Microbial Diseases of the Nervous System
1/75
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
76 Terms
What are the three layers of the meninges?
Dura mater (outermost), Arachnoid mater (middle), Pia mater (innermost).
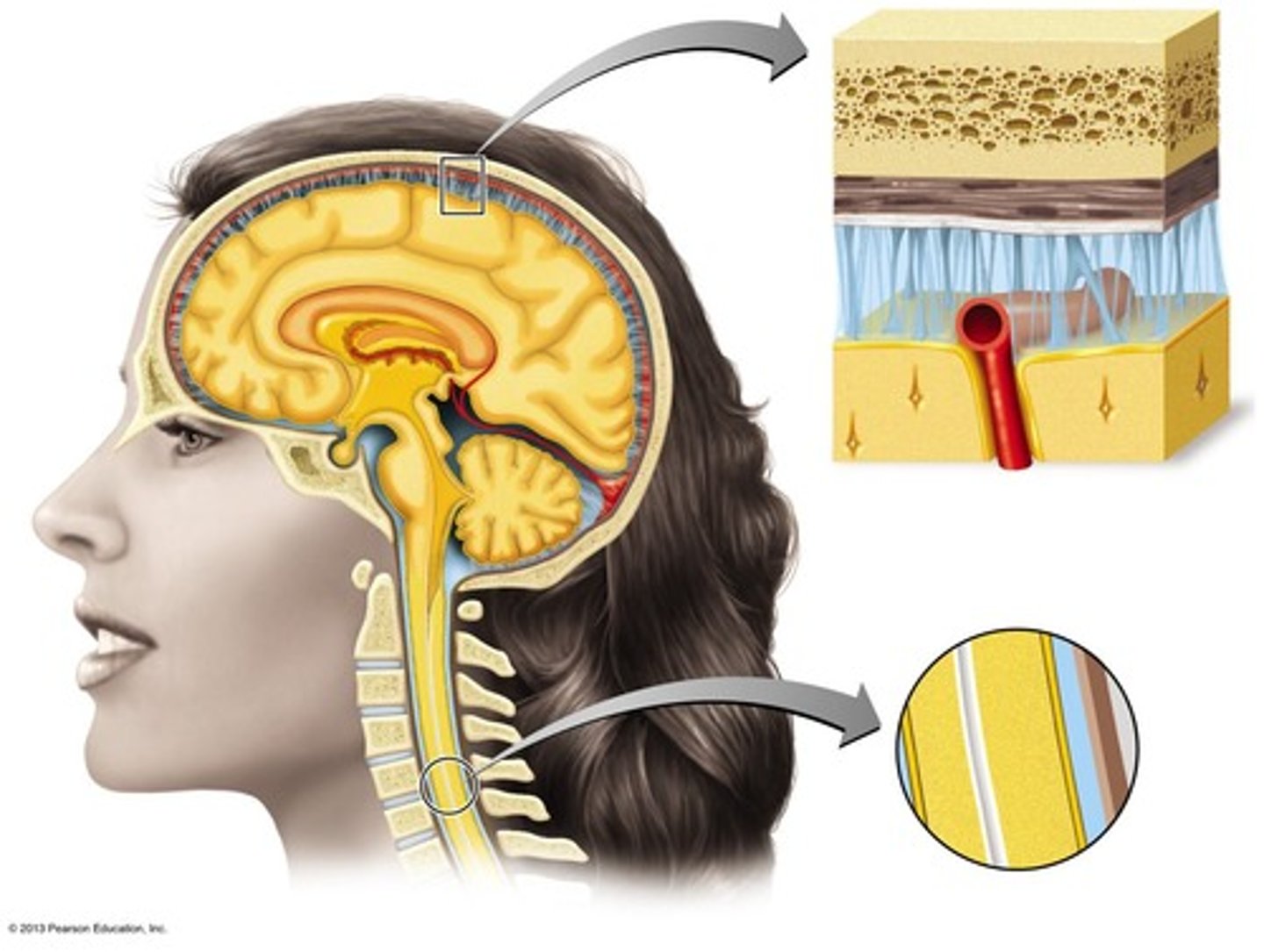
What does the arachnoid mater contain?
