Adults II exam 1 review
1/162
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
163 Terms
High-Acuity Definition
Refers to complex patients with unpredictable outcomes, often found in critical care or intensive care units.
What factors Contribute to High-Acuity Admissions
Includes acute issues (trauma, stroke, aneurysm), age (really young and really old), exacerbation of chronic conditions (HF, kidney disease, DM, COPD), lack of access to care, economic factors, and noncompliance.
Nursing Care Considerations
Care must be individualized due to diverse cultural and educational backgrounds of clients and families.
What are the major areas to consider when caring for high-acuity patients?
High-acuity environment
Pharmacological management and issues
Nutritional support
Older adult considerations
Palliative and end of life care
High-Acuity Environment - The Good
Features rapid access to labs, specialists, 24-hour care, and quick medication access.
High-Acuity Environment - Not So Good
Characterized by overcrowding, excessive equipment, information overload, and limited communication.
Physical Stressors in High-acuity environments Environments
Include lack of sleep, isolation, pain, immobility, overstimulation, and pharmacological effects (sedatives, antipsychotics)
Social and Psychological Stressors in High-acuity environments
Encompasses anxiety, grief, family dynamics, financial stress, and post-stay concerns.
Common Complications from Stressors
Include venous thromboembolism (VTE) due to lack of mobility, GI bleed, and delirium.
How are the common stressors treated?
VTE: prophylaxis, anticoagulants, compression stockings, sequential devices
GI bleed: PPI for stress prophylaxis
Delirium: address the main issue
Delirium
An acute disorder marked by confusion, attention deficits, and fluctuating mental status, often misinterpreted stimuli. Developed QUICKLY
What are common causes of delirium?
Infectious process, adverse drug reactions, metabolic conditions, lack of sleep
Delirium Assessment and Treatment
Involves identifying and treating underlying causes, with prevention as the primary goal.
Why are antipsychotics the last resort for treatment of deliurm?
Meds like Haldol and benzos can have dangerous side effects
Nurse’s Role in Facilitating Care
Involves acknowledging stressors, assessing clients, managing stressors, and connecting to resources.
Areas for Pharmacological Management
Areas that deal with pain, sedation, chronic and acute illness management.
Pain in High-Acuity Clients
Can be acute or chronic, with varying perceptions influenced by psychosocial factors.
Common Pain Assessment Tools
Include numeric pain scale, FACES, Behavioral Observation Scale, and Critical Care Pain Observation Tool.
What’s the most reliable way to assess pain?
Patient report
Pain Management
Involves using opioids and non-opioids, with a focus on managing anxiety to alleviate pain.
Nurse’s Role in Pain Management
Includes frequent assessment, advocacy for pain control, look into potential side effects and complications, and education for clients and families (narcotic hesitancy)
High-Acuity Client Pain Management Complications
Include respiratory depression, altered consciousness, and polypharmacy.
Sedation for High-Acuity Clients
Commonly used in critical care, especially for ventilated patients or to manage delirium.
Common Sedation Assessment Tools
Include Richmond Agitation and Sedation Scale (RASS) and Pasero Opioid-Induced Sedation Scale (POSS).
Nutritional Support Importance
Essential for recovery, with many high-acuity clients unable to take in nutrition independently.
What complications can occur from sedation to high-acuity patients?
Long-term PTSD, increased delirium, resp distress, and drug interactions
Routes of Nutrition
Include oral, enteral, and parenteral feeding methods.
Why do high acuity patients usually have special nutritional needs?
D/t disease processes like liver failure, renal failure, and heart failure
Nurse’s Role in Nutritional Delivery
Involves checking orders, maintaining feeding tubes, and assessing for intolerance.
What are key notes to make for oral feedings for high-acuity patients?
Preferred method
Helps body maintain normal process
Always assess client’s readiness to feed
May require supplementation d/t lack of energy/appetite (Ensure drink for a calorie dense diet)
What are key notes to make for enteral/tube feedings for high-acuity patients?
Different tubes have different functions
Nasogastric tube (NG): down the nare, esophagus, stomach
Dobhoff tube: goes down nare, esophagus, stomach, and intestine
PEG tube: directly through the abd wall into the stomach
They help maintain GI function and reduce metabolic stress
Helps with inflammatory bowel disorders
What are key notes to make for parenteral feedings for high-acuity patients?
Last resort for feeding. Commonly seen in patients with pancreatitis
TPN is the most common, but poses a high risk for infection (change every 24-72 hrs)
Taper d/t risk of hypo/hyperglycemia
Why must TPN be tapered on and off?
