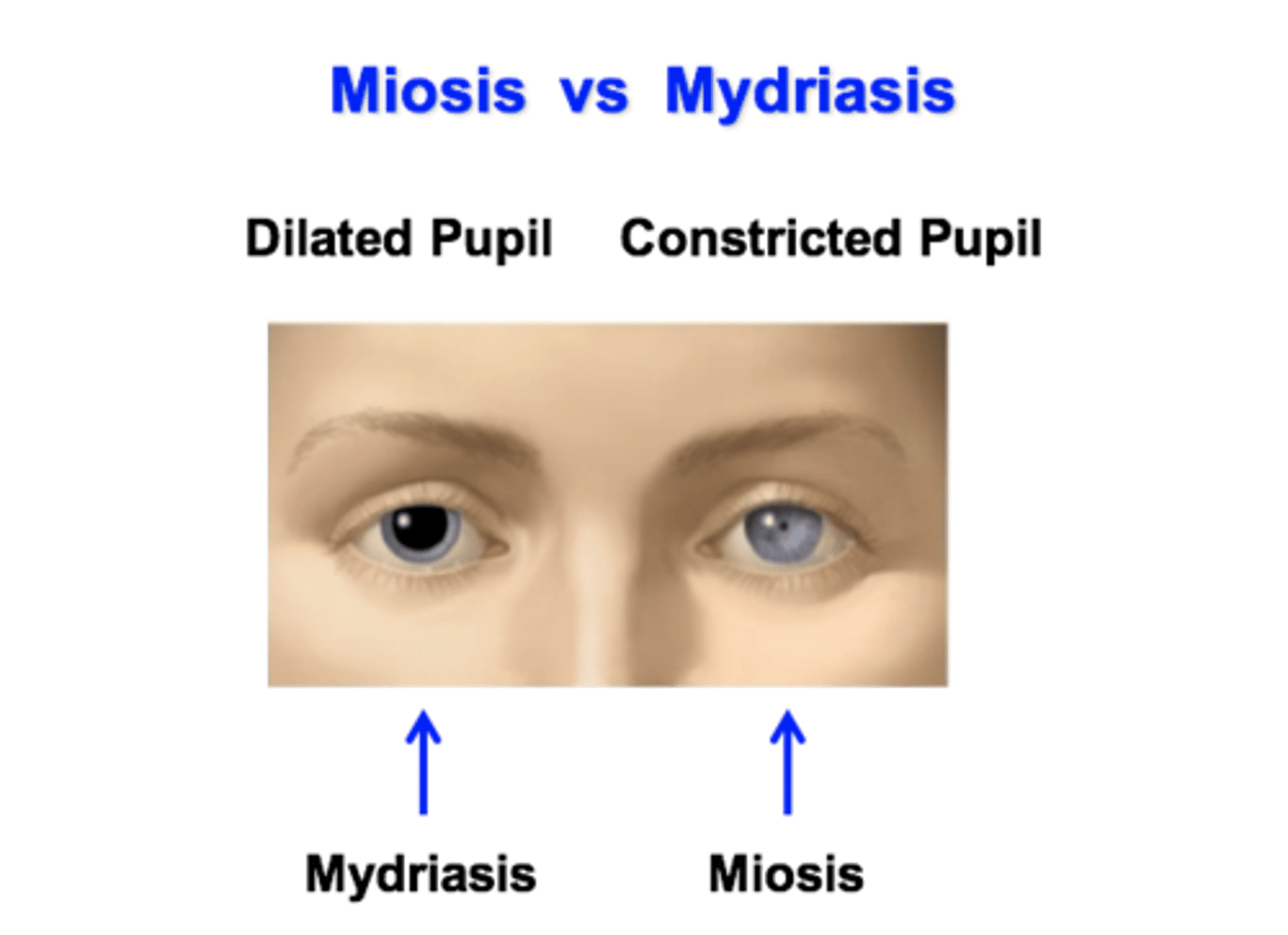
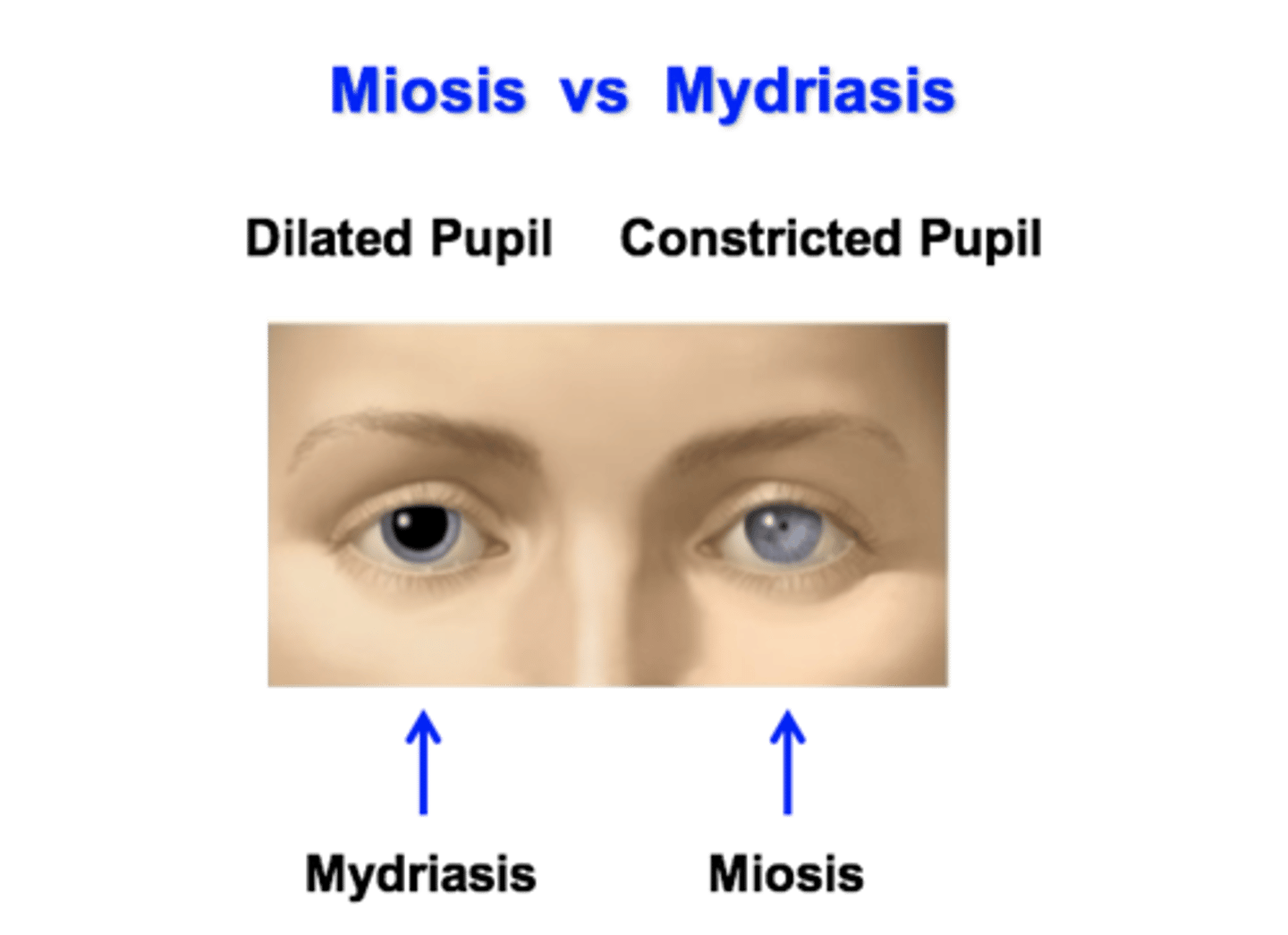
What is mydriasis?
Pupil dilation by contraction of radial/ dilator muscle (iris smooth muscle).
- This is sympathetic innervation of the iris
Where do sympathetic fibres innervating the dilator/ radial muscle come from?
The superior cervical ganglion
Describe neurotransmitter in the sympathetic NS
Acetylcholine is released from the pre-ganglionic fibres and binds to nicotinic receptor.
Noradrenaline is released from post-synaptic fibres and binds to a1 (adrenergic) receptors.
What is the effect of an a1 adrenoreceptor agonist on the pupil?
Mydriasis
- Pupil dilation by contraction of radial/ dilator muscles

What is the effect of an a1 adrenoreceptor antagonist on the pupil?
Miosis
- Pupil contraction by contraction of sphincter/ constrictor smooth muscle (iris muscles)

What is miosis?
Pupil constriction by contraction of sphincteric constrictor smooth muscle
Where do parasympathetic fibres innervating the sphincter/ constrictor muscle come from?
Cranial parasympathetic axons innervate the ciliary ganglion (back of the eye).
Postganglionic fibres innervate the sphincteric constrictor smooth muscle
Describe neurotransmitter in the parasympathetic NS
