Immunology Unit 11
1/24
Earn XP
Description and Tags
HIV/AIDS
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
25 Terms
What is acquired immunodeficiency syndrome (AIDS)?
a chronic immune deficiency caused by HIV
What is reverse transcriptase?
an enzyme found in RNA in the core of retroviruses
converts RNA to DNA
viruses that have this RNA are known as retroviruses
What are the two types of HIV that cause AIDS?
HIV type 1
causes the vast amount of infections globally, split into 3 groups:
Group M (major) makes up 90% of all HIV 1 infections
Group O (outlier) is endemic to West Central African nations
Group N (neither) is found in Cameroon
HIV type 2
prevalent in West Africa (very low in the US)
less virulent than type 1
treatment is different for each type
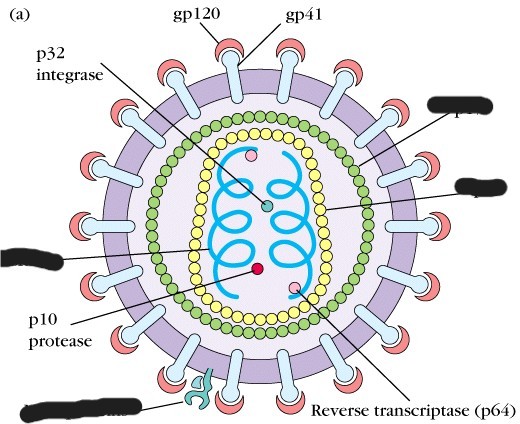
List and describe the 2 main structures of the HIV
envelope
double membrane
contains knob-like glycoproteins (gp120) with another glycoprotein on top (gp41)
core
surrounded by structural proteins
contains single stranded RNA
also contains protease (p10), integrase (p32), and reverse transcriptase
What are the 3 predominant genes found in the virus’ genome?
gag gene
encodes for viral core particles (protease and integrase)
env gene
encodes for the envelope proteins p41 and p120
pol gene
encodes for reverse transcriptase
What types of cells is HIV drawn to?
mostly CD4 T lymphocytes (T helper cells)
CD4 acts as a receptor for gp120 to attach and enter the cell
can also invade other CD4 cells: macrophages and monocytes
these cells can enable HIV 1 to enter the CNS
How does HIV invade CD4 host cells? (4 steps)
gp120 (envelope protein) binds to CD4 and the co-receptor CCR5 or CXCR4 on the host cell
virus must bind to both to enter the cell
gp41 (envelope protein) undergoes a confirmational change and inserts itself into the T cell membrane
HIV and T cell membranes fuse
core contents inside the HIV enter the CD4 cell
Describe the 6 steps of HIV replication
reverse transcriptase transcribes viral RNA into DNA
using integrase, HIV inserts the new viral DNA into the host genome
transcription of the host DNA with the inserted viral DNA takes place
replication occurs: the virus uses the host cell’s machinery to make chains of HIV proteins
mature virions are produced and escape from the cell, looking to infect more CD4 cells
CD4 cells are eventually destroyed
How is HIV 1 and HIV 2 transmitted?
HIV 1
cervicovaginal, penile, rectal, oral, percutaneous (skin puncture), intravenous, in utero, or breastfeeding routes
HIV 2
primarily by heterosexual contact
80% of HIV 1 infected adults are infected through exposure to __________, while 20% are infected through the _______ route
mucosal surfaces containing the virus, percutaneous or IV
HIV can be transmitted as:
the virus itself
OR as a cell-associated HIV
Which 9 fluids has HIV 1 been isolated from?
blood, semen, vaginal secretions, saliva, tears, breastmilk, CSF, urine, and amniotic fluid
Which 4 fluids are known for transmitting HIV?
blood, semen, vaginal secretions, and breastmilk
What are the 5 stages of HIV (according to the CDC)?
Stage 0
early stage, inferred from a negative or indeterminate test result within 6 months of a confirmed test
Stages 1, 2, 3
based on CD4 lymph count
Stage Unknown
stage can change after diagnosis
Describe how HIV progresses
Stage 0 can last months to years after initial infection
can be completely asymptomatic or exhibit mild, chronic lymphadenopathy
HIV 1 soon causes a progressive derangement of immune function
2 to 10 years after infection, virus replication can flare up again, and the infection enters the final stage
8 to 10 years can pass before AIDS finally develops
different manifestations based on the host
end stage (stage 3)
CD4 lymph count is < 200 cells (normal is 500-1200)
neoplasms and opportunistic infections
How can infected CD4 cells destroy more CD4 cells?
gp120 can break off of the virus and bind to CD4 receptors on uninfected cells
this stimulates the immune system to destroy these cells
so not only can viral replication induce CD4 cell death, HIV can also cause the immune system to destroy its own cells
The normal ratio of CD4 T lymphocytes to CD8 lymphocytes is 2:1. What is the ratio in HIV/AIDS?
0.5:1
it is reversed
normally, there are 65% CD4 cells and 35% CD8 cells in the body, in AIDS, it is reversed (more T regs)
What is syncytia?
when HIV infected cells and uninfected cells fuse together into giant, nonfunctional cells
List 10 opportunistic infections, and 2 neoplasms that are common in AIDS
opportunistic infections/pathogens
P. jiroveci
Cytomegalovirus
Mycobacterium avium
Cryptococcus (fungal)
Toxoplasmosis
M. tuberculosis
Herpes Simplex Virus
Legionella
Histoplasma capsulatum
Cryptosporidiosis
neoplasms
Kaposi sarcoma and malignant B-cell lymphoma
Which acute phase reactants are seen in HIV/AIDS?
alpha 1 antitrypsin and serum amyloid (seen before antibody appears)
What is seronegativity, and what is it in HIV/AIDS?
seronegativity: the absence of specific antibodies for an antigen (virus, bacteria, RF, etc.), ABs are not created yet
the first 6 to 12 weeks in HIV
antibodies for gp41 in patient plasma are detectable:
all throughout the infection
List 2 screening methods and 4 confirmatory tests for detecting HIV/AIDS
screening tests
ELISA
rapid testing (fast but not sensitive)
confirmatory tests
RNA detection nucleic acid amplification testing (NAAT)
western blot (detects proteins)
PCR
quantitative RNA assay
What 2 tests are used for monitoring HIV?
viral load testing and CD4 lymphocyte testing (flow cytometry for immune function)
What are the 7 treatments (not cures) for HIV/AIDS?
nucleoside and non-nucleoside reverse transcriptase inhibitors
blocks reverse transcriptase; no replication occurs
protease inhibitors
prevents protease from replicating
fusion inhibitors
inhibits virus from fusing into CD4 cells
entry inhibitors (CCR5 antagonist)
keeps the virus from binding to co-receptors on CD4 cells
integrase strand transfer inhibitors
prevents HIV from integrating its genome into the host cell’s genome
pre and postexposure prophylaxis