physio exam 3
0.0(0)
Card Sorting
1/106
There's no tags or description
Looks like no tags are added yet.
Last updated 8:19 PM on 4/24/23
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
107 Terms
1
New cards
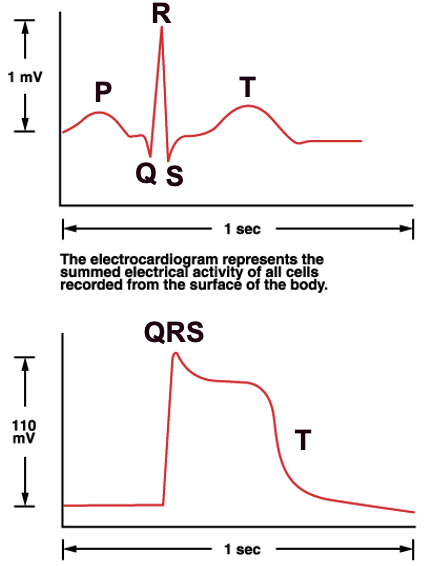
electrocardiogram ECG
what are P, QRS,T
what are P, QRS,T
eletrical view of 3D heart
sum of total electrical activities
represents sum of multiple action potentials
ECG v cardiac AP
1887 first ECG
3 major components:
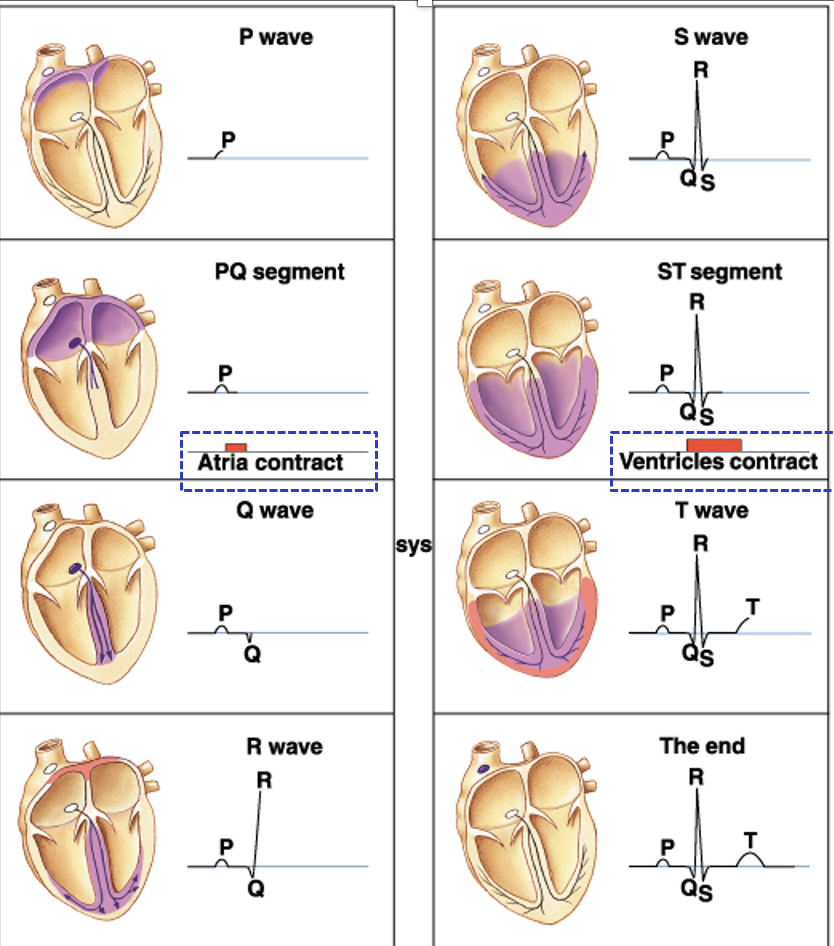
* P wave: atrial depolarization/ contraction
* QRS complex: ventricular depolarization/ contraction
* T wave: ventricular repolarization
extracellular, whole heart: distinct PQRST peaks/troughs
intracellular, one cardiac muscle fiber: no P, combined QRS, and downwards T
sum of total electrical activities
represents sum of multiple action potentials
ECG v cardiac AP
1887 first ECG
3 major components:
* P wave: atrial depolarization/ contraction
* QRS complex: ventricular depolarization/ contraction
* T wave: ventricular repolarization
extracellular, whole heart: distinct PQRST peaks/troughs
intracellular, one cardiac muscle fiber: no P, combined QRS, and downwards T
2
New cards
what ECG tells us 4
1. heart rate: tachycardia vs bradycardia
2. Does a QRS complex follow each P wave, and is the P-R semgent constant in length? if not, there might be problems of signaling conduction through AV node, action potentials from SA may fail to be sent to AV node
3. Normal wave form: is it present
4. Abnormal recordings, irregular rhythm?
3
New cards
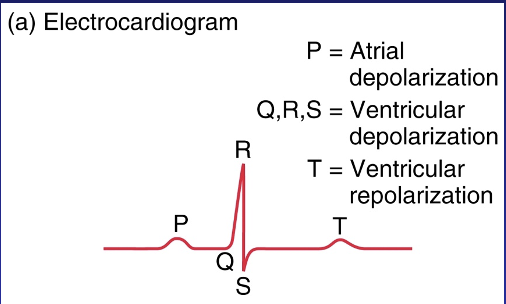
ECG: normal v abnormal
3rd degree block, atrial fibrillation, ventricular fibrillation
describe/draw
3rd degree block, atrial fibrillation, ventricular fibrillation
describe/draw
normal: typical P, QRS, T waves
third degree block: ventricles are not contracting
atrial fib: HB faster, p-wave gone, atria not contracting
ventricular fib: ventricles are fluttering, SA/AV node control is gone, receives local signals instead
third degree block: ventricles are not contracting
atrial fib: HB faster, p-wave gone, atria not contracting
ventricular fib: ventricles are fluttering, SA/AV node control is gone, receives local signals instead
4
New cards
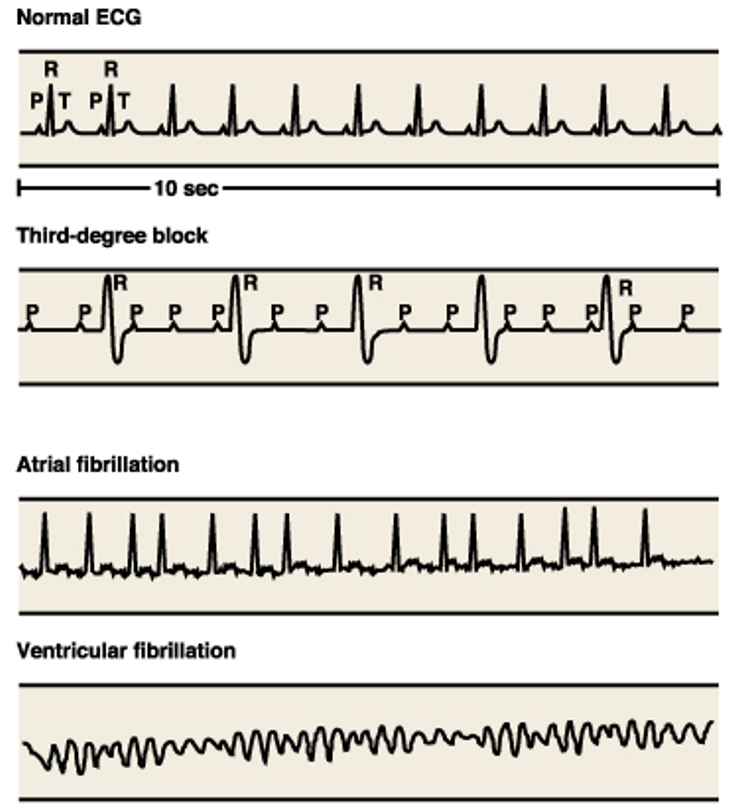
depolarization of heart and the wave type
P, PQ, Q, R, S, ST, T, end
P, PQ, Q, R, S, ST, T, end
5
New cards
cardiac cycle: diastole, systole, which phases
diastole: relaxation/filling, 70% of the cycle, phases 1/2/5
systole: contraction, 30%, phases 3/4
5 phases of the cycle:
1. mid/late diastole:
2. atrial systole
3. iso-volumic contraction
4. ventricular ejection
5. iso-volumic relaxation
systole: contraction, 30%, phases 3/4
5 phases of the cycle:
1. mid/late diastole:
2. atrial systole
3. iso-volumic contraction
4. ventricular ejection
5. iso-volumic relaxation
6
New cards
cardiac cycle
1. late diastole: heart at rest, atrial and ventricle diastole, atria filling with blood, ventricle just finished a contraction, ventricles passively fill with blood \~80%
* Pvc > Pa > Pv
2. atrial systole: completion of ventricular filling: atrial systole\~20% of blood fills, some goes into ventricles, small amount of blood forced backward into veins because there are no one-way valves to block backflow
* Pa > Pv
* EDV: maximum amount of blood in ventricles occurs at the end of ventricular relaxation 135mL
3. early ventricular contraction and the first heart sound: atria contracting, depolarization moving towards heart apex, ventricle systole = blood pushed to AV valves, forces them closed so blood cannot flow into atria, closure of AV valve = LUB
* isovolumic ventricular contraction: AV and semilunar valves are closed, V blood has no where to go, V continues to contract, high pressure, no change in volume
* Paorta > Pv > Pa
4. ventricular ejection: heart pumps, ventricles contract to generate enough pressure to open semilunar valve and push blood into the arteries, atria continues to fill
* Pv > Paorta
* ESV: minimum amount of blood in ventricles 65mL
5. isovolumic ventricular relaxation and second heart sound: ventricles repolarize and relax, V pressure decreases below A pressure = blood flows backward into the heart against semilunar valve forcing them closed = dub sound
* Paorta > Pv > Pa
7
New cards
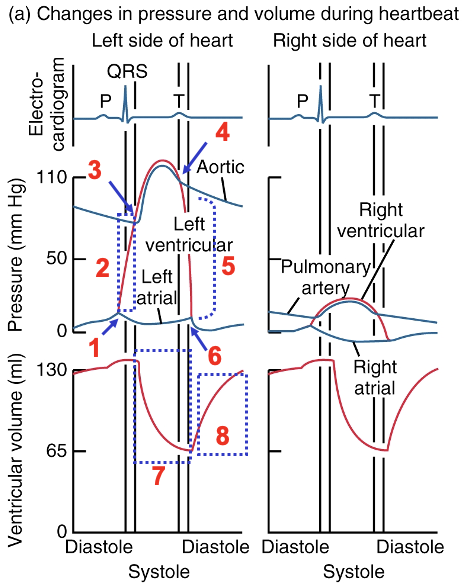
Wiggers Diagram: L26S3-4
SL valves open/close
AV valves open/close
ventricular ejection/filling
isovolumetric contraction/relaxation
SL valves open/close
AV valves open/close
ventricular ejection/filling
isovolumetric contraction/relaxation
SL = pulmonary
SL: ventricular volume decreases, ventricular pressure systole increases
AV: ventricular volume diastole increases
\
SL valves open? 3
SL valves close? 4
AV valves open? 6
AV valves close? 1
Ventricular ejection? 7
Ventricular filling? 8
Isovolumetric contraction? 2
Isovolumetric relaxation? 5
SL: ventricular volume decreases, ventricular pressure systole increases
AV: ventricular volume diastole increases
\
SL valves open? 3
SL valves close? 4
AV valves open? 6
AV valves close? 1
Ventricular ejection? 7
Ventricular filling? 8
Isovolumetric contraction? 2
Isovolumetric relaxation? 5
8
New cards
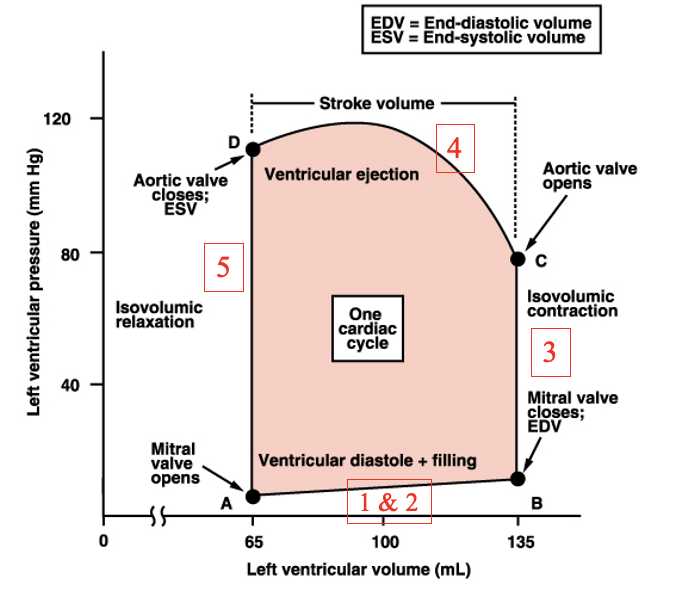
pressure-volume loop
draw and label
draw and label
change in volume and pressure
Pressure/volume loop = P x V = area = work, 1 ml = 1 cm^3, area tells us how much work is done by heart,
A: mitral valve opens
B: mitral valve closes, EDV
C: aortic valve opens
D: aortic valve closes, ESV
A → B: passive filling and atrial contraction, steps 1+2 cardiac cycle
B → C: isovolumic contraction, step 3
C → D: ejection of blood into aorta. step 4
D → A: isovolumic relaxation, step 5
Pressure/volume loop = P x V = area = work, 1 ml = 1 cm^3, area tells us how much work is done by heart,
A: mitral valve opens
B: mitral valve closes, EDV
C: aortic valve opens
D: aortic valve closes, ESV
A → B: passive filling and atrial contraction, steps 1+2 cardiac cycle
B → C: isovolumic contraction, step 3
C → D: ejection of blood into aorta. step 4
D → A: isovolumic relaxation, step 5
9
New cards
work performed by the heart
work = g x cm = P x V = (force/area) \* V
area of pressure-volume loop = work of 1 cycle
right ventricle has smaller pressure than left ventricle
Work of LV > RV why? RV pressure is less than LV pressure, volume is the same for both, right ventricle works less than LV, RV only covers pulmonary but LV covers the rest of of system
area of pressure-volume loop = work of 1 cycle
right ventricle has smaller pressure than left ventricle
Work of LV > RV why? RV pressure is less than LV pressure, volume is the same for both, right ventricle works less than LV, RV only covers pulmonary but LV covers the rest of of system
10
New cards
2 factors affecting the work done by the heart
* increases EDV: preload, good for heart, pressure stays the same and volume increases
* increasing afterload: bad for cardiovascular system, volume stays the same but pressure increases
* increasing afterload: bad for cardiovascular system, volume stays the same but pressure increases
11
New cards
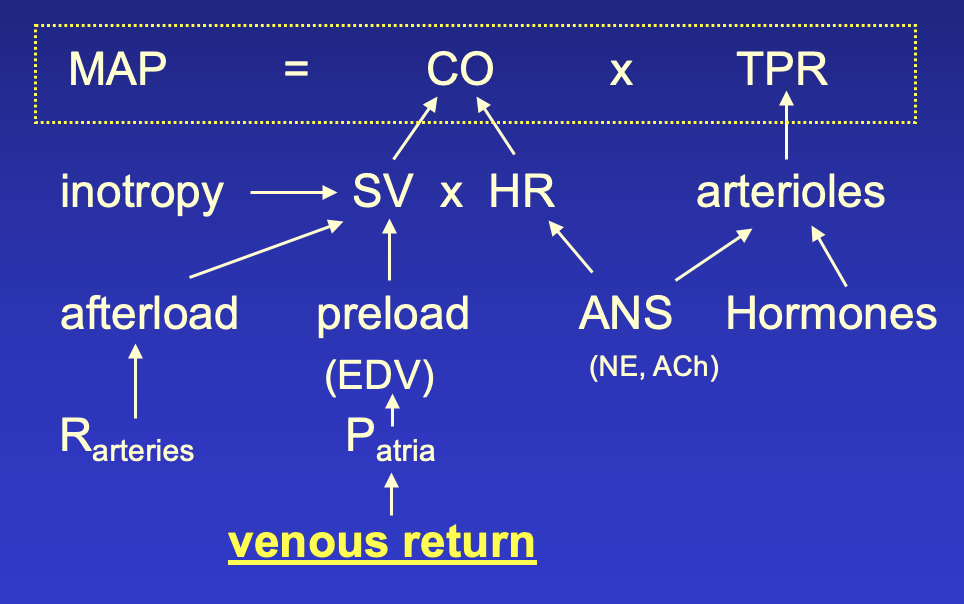
cardiac output
CO = HR x SV
measure of cardiac performance
Flow Q = /\\P / R = arterial pressure / Rtotal peripheral
MAP = CO x TPR
mean arterial pressure = cardiac output x total peripheral resistance
MAP: baroreceptors, can be easily monitored?, used to change cardiac function, too high? ejecting too much blood, must decrease CO to decrease MAP
measure of cardiac performance
Flow Q = /\\P / R = arterial pressure / Rtotal peripheral
MAP = CO x TPR
mean arterial pressure = cardiac output x total peripheral resistance
MAP: baroreceptors, can be easily monitored?, used to change cardiac function, too high? ejecting too much blood, must decrease CO to decrease MAP
12
New cards
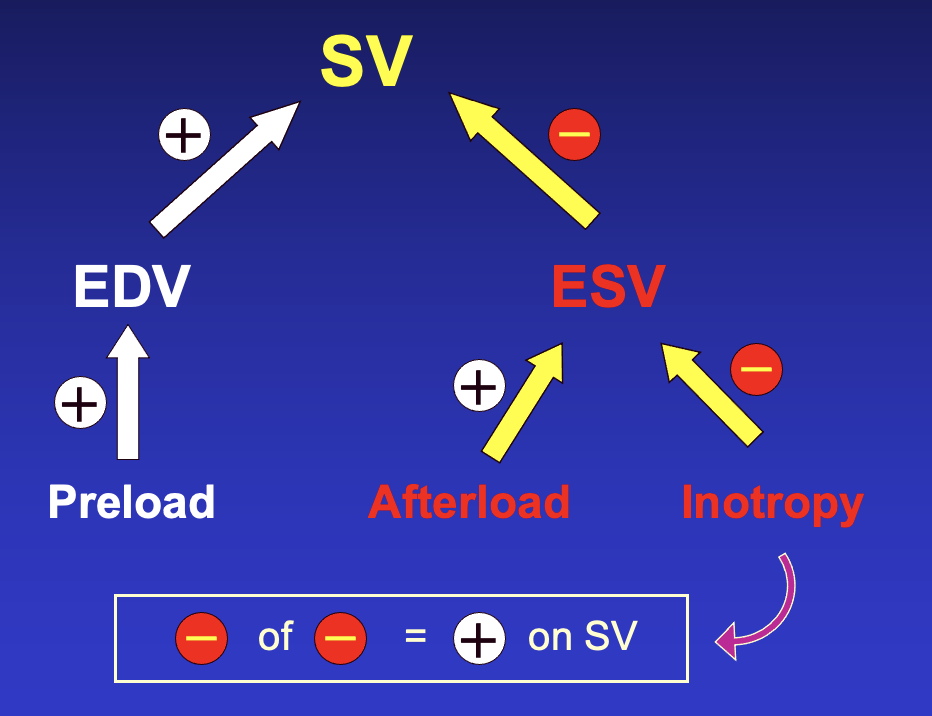
EDV and ESV and SV
SV = EDV - ESV
SV: volume of blood pumped per ventricle per contraction, directly related tp force generated by cardiac muscle during contraction
EDV: preload is affected by:
* elasticity of ventricle wall, filling time, more space for blood to fill = longer filling time
* venous return → filling pressure = Pa-Pv, Pa is affected by venous return
ESV: affected by
* afterload: arterial or aortic resistance (cannot eject blood as much)
* inotropy: contractility, increase inotropy? ESV decreases - like squeezing a water bottle, high contractility is bad because there will be less leftover blood in the heart
these factors dictate work done by the heart
SV: volume of blood pumped per ventricle per contraction, directly related tp force generated by cardiac muscle during contraction
EDV: preload is affected by:
* elasticity of ventricle wall, filling time, more space for blood to fill = longer filling time
* venous return → filling pressure = Pa-Pv, Pa is affected by venous return
ESV: affected by
* afterload: arterial or aortic resistance (cannot eject blood as much)
* inotropy: contractility, increase inotropy? ESV decreases - like squeezing a water bottle, high contractility is bad because there will be less leftover blood in the heart
these factors dictate work done by the heart
13
New cards
preload
Frank-Starling
Frank-Starling
initial stretching of the cardiac myocytes prior to contraction
aka the degree of myocardial stretch before contraction
muscle length → preload → EDV