Acetylcholine is released from the pre-ganglionic fibres and binds to nicotinic receptor.
Acetylcholine is released from post-ganglionic fibres and binds to M3 muscarinic receptors on effector muscles
Describe the mechanism of sympathetic activation in the eye
1. NA binds to a1 adrenergic receptors.
2. Activate PLC.
3. Increases amount of IP3.
4. There is an increase in Ca2+
5. This induces contraction.
(dilator/ radial muscles)
Describe the mechanism of parasympathetic activation in the eye
1. Ach binds M3 receptor
2. Activate PLC
3. Increase IP3
4. There is an increase in Ca2+
5. This induces contraction
(sphincter/ constrictor muscles)
Describe how an increase in Ca2+ leads to muscle contraction
1. Calcium/Calmodulin binds to myosin light chain kinase (MLCK)
2. MLCK uses ATP to phosphorylate myosin cross bridges
3. Phosphorylated cross bridges bind to actin - produce tension.
What is the effect of an M3 muscarinic antagonist on the pupil?
Mydriasis
- Pupil dilation by contraction of radial/ dilator muscles

Describe the pupillary light reflex
In bright light, there is miosis (contraction of sphincter/ constrictor muscles) leading to pupil getting smaller (constricting).
In low light, there is mydriasis (contraction of radial/ dilator muscles) leading to pupil get larger (dilating).