To prevent hyper/hypoglycemia
Older Adult High-Acuity Client Considerations
Focus on physiological changes, atypical presentations, comorbidities, and cognitive changes.
What are expected system changed in older adult clients?
Neuro: decreased neurotransmitter production, permeable BBB, dilation of ventricles
Cardio: decreased elasticity and increased stiffness of walls
Resp: calcification of costal cartilage, decreased chest wall compliance, decreased RBCs O2 carrying capacity, loss of lung elasticity
GI: decreased saliva, thirst response, Lower Esophageal Sphincter function, digestive function, GI tract absorption, decreased blood flow to liver
GU: decreased GFR, creatinine clearance, UTI risk, incontinence
Integ: loss of elasticity, decreased subq tissue, thinning of skin, fragile blood vessels, reduction of lean body mass
Musculo: decreased muscle mass, joint stiffness, decreased mobility, loss of bone mass
What can extreme confusion indicate in older adults?
UTI
What are some pharmacological considerations that nurses should consider when caring for older clients?
Physiological changes like decreased absorption and liver and kidney changes
Polypharmacy
Adverse reactions that certain drugs can cause. Like delirium, hypotension, renal or hepatic impairment
Palliative Care
An interdisciplinary approach aimed at relieving suffering and improving quality of life without withdrawing care. Ex. cancer, HF, dementia
Hospice Care
A form of palliative care for patients with a prognosis of six months or less to live.
End of Life Care
Focuses on comfort and support during the final phase of a patient’s illness. Clients can receive both hospice and palliative care
Withdrawal of Care
Involves stopping life-supporting measures (dialysis, ventilator support, vasopressor support), often accompanied by medications to ease symptoms.
Bereavement and Grief
Each person experiences these differently; nurses facilitate and normalize the process for families.
Self-Care in High-Acuity Environment
Caregivers must prioritize their well-being and seek help to process their feelings.
How is body perfusion measured?
Cardiac Output (CO)
How does blood flow through the heart?
■ Return through IVC and SVC
■ RA through TCV to RV
■ RV through PV out the PA
■ O2-CO2 exchange in lungs
■ Back by PV to LA
■ Through MV to LV
■ Through AV and out the Aorta
■ Systemic perfusion
What is CO? stroke volume? heart rate?
CO: amount of blood ejected by each ventricle per minute. Normal is 5-6L/min
Stroke volume: volume of blood pumped with each beat (contraction of the ventricle) so it depends on the contractility of the heart and end-diastolic volume
Heart Rate: # of times the heart beats per min
What’s the equation of CO?
CO = SV*HR
What factors affect CO (HR, SV)?
HR
SNS and PSNS can either lead to tachy which increased CO or induces relaxation whcih decreased CO
Positive chronotropes (epinephrine, atropine) increase HR which increased CO and negative chronotropes (beta blockers) decrease HR
Dysrhythmias
SV
Preload, Afterload, and Contractility affected SV which affects CO
What are preload, afterload, and contractility?
Preload: blood volume entering the ventricle after they’ve filled up. Affected by venous return, volume, or Afib
Afterload: pressure ventricles undergo to pump blood out of the ventricle. Affected by HTN (increased pressure to heart), atherosclerosis/blockages (narrowing of vessels affected blood flow), vasoconstriction
Contractility: strength of heart during a contraction, so if it’s decreased, so will CO
What does CO compensation look like?
Increased HR
The body will try to maintain the SV, but compensation will fail with sustained increase in HR and SV will drop
Decreased SV
HR will increase. Ex. hypovolemia
Increased SV
HR will decrease as is noted in endurance athletes
What are modifiable RFs of cardiovascular issues?
Smoking: causes vasoconstriction which decreases CO
HTN
Hyperlipidemia: plaque build up
Inactivity
Obesity
Diabetes
What are common manifestations of cardiovascular issues?
■ Neuro: Lethargy, dizziness, altered LOC, syncope (not enough blood/oxygen to brain)
■ CV: hypotension, weak and thready pulse (body is going to perfuse the main organs), angina, edema
■ Resp: Dyspnea (fluid accumulation), tachypnea
■ GI: Nausea
■ GU: oliguria (no kidney perfusion) this is usually the first system affected
■ Integ/Musc: cool, clammy skin, possible diaphoresis (d/t increased heart workload)
■ Psychosocial: anxiety
What do labs show with cardiovascular issues?