Frank-Starling mechanism: optimal filling pressure and stroke volume curve, length-tension relationship, stroke volume is proportional to EDV
aka the degree of myocardial stretch before contraction
muscle length → preload → EDV
Frank-Starling mechanism: optimal filling pressure and stroke volume curve, length-tension relationship, stroke volume is proportional to EDV
14
New cards
factors determining R ventricular preload - 11
\
LVP determined by same but with central venous pressure than pulmondary
\
LVP determined by same but with central venous pressure than pulmondary
positively impacted by
* atrial contractility
* ventricular compliance: ventricle relaxes more = more blood
* venous pressure: more blood returning, negatively impacted by venous compliance, increased by venous volume
negatively impacted by
* heart rate: filling time is decreased when heart rate increases
* inflow resistance: high? less blood can flow through
\
venous return + total blood volume:??
* muscle contraction increases preload
* respiration deep breaths increases preload
* high gravity decreases preload
* vasoconstriction increases preload
* atrial contractility
* ventricular compliance: ventricle relaxes more = more blood
* venous pressure: more blood returning, negatively impacted by venous compliance, increased by venous volume
negatively impacted by
* heart rate: filling time is decreased when heart rate increases
* inflow resistance: high? less blood can flow through
\
venous return + total blood volume:??
* muscle contraction increases preload
* respiration deep breaths increases preload
* high gravity decreases preload
* vasoconstriction increases preload
15
New cards
afterload
the combined load of EDV and arterial resistance during ventricular contraction
the resistance to ventricular ejection
the load that the heart must eject the blood against
aortic pressure: increased in hypertension
the resistance to ventricular ejection
the load that the heart must eject the blood against
aortic pressure: increased in hypertension
16
New cards
positive inotropy
starlings law of the heart
starlings law of the heart
starlings law of the heart:
* as EDV increases, pressure generated increases
positive inotropes: anything that affects contractility
* NE
* increases pressure without a change in volume
* increases contractility
* positively influence stroke volume
* squeezing more? ESV decreases, SV increases
* as EDV increases, pressure generated increases
positive inotropes: anything that affects contractility
* NE
* increases pressure without a change in volume
* increases contractility
* positively influence stroke volume
* squeezing more? ESV decreases, SV increases
17
New cards
effects on SV - flow chart
preload, afterload, inotropy
18
New cards
overall goal of the CV system
flow chart of what things affect MAP = CO x TPR
flow chart of what things affect MAP = CO x TPR
maintain mean arterial pressure
19
New cards
respiration: gases kinds
properties of gases 2
convection
properties of gases 2
convection
properties of gases: partial pressure, solubility
respiration dependent on gas exchange
convection: gases traveling in liquid + air, like conduction
pH regulation, breathing air, breathing water, physical properties of gases
respiratory gases: O2 + CO2
* O2 simple diffusion, convective gas transport
* convective gas transport = transport by bulk flow: occurs when a gas or aqueous solution flows and they are carried by the fluid flow
* CO2 both^ + active transport: related to pH regulation which is important with active transport and rapid movement
respiration dependent on gas exchange
convection: gases traveling in liquid + air, like conduction
pH regulation, breathing air, breathing water, physical properties of gases
respiratory gases: O2 + CO2
* O2 simple diffusion, convective gas transport
* convective gas transport = transport by bulk flow: occurs when a gas or aqueous solution flows and they are carried by the fluid flow
* CO2 both^ + active transport: related to pH regulation which is important with active transport and rapid movement
20
New cards
fractional composition of Air
facts about the composition and can it change?
facts about the composition and can it change?
doesn’t change with altitude
Patm changes with altitude
can change in confined spaces, due to biological processes like decay and respiration
example: gopher burrow - confined area, limited air, O2 down CO2 up
O2 \~ 20.95%
CO2 \~ 0.03%
nitrogen \~ 78.09%
argon \~ 0.93%
Patm changes with altitude
can change in confined spaces, due to biological processes like decay and respiration
example: gopher burrow - confined area, limited air, O2 down CO2 up
O2 \~ 20.95%
CO2 \~ 0.03%
nitrogen \~ 78.09%
argon \~ 0.93%
21
New cards
Daltons Law of Partial Pressures
Ptotal sea level + mt everest
Ptotal sea level + mt everest
P total = 760mmHg @ sea level = pO2 + pCO2 + pN2
P total = (0.209)(760) + (0.0003)(760) + (0.78)(760) = 760mmHg
pO2 = Patm \* %comp = 158.8mmHg @sea level
pO2 @ Mt. Everest = 0.209 \* 250 = 52.3mmHg
3 times less partial pressure of O2 = 3x harder to breath
P total = (0.209)(760) + (0.0003)(760) + (0.78)(760) = 760mmHg
pO2 = Patm \* %comp = 158.8mmHg @sea level
pO2 @ Mt. Everest = 0.209 \* 250 = 52.3mmHg
3 times less partial pressure of O2 = 3x harder to breath
22
New cards
water vapor pressure
Pgas not affected much by temperature
Ph2o = water vapor pressure IS affected by temperature
increase temp = increase ph2o
humid day = harder to breath
Ph2o = water vapor pressure IS affected by temperature
increase temp = increase ph2o
humid day = harder to breath
23
New cards
calculating Pgas
MUST take into consideration Ph2o
Ptotal: (0.209)(Patm-Ph2o) + (0.0003)(Patm-Ph2o) + (0.78)(Patm-Ph2o)
@ 37°C, PH2O = 47 mm Hg
Ptotal: (0.209)(Patm-Ph2o) + (0.0003)(Patm-Ph2o) + (0.78)(Patm-Ph2o)
@ 37°C, PH2O = 47 mm Hg
24
New cards
Henry’s Law
def, dep on 3, equation
def, dep on 3, equation
determine the amount of gas dissolved in fluids (solubility)
dependent on temperature, ionic strength of fluid, and type of gas
\[gas\] = alpha(gas) x Pgas
alpha = solubility coefficient
dependent on temperature, ionic strength of fluid, and type of gas
\[gas\] = alpha(gas) x Pgas
alpha = solubility coefficient
25
New cards
CO2 in water
CO2 much more soluble in water than O2
CO2 dissolved in water determined by: gas solubility and CO2 partial pressure
gas solubility depends on temp
solubilities of gases in water @ 15C @ 1 atm
* Oxygen: 34.1 ml / L h2o
* Nitrogen: 16.9 ml / L h2o
* CO2: 1019 ml / L h2o
difference between O2 and CO2 concentration 21% to 0.03%, there is 700x difference in their concentrations
difference between O2 and CO2 solubility is 34.1 to 1019, there is a 30x difference in their solubilities
700 difference / 30 difference = 23x
oxygen solubility is 30 times lower than CO2, but the concentration is significantly greater 700x more
even though CO2 is more soluble, O2 concentration in water will be higher than CO2
O2 is 23 times more dissolved in water bc partial pressure > solubility
CO2 dissolved in water determined by: gas solubility and CO2 partial pressure
gas solubility depends on temp
solubilities of gases in water @ 15C @ 1 atm
* Oxygen: 34.1 ml / L h2o
* Nitrogen: 16.9 ml / L h2o
* CO2: 1019 ml / L h2o
difference between O2 and CO2 concentration 21% to 0.03%, there is 700x difference in their concentrations
difference between O2 and CO2 solubility is 34.1 to 1019, there is a 30x difference in their solubilities
700 difference / 30 difference = 23x
oxygen solubility is 30 times lower than CO2, but the concentration is significantly greater 700x more
even though CO2 is more soluble, O2 concentration in water will be higher than CO2
O2 is 23 times more dissolved in water bc partial pressure > solubility
26
New cards
water as respiratory medium
increase Patm, increase \[gases\] dissolved in water
\[O2\] air: 209 (700x more than CO2), water 4.7 (23 times more than CO2)
\[CO2\] air: 0.3 , water: 0.16
ratio of 44:1
44X harder to extract O2 from water than air
gill’s are more energy efficient than lungs - use mass movement to move water across gills
air is better respiratory medium because oxygen concentration has greater concentration of O2 than water
\[O2\] air: 209 (700x more than CO2), water 4.7 (23 times more than CO2)
\[CO2\] air: 0.3 , water: 0.16
ratio of 44:1
44X harder to extract O2 from water than air
gill’s are more energy efficient than lungs - use mass movement to move water across gills
air is better respiratory medium because oxygen concentration has greater concentration of O2 than water
27
New cards
comparison of air v water as a respiratory medium 5
1. \[O2\] 44x greater in air
2. viscosity: H2O 50x greater than air
3. diffusion rate
* flux
* J = K A/\\C / /\\x
* K = diffusion coefficient in air = cm^2/atm\*min
* K is 8000x lower in H2O vs air
4. thermal conductivity: H2O 25x greater than air
5. heat capacity: H2O 3000x greater than air
28
New cards
respiration in water
\[O2\] 44x lower in water → higher ventilation rate
density and viscosity is greater than air
unidirectional flow
humans breath tidally in and out
energy demanding to breath tidally in water, so its unidirectionally
density and viscosity is greater than air
unidirectional flow
humans breath tidally in and out
energy demanding to breath tidally in water, so its unidirectionally
29
New cards
structure of fish’s gill
teleost: bony fish
gills: typically 4 arches, water from mouth flows over gills
lamella: singular gills? used to increase SA?