The subarachnoid space, which contains cerebrospinal fluid (CSF). -it's web like
meninges
three protective membranes that surround the brain and spinal cord
What is the function of the blood-brain barrier?
a filtering mechanism of the capillaries that carry blood to the brain and spinal cord tissue, blocking the passage of certain substances
What is the subdural space?
Potential space between dura and arachnoid maters
what does the blood brain barrier allow to go through?
water, most gasses, lipid soluble compounds, glucose & amino acids (which require active transport)
what does the blood brain barrier not allow to go through?
hydrophilic compounds (most drugs), some hydrophobic molecules (which require active transport)
What is meningitis?
Inflammation of the meninges.
What is encephalitis?
Inflammation of the brain.
What is meningoencephalitis?
Inflammation of both the brain and meninges.
what may inflammation of the nervous system be caused by?
bacteria or viruses
lumbar punch "spinal tap"
a medical procedure used to collect cerebrospinal fluid (CSF) from the lower back -no penetration of bone & preferred method of sampling (safe place to access lumbar region)
What is viral meningitis and how does it differ from bacterial meningitis?
Viral meningitis is more common and less severe, often caused by enteroviruses, while bacterial meningitis has more severe symptoms and can lead to serious complications.
what is viral meningitis termed as and when does it usually occur?
aseptic meningitis and tends to be seasonal (summer/fall)
What are the initial symptoms of bacterial meningitis?
Fever, headache, and stiff neck, followed by nausea and vomiting but may progress to convulsions and coma
What is Haemophilus influenzae meningitis?
A bacterial meningitis caused by Gram-negative aerobic bacteria (normal throat microbiota), primarily affecting children aged 6 months to 4 years.
what can Haemophilus influenzae meningitis cause & how can it be treated?
causes pneumonia and ear infections which can be treated with antibiotics -Hib vaccine
What is Neisseria meningitis?
Also known as meningococcal meningitis, it is caused by Gram-negative aerobic cocci and can lead to severe outcomes, particularly in children under 2 years.
How is Neisseria meningitidis spread?
spread by droplet aerosol (40% of people are healthy nasopharyngeal carriers)
what are signs of Neisseria meningitis and how can it be treated?
begins as throat infection, rash (a rapid production of endotoxin) and treated with antibiotics with a mortality rate of 9-12%
What is Streptococcus pneumoniae meningitis?
"pneumococcal meningitis" it is a gram positive diplococcus and the leading cause of bacterial meningitis
how is Streptococcus pneumoniae meningitis treated?
treated with antibiotics but resistance is growing and is preventable by vaccination
Who does Streptococcus pneumoniae affect and what can it cause?
most common in children 1 month to 4 years, 70% of people are healthy nasopharyngeal carriers (mortality 30% children, 80% elderly) and may cause pneumonia and ear infections
What is listeriosis?
A disease caused by Listeria monocytogenes (gram postive aerobic rod) that can lead to severe outcomes, especially in newborns. (delayed infection 60% mortality)
How is Listeriosis transmitted?
usually foodborne, it can be transmitted to fetus via placenta (abortions & still births), spreads cell to cell via actin filaments
What is Hansen's Disease (leprosy)?
caused by Mycobacterium leprae an acid fast rod that grows best at 30'C and affects peripheral nerves and skin cells.
how is Hansen's disease transmitted?
transmission requires prolonged contact with an infected person
how can Hansen's disease be treated?
treated with rifampin and clofazimine (fat soluble and highly diffusible)
What are the two forms of Hansen's disease?
Tuberculoid (neural) leprosy and lepromatous (progressive) leprosy.
tuberculoid (neural) leprosy
nerve cells are infected, loss of sensitivity and may recover spontaneously

lepromatous (progressive) leprosy
skin cells are infected, severs tissue damage and host has CM response
What is botulism?
A disease caused by Clostridium botulinum, a gram positive, endospore forming obligate anaerobe
how is botulism characterized?
characterized by flaccid paralysis due to the botulinum toxin (blocks release of neurotransmitter acetylcholine, causing flaccid paralysis)
What are the symptoms of botulism?