■ Total cholesterol: elevated levels increase risk of plaque formation leading to lack of perfusion
■ Triglycerides
■ Chemistry panel: gives info on the contractility of the heart. Focus is on potassium, calcium, and magnesium
■ CBC: look at Hgb or Hct to determine oxygen-carrying capacity of blood
■ BNP: enzyme released when the body senses a large stretch in the artery. Increased levels show individuals dealing with fluid overload
■ Cardiac Enzymes: enzymes released when there’s muscle damage
What diagnostics are taken to determine cardiovascular issues?
■ EKG/ECG: look at electrical conduction of the heart
■ Echocardiogram: ultrasound of the heart showing the structure of the heart and measuring the output of the different ventricles, see valve function
■ Cardiac stress test: look at ECG reading to determine changes in heart rhythm
■ Calcium scan: helps identify plaques or hardening in the heart usually in coronary arteries
■ Cardiac catheterization
■ Chest X-ray
What is the purpose of cardiac catherization?
It allows for blood flow to be restored, usually d/t an obstruction in the coronary artery
What are the different techniques of cardiac catherization?
Percutaneous Transluminal Coronary Angioplasty (PTCA): balloon that widens the artery
Directional Coronary Atherectomy (DCA): digs plaque out of artery
Intracoronary Stents: most common and has stents widen the artery
Coronary Artery Bypass Graft (CABG): alternate cath in case obstruction is too big
What allergy should the nurse be on the look out for if a patient is going through cardiac catherization?
iodine/shellfish
What are the main things to observe in a patient following a cardiac cath procedure?
VS q15min then q30min, then q1hr
Check for bleeding
Make sure patient lays flat following a femoral artery procedure
Check site distal to cath insertion for sensation
Check for adequate perfusion (LOC, BP, UOP, cap refill)
Monitor weight for retention
What does nursing care for a CABG patient look like?
ICU right after surgery with chest tubes (monitor Output)
Check sugar, chem panels, and other tests
What does nutrition for a patient with cardiovascular issues look like?
Low saturated fat, high complex carb diet
High fiber
Possible fluid or sodium retention
Diabetes control
Reduced alcohol d/t risk of cardiomegaly
No smoking
What is Coronary Artery Disease (CAD)?
Deposition of lipids that cause narrowing of arteries IN THE HEART
What’s the patho of CAD?
Damage to the tunica intima allows for lipids to deposit into the wall forming a plaque.
The plaque attracts more lipids which further narrows the vessel. If the plaque gets thick enough, the tissue distal to it gets less perfused and can ultimately lead to tissue ischemia.
Additionally, piece of the plaque can break off and become a clot/thrombus that can further occlude vessels further down and lead to tissue death
Why does location matter when discussing CAD?
The higher the occlusion the more dangerous it is since it determines how much of the vessel doesn’t get perfused
What are manifestations of CAD?
■ Neuro: Fatigue
■ CV: Angina possible
■ Resp: SOB
■ Other: There are often not many manifestations until there is a severe compromise, especially if the plaque has built slowly over time.
What labs are done with CAD?
C-reactive protein: for inflammation
Total cholesterol: determines lipid deposit
LDL (bad)
HDL (good)
Triglycerides
What diagnostics are done for CAD?
EKG: determines if the occlusion is severe enough to cause ischemia
Echocardiogram: look at function of heart, not show occlusions (TEE or TTE)
Doppler flow: looks for occlusions in arteries
Stress Test: determine abnormalities in the EKG
Angiogram: cath placed to visualize a reduction of flow in the arteries
Coronary artery calcium scan: determine calcification of arteries
How is CAD managed?
Meds
“__statin” to lower lipid levels
Niacin to lower LDL
Antiplatelet/coagulant therapy for clots
Cardiac cath or CABG
Low fat, high fiber diet
No need for sodium restriction
What is angina pectoris?
Pain in the chest d/t the heart needing more oxygen than it’s getting
What’s the patho of angina pectoris?
An underlying disease causes the myocardial oxygen demand to exceed the supply available, so the tissue becomes ischemic since it’s not being properly perfused
This ischemia of tissues triggers pain usually around the chest region
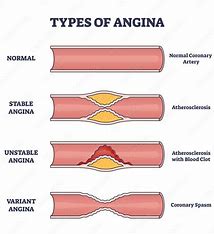
What are the 3 types of angina?
Stable
Caused by a PREDICTABLE emotion or exertion
Plaque is fixed and stable
Relieved by rest, nitroglycerin, or both
Unstable
Caused by an UNPREDICTABLE emotion or exertion
Pain is d/t further platelet aggregation and usually occurs at night
Not relieved with rest or nitro and is considered a medical emergency
Variant (Prinzmetal’s)
Caused by CORONARY ARTERY SPASM during rest periods or randomly
No plaque build up, but the spasms narrow the vessel
Oftens occurs durinf times of rest (at night)
Related to stimulant use (cocaine) and can show elevated ST on an EKG
What can cause angina?