* alveola = lamella, similar functions
* H2O flows across well-vascularized lamellae in opposite direction of blood
operculum: flap that covers the gills
sheet flow: water passing in between gill lamella
* countercurrent flow: water goes one way and blood flows the opposite direction so oxygen can get into blood
* increase Pblood
* decrease thickness of sheet
* when thickness is wide = water can pass through easier
* when gap is smaller = better O2 exchange
* increasing thickness of sheet decreases the gap?
* LECTURE 29 SLIDE 2
gills: typically 4 arches, water from mouth flows over gills
lamella: singular gills? used to increase SA?
* alveola = lamella, similar functions
* H2O flows across well-vascularized lamellae in opposite direction of blood
operculum: flap that covers the gills
sheet flow: water passing in between gill lamella
* countercurrent flow: water goes one way and blood flows the opposite direction so oxygen can get into blood
* increase Pblood
* decrease thickness of sheet
* when thickness is wide = water can pass through easier
* when gap is smaller = better O2 exchange
* increasing thickness of sheet decreases the gap?
* LECTURE 29 SLIDE 2
30
New cards
gill surface area also varies among fish taxa
thickness of the membrane
thickness of the membrane
larger gill SA = extract more oxygen
greater O2 extraction = more active
skipjack tuna: very active: 13.2cm^2/g
plaice: active: 4.33
oyster toadfish: sluggish: 2.14
climbing perch: very sluggish: 1.50
thickness of membrane:
* too thin? gills can collapse out of water
* thin is good
* too thick? more difficult to breath
greater O2 extraction = more active
skipjack tuna: very active: 13.2cm^2/g
plaice: active: 4.33
oyster toadfish: sluggish: 2.14
climbing perch: very sluggish: 1.50
thickness of membrane:
* too thin? gills can collapse out of water
* thin is good
* too thick? more difficult to breath
31
New cards
concurrent design
water and blood flow in the same direction
water pressure decreases, blood pressure increases = the water and blood will eventually have the same pressure = no exchange of O2
when first in contact with water, pressure gradient is high but after long exposure, pressure gradient decreases to 0
no continuous pressure gradient/ O2 exchange
diffusion = K \* A (PO2water - PO2 tissue) / distance
\
water pressure decreases, blood pressure increases = the water and blood will eventually have the same pressure = no exchange of O2
when first in contact with water, pressure gradient is high but after long exposure, pressure gradient decreases to 0
no continuous pressure gradient/ O2 exchange
diffusion = K \* A (PO2water - PO2 tissue) / distance
\
32
New cards
countercurrent design
allows for greater transfer of O2 from water to blood
pressure gradient is constant because
better for transfer of O2 bc gradient is maintained
pressure gradient is constant because
better for transfer of O2 bc gradient is maintained
33
New cards
O2 uptake efficiency
def, increase by 3, equation
def, increase by 3, equation
O2 uptake efficiency: % removed from medium
U = (PO2 in - PO2 out) \* 100 / PO2 in
oxygen uptake efficiencies vary among species, physiological states: active and high
surface area and thickness effect O2 uptake efficiency
increase O2 uptake efficiency? 1) increase SA 2) thickness thinner 3) ventilation/perfusion ratio
U = (PO2 in - PO2 out) \* 100 / PO2 in
oxygen uptake efficiencies vary among species, physiological states: active and high
surface area and thickness effect O2 uptake efficiency
increase O2 uptake efficiency? 1) increase SA 2) thickness thinner 3) ventilation/perfusion ratio
34
New cards
uptake efficiency determined by 2
capacity and flow
gas transfer capacity: a composite value determined by thickness, conductance of tissue, mucus layers, Krogn’s coefficient of fas molecules in the relevant fluids
gas transfer capacity C = O2 uptake rate (flux) / partial pressure difference
flux = K \* A \* /\\P / x
\
flow Q: of blood and water across diffusion surface
if water flow is very high relative to blood flow, there is little change in its PO2 as it flows across gills (going too fast for maximum diffusion)
gas transfer capacity: a composite value determined by thickness, conductance of tissue, mucus layers, Krogn’s coefficient of fas molecules in the relevant fluids
gas transfer capacity C = O2 uptake rate (flux) / partial pressure difference
flux = K \* A \* /\\P / x
\
flow Q: of blood and water across diffusion surface
if water flow is very high relative to blood flow, there is little change in its PO2 as it flows across gills (going too fast for maximum diffusion)
35
New cards
diffusion distance (water-blood) varies among fish taxa
3\~8 um diff distance in fish,
diff distance in humans is 0.4um
the slower the fish the greater the diff distance
diff distance in humans is 0.4um
the slower the fish the greater the diff distance
36
New cards
two measures that underlie ventilation: perfusion ratio
ventilation rate / blood perfusion rate = Vg/Q = ratio
if blood or water moves too fast = efficiency decreases
1:1 ratio is best
most fish have 10:1 ratio, more water must be perfused to get the same amount of oxygen as air (since water PO2 is low, the capacity rate values are low)
ventilating air is easier than water
2 disadvantages of fish: 1) oxygen content in water is LOW 2) water movement requires more energy x10 more
if blood or water moves too fast = efficiency decreases
1:1 ratio is best
most fish have 10:1 ratio, more water must be perfused to get the same amount of oxygen as air (since water PO2 is low, the capacity rate values are low)
ventilating air is easier than water
2 disadvantages of fish: 1) oxygen content in water is LOW 2) water movement requires more energy x10 more
37
New cards
how do water-breathers ventilate
1. buccal pumping:
* floor of mouth is raised/lowered
* water flows into mouth through gills and out the operculum
* water flows through pressure gradient
* P external > Pbuccal + mouth opens (volume increase) = water enters the mouth
* mouth closes (volume decreases) + Pbuccal > P external = water leaves the gills/operculum to external
2. ram ventilation:
* mouth opens, swimming motion forces continuous flow across gils
* as swimming speed increases = faster ventilation = more oxygen
* gape: wide gape = more water = more oxygen
* smaller gapes not as good
* only used for faster swimming, will not work if fish swims too slowly
38
New cards
3 organs, respiration of air
1. gills
* terrestrial arthropods
* rigid
* evaginated
* breath air
2. trachea
* insects
* passive diffusion
* open circulatory system
* have another system to supply oxygen - tracheal
* there is a little bit of fluid in tracheole tips
* fluid levels in tracheole tips drops during high metabolic demand = increases gas diffusion rates
3. lung
* invaginated
* diffusion lungs:
* molluscs
* air coming in and out is passive
* not very invaginated - like a simple bag
* lower SA
* can explain why snail is slow
* ventilation lungs:
* tidal flow
* unidirectional flow
* bidirectional flow = less efficient
* crosscurrent efficiency: in between concurrent and countercurrent
39
New cards
structure of mammalian lung
develops as a diverticulum of gut
right lung: 3 lobes, upper, middle, lower
left lung: 2 lobes, upper + lower
functionally the same LL and RL
diaphragm: membrane of muscles, designed to recoil, when it contracts it pushes down, when it relaxes it recoils up
pleural space: space covers the ribs, surrounded by membrane and fluid, fluid has negative pressure, no negative pressure = lungs collapse?
trachea: divides bronchi into L and R
highly subdivided in mammals
much simpler in amphibians and reptiles
right lung: 3 lobes, upper, middle, lower
left lung: 2 lobes, upper + lower
functionally the same LL and RL
diaphragm: membrane of muscles, designed to recoil, when it contracts it pushes down, when it relaxes it recoils up
pleural space: space covers the ribs, surrounded by membrane and fluid, fluid has negative pressure, no negative pressure = lungs collapse?
trachea: divides bronchi into L and R
highly subdivided in mammals
much simpler in amphibians and reptiles
40
New cards
conducting airways v respiratory airways
trachea, main bronchi, bronchiole, terminal bronchiole = conducting airways, dead space, not designed for gas diffusion
\
respiratory bronchiole, alveolar duct, alveolus, alveolar sac = respiratory airways, involved in gas exchange
* alveolus = exchange surface
\
respiratory bronchiole, alveolar duct, alveolus, alveolar sac = respiratory airways, involved in gas exchange
* alveolus = exchange surface
41
New cards
pressure and volume change in the lung
pneumothorax
how does lung remain expanded
pneumothorax
how does lung remain expanded
inhalation: diaphragm contracts/ lowers, Patm > Plung, volume increases, active part of breathing, easy to breath in because of pressure difference
exhalation: diaphragm relaxes/raises, Plung > Patm, volume decreases, easy to breath out because of pressure difference, passive because muscle relaxing
\
lung membrane-encased and remain expanded because of negative pressure of fluid filled pleural cavity
\
pneumothorax: if pleural cavity is punctured and negative pressure destroyed (aka replaced with air) lung often collapses
exhalation: diaphragm relaxes/raises, Plung > Patm, volume decreases, easy to breath out because of pressure difference, passive because muscle relaxing
\
lung membrane-encased and remain expanded because of negative pressure of fluid filled pleural cavity
\
pneumothorax: if pleural cavity is punctured and negative pressure destroyed (aka replaced with air) lung often collapses
42
New cards
volume changes in the lung
residual volume
during high activity, tidal volume _?
vital capacity
residual volume
during high activity, tidal volume _?
