1.04 Non-Medical Sciences
1/84
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
85 Terms
What are the different types of numerical data? (2)
-continuous: data w/full range of fractions, potentially infinite no. of possible values e.g. weight, height
-discrete: data w/o fractions, whole numbers (no. of patients)
What are the different types of categorical data? (5)
-binary: 2 options (yes/no)
-nominal: groups that cannot be arranged in order (blood types, eye colour)
-ordinal: ranked, data consts of labels (non-numeric) or subjective (numeric) that can be arranged in order e.g. pain rating out of 10
-quantitative: countable + measurable factors obtained from questionnaires
-qualitative: more detiled descriptions obtained from in-depth interview and focus groups e.g. ethnography
Outline the measures of central tendency (3)
- mean: "average" of the data series
- mode: "most frequently occuring variable in the data series"
-median: middle value of the data series
What is standard deviation?
-used for data which is normally distributed to see how much data vary around their mean
What does a low standard deviation indicate?
-spread of data is v. close to the mean
What percentage of the data is a) within 1 s.d. b) within 2 s.d. 3) within 3 s.d.
1) 68%
2)95%
3: 99.7%
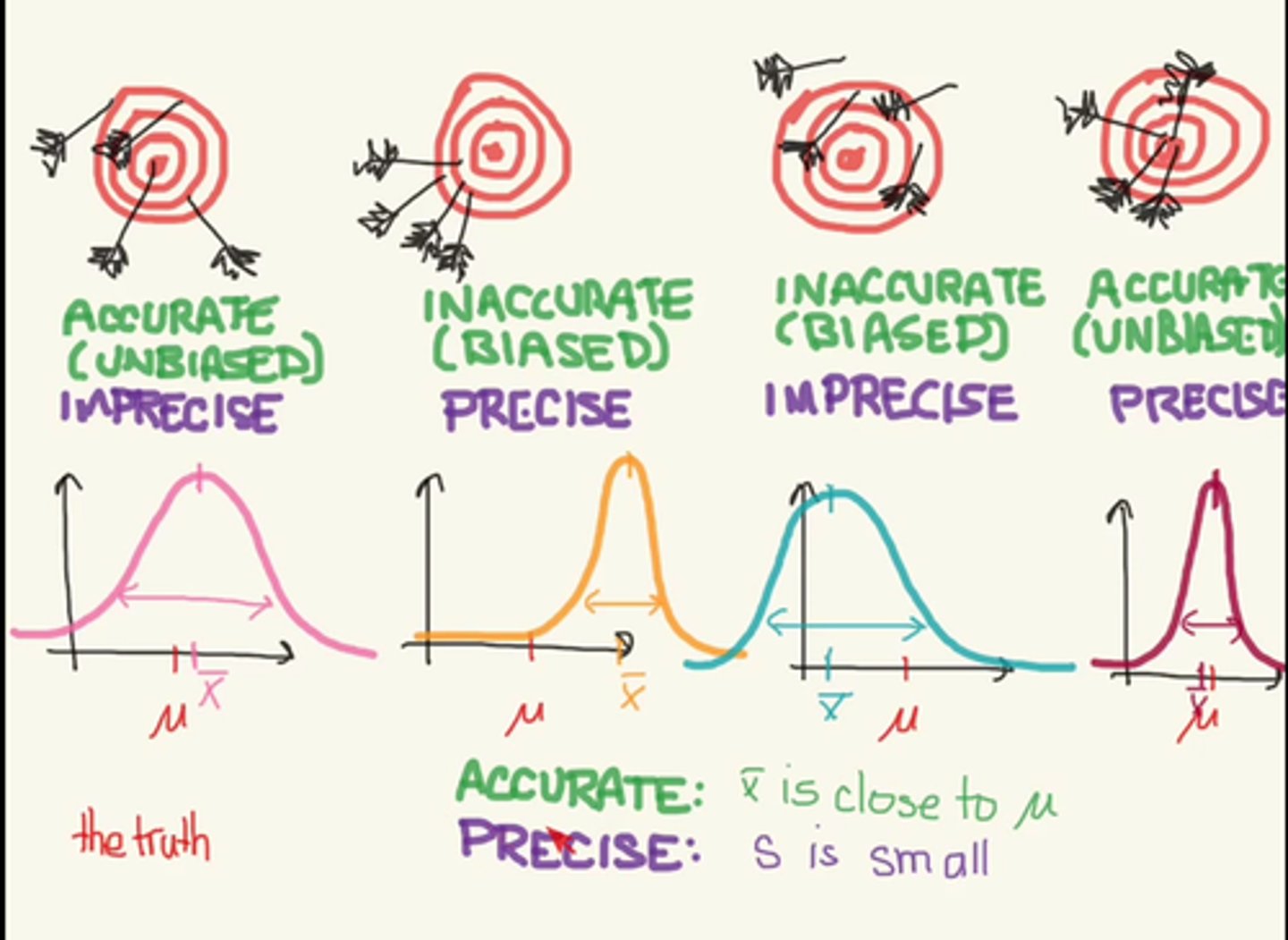
What is the difference between μ and x̄?