There is consensual pupil response
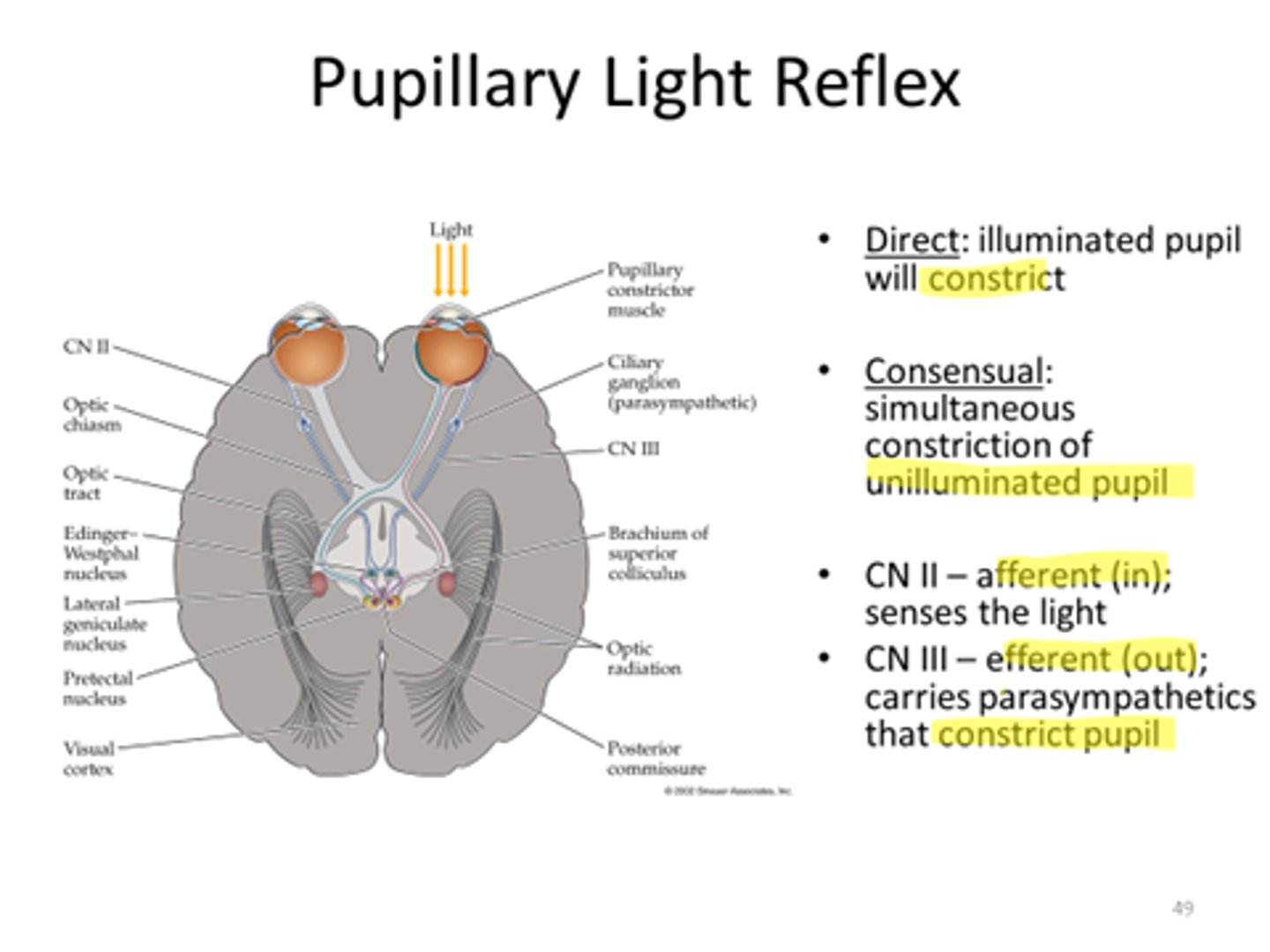
What is consensual pupil response?
When a response in one eye will stimulate same response in the other
For example:
When shining a light in one pupil and it constricts, the opposite pupil should also constrict
Give an example of a muscarinic agonist and antagonist
Muscarinic agonist
- Pilocarpine
Muscarinic antagonist
- Atropine
Describe how the eye focuses on near objects
Ciliary muscles contract
Constrictor/ radial iris muscles contract
Lens becomes more convex (more rounded)
Light is refracted more
Light rays focused onto the retina
Describe how the eye focuses on a distant object.
Ciliary muscles relax.
Constrictor/ radial iris muscles relax
The lens becomes more flat.
Light is refracted less
Light rays focused onto the retina
What do we use muscarinic antagonists for?
1. Ocular examinations
- enlarge pupil to observe back of retina
2. Anterior Uveitis treatment
- inflammation of the eye
2. Lazy eye (amblyopia) treatment
What muscarinic antagonist do we use for ocular examinations?
Tropicamide
What muscarinic antagonist do we use for amblyopia treatment?
Atropine
- We use atropine in the good eye to force the lazy eye to work
When do we not use muscarinic antagonists (contraindication)?
Closed angle glaucoma (impairs drainage of aqueous humour)
What are mydriatics?
Drugs which block constrictor iris smooth muscle
- This leads to pupil dilation
What are cycloplegics?
Drugs which paralyse ciliary muscle
- This prevents lens accommodation
What is a key difference between the muscarinic antagonists?
The duration of action
- We choose a muscarinic antagonist by determining how long we want the effect to be and therefore the recovery time of the patient.
For example, atropine has a long recovery time (so can force patient's lazy eye to work).
Whereas tropicamide has a short duration of action (want patient recovery time to be quick).