vital capacity
inhalation is active, exhalation is passive, recoil from intercostal muscles
during high activity: tidal volume increases and utilizes inspiratory/ expiratory reserves
residual volume: lungs never empty completely
vital capacity: maximum breathing in and out, cannot maintain this maximum, typically 6L which almost matches blood volume \~5L (but lung never fully empties so approx 1:1 ratio)
\
during high activity: tidal volume increases and utilizes inspiratory/ expiratory reserves
residual volume: lungs never empty completely
vital capacity: maximum breathing in and out, cannot maintain this maximum, typically 6L which almost matches blood volume \~5L (but lung never fully empties so approx 1:1 ratio)
\
43
New cards
alveolar ventilation volume
alveolar ventilation rate
if tidal V = dead V
low ventilation rate vs high
total volume of air
alveolar ventilation rate
if tidal V = dead V
low ventilation rate vs high
total volume of air
alveolar ventilation volume (Va) = tidal - dead
Va = Vt-Vd
alveolar ventilation rate = Va \* frequency of breath
dead = anatomical dead space = conducting airways \~ 150ml
dead space never changes (with age yes but not important)
air must travel through the dead space before it can reach the respiratory airways
if tidal volume = dead volume … then = 0 ventilation volume
breathing
breathing shallow and quick = low ventilation rate
deep long slow breaths = high ventilation rate
total volume of air 6000mL
as tidal increases frequency of breath decreases
Va = Vt-Vd
alveolar ventilation rate = Va \* frequency of breath
dead = anatomical dead space = conducting airways \~ 150ml
dead space never changes (with age yes but not important)
air must travel through the dead space before it can reach the respiratory airways
if tidal volume = dead volume … then = 0 ventilation volume
breathing
breathing shallow and quick = low ventilation rate
deep long slow breaths = high ventilation rate
total volume of air 6000mL
as tidal increases frequency of breath decreases
44
New cards
bicarbonate and pH
what happens when ventilation rate too low, too high,
what happens when ventilation rate too low, too high,
if ventilation rate is too low, alveolar CO2 builds up and results in hypercapnia = high blood pCO2 = respiratory acidosis = drop in plasma pH due to the release of H
if ventilation rate too rapid, CO2 is eliminated too quickly and can result in respiratory alkalosis
metabolic pathways consume O2 and produce CO2 which have consequences in the blood
CO2 high = proton concentration high = pH low
CO2 + H2O
if ventilation rate too rapid, CO2 is eliminated too quickly and can result in respiratory alkalosis
metabolic pathways consume O2 and produce CO2 which have consequences in the blood
CO2 high = proton concentration high = pH low
CO2 + H2O
45
New cards
regulation of ventilation - water and air breathers
phrenic nerve
phrenic nerve
water breathers: respond to O2 decrease in blood and tissues
air breathers: chemoreceptors respond to increase CO2/H
* chemoreceptors:
1. carotid and aortic bodies: detect increased CO2 and/or low pH
2. cerebrospinal fluid chemoreceptors: has poor buffering ability, very sensitive to pH, medullary receptors respond to high CO2 and low pH
3. peripheral chemoreceptors
* pulmonary stretch receptors: prevents overexpansion, help regulate inflation of lungs
* phrenic nerve: diaphragm relays inspiratory signal from medulla respiratory center (nerve > medulla > signal to diaphragm), inflation of lung inhibits inspiratory activity in medulla = reduces the frequency of breathing
* increase activity? increase phrenic nerve activity, increase in discharge rate drops lung pressure
* discharge rate is enhanced by high PaCO2 (rapid rise results in deeper inspiration)
air breathers: chemoreceptors respond to increase CO2/H
* chemoreceptors:
1. carotid and aortic bodies: detect increased CO2 and/or low pH
2. cerebrospinal fluid chemoreceptors: has poor buffering ability, very sensitive to pH, medullary receptors respond to high CO2 and low pH
3. peripheral chemoreceptors
* pulmonary stretch receptors: prevents overexpansion, help regulate inflation of lungs
* phrenic nerve: diaphragm relays inspiratory signal from medulla respiratory center (nerve > medulla > signal to diaphragm), inflation of lung inhibits inspiratory activity in medulla = reduces the frequency of breathing
* increase activity? increase phrenic nerve activity, increase in discharge rate drops lung pressure
* discharge rate is enhanced by high PaCO2 (rapid rise results in deeper inspiration)
46
New cards
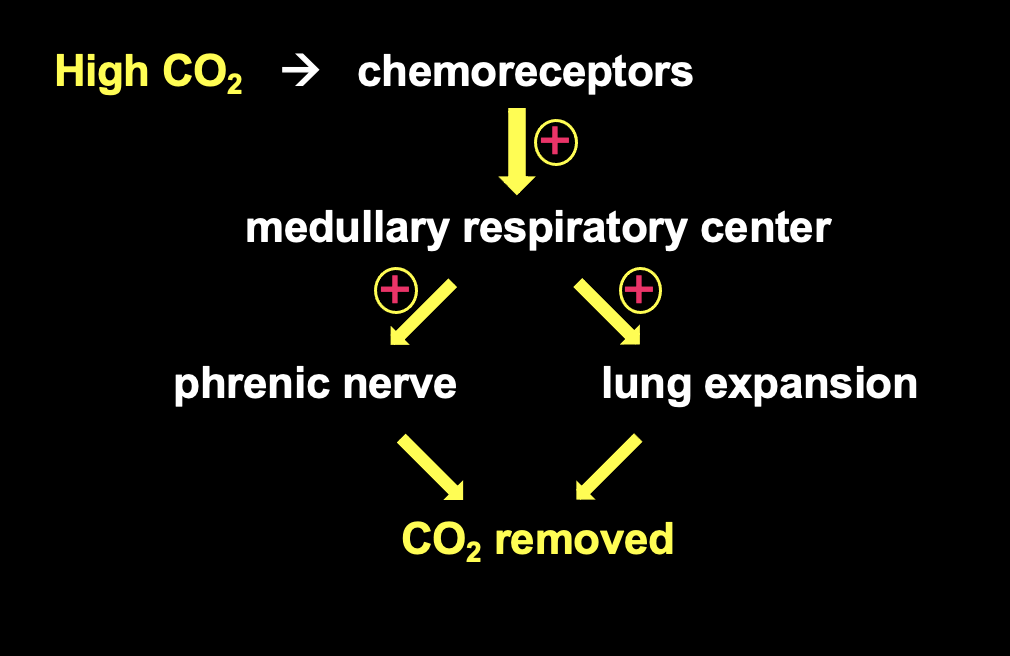
air breathers pathway to remove CO2
regulated by
how everything work together - draw flow chart
regulated by
how everything work together - draw flow chart
respiration regulated by brain, medulla respiratory center
lung expansion + phrenic nerve = breathing bigger to get rid of CO2
lung expansion + phrenic nerve = breathing bigger to get rid of CO2
47
New cards
respiratory pigments
funx 3
funx 3
in absence of resp pigments, O2 in solution in blood would be 0.3ml O2/ 100ml blood, but should be 20+ml O2 / 100ml blood \~70x greater
function:
1. increase carrying capacity (x70 more)
2. maintain PO2 gradient (air > blood > tissue)
3. transport (air > lung > blood > tissue)
function:
1. increase carrying capacity (x70 more)
2. maintain PO2 gradient (air > blood > tissue)
3. transport (air > lung > blood > tissue)
48
New cards
types of respiratory pigments
hemoglobin and myoglobin: heme Fe2+, vertebrates, myoglobin mostly in muscle and stores O2 rather than transport O2
hemocyanin: copper, invertebrates, not in cells, bluish color = oxygenated
hemerythrin: no heme, annelids and brachiopods, iron directly binds to protein
hemocyanin: copper, invertebrates, not in cells, bluish color = oxygenated
hemerythrin: no heme, annelids and brachiopods, iron directly binds to protein
49
New cards
structure of vertebrate hemoglobin and myoglobin
4 types hb
4 types hb
Hb is tetrameric, 4 subunits, 2 alpha + 2 beta, each with heme
myoglobin has 1 subunit looks like alpha, 1 heme
oxy Hb: O2 bound
deoxy Hb: no O2
carboxy Hb: CO bound
carbamino Hb: CO2 bound
CO competes with O2, CO2 doesn’t compete with O2
binding affinity of CO is 200x greater than O2 = very bad
\
myoglobin has 1 subunit looks like alpha, 1 heme
oxy Hb: O2 bound
deoxy Hb: no O2
carboxy Hb: CO bound
carbamino Hb: CO2 bound
CO competes with O2, CO2 doesn’t compete with O2
binding affinity of CO is 200x greater than O2 = very bad
\
50
New cards
hemoglobin in red blood cells erythrocytes
matured RBC contain what?
hematocrit
erythropoiesis
intracellular v extracellular Hb
matured RBC contain what?
hematocrit
erythropoiesis
intracellular v extracellular Hb
mammalian RBC: 4-10um
matured RBC: no nucleus, no mito, no ribosome, no energy use, carries hemoglobin
hematocrit: percentage of total blood volume occupied by RBC
erythropoiesis: making RBC, bone marrow, hormone erythropoetin secreted from kidney stimulate synthesis of RBC, stimulated in low O2 conditions
in some invertebrates, Hb can be found in the blood plasma = extracellular Hb
hemoglobin in RBC = intracellular Hb
matured RBC: no nucleus, no mito, no ribosome, no energy use, carries hemoglobin
hematocrit: percentage of total blood volume occupied by RBC
erythropoiesis: making RBC, bone marrow, hormone erythropoetin secreted from kidney stimulate synthesis of RBC, stimulated in low O2 conditions
in some invertebrates, Hb can be found in the blood plasma = extracellular Hb
hemoglobin in RBC = intracellular Hb
51
New cards
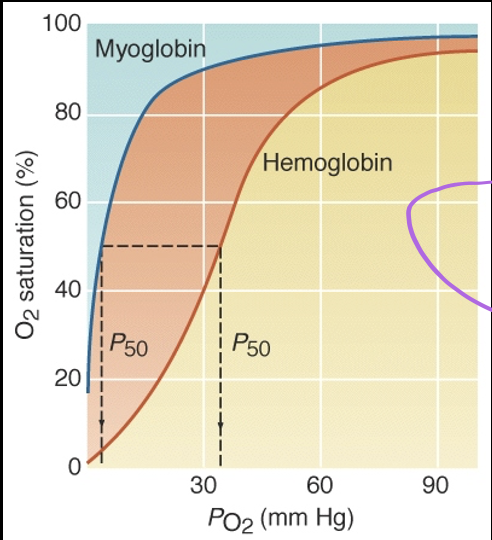
oxygen dissociated curve of hemoglobin is sigmoidal
P50
P50
subunit cooperativity: oxygenation of first subunit enhances binding affinity of the other subunits
myoglobin curve NOT cooperative, hyperbolic, has higher O2 affinity, lower P50, only has 1 binding site so cannot be cooperative
the greater P50 = O2 binding affinity is lower
hemoglobin has lower affinity for O2 than myoglobin
it only takes \~4mmHg PO2 to saturated myoglobin 50%
it takes 32mmHg PO2 to saturate hemoglobin 50%
lower affinity means that O2 comes off more easily
myoglobin used for O2 storage and isn’t used until O2 saturation of Hb is very low
myoglobin curve NOT cooperative, hyperbolic, has higher O2 affinity, lower P50, only has 1 binding site so cannot be cooperative
the greater P50 = O2 binding affinity is lower
hemoglobin has lower affinity for O2 than myoglobin
it only takes \~4mmHg PO2 to saturated myoglobin 50%
it takes 32mmHg PO2 to saturate hemoglobin 50%
lower affinity means that O2 comes off more easily
myoglobin used for O2 storage and isn’t used until O2 saturation of Hb is very low
52
New cards
factors that influence O2 binding affinity of Hb - 3
temperature:
* Hb has greater affinity for O2 at cooler temps
* temp high PO2 increases, binding affinity lower
* temp low, PO2 decreases, binding affinity higher
* slide 2 lect 30b
acidity:
* Bohr effect: reduction in binding affinity of Hb for oxygen as pH drops, effects of proton concentration on respiratory pigments
* significant because changes in blood PCO2 can indirectly affect O2 binding by changing blood pH
* high pCO2 at tissues enhances offloading of O2
* lower pH = lower O2 binding affinity
* atrial system O2 binding: high, more important because O2 is going to lung
* venous system O2 binding: lower, not as important because O2 is going to other tissues
* close to muscles/tissues: CO2 level is higher, pH low, binding affinity low, hemoglobin offloads more O2
* high PCO2 = more offloading
* average pH 7.2 < 7.4 < 7.6, death @6.8 + 7.8
organic phosphates:
* DPG: 2,3 diphosphoglycerate - naturally produced by erythrocytes by anaerobic glycolysis
* reduces binding affinity
* enhances O2 release
* binds near O2 binding site
* produced in response to low blood PO2
* improves offloading in tissues, not onloading in lung capillaries
* tries to provide more O2 to tissues
* inositol triphosphate - birds
* ATP - fish
* Hb has greater affinity for O2 at cooler temps
* temp high PO2 increases, binding affinity lower
* temp low, PO2 decreases, binding affinity higher
* slide 2 lect 30b
acidity:
* Bohr effect: reduction in binding affinity of Hb for oxygen as pH drops, effects of proton concentration on respiratory pigments
* significant because changes in blood PCO2 can indirectly affect O2 binding by changing blood pH
* high pCO2 at tissues enhances offloading of O2
* lower pH = lower O2 binding affinity
* atrial system O2 binding: high, more important because O2 is going to lung
* venous system O2 binding: lower, not as important because O2 is going to other tissues
* close to muscles/tissues: CO2 level is higher, pH low, binding affinity low, hemoglobin offloads more O2
* high PCO2 = more offloading
* average pH 7.2 < 7.4 < 7.6, death @6.8 + 7.8
organic phosphates:
* DPG: 2,3 diphosphoglycerate - naturally produced by erythrocytes by anaerobic glycolysis
* reduces binding affinity
* enhances O2 release
* binds near O2 binding site
* produced in response to low blood PO2
* improves offloading in tissues, not onloading in lung capillaries
* tries to provide more O2 to tissues
* inositol triphosphate - birds
* ATP - fish
53
New cards
CO2 binding affinity of Hb and total CO2 content in blood
how is CO2 in body as
Haldane effect
venous vs atrial
oxygenated vs deoxygenated Hb
how is CO2 in body as
Haldane effect
venous vs atrial
oxygenated vs deoxygenated Hb
CO2 in body as
1. dissolved gas (molecular) 5%>
2. bicarbonate (+ carbonate) \~90%
3. carbamino Hb \~5-10%
Haldane effect: deoxygenated blood in venous system contains more CO2 than arterial blood
venous system: has MORE CO2
atrial system: has LESS CO2
CO2 unloads rapidly in lungs where pCO2 is low
Hb that are fully oxygenated can carry less CO2 than deoxygenated Hb
1. dissolved gas (molecular) 5%>
2. bicarbonate (+ carbonate) \~90%
3. carbamino Hb \~5-10%
Haldane effect: deoxygenated blood in venous system contains more CO2 than arterial blood
venous system: has MORE CO2
atrial system: has LESS CO2
CO2 unloads rapidly in lungs where pCO2 is low
Hb that are fully oxygenated can carry less CO2 than deoxygenated Hb
