Topic 12: UMN & LMN Lesions: Facial Weakness, Stroke, and Spinal Cord Disorders
1/99
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
100 Terms
What are the characteristics of LMN facial weakness?
Ipsilateral weakness of both upper and lower facial muscles (the entire half of the face appearing weak or drooping.)
What is the clinical presentation of a patient with LMN facial weakness?
Inability to raise the eyebrow, close the eye, or smile on the affected side.
What is a common causes of LMN facial weakness?
Bell's Palsy, which is acute LMN facial paralysis possibly due to viral inflammation of Facial Nerve CN VII (often herpes simplex).
What additional signs may accompany LMN facial weakness?
Hyperacusis, loss of taste in the anterior 2/3 of the tongue, and decreased lacrimation/salivation, depending on lesion location.
What is the presentation of UMN facial weakness?
Contralateral weakness of the lower facial muscles only, with forehead muscles spared due to bilateral innervation.
Why is the forehead spared in UMN facial weakness?
The upper face motor neurons receive bilateral corticobulbar input, while lower face motor neurons receive only contralateral input.
Where is the lesion located in UMN facial weakness?
In the corticobulbar tract, often in the cerebral cortex, internal capsule, or brainstem (above the facial nucleus).
What are the signs of UMN facial weakness?
Patients can raise eyebrows symmetrically and close both eyes, but may have a flattened nasolabial fold and drooping of the mouth corner on the contralateral side.
What is a common cause of UMN facial weakness?
Stroke, specifically due to an infarct of the Middle Cerebral Artery (MCA).
Where are UMN cell bodies located?
In the primary motor cortex (precentral gyrus) and in brainstem motor nuclei giving rise to descending tracts.
What is the difference in facial muscle weakness between UMN and LMN lesions?
LMN lesions cause weakness in the entire ipsilateral face, while UMN lesions cause weakness in the contralateral lower face only, sparing the forehead.
What is Bell's Palsy?
An acute LMN facial paralysis, possibly due to viral inflammation of CN VII Facial Nerve, often caused by herpes simplex virus.