μ= mean taken for an entire population
x̄= mean of a sample
How do you determine a) accuracy b) precision from a normal distribution
a) x̄ is close to μ
b) s is small
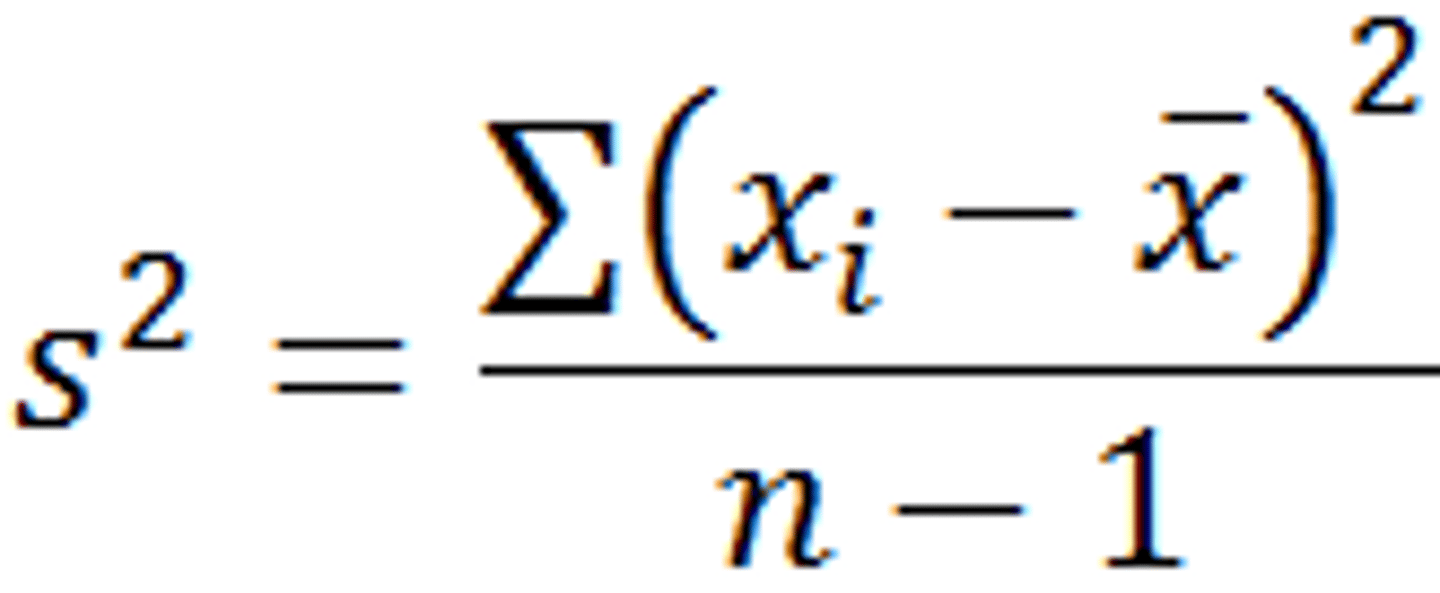
What is variance?