54
New cards
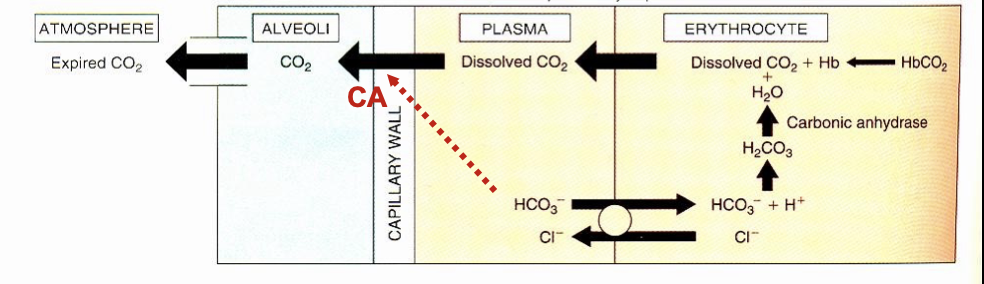
CO2 transport in tissue capillaries
CO2 produced in tissues → lungs
1. tissues: CO2 made
2. interstitial fluid: dissolved CO2
3. capillary wall
4. plasma: some CO2 remains dissolved
5. RBC: some remains dissolved, dissolved CO2 + Hb → HbCO2, dissolved CO2 + H2O + carbonic anhydrase = H2CO3 = H + HCO3
6. plasma: HCO3 passed from RBC to plasma, plasma \[Cl-\] sent to RBC, neutral cell charge
carbonic anhydrase in RBC not plasma
chloride shift: anion exchange, co-transport of Cl ion into RBC while bicarbonate moves into plasma, maintains electroneutrality, antiporter
consequence of chloride shift: Bohr effect
Bohr effect: transfer of bicarbonate out of the RBC to plasma raises H in RBC, decreases pH, helps offload O2 from Hb by reducing binding affinity
1. tissues: CO2 made
2. interstitial fluid: dissolved CO2
3. capillary wall
4. plasma: some CO2 remains dissolved
5. RBC: some remains dissolved, dissolved CO2 + Hb → HbCO2, dissolved CO2 + H2O + carbonic anhydrase = H2CO3 = H + HCO3
6. plasma: HCO3 passed from RBC to plasma, plasma \[Cl-\] sent to RBC, neutral cell charge
carbonic anhydrase in RBC not plasma
chloride shift: anion exchange, co-transport of Cl ion into RBC while bicarbonate moves into plasma, maintains electroneutrality, antiporter
consequence of chloride shift: Bohr effect
Bohr effect: transfer of bicarbonate out of the RBC to plasma raises H in RBC, decreases pH, helps offload O2 from Hb by reducing binding affinity
![CO2 produced in tissues → lungs
1. tissues: CO2 made
2. interstitial fluid: dissolved CO2
3. capillary wall
4. plasma: some CO2 remains dissolved
5. RBC: some remains dissolved, dissolved CO2 + Hb → HbCO2, dissolved CO2 + H2O + carbonic anhydrase = H2CO3 = H + HCO3
6. plasma: HCO3 passed from RBC to plasma, plasma \[Cl-\] sent to RBC, neutral cell charge
carbonic anhydrase in RBC not plasma
chloride shift: anion exchange, co-transport of Cl ion into RBC while bicarbonate moves into plasma, maintains electroneutrality, antiporter
consequence of chloride shift: Bohr effect
Bohr effect: transfer of bicarbonate out of the RBC to plasma raises H in RBC, decreases pH, helps offload O2 from Hb by reducing binding affinity](https://knowt-user-attachments.s3.amazonaws.com/044d921c58354c4cb87a4eab61810d15.jpeg)
55
New cards
CO2 transport in pulmonary capillaries
RBC → plasma → capillary wall → alveoli → atmosphere
1. RBC: HbCO2 → dissolved CO2 + Hb, HCO3 + H = H2CO3 = dissolved CO2 + H2O, Cl- moved to plasma
2. Plasma: HCO3 goes back to RBC to make dissolved CO2, Cl reenters plasma, dissolved CO2 from RBC enters,
3. lung capillary wall: dissolved CO2 passes, contain carbonic anhydrase which converts HCO3 → CO2
4. alveoli: CO2 released as gas to atmosphere
5. atmosphere: expired CO2
chloride shift: H2CO3 back to RBC, Cl back to plasma
lung capillaries are continuous and unique because they have carbonic anhydrase in endothelium which speeds up bicarbonate conversion
1. RBC: HbCO2 → dissolved CO2 + Hb, HCO3 + H = H2CO3 = dissolved CO2 + H2O, Cl- moved to plasma
2. Plasma: HCO3 goes back to RBC to make dissolved CO2, Cl reenters plasma, dissolved CO2 from RBC enters,
3. lung capillary wall: dissolved CO2 passes, contain carbonic anhydrase which converts HCO3 → CO2
4. alveoli: CO2 released as gas to atmosphere
5. atmosphere: expired CO2
chloride shift: H2CO3 back to RBC, Cl back to plasma
lung capillaries are continuous and unique because they have carbonic anhydrase in endothelium which speeds up bicarbonate conversion
56
New cards
CO2 bound to Hb
CO2 bound to Hb in RBC = carbamino Hb
hemoglobins affinity for CO2 is lower when O2 is bound = haldane effect
pulmonary capillaries uptake of O2 facilitation offloading of CO2
when HCO3 + H → CO2 + H2O, pH rises = O2 binding affinity rises
hemoglobins affinity for CO2 is lower when O2 is bound = haldane effect
pulmonary capillaries uptake of O2 facilitation offloading of CO2
when HCO3 + H → CO2 + H2O, pH rises = O2 binding affinity rises
57
New cards
how does the Haldane and Bohr effect work together with CO2
Bohr effect: pH drops, O2 binding affinity drops
Haldane effect: deoxygenated blood contains more CO2 than arterial blood
\
when bicarb converted to CO2, pH increases, which increases O2 binding affinity =Bohr effect
better O2 binding affinity = more oxygenated blood (contains less CO2 than arterial blood) = Haldane effect
Haldane effect: deoxygenated blood contains more CO2 than arterial blood
\
when bicarb converted to CO2, pH increases, which increases O2 binding affinity =Bohr effect
better O2 binding affinity = more oxygenated blood (contains less CO2 than arterial blood) = Haldane effect
58
New cards
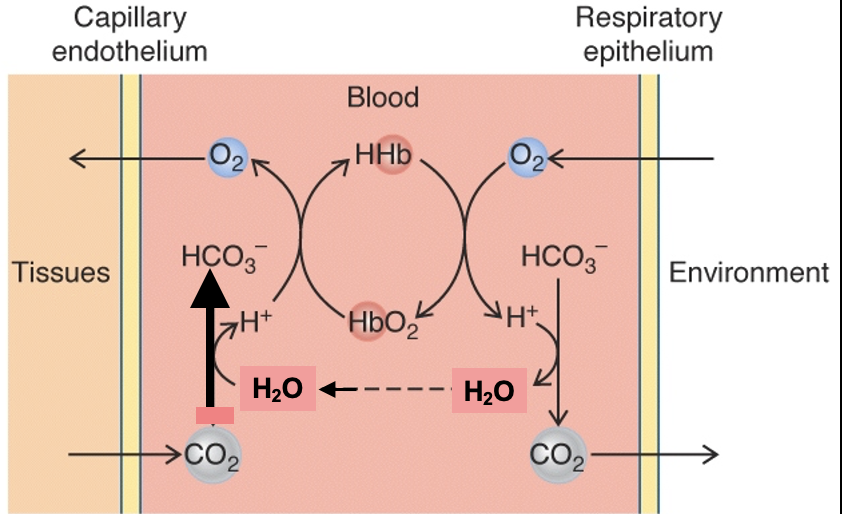
acidification and Hb and O2 and H
cycle of HHb, HbO2, tissues, blood, environment
cycle of HHb, HbO2, tissues, blood, environment
acidification is offset by the fact that H can bind directly to Hb and is displaced by O2
Hb acts as pH buffer in blood
O2 binding to Hb at respiratory surface facilitates formation of CO2
release of O2 from Hb in tissues facilitates formation of HCO3
Hb acts as pH buffer in blood
O2 binding to Hb at respiratory surface facilitates formation of CO2
release of O2 from Hb in tissues facilitates formation of HCO3
59
New cards
regulation of body pH
3 major influences on body pH (easy)
alkaline tide
3 major influences on body pH (easy)
alkaline tide
gas exchange is inherently linked to acid-base balance
major influences on body pH:
1. CO2 \*most important
2. ingested food: meats result in net uptake of acid, plant material net uptake of base
3. anaerobic metabolism: net acid production, metabolic acidosis
also can see changes in blood pH due to acid movement across fluid compartments: alkaline tide → acid transferred from blood to stomach after a large meal
major influences on body pH:
1. CO2 \*most important
2. ingested food: meats result in net uptake of acid, plant material net uptake of base
3. anaerobic metabolism: net acid production, metabolic acidosis
also can see changes in blood pH due to acid movement across fluid compartments: alkaline tide → acid transferred from blood to stomach after a large meal
60
New cards
respiratory disturbance
metabolic disturbances
metabolic disturbances
an abnormal alteration of the rate of CO2 elimination by lung/gill
respiratory acidosis: impaired exhalation of CO2
respiratory alkalosis: increased exhalation of CO2
\
metabolic disturbance: 1) altered blood bicarbonate concentration 2) numerous possible causes
* metabolic acidosis: loss of HCO3, increase H, in GI fluids or in saliva, anaerobic metabolism = lactic acid accumulation
* metabolic alkalosis: alkaline tide
\
pH can change based on respiration and metabolism
alkaline tide: after big meal, normal stomach pH acidic, meal increases pH, lots of protons pumped into stomach to maintain low stomach pH = metabolic alkalosis because protons are removed from the rest of the body
respiratory acidosis: impaired exhalation of CO2
respiratory alkalosis: increased exhalation of CO2
\
metabolic disturbance: 1) altered blood bicarbonate concentration 2) numerous possible causes
* metabolic acidosis: loss of HCO3, increase H, in GI fluids or in saliva, anaerobic metabolism = lactic acid accumulation
* metabolic alkalosis: alkaline tide
\
pH can change based on respiration and metabolism
alkaline tide: after big meal, normal stomach pH acidic, meal increases pH, lots of protons pumped into stomach to maintain low stomach pH = metabolic alkalosis because protons are removed from the rest of the body
61
New cards
summary of O2 binding affinity, CO2 transport, body pH
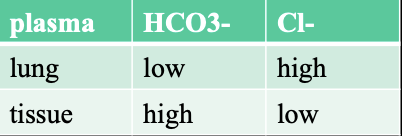
lung vs tissue levels of HCO3 and Cl in plasma (table)
lung vs tissue levels of HCO3 and Cl in plasma (table)
O2 binding affinity: temp, pH (Bohr), DPG, other gases
CO2 transport: bicarbonate and chloride levels, affinity of Hb for CO2 (Haldane effect), intracellular pH of RBC (Bohr)
body pH: CO2, HCO3, H+
around lung: CO2 removed, O2 onload high
around tissue: CO2 made, O2 offload high
CO2 transport: bicarbonate and chloride levels, affinity of Hb for CO2 (Haldane effect), intracellular pH of RBC (Bohr)
body pH: CO2, HCO3, H+
around lung: CO2 removed, O2 onload high
around tissue: CO2 made, O2 offload high
62
New cards
water and osmotic regulation
osmoregulators
conformeres
organs
osmoregulators
conformeres
organs
osmoregulators: maintain constant blood osmotic pressure regardless of ambient osmotic pressure
conformers: permit their blood osmotic pressure to match ambient osmotic pressure
osmoregulatory organs: kidney, extra-renal
nitrogeneous wastes
conformers: permit their blood osmotic pressure to match ambient osmotic pressure
osmoregulatory organs: kidney, extra-renal
nitrogeneous wastes
63
New cards
challenges in osmoregulation 2
3 types water - what is in each
electrolyte vs non
3 types water - what is in each
electrolyte vs non
1. retaining H2O - 3 types of water
1. intracellular fluid: majority of water in body, 28kg
2. interstitial fluid
3. blood plasma: 3kg
2. maintaining appropriate concentrations of solutes in extra/intra cellular compartments
\
major electrolyte: compound that dissociates into charged ions
plasma: Na, Cl
interstitial: Na, Cl
intracellular: K, HPO4, proteins
non electrolytes: glucose lipids
these influence osmolarity
64
New cards
factors affecting ion/water exchange 5
1. animal-environment gradient
* fresh water v salt water
2. surface-volume ratio
* smaller organisms desiccate more easily because small animal surface-area is larger
3. integument permeability
* integument = barrier = skin, insect cuticle
4. metabolic factors
* feeding and excretion rates and water (using O2 and making Co2 + H2O)
5. respiration
* loosing water as breathing in all air breathers
* nose temp is lower but higher than air
* warm air holds more water than cold air
* water vapor pressure in lungs is high
* breathing out: holding onto water vapor
* nose system holds water vapor good
* breathing through mouth = more water loss
65
New cards
water uptake
water output
water output
food 30%, drinking 60%, and metabolic water 10%
output per day: 60% urine, skin + lungs 28%, feces 4%, sweat 8%
metabolic water: C6H12O6 + 6O2 = 6CO2 + 6H2O
metabolic H2O production: lipids (most water produced - like migratory birds) > carb > protein w uric acid production > protein w urea production
marine animals: seals?
* eat invertebrates: skinner, more salts compared to fish, seals have to remove excess salt meaning it removes water too
* eat fish
output per day: 60% urine, skin + lungs 28%, feces 4%, sweat 8%
metabolic water: C6H12O6 + 6O2 = 6CO2 + 6H2O
metabolic H2O production: lipids (most water produced - like migratory birds) > carb > protein w uric acid production > protein w urea production
marine animals: seals?
* eat invertebrates: skinner, more salts compared to fish, seals have to remove excess salt meaning it removes water too
* eat fish
66
New cards
osmolarity + osmolars
measure of effective osmotic pressure of solutes in fluids, largely correlates with number of solute particles
non dissociable solutes: 1M = 1 Osm
dissociable solutes: must consider # charges when calculating
* NaCl (0.05M) → Na + Cl (2 x 0.05) = 0.1 Osm
* MgCl2 (0.05M) → Mg + 2Cl (3 x 0.05) = 0.15 Osm
non dissociable solutes: 1M = 1 Osm
dissociable solutes: must consider # charges when calculating
* NaCl (0.05M) → Na + Cl (2 x 0.05) = 0.1 Osm
* MgCl2 (0.05M) → Mg + 2Cl (3 x 0.05) = 0.15 Osm
67
New cards
water and salt physiology: cell-volume regulation
how hypertonic and hypotonic solutions affect cell volume
how to regulate cell-volume?
how to decrease osmolarity 2
how hypertonic and hypotonic solutions affect cell volume
how to regulate cell-volume?
how to decrease osmolarity 2
problems: need to maintain cell volume, hypotonic solution (solutes leave cell to maintain volume) and hypertonic solution (increase solutes in cell to maintain volume)
answer: organic solutes for cell-volume regulation
* increase organic solutes to maintain volume, will also increase Osm
\
crab - how to decrease osmolarity?