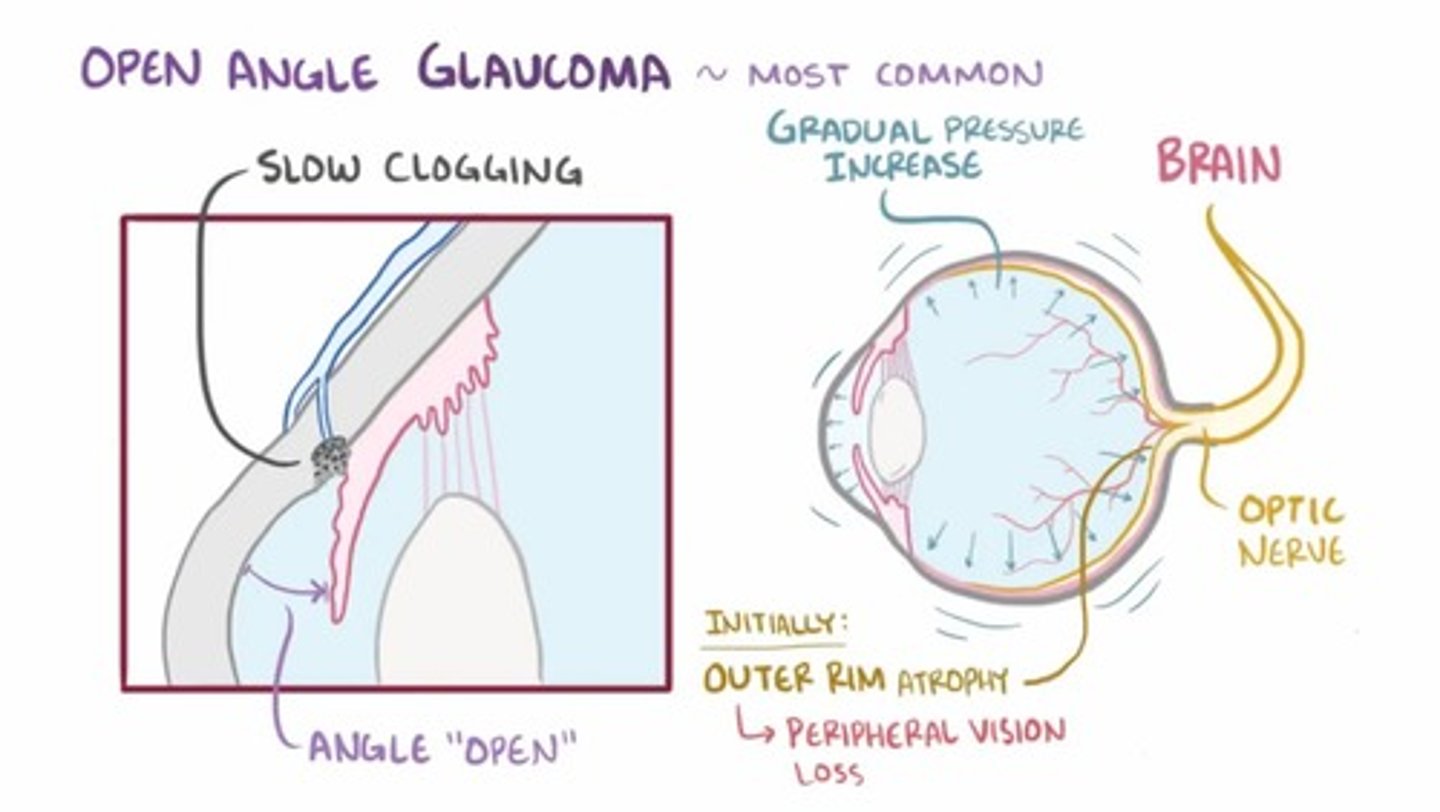
What is glaucoma?
A group of eye conditions that damage the optic nerve.
It is characterised by high intraocular pressure.
It can happen in one eye or both eyes.
What are the different classes of glaucoma?
1. Primary
2. Secondary
3. Developmental
What are risk factors for glaucoma?
1. Older age - open angle glaucoma more common
2. High blood pressure
- increases intraocular pressure
3. Afro-Caribbean origin - increased risk of open angle glaucoma
4. East Asian origin have greater risk of closed angle glaucoma
5. Family history of glaucoma
6. Diabetes
What is the effect of glaucoma in patients vision?
In glaucoma, you start to lose peripheral vision.
Compare normal intra-ocular pressure to intra-ocular pressure in patients with glaucoma
Normal: 12-20 mmHg
Glaucoma: intra-ocular pressure > 21 mmHg
But, people can have glaucoma without a high intra-ocular pressure.
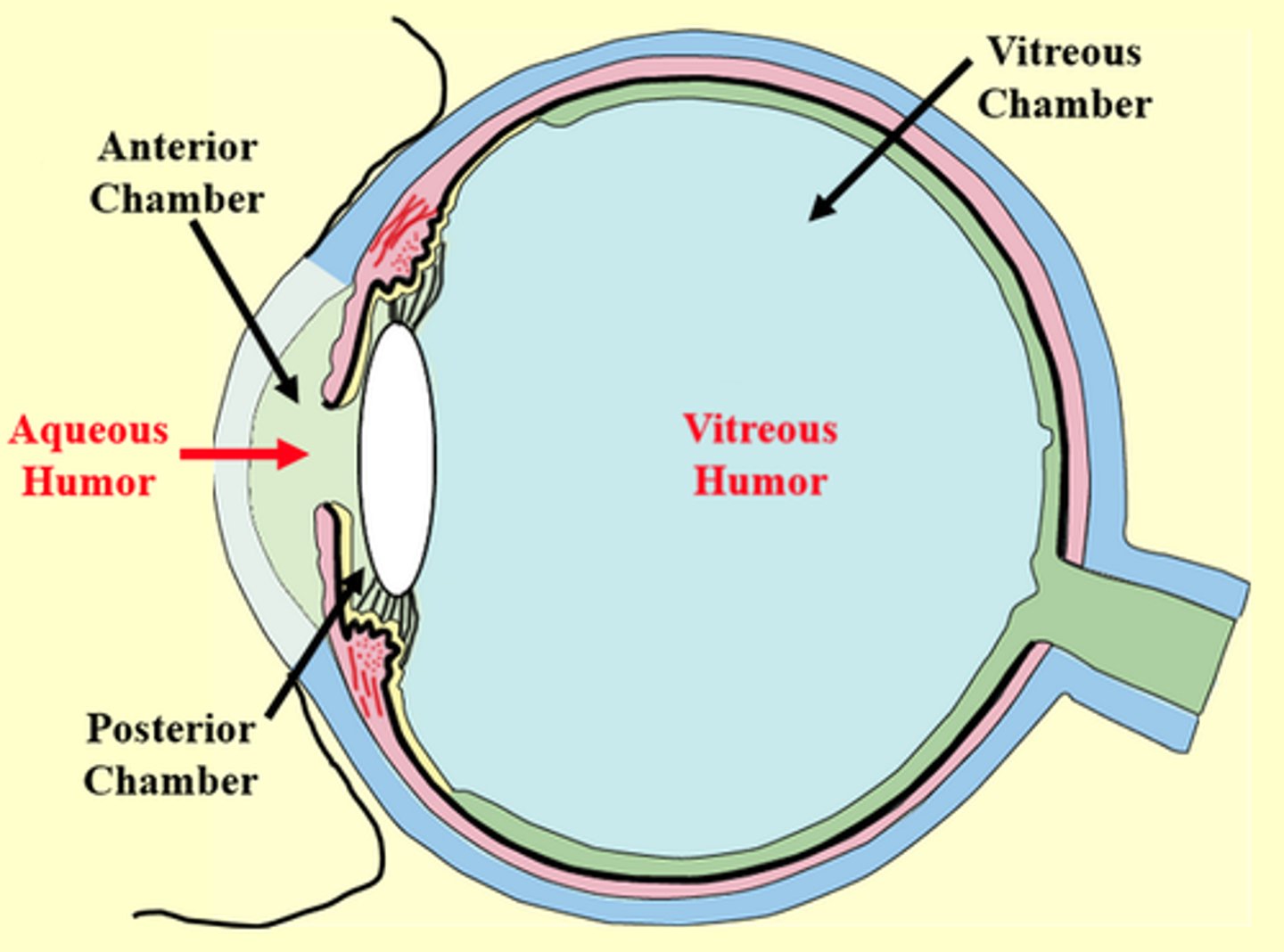
What determines the intra-ocular pressure?