-looks at the average degree to which each point differs from the mean- the avg. of all data points
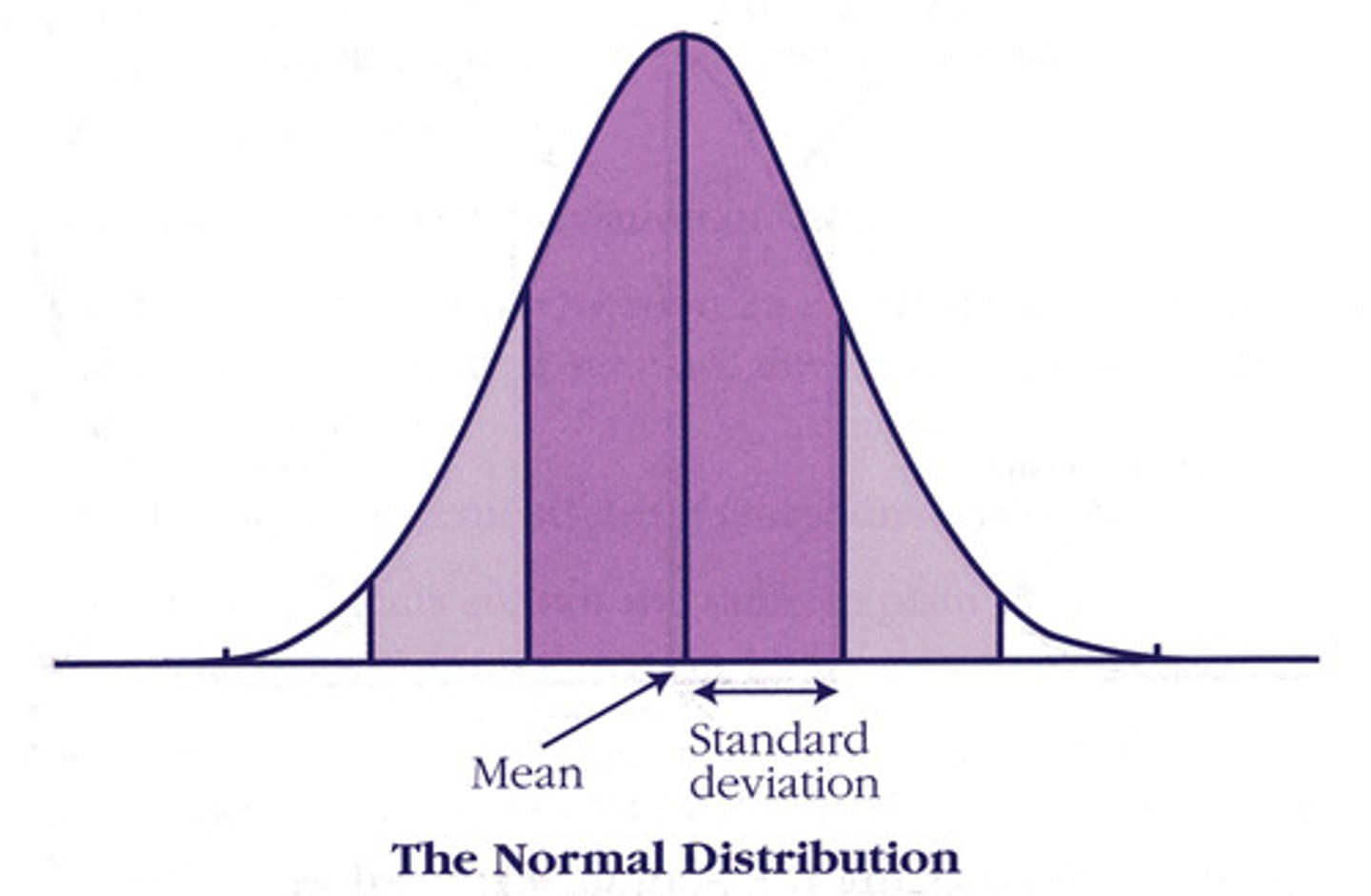
What is the normal distribution?
