Equine interpretation workshop
1/19
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
20 Terms
Case 1
A 1-year-old Thoroughbred filly presents with projective watery diarrhoea of 2 weeks' duration. The BCS is 1/5, with well visible ribs, tucked-up abdomen, undeveloped musculature of the hind limbs and forelimbs. The filly has dull demeanour. The heart rate is 60 beats per minute, respiratory rate is 12 breaths per minute and rectal temperature is 38.8°C. Mucous membranes are tacky, dry with a CRT of 3 seconds. Gastrointestinal borborygmic are loud, watery on all quadrants. Digital pulses are palpable but not increased.
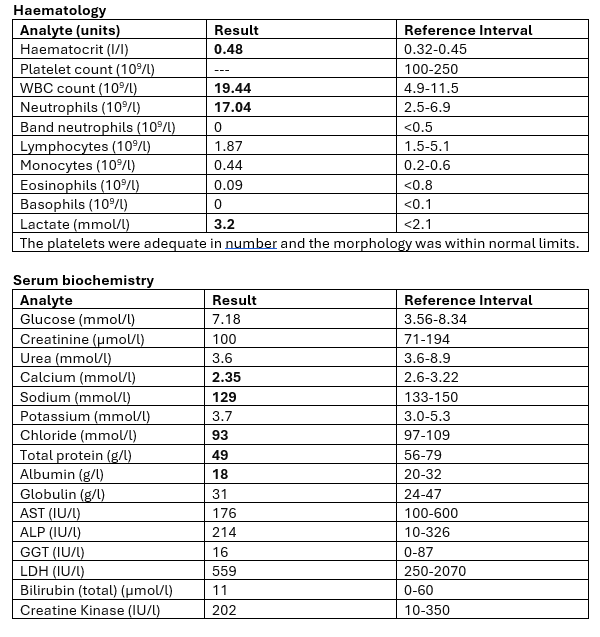
interpret the haem and biochem
The elevated haematocrit suggests haemoconcentration (dehydration, hypovoleamia)
There is a mature neutrophilia.
Band neutrophils are not observed but in deciding between stress neutrophilia and inflammatory neutrophilia,
we are not seeing the lymphopenia we would expect in a classic glucocorticoid stress leucogram making an inflammatory explanation more likely. → likely chronic condition
Lactate is elevated suggesting poor perfusion (consistent with noted haemoconcentration/ hypovolaemia)
Albumin (and therefore total protein) is low but there is not evidence to suggest any hepatic pathology that could compromise production meaning that excessive albumin losses are more likely (acute phase inflammatory repose is another possibility).
Albumin-losing conditions are often either protein losing enteropathy or protein losing nephropathy.
A history of diarrhoea makes PLE the more likely of the 2. Urine protein analysis would confirm the absence of PLN if required.
Na and Cl are reduced by similar amounts suggesting that electrolytes as well as water are being lost in diarrhoea fluid (secretory diarrhoea).
This has a greater impact on circulating volume and perfusion that would the loss of water alone.
Calcium circulates in 3 forms (ionised, albumin bound and complexed with e.g phosphate) the lower albumin bound fraction has reduced the total measured calcium iCa is unlikely to have been affected (i.e., this is not truly a physiologically hypocalcaemic disorder)
low wbc
salmonella risk and must isolate
what is there a risk of if giving fluids when low albumin
it will dilute the albumin so theres risk of oedema
Case 1
A 1-year-old Thoroughbred filly presents with projective watery diarrhoea of 2 weeks' duration. The BCS is 1/5, with well visible ribs, tucked-up abdomen, undeveloped musculature of the hind limbs and forelimbs. The filly has dull demeanour. The heart rate is 60 beats per minute, respiratory rate is 12 breaths per minute and rectal temperature is 38.8°C. Mucous membranes are tacky, dry with a CRT of 3 seconds. Gastrointestinal borborygmic are loud, watery on all quadrants. Digital pulses are palpable but not increased.
interpret this history and clinical exam
tachycardic
because of hypovolaemia from loss of fluid from diarrhoea
slight pyrexia
What does evelated Haematocrit (the percentage of whole blood made up of red blood cells) suggest
Suggests dehydration and hypovolaemia
What can help distinguish between stress neutrophilia and inflammatory neutrophilia?
We could expect lymphopenia in a classic glucocorticoid stress leucogram
What would elevated lactate suggest
Poor prefusion- consistent with hypovolaemia
What are albumin-losing conditions categorised as?