The rate of formation and rate of drainage of Aqueous Humour (AH).
- AH is produced continuously by ciliary body epithelium
- It is released into posterior chamber
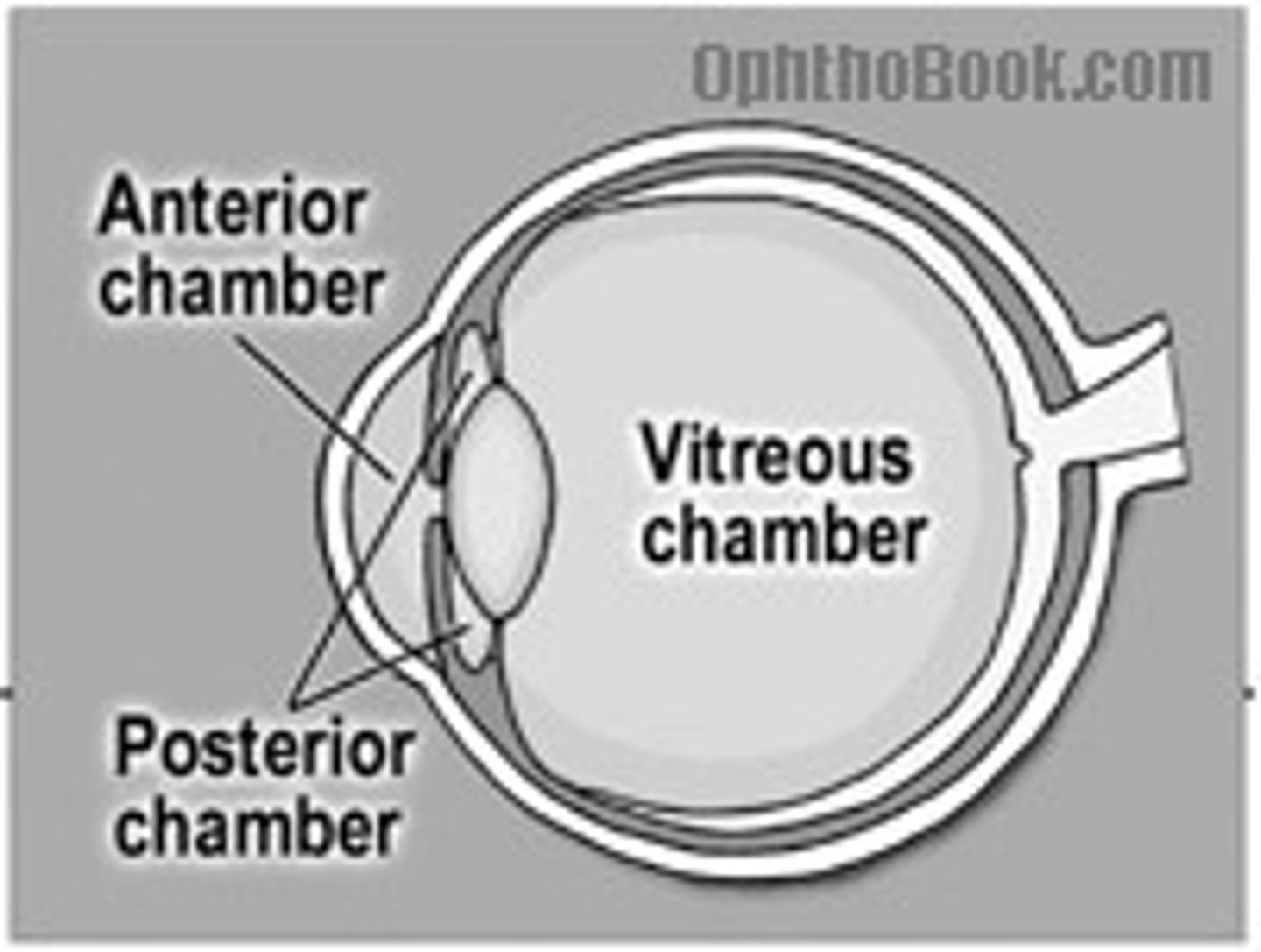
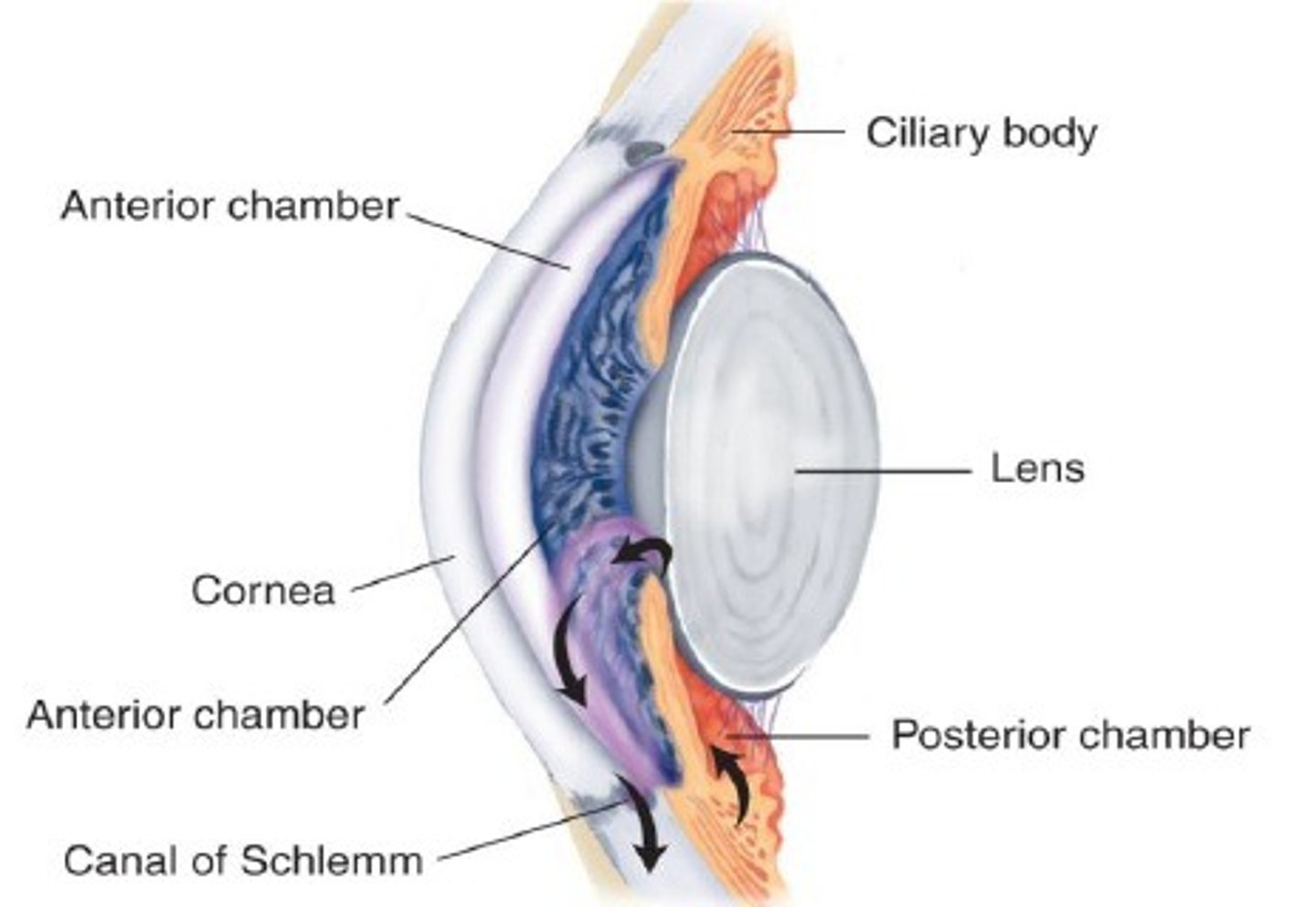
Describe circulation of the aqueous humour (AH)
1. AH is produced by ciliary body
2. AH flows from the posterior chamber through the iris into the anterior chamber