-an arrangement of a data set in which most values cluster in the middle of the range and the rest taper of symmetrically toward either extreme
-aka "Gaussian" distribution or bell shaped curve
What does the y-axis show in normal distribution?
-relative probability
What does the width of the curve show in normal distribution?
-standard deviation
What is the normal distribution always entered around?
-the average value
What do you need to know to draw a normal distribution? (2)
-the average measurement-> tells you where the center of the curve goes
-the standard deviation of the measurements, this tells you how wide the curve should be; the width of the curve determines how tall it is, the wider the curve, the shorter. The narrower the curve, the taller
What are the properties of normal distribution? (2)
-continuous, symmetrical distribution
-mean, mode, median (look at notes for skewed distributions)
What is health equity?
-absence of unfair health disparities that systematically & adversely affect disadvantaged social groups
What is meant by equity of access?
-the service is available fairly for all those who need it
What are health inequalities?
variations in health between population groups, resulting from a variety of societal and economic processes that are unequally distributed within or between populations
What would equality of access to services suggest?
-all people would have equal or equivalent e.g. all lived within 10 mins walk of a GP, or waited the same length of time for an appointment
Outline the Marmot review into health inequalities
-the conditions in which people are born, grow, live, work and age can lead to health inequalities
-draws attention to the evidence that most people in England aren't living as long as the best off in society and spend longer in ill-health - premature illness and health affects everyone below the top so it argues that traditionally gov. policies have focused resources only on some segments of societies
-people living in the poorest neighbourhoods in England will on avg. die 7 yrs earlier than people living in the richest neighbourhoods + spend more of their lives w/ disability
-the lower one's social and economic status, the poorer one's health is likely to be
-health inequalities arise from a complex interaction of many factors: housing, income, disability, education, social isolation (HIDES)
What are the social inequalities in health? (3)
-rates of disease
-health outcomes
-access to healthcare
Which risk factors accounted for inequalities in health outcomes in the 19th century? (3)
-overcrowding
-poor sanitation
-availability of local treatment facilities
Which risk factors accounted for inequalities in health outcomes in modern society?
(-not everyone can afford treatment)
-detrimental behaviours e.g. poor diet, inadequate exercise + smoking are higher in populations w/lower socioeconomic status
Describe the link between socioeconomic status and health
-generally it has been indicated that there is a correlation between wealth & longevity
-people of higher socioeconomic status have better continuity of care + more knowledge about their care e.g. women of higher socioeconomic (higher income and education levels) status tend to have more awareness and the ability to take time to regularly visit their doctor therefore receive more screenings for cervical & breast cancer
Apart from socioeconomic status, what else contributes to healthcare inequalities?
-race, ethnicity, gender, mental illness and disability
What is the definition of health?