1. accelerating oxidation - AA can be metabolized (decreasing \[organic solutes\] decreases osm
2. transport of AA out of cells - removing organic compounds
answer: organic solutes for cell-volume regulation
* increase organic solutes to maintain volume, will also increase Osm
\
crab - how to decrease osmolarity?
1. accelerating oxidation - AA can be metabolized (decreasing \[organic solutes\] decreases osm
2. transport of AA out of cells - removing organic compounds
68
New cards
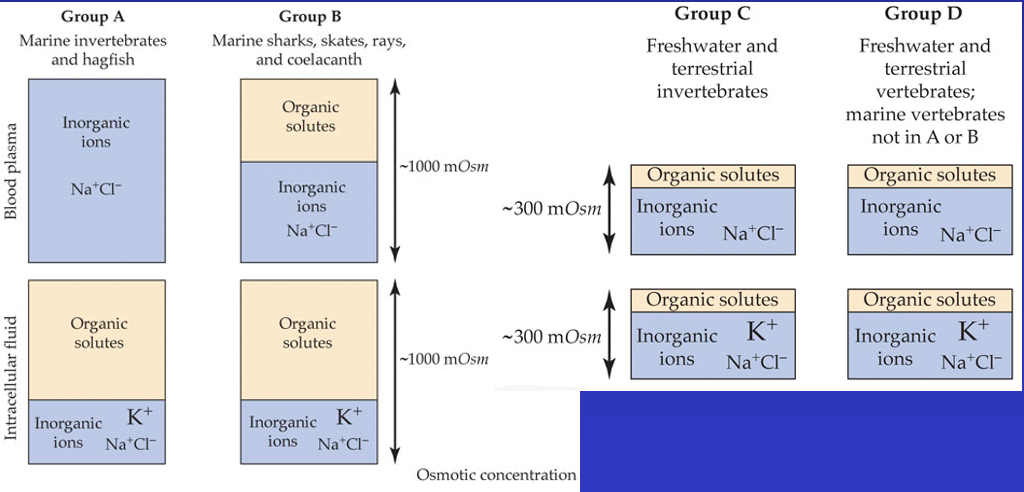
adjustment of intracellular osmotic pressure among animal groups ???? what is going on
all 4 groups are about the same in concentrations of inorganic ions in their intracellular fluids due to the contribution of organic solutes
group A: marine invertebrates and hagfish \~1000 mOsm each
* plasma = only inorganic ion - Na, Cl
* interstitial fluid = organic solutes, K, Na,Cl
group B: marine sharks, skates, rays, coelacanth \~1000 mOsm each
* blood plasma = organic solutes + Na Cl
* interstitial fluid = organic solutes and K, Na, Cl
group C: freshwater and terrestrial invertebrates \~300 mOsm each
* plasma: Na Cl > organic solutes
* interstitial fluid: K Na Cl > organic
* osmolarity is changing based on organic solutes
group D: freshwater and terrestrial vertebrates \~300 mOsm each
* plasma: Na Cl > organic solutes
* interstitial fluid: K Na Cl > organic
* osmolarity is changing based on organic solutes
group A: marine invertebrates and hagfish \~1000 mOsm each
* plasma = only inorganic ion - Na, Cl
* interstitial fluid = organic solutes, K, Na,Cl
group B: marine sharks, skates, rays, coelacanth \~1000 mOsm each
* blood plasma = organic solutes + Na Cl
* interstitial fluid = organic solutes and K, Na, Cl
group C: freshwater and terrestrial invertebrates \~300 mOsm each
* plasma: Na Cl > organic solutes
* interstitial fluid: K Na Cl > organic
* osmolarity is changing based on organic solutes
group D: freshwater and terrestrial vertebrates \~300 mOsm each
* plasma: Na Cl > organic solutes
* interstitial fluid: K Na Cl > organic
* osmolarity is changing based on organic solutes
69
New cards
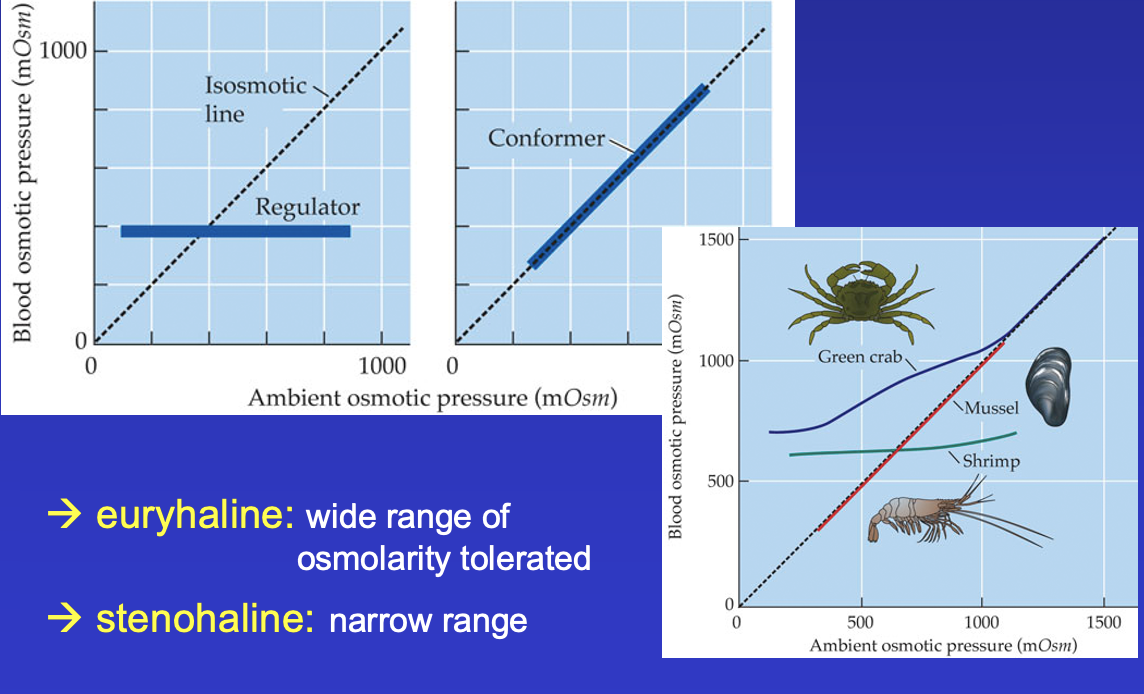
osmoconformers - types of animals
osmoregulators
euryhaline
stenohaline
osmoregulators
euryhaline
stenohaline
osmoconformers: marine invertebrates, follows isomotic line?
osmoregulators: teleosts, vertebrates, remains constant regardless of isosmotic line
some animals (green crab) can use both conformers and regulators depending on ambient osmotic pressure
euryhaline: wide range of osmolarity tolerated (green crab)
stenohaline: narrow range of osmolarity tolerated (shrimp, mussel)
osmoregulators: teleosts, vertebrates, remains constant regardless of isosmotic line
some animals (green crab) can use both conformers and regulators depending on ambient osmotic pressure
euryhaline: wide range of osmolarity tolerated (green crab)
stenohaline: narrow range of osmolarity tolerated (shrimp, mussel)
70
New cards
osmoconformers
elasmobranchs - how isotonic
elasmobranchs - how isotonic
hagfish osmotic concentration similar to sea water \~1000
lamprey osmotic concentration 300 much lower than sea water
elasmobranchs (sharks, rays, dogfish) blood salt is 1/3 that of sea water, but still isotonic due to TMAO and urea
extraosmolytes: Urea and TMAO, organic compounds
why both TMAO and Urea?
1. Urea in high concentrations can denature proteins, TMAO will stabilize them
2. often both made together
\
lamprey osmotic concentration 300 much lower than sea water
elasmobranchs (sharks, rays, dogfish) blood salt is 1/3 that of sea water, but still isotonic due to TMAO and urea
extraosmolytes: Urea and TMAO, organic compounds
why both TMAO and Urea?
1. Urea in high concentrations can denature proteins, TMAO will stabilize them
2. often both made together
\
71
New cards
osmoregulators
organs of osmotic reguation 3
organs of osmotic reguation 3
osmotic concentration closely regulated
teleosts live in marine/fresh water but all maintain similar blood osmolarity 300-400mOsm → regulated at organs
organs of osmotic regulation
1. gills: fish, aquatic
2. salt glands: marine reptiles, birds
3. kidneys: mammals, fish, birds
teleosts live in marine/fresh water but all maintain similar blood osmolarity 300-400mOsm → regulated at organs
organs of osmotic regulation
1. gills: fish, aquatic
2. salt glands: marine reptiles, birds
3. kidneys: mammals, fish, birds
72
New cards
osmotic regulation depends on U/P ratio
ratio when isosmotic
effects on water excretion, solute excretion, composition of blood plasma
ratio when isosmotic
effects on water excretion, solute excretion, composition of blood plasma
U/P ratio = urine concentration / plasma concentration
U/P = 1 isosmotic urine
U/P < 1 = diluted urine
U/P > 1 = concentrated urine
range human: 0.1-4 (40x difference)
\
effects on water excretion:
* diluted: water in urine > water in plasma
* concentrated: water in plasma > water in urine
effects on solute excretion:
* diluted: solutes in plasma > solutes in urine
* concentrated: solutes in urine > solutes in plasma
effects on composition of blood plasma:
* diluted: osmotic pressure of plasma increases
* concentrated: osmotic pressure of plasma decreases
U/P = 1 isosmotic urine
U/P < 1 = diluted urine
U/P > 1 = concentrated urine
range human: 0.1-4 (40x difference)
\
effects on water excretion:
* diluted: water in urine > water in plasma
* concentrated: water in plasma > water in urine
effects on solute excretion:
* diluted: solutes in plasma > solutes in urine
* concentrated: solutes in urine > solutes in plasma
effects on composition of blood plasma:
* diluted: osmotic pressure of plasma increases
* concentrated: osmotic pressure of plasma decreases
73
New cards
freshwater animals / teleost
2 different ways to regulate water and osmotic balance
how to avoid excess water
how to replace salts lost
2 different ways to regulate water and osmotic balance
how to avoid excess water
how to replace salts lost
1. hyperosmotic body fluids
2. gain H2O by osmosis, ionic loss by diffusion (via gills)
\
problem + solution
* to avoid excess water - dilute urine, no drink
* to replace salts lost - active uptake by chloride cells and pavement cells found in the fish gill epithelium
\
chloride cell: active Cl transport, Cl is anitported with HCO3, Cl in HCO3 out
pavement cell: antiported H with Na, active Na transport, Na in H out
74
New cards
ocean animals marine teleost
3 ways to replace water loss
how to remove uptaken salts
3 ways to replace water loss
how to remove uptaken salts
1. hyposmotic body fluids
2. loss of H2O by osmosis, ionic gain by diffusion
\
3 to replace water loss: drinking, H2O absorption in gut, concentrated urine
to remove up-taken salts: active secretion
75
New cards
marine reptiles and birds
idk how to do this
how to maintain hyposmotic blood to seawater
idk how to do this
how to maintain hyposmotic blood to seawater
confront problems of water loss (skin) and salt loading (by drinking and food uptake)
no concentrated urine
blood osmotic pressure much less than sea water
problem: maintaining hyposmotic blood to seawater?
solution: salt glands for osmotic and ionic regulation, salt glands found in head? ducts well arranged with capillaries, blood flow through capillaries, Na/K pump, Na and Cl pumped into secretory tubules
no concentrated urine
blood osmotic pressure much less than sea water
problem: maintaining hyposmotic blood to seawater?
solution: salt glands for osmotic and ionic regulation, salt glands found in head? ducts well arranged with capillaries, blood flow through capillaries, Na/K pump, Na and Cl pumped into secretory tubules
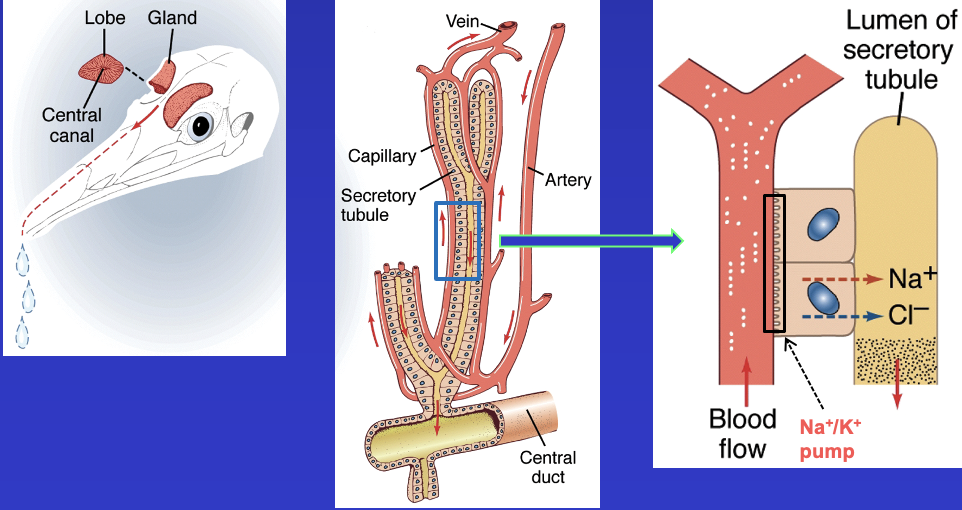
76
New cards
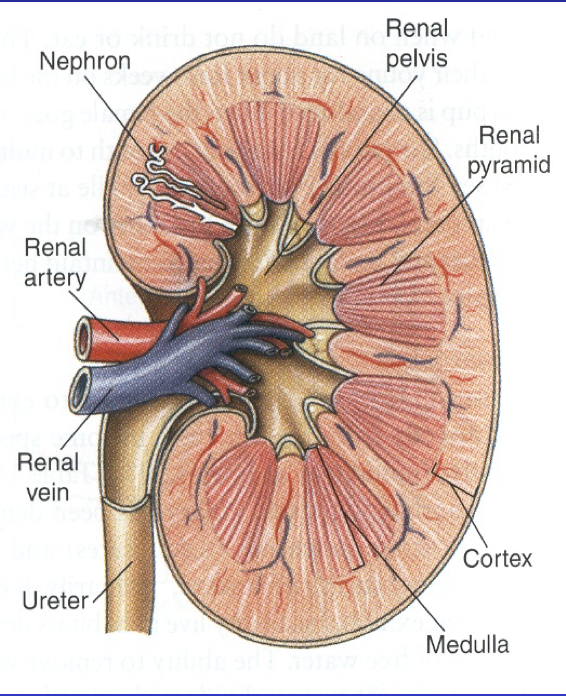
kidney structure picture - definitions
cortex: surrounds inner body of medulla, consists of Bowmans caupsules, beginning of collecting ducts, some tubule?