What is the significance of the stylomastoid foramen in LMN lesions?
It is the exit point for the facial nerve (CN VII) after it passes through the facial canal in the temporal bone.
Does the facial motor nucleus contain UMN or LMN fibers?
It contains LMN motor fibers that, when lesioned, result in ipsilateral weakness of facial muscles.
What are the potential effects of a lesion in the facial nerve?
It can lead to symptoms such as facial drooping, loss of taste, and decreased salivation.
What are the main structures through which UMN axons descend?
Subcortical white matter, internal capsule, brainstem, spinal cord.
What are the typical causes of UMN lesions?
Cerebrovascular accidents (CVAs), also known as strokes.
What are the two main Stroke categories?
1. Ischemic Stroke (e.g., thrombotic/embolic stroke), 2. Hemorrhagic Stroke
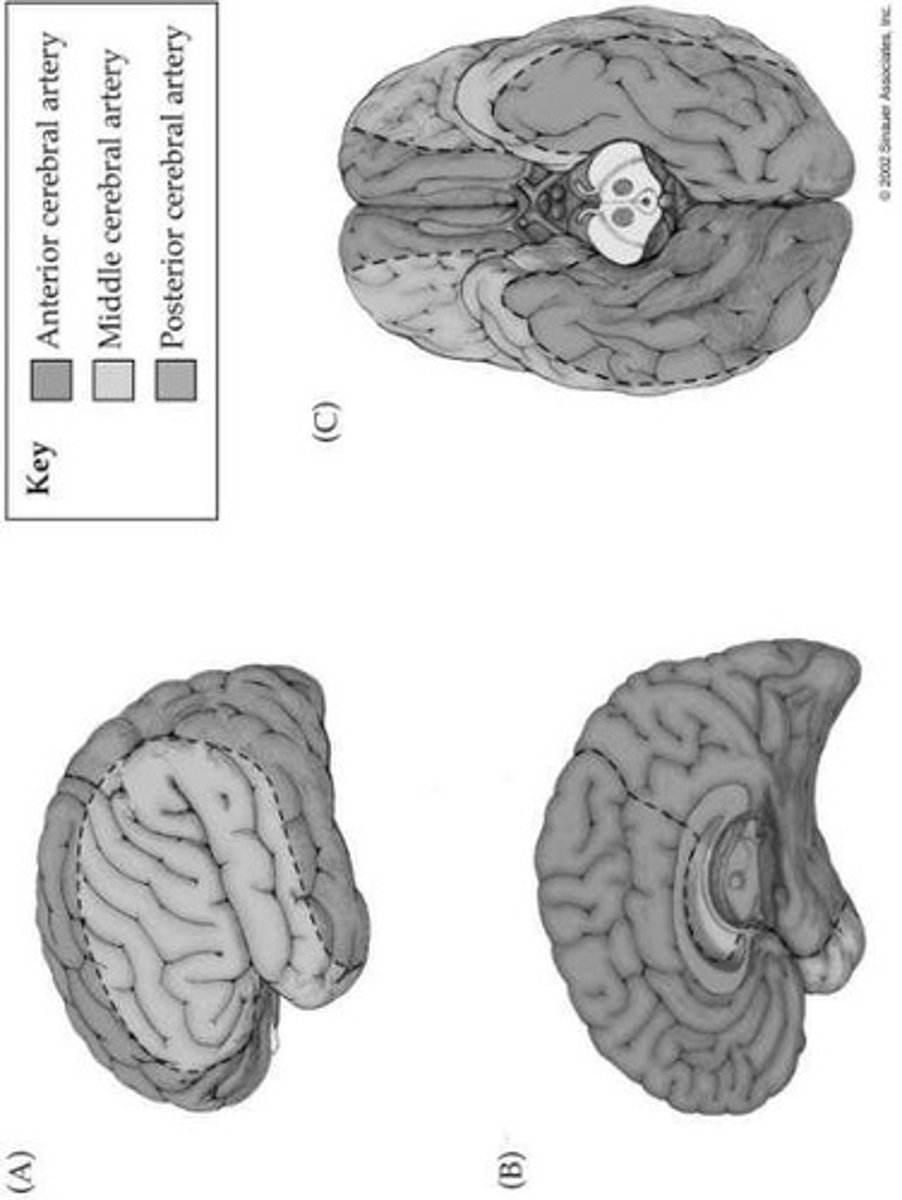
Which arteries supply the motor cortex?
The anterior cerebral artery (ACA) and the middle cerebral artery (MCA).
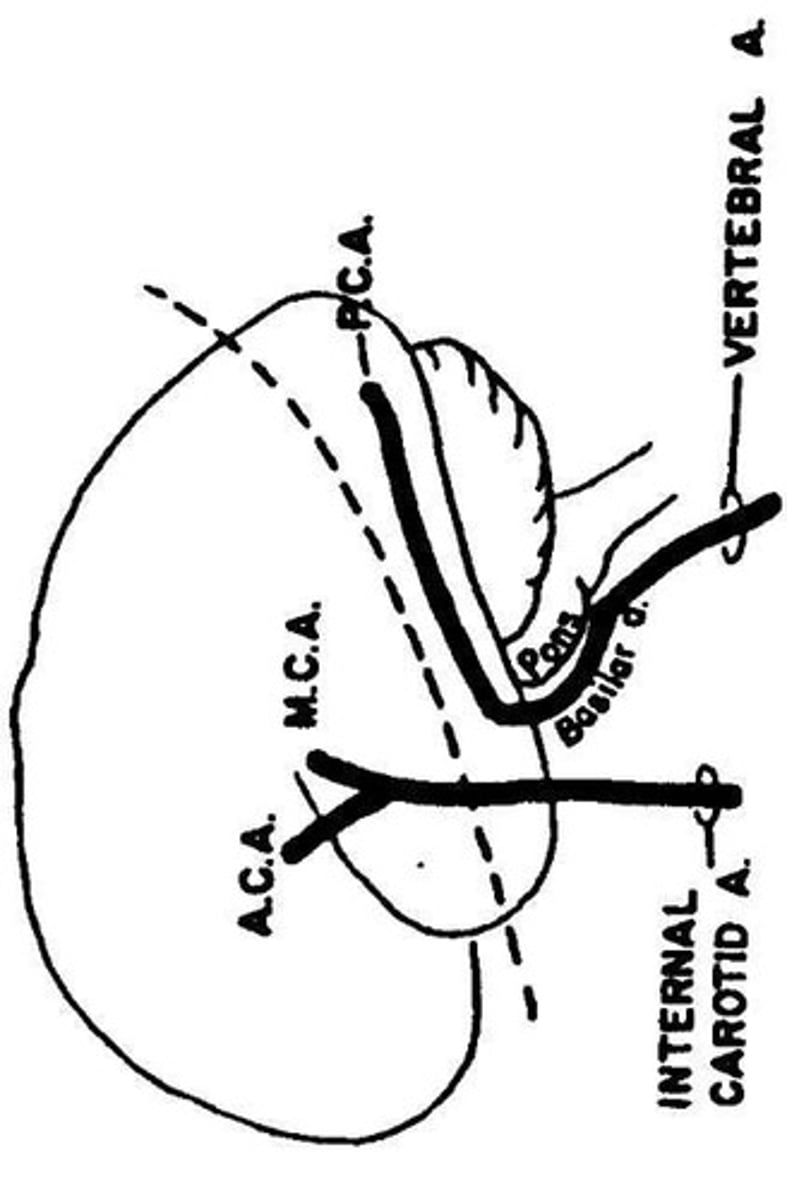
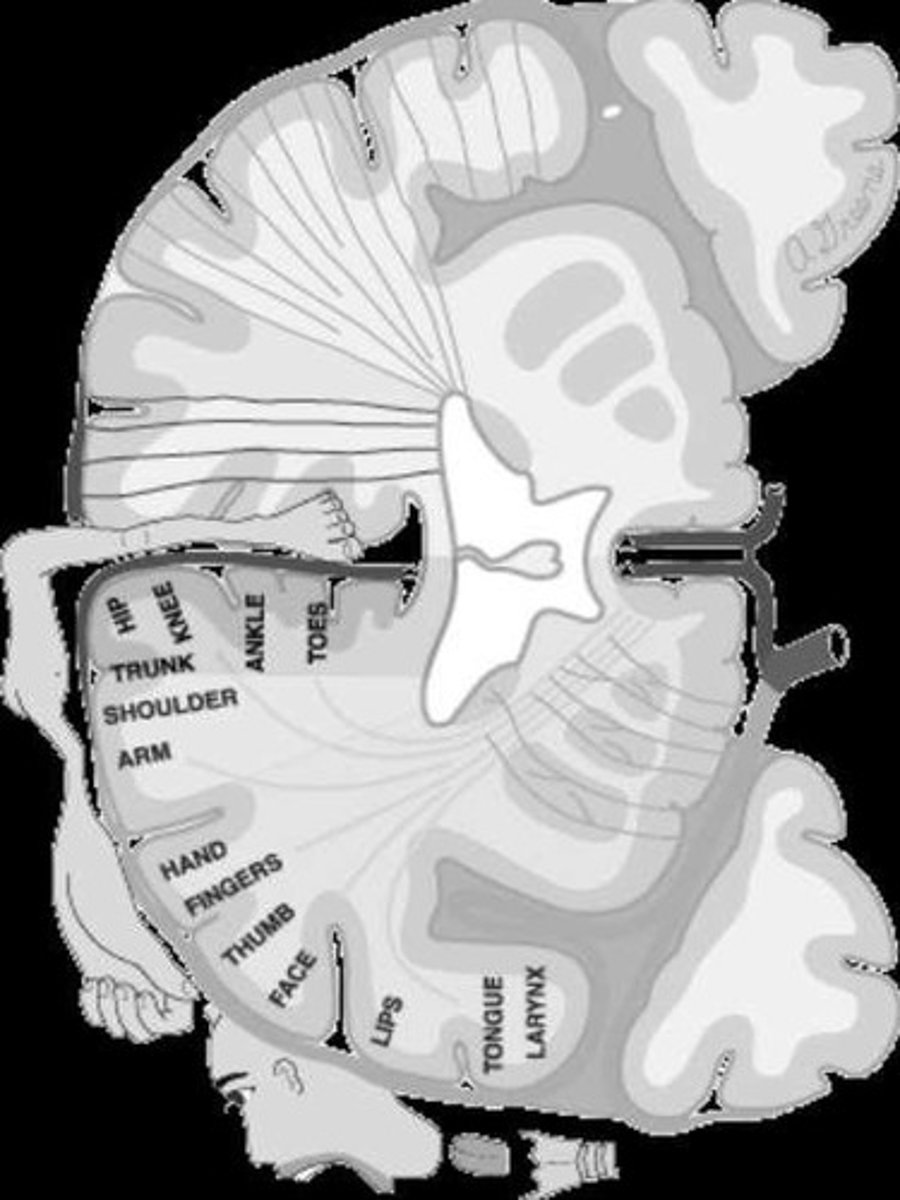
What area does the anterior cerebral artery (ACA) supply?