Albumin-losing conditions are often either protein losing enteropathy or protein losing nephropathy.
-Diarrhoea would confirm PLE
-Urine protein analysis would confirm the absence of PLN
What would make us suspect secretory diarrhoea?
Sodium and chlorine are reduced by similar amounts
Case 2
A 23-year-old Shetland pony mare is examined for severe deficits in proprioception (sense of body position) (grade 4/5) and inappetence. The menace response is delayed (blink in response to a threatening hand movement toward the eye) PLR is normal.
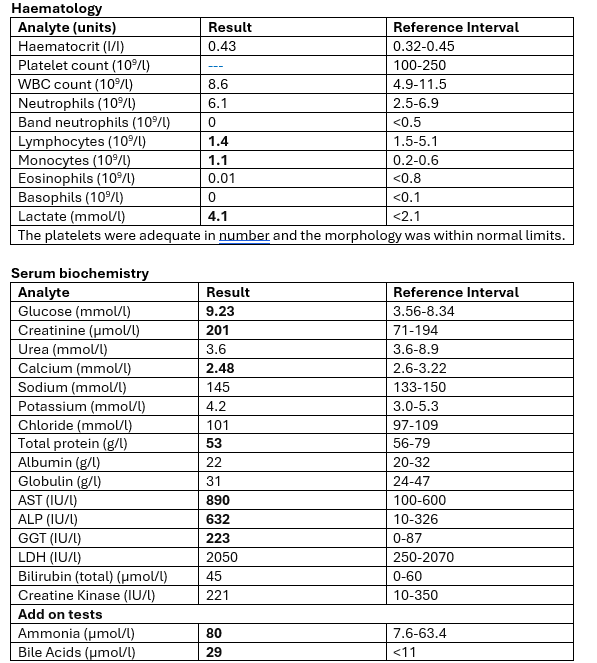
interpret the haem and biochem
There is a moderate monocytosis, we can see this as part of stress leucogram and chronic inflammation.
In this case there is no other evidence of either of these.
Fibrinogen or serum amyloid A could be added to objectively assess inflammatory status (normal neutrophil count does not exclude inflammation especially in horses)
it would have limited practical value given the remainder of the profile results.
Lactate suggests compromised perfusion.
Creatinine elevation may have a pre-renal origin consistent with hypovolaemia and poor perfusion.
USG is not available to classify the azotaemia as renal vs pre-renal.
Elevated glucose represents a stress response and although there is evidence of hepatic dysfunction it is not severe enough to have compromised glucose manufacture.
There is mild hypocalcaemia which is not clearly due to hypoalbuminaemia (TP is low and albumin is more towards the low end of its interval than globulin is so perhaps there is some degree of relative hypoalbuminaemia)
if further evidence of its significance is needed iCa measurement might help.
The liver enzymes indicate hepatic pathology, and the functional tests indicate disrupted hepatobiliary function.
The ammonia in particular provides strong evidence of porto-systemic shunting and gives and explanation for the neurological clinical signs (hepatic encephalopathy)
for a shetland with a PCV of 0.43, and the ref is 0.32-0.45 is this normal
not for a shetland
is within the range but expect it to be in the 0.3s for shetlands
other than the liver where else can AST come from
muscle → also look at CK to know if its m (And other liver enzymes)
what do higher bile acids indicate for the prognosis
higher bile acids = worse prognosis
how can high ammonia make a horse look dull
hepatic encephalopathy
ammonia builds up
has inhibitory effect on the brain
so horse looks dull
Does a normal neutrophil exclude inflammation?
no- particularly not in horses
What does high lactate suggest?
Compromised perfusion
Case 2
A 23-year-old Shetland pony mare is examined for severe deficits in proprioception (sense of body position) (grade 4/5) and inappetence. The menace response is delayed (blink in response to a threatening hand movement toward the eye) PLR is normal.
what are the next steps in this case
investigate liver more
us
biopsy
What may high creatinine be consistent with?
Creatinine elevation may have a pre-renal origin consistent with hypovolaemia and poor perfusion.
What can USG not classify?
If azotaemia is renal or pre-renal
What do liver enzymes indicated?
Hepatic pathology
What does high ammonia suggest?
High ammonia provides strong evidence of porto-systemic shunting and gives and explanation for the neurological clinical signs (hepatic encephalopathy)