medulla: loops of Henle, collecting ducts
renal pyramid: lots of nephrons
renal pelvis
ureter: caries fluid from kidney to bladder
renal artery, vein
functional unit of kidney = nephron, makes urine
medulla: loops of Henle, collecting ducts
renal pyramid: lots of nephrons
renal pelvis
ureter: caries fluid from kidney to bladder
renal artery, vein
functional unit of kidney = nephron, makes urine
77
New cards
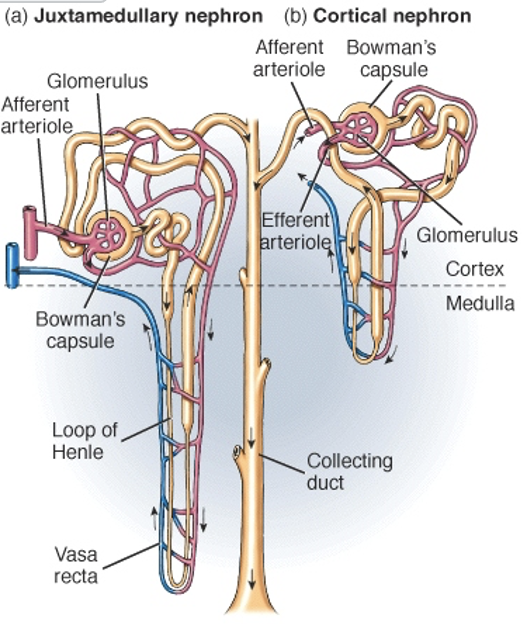
nephron
glomerulus + tubule
glomerulus: capillary clump surrounded by bowmans capsule, center of filtration
kidney tubule: 4 tubules
* proximal tubule
* loop of henle: thick and thin parts, long,
* distal tubule: collected to collecting duct
* collecting duct: where urine is found
* renal pelvis
cortical nephron: ??
glomerulus: capillary clump surrounded by bowmans capsule, center of filtration
kidney tubule: 4 tubules
* proximal tubule
* loop of henle: thick and thin parts, long,
* distal tubule: collected to collecting duct
* collecting duct: where urine is found
* renal pelvis
cortical nephron: ??
78
New cards
renal vasculature flow through
renal artery →
afferent arteriole
glomerular capillaries:
efferent arteriole
vasa recta
venules
renal vein
afferent arteriole
glomerular capillaries:
efferent arteriole
vasa recta
venules
renal vein
79
New cards
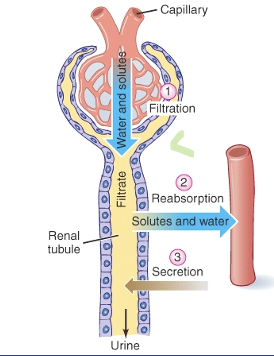
3 processed contribute to urine formation
amount secreted equation
amount secreted equation
filtration: ultrafiltration, large molecules unable to pass through, primary urine, through tubule
reabsorption: solutes and water
secretion
amount excreted = filtered + secreted - reabsorbed
fenestrated capillary
reabsorption: solutes and water
secretion
amount excreted = filtered + secreted - reabsorbed
fenestrated capillary
80
New cards
filtration
where is it
what is filtered, how much
filtration barriers
where is it
what is filtered, how much
filtration barriers
glomerulus
all constitutes of the blood except blood cells and proteins
15-25% of water and solutes (glucose + ions) in the plasma filtered
kidney filters 180L per day, 7.5 L per hour, blood is 5-6L, only 3L is plasma which is the true thing being filtered because RBC cannot be filtered
filtration barrier: 3 layers
1. glomerular fenestrated capillary endothelium
2. basement membrane
3. podocytes: filtration slits, control the amount filtered, regulated by AND, can “open and close”
all constitutes of the blood except blood cells and proteins
15-25% of water and solutes (glucose + ions) in the plasma filtered
kidney filters 180L per day, 7.5 L per hour, blood is 5-6L, only 3L is plasma which is the true thing being filtered because RBC cannot be filtered
filtration barrier: 3 layers
1. glomerular fenestrated capillary endothelium
2. basement membrane
3. podocytes: filtration slits, control the amount filtered, regulated by AND, can “open and close”
81
New cards
Flux across the glomerular capillaries formula
why pi bowman space = 0?
when flux is positive/negative
why pi bowman space = 0?
when flux is positive/negative
Flux (J) = blood pressure - osmotic pressure
J = (Pgc - Pbs) - 1(pi gc - pi bs)
GC = glomerular capillary
BS = bowman space
why pi bowman space = 0? because proteins are not filtered into the tubule so omsotic pressure is always 0
flux is + ? favor filtration
flux - ? not favor filtration
J = (Pgc - Pbs) - 1(pi gc - pi bs)
GC = glomerular capillary
BS = bowman space
why pi bowman space = 0? because proteins are not filtered into the tubule so omsotic pressure is always 0
flux is + ? favor filtration
flux - ? not favor filtration
82
New cards
resistance of afferent and efferent arterioles
influence __?
RAA and REA
influence __?
RAA and REA
resistance of afferent and efferent arterioles **influence filtration rate**
increasing diameter of afferent art. increases globular pressure
AA: blood coming to center = glomerulus + bowman space
EA: blood going away from center
resistance AA increase? less blood to glomerulus = decreased filtration
resistance AA decrease? filtration increases
REA increase? filtration increases, vasoconstriction, because less blood is leaving capillary = more blood staying in glomerulus = filtration high
increasing diameter of afferent art. increases globular pressure
AA: blood coming to center = glomerulus + bowman space
EA: blood going away from center
resistance AA increase? less blood to glomerulus = decreased filtration
resistance AA decrease? filtration increases
REA increase? filtration increases, vasoconstriction, because less blood is leaving capillary = more blood staying in glomerulus = filtration high
83
New cards
glomerulus filtration rate
def
how to measure it
high GFR = ?
input, output
def
how to measure it
high GFR = ?
input, output
how much blood is filtered in a given time
also establishes rates of other processes like secretion and reabsorption
GFR high = kidney function is high
measure GFR:
* measure clearance of molecule that is filtered but NOT reabsorbed or secreted (inulin)
* renal clearance: volume of plasma from which a substance is completely removed per time
* blood = input, urine = output
* inulin polysacc from plants cannot use it so only filtered out
* Liters per hour
also establishes rates of other processes like secretion and reabsorption
GFR high = kidney function is high
measure GFR:
* measure clearance of molecule that is filtered but NOT reabsorbed or secreted (inulin)
* renal clearance: volume of plasma from which a substance is completely removed per time
* blood = input, urine = output
* inulin polysacc from plants cannot use it so only filtered out
* Liters per hour
84
New cards
clearance of inulin - idk this
inulin clearance = U\[inulin\] x Vu / P\[inulin\] = GFR
inulin clearance = urine inulin concentration x urine volume / plasma inulin concentration
if clearance of substance < GFR, substance is REABSORBED
if clearance of substance > GFR, substance is SECRETED
inulin clearance = urine inulin concentration x urine volume / plasma inulin concentration
if clearance of substance < GFR, substance is REABSORBED
if clearance of substance > GFR, substance is SECRETED
85
New cards
filtered load, % reabsorbed, % water reabsorbed
other things to calculate if Vu and plasma and urine concentrations known
filtered load of a compound: Pion x GFR (amount filtered from plasma in mg or moles per hour)
% ion reabsorbed = filtered load - excreted load / filtered load
% water reabsorbed = GFR - Vu / GFR
* majority of water will be reabsorbed, 180L water filtered through but average 1L urine / day
urinary excretion rate = Uion x Vu
filtered load of a compound: Pion x GFR (amount filtered from plasma in mg or moles per hour)
% ion reabsorbed = filtered load - excreted load / filtered load
% water reabsorbed = GFR - Vu / GFR
* majority of water will be reabsorbed, 180L water filtered through but average 1L urine / day
urinary excretion rate = Uion x Vu
86
New cards
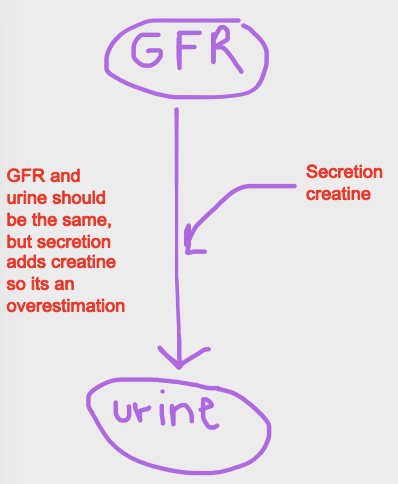
clearance of creatinine v inulin
lnulin must be injected to determine GFR
clinically easier to use creatine to estimate GFR
creatinine is filtered + small amount secreted
over or underestimation of GFR with small secretion of creatinine? overestimation because GFR and urine vole. should be the same but secretion adds creatine into urine os its an overestimation
clinically easier to use creatine to estimate GFR
creatinine is filtered + small amount secreted
over or underestimation of GFR with small secretion of creatinine? overestimation because GFR and urine vole. should be the same but secretion adds creatine into urine os its an overestimation
87
New cards
tubular reabsorption
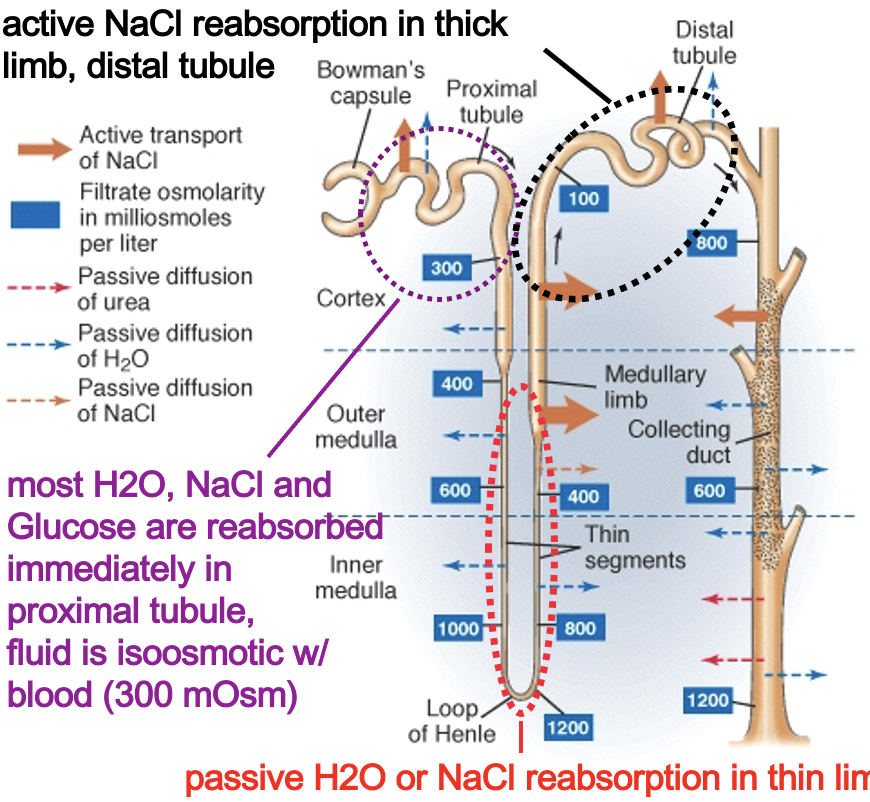
proximal tubule: major reabsorption site, very isosmotic, selective reabsorption, equal osmolarity to blood, most H2O, NaCl and glucose are reabsorbed immediately here, energy required
distal tubule: active NaCl reabsorption in thick limb
loop of Henle: passive H2O and NaCl reabsorption in thin limb, max osmolarity 1200, because of reabsorption filtrate reaching Loop of Henle contains little glucose or amino acids,
nephron structural unit of kidney
proximal tube is 300 osmolarity which is equal to the blood
urine can be diluted 10x than normal (300 → 30)
urine can be concentrated 4x than normal (300 → 1200)
40x range in concentration/dilution of urine
wide range of urine concentration