The medial and superior surface of the motor cortex, corresponding to the lower extremity motor control.
What is the result of an UMN lesion in the ACA territory?
Contralateral leg weakness or paralysis with UMN signs like spasticity and hyperreflexia.
What area does the middle cerebral artery (MCA) supply?
The lateral and inferior surface of the motor cortex, corresponding to the face and upper extremity motor control.
What is the result of an UMN lesion in the MCA territory?
Contralateral face and arm weakness or paralysis with UMN signs like spasticity and hyperreflexia.
What is the somatotopic organization of the motor cortex?
Medial = Lower limb (ACA territory); Lateral = Upper limb and face (MCA territory).
What gait implications arise from an ACA stroke?
Circumduction gait due to dorsiflexor weakness and plantarflexor/knee extensor spasticity.
What is the internal capsule?
A compact bundle of UMN white matter fibers in the subcortical brain, passing between the thalamus and the lentiform nucleus.
What does the posterior limb of the internal capsule contain?
Descending corticospinal and corticobulbar fibers, which are major motor tracts.

Why is the internal capsule considered vulnerable?
Almost all UMN motor axons funnel through it.
What is the primary effect of a lesion in the internal capsule?
It affects all upper motor neuron (UMN) fibers from the cortex on one side, resulting in contralateral hemiplegia or hemiparesis.
What areas of the body are affected by contralateral hemiplegia due to internal capsule stroke?
The contralateral half of the body (including face, arm, and leg). The contralateral forehead is spared.
Why is the forehead spared in an internal capsule stroke?
Because of bilateral innervation to the forehead from the corticobulbar tracts.
What are some additional findings associated with a stroke in the internal capsule?
Contralateral UMN signs such as spasticity, hyperreflexia, pathological reflexes (e.g., Babinski), clonus, and minimal atrophy.
What is a classic example of a stroke in the internal capsule?
A 'pure motor stroke' from a lacunar infarct.
What arteries supply the internal capsule?
The lenticulostriate arteries, which are small, deep branches of the middle cerebral artery (MCA).
What condition makes the internal capsule vulnerable to strokes?
Hypertensive small vessel disease, leading to lacunar strokes.
What is a key point regarding the size of infarcts in the internal capsule?
Even a small infarct can produce profound motor deficits.
What is the vertebrobasilar (VB) system?
It is the combined arterial supply to the posterior part of the brain, arising from the two vertebral arteries that form the basilar artery.
What areas does the vertebrobasilar system supply?
The brainstem, cerebellum, and posterior parts of the cerebral hemispheres, including the occipital lobes.
What are the main branches of the vertebral artery?
Lateral and paramedian branches, anterior spinal artery, and posterior inferior cerebellar artery (PICA).
What does the basilar artery supply?
It supplies the pons, midbrain, and cerebellum.
What are the main branches of the basilar artery?
Anterior inferior cerebellar artery (AICA), superior cerebellar artery (SCA), circumferential branches, and paramedian branches.
What clinical syndromes can result from vertebrobasilar system strokes?
Lateral medullary syndrome and 'locked-in' syndrome.
What is the role of the anterior spinal artery?
It supplies the anterior 2/3 of the spinal cord, including the regions transmitting motor control and pain/temperature information.
What are the symptoms of anterior spinal artery syndrome?
Bilateral upper motor neuron weakness below the lesion, bilateral loss of pain/temperature sensation below the lesion, & preserved dorsal column function (light touch, vibration, proprioception).