Decreased O2 supply
CAD, coronary artery spasms, dysrhythmias, anemia, severe resp disease, substance use
Increased O2 demand
Tachycardia, valvular disease, anxiety, hyperthermia, physical exertion
What are manifestations of angina?
■ Neuro: Lethargy, dizziness, altered LOC, syncope
■ CV: hypotension, weak and thready pulse (vasoconstriction), angina, tachycardia
■ Resp: SOB, tachypnea (to meet O2 demand)
■ GI: Nausea, vomiting
■ GU: oliguria
■ Integ/Musc: cool, clammy skin, possible diaphoresis
■ Psychosocial: anxiety
■ Pain-can be located in the chest, back or other areas of the torso. Can also have variations in severity and duration depending on the individual
What labs are taken for angina?
Cardiac enzymes
Troponin (MOST INDICATIVE)
CK
CK-MB
Myoglobin
CBC: RBCs and WBCs
CRP: inflammation
Chem panel: Mg, K, Ca
How is angina diagnosed?
EKG: ST depression or T inversion with ischemia
Echo: visualize ventricles and chambers of the heart
Stress Test, Calcium Scan, Cardiac cath, angiography, chest x-ray
How is angina treated?
Meds
Nitro: vasodilator that opens up arteries to increase flow. Monitor BP
“__pril”: ACE inhibitor
“__olol”: beta blockers decrease HR to decrease O2 demand
Nifedipine, verapamil: CCBs to regulate spasms
“__statins”: lipid lowering agent
ASA, heparin, warfarin: anticoagulant
Morphine: help with pain and dilates coronary arteries
Supplemental O2
How are the different types of aginna treated?
Stable
nitro for breakthrough pain
Stent or CABG
Unstable
nitro, aspirin for plaque, O2, IV
When should nitro stop being used?
If 5 doses are given 3 min apart and the pain isn’t relieved
What’s the nutrition for a person with angina?
Low sat fat, high complex card, high fiber diet
Reduce alcohol and simple sugars
High Omega-3 fatty acids
Strict diabetes control
What’s the patho of a myocardial infarction?
Something causes the coronary artery to no longer be able to supply blood to the heart
Occlusion of vessel d/t stable CAD or plaque rupture
Spasms of arty d/t stimulant use
Supply-demand mismatch d/t hypovolemia, hemorrhage, or tachycardia
The tissue distal to the blockage soon begins to die and cannot be reversed
If enough tissue is affected, the person may die
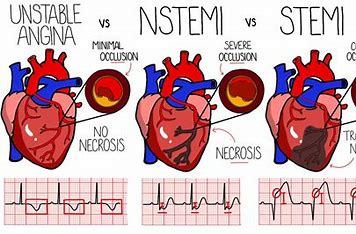
What’s the difference between unstable angina, a STEMI and NSTEMI when discussing myocardial infarctions?
Unstable angina: minimal occlusion, T wale inversion, no necrosis
NSTEMI: severe occlusion, ST depression, necrosis
STEMI: complete occlusion, ST elevation, transmural necrosis
What are manifestations of an MI?
■ Neuro: Lethargy, dizziness, altered LOC, syncope
■ CV: hypotension, weak and thready pulse, angina, tachycardia, possible early hypertension
■ Resp: SOB, tachypnea, crackles (pressure backing up in left atrium, then to the lungs)
■ GI: Nausea, vomiting
■ GU: oliguria
■ Integ/Musc: cool, clammy skin, possible diaphoresis , JVD
■ Psychosocial: anxiety, feeling of impending doom
■ Other: There is often a difference in the presentation with men and women
What labs are taken for an MI?
Cardiac enzymes: troponin, myoglobin, CK, CK-MB
CBC
PT/INR: bleeding times determine coagulant use
Chem panel
How is an MI diagnosed?
EKG: ST depression for NSTEMI and ST elevation for STEMI (elevated in 3 leads)
Echo, TEE, Angiography
How are STEMIs and NSTEMIs managed?
STEMI
thrombins, thienopyridines (clopidogrel or aspirin), heparin, “__prils”, O2, morphine, beta blockers, CABG, PCI, nitro, statins
NSTEMI
aspirin, ACEI, beta blocker, CCBs, heparin, statin, nitro, O2
What’s the difference in priority when dealing with a NSTEMI patient compared to a STEMI patient?