3. Then AH is drained mostly into the trabecular meshwork(90%)
(Canal of Schlemm & into vein) but some does drain into uveoscleral outflow (10%).
What is the aqueous humour composed of?
1. Bicarbonate
2. Lactate (high) - anaerobic glycolysis
3. Ascorbate (high) - protects a against UV radiation (can form radicals)
Other:
4. Glucose
5. Albumin
6. K+, Cl-, Ca2+
7. IgG
Nearly completely protein-free
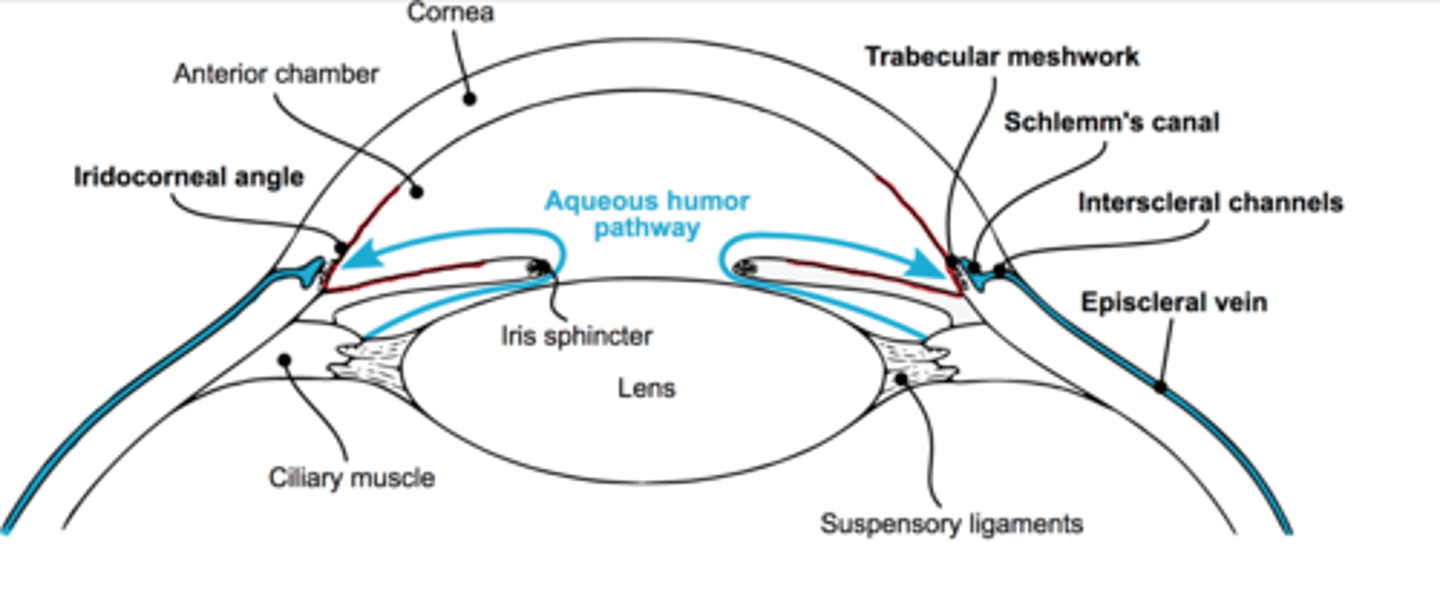
What is open angle glaucoma?