What does the posterior inferior cerebellar artery (PICA) supply?
It supplies the inferior cerebellum and lateral medulla.
What can infarction in the pyramidal region of the medulla cause?
Bilateral loss of UMN output leading to quadriplegia.
What cranial nerve may be affected by infarction in the anteromedial medulla?
The hypoglossal nerve (CN XII), causing tongue weakness.
What are the other posterior circulation branches that supply the brainstem and cerebellum?
Posterior cerebral artery (PCA), basilar artery branches, superior cerebellar artery (SCA), anterior inferior cerebellar artery (AICA), posterior inferior cerebellar artery (PICA), vertebral artery branches, and anterior spinal artery.
What is the function of radicular arteries?
They reinforce the spinal cord circulation at multiple levels.
What is the Artery of Adamkiewicz and its significance?
It is typically located in the lower thoracic region (T9-L2) and supplies the anterior 2/3 of the spinal cord. Sudden occlusion can cause bilateral upper motor neuron weakness and loss of pain and temperature sensation below the lesion.
What are the effects of complete transection of the spinal cord above C5?
It results in quadriplegia (paralysis of all four limbs), sensory loss below the lesion, and major risk for respiratory failure.
What is the outcome of complete transection between T2-T12?
It results in paraplegia (paralysis of both lower limbs), with arm function spared and trunk/legs affected depending on the level.
What is the risk of respiratory failure with cervical cord injuries at C1-C4?
There is a major risk for respiratory failure as the phrenic nerve (C3-C5) supplies the diaphragm.
What happens with transection between C1-C3?
It usually leads to complete loss of independent respiration, requiring ventilator support.
What is the respiratory function at C4 spinal cord injury?
Some diaphragm function may remain, leading to variable respiratory compromise.
What is the respiratory outcome for injuries at C5 and below?
The diaphragm is spared, allowing the patient to breathe independently.
What is Multiple Sclerosis (MS)?
A demyelinating disease of the CNS affecting UMNs and other CNS regions (somatosensory, special sensory, cerebellum, etc.).
Which nervous system is primarily affected in MS?
The central nervous system (CNS).
What type of pathology is seen in MS?
Multiple scattered areas of demyelination that cannot be explained by a single lesion.
Is MS considered an UMN disorder?
Yes, because demyelination can involve UMN pathways in the subcortical region, brainstem, and spinal cord.
What is Lhermitte's sign, and which disease is it associated with?
An electric shock-like sensation radiating down the spine with neck flexion; associated with MS.
What visual symptom is common in MS?
Optic neuritis leading to visual disturbances or blindness.
What pupillary finding is associated with MS?
Afferent pupillary reflex defect (Marcus Gunn pupil).
What motor findings may occur in MS?
Weakness, hyperreflexia, spasticity, Babinski sign, gait disorders, tonic spasms.
What sensory findings may occur in MS?
Numbness, paresthesia, trigeminal neuralgia, pain, loss of vibration/position sense, incoordination.
What cerebellar findings may occur in MS?
Ataxia, tremor, dysmetria, nystagmus, vertigo.
What autonomic dysfunctions may occur in MS?
Urinary frequency, retention, incontinence, bowel dysfunction, sexual dysfunction.
What psychiatric/cognitive symptoms may be seen in MS?
Depression, cognitive impairment, fatigue.
What is Posterolateral Sclerosis (Subacute Combined Systems Disease)?
A degenerative spinal cord condition caused by long-term vitamin B12 deficiency.
Which spinal cord tracts are affected in Posterolateral Sclerosis?
Dorsal columns (sensory: vibration, proprioception, fine touch) and lateral corticospinal tracts (UMNs).
Why is Posterolateral Sclerosis considered an UMN disease?
Because it involves the lateral corticospinal tracts, producing UMN signs like spasticity, hyperreflexia, and Babinski.
What sensory deficits occur in Posterolateral Sclerosis?
Loss of vibration, proprioception, and fine touch due to dorsal column involvement.
What is ALS (Amyotrophic Lateral Sclerosis)?
A motor neuron disease that affects both UMNs and LMNs, leading to progressive weakness.