You want to try to reduce the stress of the heart and get them stable since there isn’t a complete occlusion
What’s an alternative for a CABG if the cath lab isn’t available when dealing with a STEMI?
TpA since it can break down the clot
What’s the nutrition of an MI patient?
NPO during the acute event
Low-sodium, low-saturated fat, low-cholesterol diet after the acute period
What are common complications of an MI?
Dysrhythmias (SVT, V-tach, V-fib)
Cardiogenic shock
HF and Pulmonary Edema(usually manifests weeks after an MI)
Cardiac arrest
What are the S&S of cardiogenic shock following an MI?
Hypotension, diaphoresis, tachycardia
Give vasopressors, O2, etc. to help heart recover
What’s the patho of heart failure (HF)?
Weakening of the heart leads to decreased CO which leads to the body not being adequately perfused.
The kidneys try to compensate by retaining Na and water which further stresses the heart
Additionally, the blood not being pumped out of the LV starts to back up into the PV and into the lungs and soon to the right side
What’s the kidney involvement in HF?
When the body isn’t getting properly perfused, the kidneys see it as hypovolemia, so they active the RAAS system to release AHD which increases sodium and water retention. This puts more pressure to the heart that’s already having issues perfusing the body
What is ejection fraction (EF) and how is it measured?
It’s how much blood the left ventricle pumps out with each contraction. Normal (55%-65%)
EF=(Stroke Volume/End-Diastolic Volume) x 100
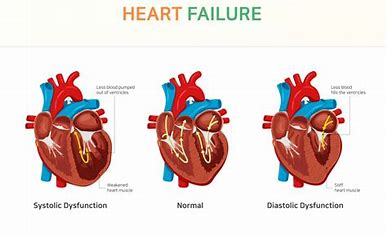
What’s the difference between HFrEF and HFpEF?
HFrEF (reduced)
“systolic” HF and involves the LV being WEAK which decreases the EF (<55%-65%)
HFpEF (preserved)
“diastolic” HF and involves the LV being stiff and smaller which means that when with an EF of 55%-65%, there isn’t enough total volume to meet the metabolic needs of the body
What are causes of HF?
CAD, MI, HTN, valvular heart disease, congenital heart defects, cardiomyopathy
Causes of exacerbations
anemia, dysrhythmias, hypervolemia, infection, PE, thyroid disorders
What are manifestations of HF?
LSHF
■ Neuro: Lethargy, dizziness, altered LOC, syncope
■ CV: hypotension (llittle blood beating), weak and thready pulse, angina, tachycardia
■ Resp: SOB, tachypnea, dyspnea, orthopnea, crackles, non-productive cough, wheezes, pink and frothy sputum (related to fluid accumulation to the lungs)
■ GI: Nausea, vomiting
■ GU: oliguria
■ Integ/Musc: cool, clammy skin, possible diaphoresis , weight gain (fluid overload0
■ Psychosocial: anxiety?
RSHF
■ Neuro: Lethargy, dizziness, altered LOC, syncope
■ CV: hypotension, weak and thready pulse, angina, tachycardia
■ Resp: SOB, tachypnea
■ GI: Nausea, vomiting, ascites (big belly), hepatomegaly
■ GU: oliguria
■ Integ/Musc: cool, clammy skin, possible diaphoresis , JVD, edema, weight gain
■ Psychosocial: anxiety, fatigue
What labs are taken for HF?
BNP: determine the stretch of vessels which helps determine fluid overload
Chem panel: looks for hemodilution and renal labs
CBC: risk for anemia d/t kidney injury
ABGs: looking for metabolic acidosis
LFTs: seen in RSHF
What diagnostics are taken for HF?
EKG, CXR, Echocardiogram (MEASURES EJECTION FRACTION), central venous pressure (MEASURES PRESSURE OF RIGHT HEART), exercise stress test, cardiac cath/angiogram
How is HF managed?
Meds
diuretics: furosemide but monitor for electrolytes imbalance (potassium)
vasodilators: nitro helps increase heart perfusion but monitor BP
morphine: decreases afterload
beta blockers: “__olol” decrease HR
ACEI: cardio protective
Positive inotropes: dopamine, dobutamine, milrinone increase contractility
What’s the nutrition of a HF patient?
sodium and fluid restriction
What are nursing considerations for a HF patient?
Check electrolytes and ABCs
Monitor I&Os
Give supplemental O2, elevate bed, elevate feet is edema is present
Maintain diet restrictions and cluster care