When trabecular meshwork and canal of Schlemm becomes blocked (so no drainage of AH), therefore there is a build up of aqueous humour (AH) leading to a rise in intra-ocular pressure.
- this is the most common cause of glaucoma
What receptors control aqueous humour formation (AH)?
AH formation is:
- Stimulated by beta agonists
- Inhibited by alpha agonists
What are different treatment options for open angle glaucoma?
1. Eye drops
2. Laser
3. Trabeculectomy (surgery)
4. Aqueous shunt implantation
What are the different eye drop treatment options for open angle glaucoma?
Decrease aqueous humour (AH) formation:
1. a1 adrenoreceptor agonists
2. a2 adrenoreceptor agonists
3. beta adrenoreceptor antagonists
4. Carbonic anhydrase inhibitor
5. Cholinergic inhibitors
6. Prostaglandin analogues.
What is closed angle glaucoma?
When drainage angle formed by iris and cornea closes or becomes obstructed.
This is a medical emergency.
All we can do is try to remove all the water from the AH to reduce the formation.
This blocks flow of aqueous humour from posterior to anterior chamber.
The onset can be sudden and result in rapid irreversible damage.
How could we treat open-angle glaucoma using a2 adrenoreceptor agonists?
If we use an a2 agonist, it decreases cAMP so decreases AH formation directly.
It also indirectly inhibits AH production in eyes by decreasing noradrenaline release from sympathetic fibres which decreases beta-adrenergic stimulation.
Describe how beta-adrenoreceptor antagonists work in treating open-angle glaucoma
Beta-adrenoreceptor antagonists decrease AH formation by preventing adrenaline from binding to beta-receptors on the ciliary body.
AH formation is cAMP-dependent, therefore it reduces amount of cAMP.
The sympathetic nerves on the ciliary body - NA (where cAMP is made).
Give an example of a beta-adrenoreceptor antagonist
Timolol
When do we not use beta-adrenoreceptor antagonists (contraindication)?
Asthma
Heart block
Bradycardia
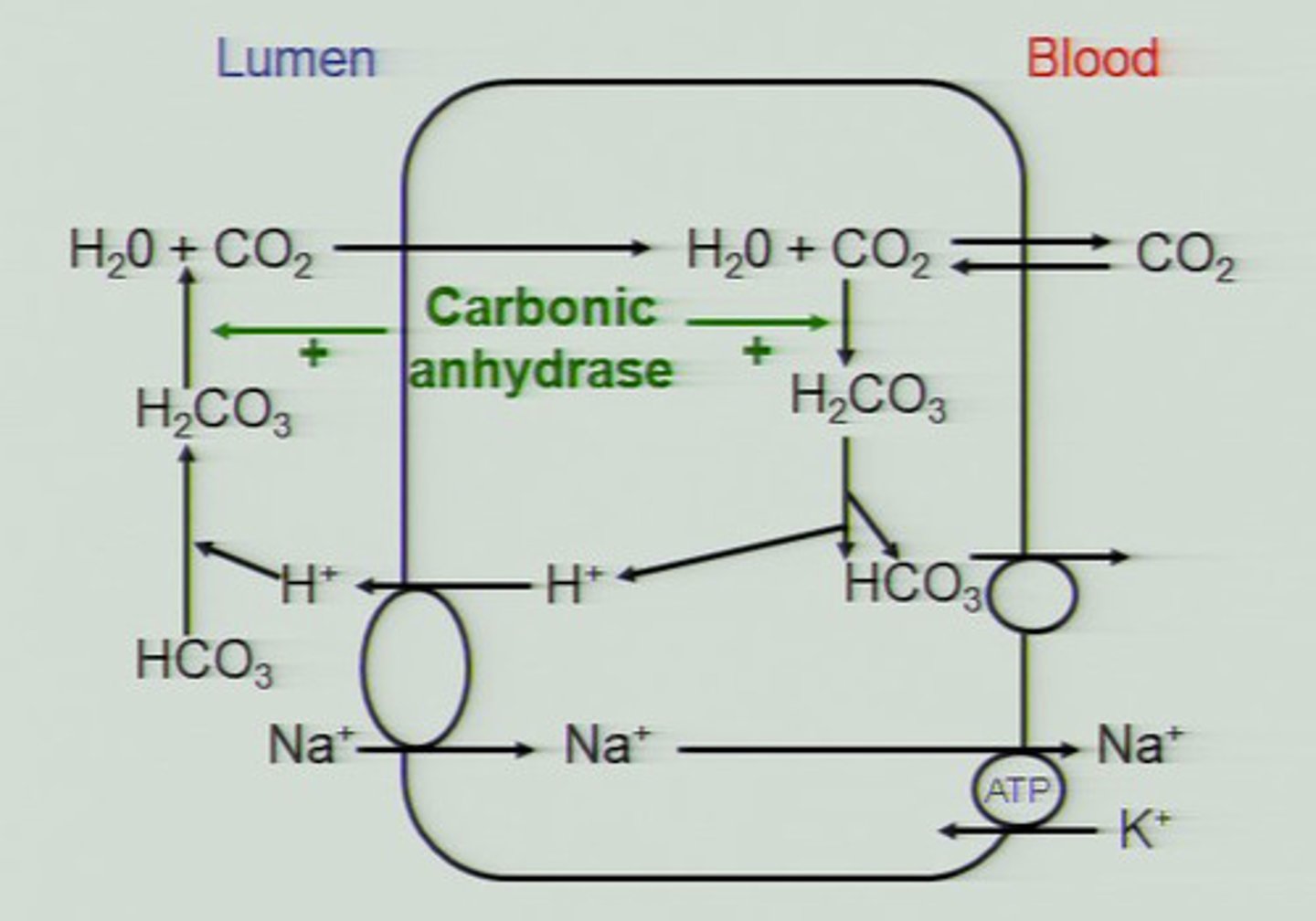
How could we treat open-angle glaucoma using carbonic anhydrase inhibitors?