Which neurons are affected in ALS?
UMNs in the motor cortex and corticospinal tracts; LMNs in the anterior horn of the spinal cord and brainstem motor nuclei.
Is sensation typically affected in ALS?
No, sensory functions are usually intact.
What EMG finding is characteristic of ALS?
Evidence of denervation and reinnervation, such as fibrillations, fasciculations, and giant motor unit potentials.
What is another name for ALS?
Lou Gehrig's Disease.
What is a parasagittal meningioma?
A tumor arising from the dura along the falx cerebri, between the two cerebral hemispheres.
Which part of the motor cortex is affected by a parasagittal meningioma?
The medial aspect of the motor cortex, which controls lower extremity function.
What is the main clinical consequence of a parasagittal meningioma?
Bilateral weakness of the lower extremities (paraparesis or paraplegia).
Why does a parasagittal meningioma cause weakness in both legs?
Because the tumor compresses the medial motor cortex on both sides, where the leg and foot are represented.
What key finding helps differentiate parasagittal meningioma from spinal cord lesions?
The presence of cortical signs (e.g., seizures, cognitive changes) in addition to bilateral leg weakness.
What type of lesion is Poliomyelitis, and what structures does it affect?
LMN lesion; attacks anterior horn cells, causing flaccid weakness, atrophy, and fasciculations.
What type of lesion is Bell's Palsy, and what is its clinical pattern?
LMN lesion; lesion of CN VII after the nucleus → ipsilateral weakness of both upper and lower face.
What type of lesion is Guillain-Barré Syndrome (GBS), and what is its mechanism?
LMN lesion; peripheral demyelination of roots and peripheral nerves → flaccid paralysis, areflexia, rapid progression, possible respiratory involvement.
What type of lesion is Stroke (CVA), and what signs are seen?
UMN lesion; affects UMNs in cortex/internal capsule/brainstem → contralateral weakness, spasticity, hyperreflexia.
What type of lesion are Medullary & Spinal Cord Vascular Lesions?
Primarily UMN lesions; involve corticospinal tracts (UMNs), though LMN nuclei can be affected if the lesion is at their level.
What type of lesion is Multiple Sclerosis (MS), and what structures are affected?
UMN lesion; CNS demyelination frequently affecting corticospinal tracts, also causes sensory and cerebellar signs.
What type of lesion is Parasagittal Meningioma (falx cerebri)?
UMN lesion; compresses medial motor cortex → bilateral lower extremity weakness.
What type of lesion is Posterolateral Sclerosis (Subacute Combined Systems Disease, B12 deficiency)?
Mixed UMN + LMN involvement (but mostly UMN + dorsal column sensory loss).
What type of lesion is Amyotrophic Lateral Sclerosis (ALS, Lou Gehrig's)?
Mixed UMN + LMN lesion; UMN signs (spasticity, hyperreflexia, Babinski) + LMN signs (fasciculations, atrophy, weakness); sensory spared.
What type of disorder is Poliomyelitis?
LMN disorder; viral illness that targets the cell bodies of lower motor neurons in the spinal cord and brainstem.
What is the pathophysiology of Poliomyelitis?
Viral destruction of LMNs causes denervation of skeletal muscle.
What are the clinical implications of Poliomyelitis?
Acute flaccid paralysis, weakness and atrophy in affected muscles, with no sensory loss.
What is the key point about Poliomyelitis?
Poliomyelitis is an LMN disease.
What type of disorder is Guillain-Barré Syndrome (GBS)?
LMN disorder; acute inflammatory demyelinating poly-radiculoneuropathy.
What is the pathophysiology of Guillain-Barré Syndrome?
Demyelination of peripheral nerves and spinal roots; severe cases may involve axonal damage.
What are the typical triggers for Guillain-Barré Syndrome?
Often occurs post-infection or post-vaccination (parainfectious/autoimmune mechanism).
What is the major risk in Guillain-Barré Syndrome?
Respiratory involvement due to weakness of diaphragm and intercostal muscles.
What are the clinical features of Guillain-Barré Syndrome?
Starts with paresthesias in extremities, followed by progressive motor weakness; areflexia; progression over weeks, then stabilization and recovery over months.