distal tubule: active NaCl reabsorption in thick limb
loop of Henle: passive H2O and NaCl reabsorption in thin limb, max osmolarity 1200, because of reabsorption filtrate reaching Loop of Henle contains little glucose or amino acids,
nephron structural unit of kidney
proximal tube is 300 osmolarity which is equal to the blood
urine can be diluted 10x than normal (300 → 30)
urine can be concentrated 4x than normal (300 → 1200)
40x range in concentration/dilution of urine
wide range of urine concentration
88
New cards
what is reabsorption driven by
active transport of Na
89
New cards
reabsorption and active Na transport
Na,K,Cl,glucose,water
Na,K,Cl,glucose,water
1. water: passive, follows Na, Cl, glucose
2. glucose transferred by cotransporters with Na into the epithelium, secondary active transporter
3. K goes into epithelial cell, concentration is high, K leaves to blood where \[K\] is low
4. Cl maintains electroneutrality and leaves tubular fluid to blood
5. NaK pump: uses ATP, active, tubular fluid to blood = reabsorption, \[Na\] inside epithelium is low, Na cotransported with HCO3
\
density of cotransporters on lumenal side can limit reabsorption - the more transporters = more reabsorption
![1. water: passive, follows Na, Cl, glucose
2. glucose transferred by cotransporters with Na into the epithelium, secondary active transporter
3. K goes into epithelial cell, concentration is high, K leaves to blood where \[K\] is low
4. Cl maintains electroneutrality and leaves tubular fluid to blood
5. NaK pump: uses ATP, active, tubular fluid to blood = reabsorption, \[Na\] inside epithelium is low, Na cotransported with HCO3
\
density of cotransporters on lumenal side can limit reabsorption - the more transporters = more reabsorption](https://knowt-user-attachments.s3.amazonaws.com/033599bfb16141ff8d8ff1de57c771bf.jpeg)
90
New cards
reabsorption limited by transport maximum for each substance - glucose
normally: glucose filtered, 100% reabsorbed
Pglucose: 1 mg/ml
Tm glucose: 320 mg/min
\
Diabetic:
Pglucose > 2mg/ml, 200mg/ 100ml
> Tm, glucose excreted
\
glucose in urine = bad = diabetic
Pglucose: 1 mg/ml
Tm glucose: 320 mg/min
\
Diabetic:
Pglucose > 2mg/ml, 200mg/ 100ml
> Tm, glucose excreted
\
glucose in urine = bad = diabetic
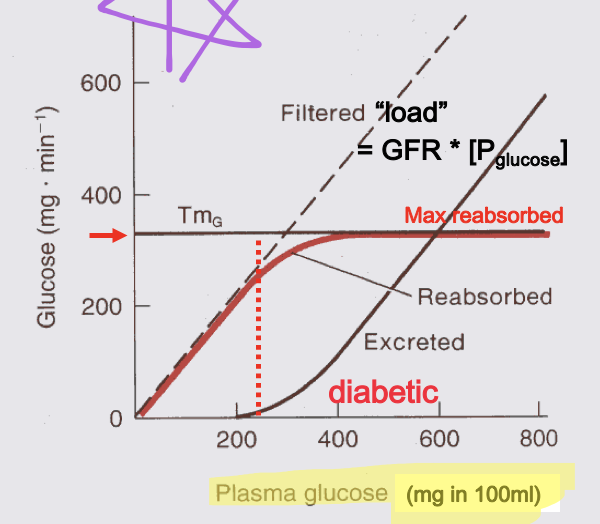
91
New cards
tubular secretion
2 major reasons why
2 major reasons why
gets rid of excess K
* why high K bad? muscles are contracting too much and cause problems = overexcitation
* K in interstitial fluid must be removed
H HCO3 NH3 for acid base balance
toxins:drugs, conjugated to organic acids, enter tubule via transporters, can’t diffuse back into blood due to high polarity
occurs mostly in distal tubules (except for H secretion) most other ions decrease steadily as they are reabsorbed
K in filtrate rises in distal and collecting ducts
* why high K bad? muscles are contracting too much and cause problems = overexcitation
* K in interstitial fluid must be removed
H HCO3 NH3 for acid base balance
toxins:drugs, conjugated to organic acids, enter tubule via transporters, can’t diffuse back into blood due to high polarity
occurs mostly in distal tubules (except for H secretion) most other ions decrease steadily as they are reabsorbed
K in filtrate rises in distal and collecting ducts
92
New cards
K is example of compound that is filtered, reabsorbed AND secreted
too high plasma K can cause muscle convulsions
proximal tubule: K absorbed via passive cotransporters driven by basolateral Na/K ATPase that drives glu, Na and H2O absorption, tubular fluid → blood
distal tubule: excess K secreted by reverse process, blood → tubular fluid
proximal tubule: K absorbed via passive cotransporters driven by basolateral Na/K ATPase that drives glu, Na and H2O absorption, tubular fluid → blood
distal tubule: excess K secreted by reverse process, blood → tubular fluid
93
New cards
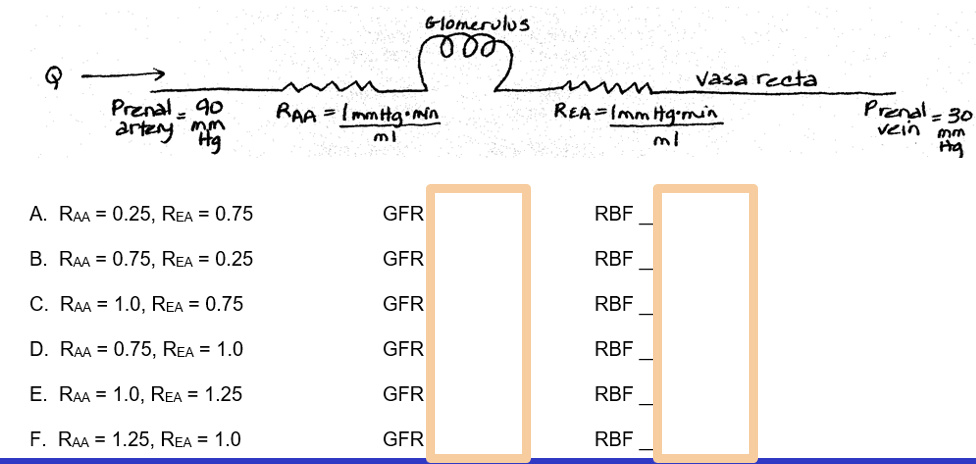
renal blood flow
glomerulus flow rate
glomerulus flow rate
renal blood flow
glomerulus flow rate
glomerulus flow rate
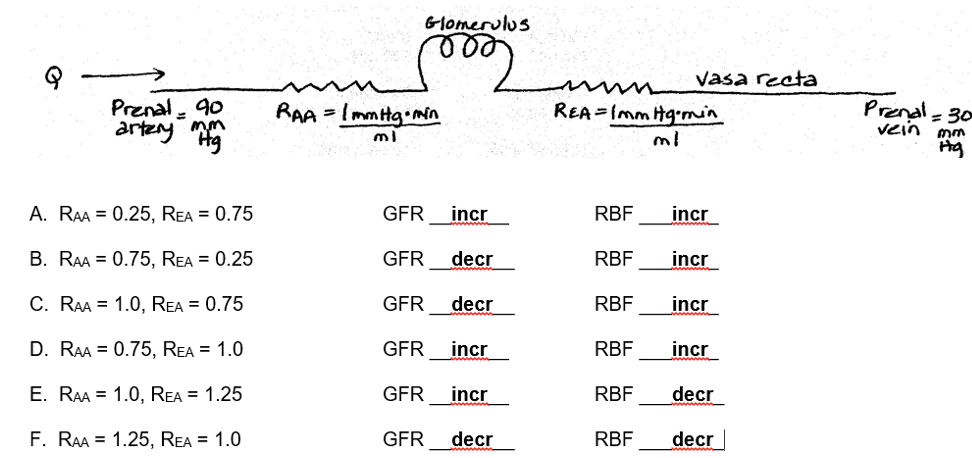
94
New cards
how is urine concentrated?
what limbs do
what vasa recta do
what limbs do
what vasa recta do
Loop of Henle
function asymmetry ascending and descending limbs
selective permeability in different parts of the tubule
standing osmotic gradient in renal medulla
function asymmetry ascending and descending limbs
selective permeability in different parts of the tubule
standing osmotic gradient in renal medulla
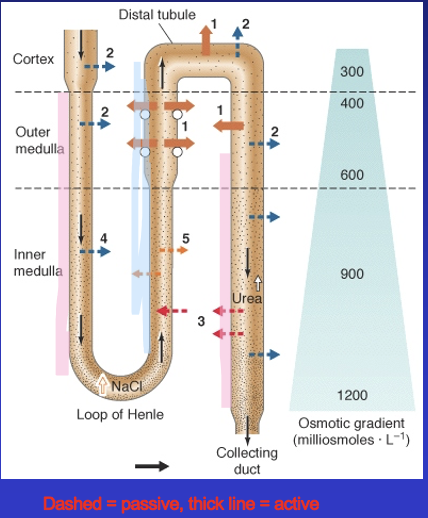
95
New cards
corticomedullary osmotic gradient
maintained by
where is highest salt content, highest osmolarity
maintained by
where is highest salt content, highest osmolarity
gradient maintained by absorption of NaCl from loop of Henle urea from collecting duct
cortical nephron
medulla area has high salt content, high osmolarity
\
cortical nephron
medulla area has high salt content, high osmolarity
\
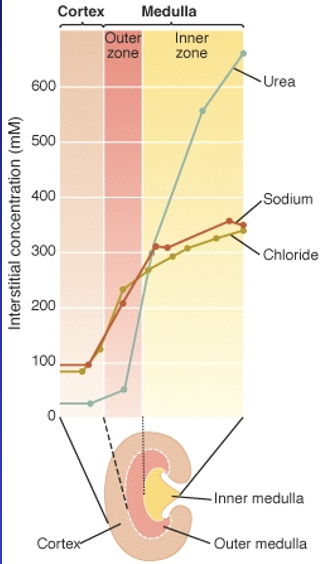
96
New cards
Loop of Henle establishes NaCl gradient in medullary interstitum
2 functions of Loop of Henle
2 functions of Loop of Henle
asymmetry of H2O and NaCl permeability in Loop allows it to work as a countercurrent multiplier
2 functions: 1) establish standing osmotic gradient 2) maintain standing osmotic gradient
how is the standing osmotic gradient established? by countercurrent multiplier function
2 functions: 1) establish standing osmotic gradient 2) maintain standing osmotic gradient
how is the standing osmotic gradient established? by countercurrent multiplier function
97
New cards
how is a countercurrent multiplier working
pumping → equilibriate → fluid advanced → repeat
Active reabsorption of NaCl
Juxtamedullary nephron
Water leaves descending passively following the ions that leave the ascending
Ascending limb and interstitial fluid wants to maintain a 200mOms difference
Descending limb wants to be equal the osmolarity as interstitial fluid Increasing osmolarity as loop of henle the deeper into the medulla
Counter current multiplication: enables the effects of the gradient to increase (started with 300 and goes up to 700, but actually gets to 1200.. How? Urea on slide 6?)
Active reabsorption of NaCl
Juxtamedullary nephron
Water leaves descending passively following the ions that leave the ascending
Ascending limb and interstitial fluid wants to maintain a 200mOms difference
Descending limb wants to be equal the osmolarity as interstitial fluid Increasing osmolarity as loop of henle the deeper into the medulla
Counter current multiplication: enables the effects of the gradient to increase (started with 300 and goes up to 700, but actually gets to 1200.. How? Urea on slide 6?)
98
New cards
single effect
The difference produced by use of metabolic energy between adjacent parts of the two oppositely flowing fluid streams in a countercurrent multiplier system
Stannding osmotic gradient is established and maintained, once gradient is established you don’t need to establish again because it should be maintained as you live
Stannding osmotic gradient is established and maintained, once gradient is established you don’t need to establish again because it should be maintained as you live
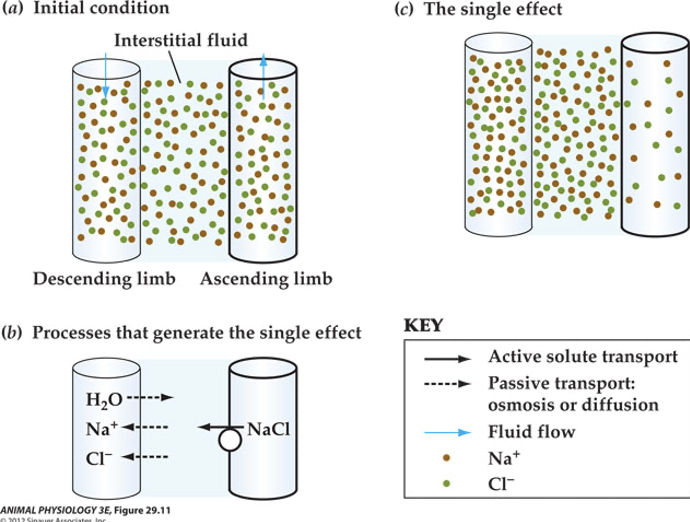
99
New cards
collecting duct
Lower portion of collecting duct also permeable to urea
high concentrations in filtrate cause urea to diffuse out into inner medulla interstitium near base of collecting duct
responsible for additional 500-600mOsm in the standing gradient
high concentrations in filtrate cause urea to diffuse out into inner medulla interstitium near base of collecting duct
responsible for additional 500-600mOsm in the standing gradient
100
New cards
final step in urine concentration
As filtrate flows down collecting duct, water diffuses into interstitium, depending on duct permeability
If H2O conservation is needed, ADH (antidiuretic hormone) opens water channels, H2O is absorbed, concentrated urine is produced
if H2O conservation not needed, duct (CD) remains impermeable water = dilute urine
top to bottom concentration gradient
side to side gradient is equivalent
If H2O conservation is needed, ADH (antidiuretic hormone) opens water channels, H2O is absorbed, concentrated urine is produced
if H2O conservation not needed, duct (CD) remains impermeable water = dilute urine
top to bottom concentration gradient
side to side gradient is equivalent