To produce AH we need bicarbonate to be actively transported out of the ciliary body. Therefore, these inhibitors reduce AH by reducing intracellular carbonate.
How could we treat open-angle glaucoma using cholinergic inhibitors?
Direct-acting cholinergic agonist that causes miosis (pupil gets smaller) and contraction of the ciliary
muscle
Give an example of cholinergic inhibitors
Muscarinic agonist:
- Pilocarpine
(Carbachol)
Give an example of a carbonic anhydrase inhibitor
Brinzolamide.
- has long half-life
How could we treat open-angle glaucoma using prostaglandin analogues?
There is improved drainage through uveoscleral outflow
Give an example of a prostaglandin analogue used to treat open-angle glaucoma
How does it work?
Latanoprost PGF2a analogue.
Latanoprost lowers the pressure in your eye by reducing the build-up of fluids
How could we treat open-angle glaucoma using laser?
Laser treatment is used in glaucoma to decrease the amount of fluid (aqueous humour) in the eye
How could we treat open-angle glaucoma using trabeculectomy surgery?
A trabeculectomy is an eye operation that improves drainage of fluid out of the eye.
How could we treat open-angle glaucoma using aqueous shunt implantation?
An aqueous shunt is a device which drains aqueous humour out of the eye to a small blister
Give an example of an a2 adrenoreceptor agonist
Brimonidine
(also: clonidine, apraclonidine)
What is dipivefrin?
A pro-drug of adrenaline.
It decreases aqueous humour (AH) production.
It is a lipophilic molecule so it is absorbed well.
How does dipivefrin work?
It reduces intraocular pressure by:
- increasing the drainage of aqueous humour
- decreasing AH production.
This is because adrenaline stimulates alpha adrenergic receptors
BUT: drawback is that it stimulates beta receptors too.
How does dipivefrin keep its effect localised?
Dipivefrin is a lipophilic molecule so it is absorbed across the cell membrane.
When it is metabolised by monoamine oxidase to adrenaline, it is poorly absorbed across the cell membrane.
What combination therapies can be used for open-glaucoma treatment?
1. Beta-adrenergic receptor blocker + carbonic anhydrase inhibitor
- timolol + brinzolamide
2. Beta-adrenergic receptor blocker + alpha-adrenergic receptor agonist
- timolol + brimonidine
3. Beta-adrenergic receptor blockers + prostaglandins
- timolol and PGF2alpha analogues
How could we treat open-angle glaucoma using a1 adrenoreceptor agonists?
If we use an a1 agonist, it causes vasoconstriction.
This decreases flow of blood around ciliary bodies and reduces AH formation
How do we treat closed-angle glaucoma?
Patient must be in hospital to treat.
We can use urea and mannitol IV.
The also treat with glycerine and isosorbide orally.
We increase blood osmolarity/
We used these to decrease intra-ocular pressure by reducing volume of water in the vitreous humour (VH).
What other treatments can be used for closed-angle glaucoma when pharmacology is not enough?
1. Laser trabeculoplasty
2. Surgical scleral flap
3. Laser iridectomy
What is the macula?
The macula is an oval-shaped pigmented region of the retina essential for 'sharp' vision
It has a high density of cones (photoreceptors)
What is age-related macular degeneration?
A severe and irreversible loss of central vision due to the destruction of the macula (black spots appear in the centre of your vision).
There is no effective treatment.
What are signs of macular degeneration?
- Blurry spots in centre of vision
- Blank or dark spots in centre of vision
- Difficulty reading
- Loss of clear colour vision
- Objects appear distorted
- Straight lines that appear crooked or wavy
What are the different types of age-related macular degeneration (AMD)?
1. Dry
- more common
- slow onset
- no successful treatment
2. Wet
- rapid onset
Describe wetage-related macular degeneration (AMD)
There is abnormal/ excessive growth of leaky blood vessels under the retina.
Blood vessel growth & leakiness is stimulated by vascular endothelial cell growth factor (VEGF)
What treatment is available for treatment of wet age-related macular degeneration (AMD)?
1. Anti-VEGF antibodies or VEGF receptor
2.VEGF binding molecules
3. Verteporfin IV followed by laser photoactivation (red laser) - photodynamic therapy
How does verteporfin work?
In the presence of light, verteporfin produces reactive oxygen species in the region of the macular damage and stops the flow of blood vessels in area.
How does anti-VEGF work?
We need VEGF for blood vessel growth.
Inhibiting it stops blood vessel growth.
Give an example of a VEGF binding molecule
Pegaptanib
How do we treat allergy?
Allergies are associated with IgE-medicated mast cell degranulation. This can lead to itch and reddening. Hence we use:
1. Histamine receptor antagonists
2. Mast cell stabilisers
3. Glucocorticoids
Give an example of a mast cell stabiliser
Sodium cromoglycate
(type of cromone)
What could cause dry eyes?
Dry eye is a clinical condition associated with decreased eye secretions.
This can occur following:
- radiotherapy
- Sjögren's syndrome
- Keratoconjunctivitis
What can we use to treat dry eyes?
1. Pilocarpine
- increases tears via muscarinic activation
2. Glucocorticoids/ immunosuppressives
3. Lifitegrast (integrin aLb2 antagonist)