Double or blurred vision, drooping eyelids, slurred speech, difficulty swallowing, dry mouth, and muscle weakness.
what are the botulnal types?
type A, B, E toxins
botulnal type A toxin
heat resistant and proteolytic, fatality 60-70%
botulnal type B toxin
fatality 25%
botulnal type E toxin
produced by organisms in marine and lake sediments, is less heat resistant than other strains
are how botulnal types diagnosed?
diagnosed by inoculating immunized mice with patient samples
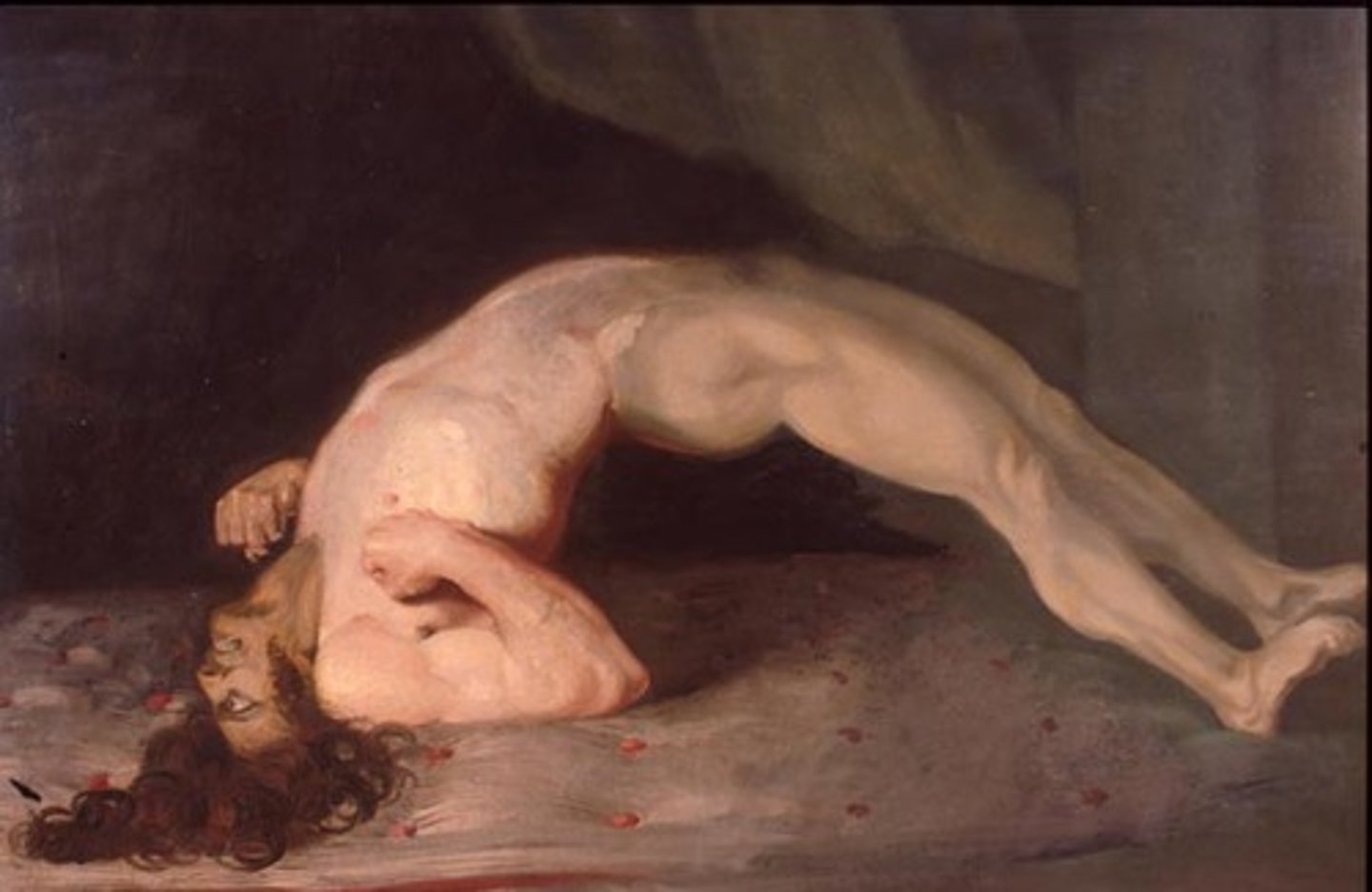
What is tetanus?
A disease caused by Clostridium tetani, leading to muscle spasms due to the tetanospasmin neurotoxin.
infant botulism
C. botulinum growing in the intestines of infants due to a lack of intestinal microbiota; associated with honey
wound botulism
growth of C. botulinum in wounds
how is wound botulism treated and prevented?
treated with respiratory assistance and antitoxins, & prevented with proper canning and use of nitrites in foods
what is Tetanus?
a gram postive, endospore forming, obligate anaerobe caused by Clostridium tetani that grows in deep wounds
What are the symptoms of tetanus?
Stiffness of the neck, jaw, and other muscles, often accompanied by a grotesque, grinning expression.
tetanospasmin
Neurotoxin causing muscle spasms in tetanus. (blocks the relaxation pathway in muscles)
how is Tetanus treated and prevented?
treated with debridement and tetanus immune globulin (TIG), prevented by vaccination with tetanus toxoid (DTaP)
DTaP vaccine
stimulated antibodies that neutralize the toxin, booster is required every 10 years
tetanus toxin
causes tetanus
What is poliomyelitis?
A viral disease caused by poliovirus, often asymptomatic but can lead to paralysis.
How is poliomyelitis transmitted?
fecal-oral route
what are symptoms of poliomyelitis?
usually asymptomatic or brief, mild illness (fever, headache, sore throat, vomiting, loss of appetite)
how is poliomyelitis diagnosed and prevented?
viral culture, RT PCRP, serology; prevented by immunization with either live/killed vaccines
what is mostly likely to be the next disease to be completely eradicated?
poliomyelitis
What is arboviral encephalitis?
Encephalitis caused by viruses carried by arthropods, such as mosquitoes.
symptoms and prevention of arboviral encephalitis?
chills, headache, fever may lead to coma and death; prevention is pest control
What is Zika virus disease?
A viral infection primarily transmitted by Aedes mosquitoes, associated with mild symptoms and severe birth defects if contracted during pregnancy.
Western Equine Encephalitis (WEE)
Togavirus; birds/horses are reservoir, sporadic 5% mortality
Eastern Equine Encephalitis (EEE)
Togavirus; birds/horses are reservoir, 100/year 30% mortality
St. Louis Encephalitis (SLE)
May be most common of all American viral encephalitides
Epidemics in the US occur most often in the Midwest and South; birds are reservoir
California encephalitis (CE)
reservoir is small animals; mild illness
West Nile encephalitis (WNE)
reservoir is primarily birds, assorted rodents, and large mammals; emerging disease (dead birds!!)
Zika Virus Disease (ZVD)
transmitted primarily through the bite of infected Aedes spp. mosquitoes; others include sexual, mother to child, blood transfusions
diagnosis of zika virus disease
diagnosis by reverse transcriptase PCR
prevention of zika virus disease
prevention by controlling mosquitoes
What is cryptococcosis neoformans meningitis?
A soil fungal infection caused by Cryptococcus neoformans, associated with pigeon/chicken droppings and can lead to meningitis.
how is cryptococcus neoformans meningitis transmitted?
transmitted by the respiratory route, spreads through blood to the CNS (mortality up to 30%)
treatment for cryptococcus neoformans meningitis
amphotericin B and flucytosine
What is African trypanosomiasis?
Also known as sleeping sickness, caused by Trypanosoma brucei gambiense, transmitted by tsetse flies.
Symptoms of African trypanosomiasis
interstitial inflammation and necrosis within lymph nodes and small blood vessels of brain and heart, leading to lethargy and death within 1-3 years
diagnosis of African trypanosomiasis
observation of motile parasites in blood, antibody detection
prevention for African trypanosomiasis
pest control, antiparasitics are curative, vaccination is not possible due to antigenic variation
treatment for African trypanosomiasis
melarsoprol (highly toxic) and eflornithine (very effective -inhibts facial hair)
What is amebic meningoencephalitis?
A rare but severe infection caused by Naegleria fowleri, typically associated with swimming in warm freshwater.
diagnosis of amebic meningoencephalitis
diagnosis usually made during autopsy (brain is mush)
What is the mortality rate for untreated amebic meningoencephalitis?
Near 100%, no effective treatment