The state of complete physical, mental and social well-being and not merely the absence of disease
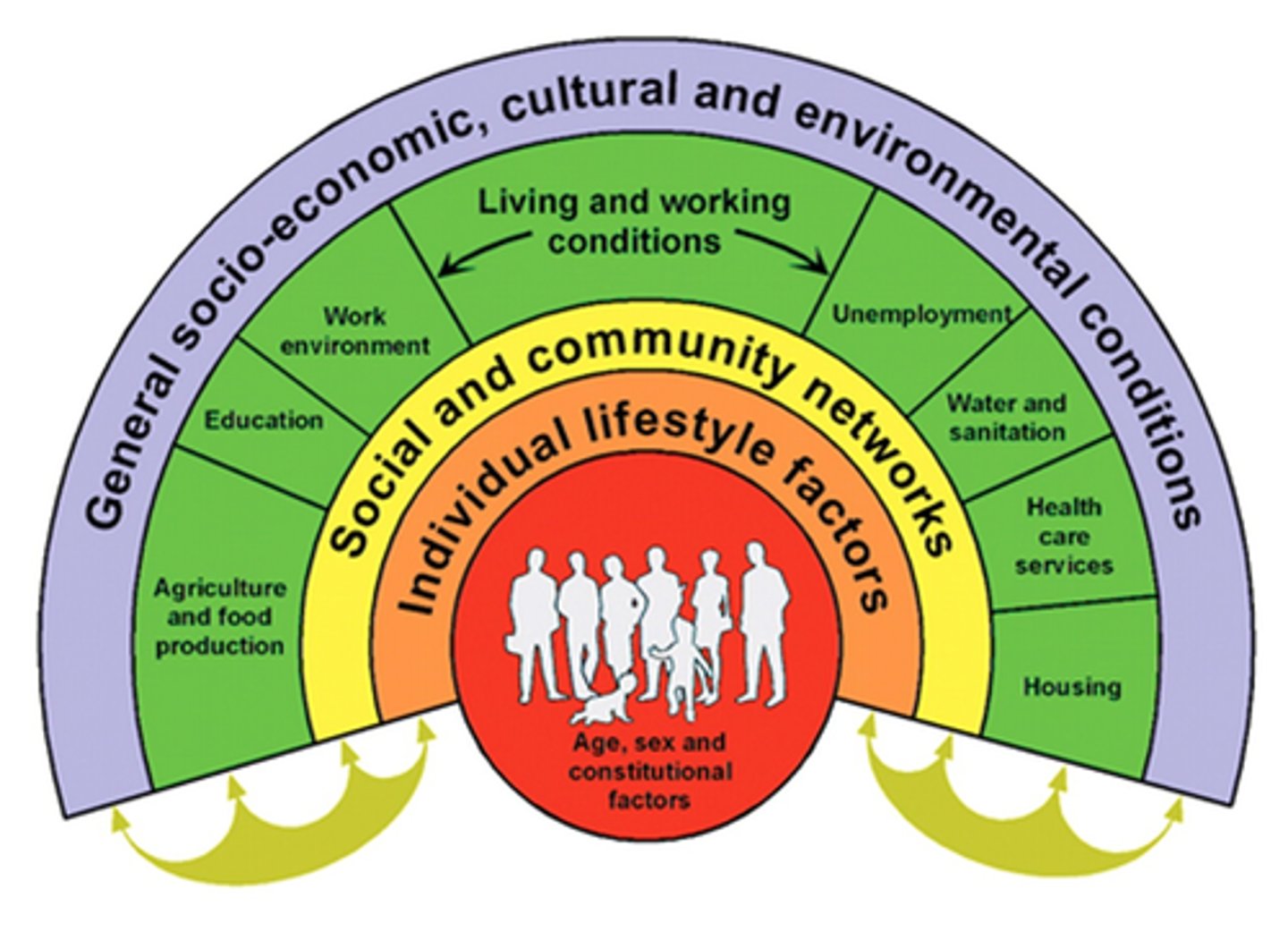
What is the Dahlgren and Whitehead 'rainbow model' (2)
-maps the relationship between the individual, their environment and health
-individuals are placed at the center and surrounding them are the various layers of influences on health- such as individual life factors, community influences, living & working conditions, and more general social conditions
Difference between health inequalities and inequities
inequity refers to unfair, avoidable differences arising from poor governance, corruption or cultural exclusion
inequality simply refers to the uneven distribution of health or health resources as a result of genetic or other factors or the lack of resources
What is meant by socioeconomic position?
- social and economic factors that influence a position that an individual/ group has in society (aka social class)based on factors such as education level, occupation, household condition, income
How can these health inequalities be tackled?
-universal action is needed, not just bottom 10% as need to reduce steepness of the social gradient of health inequalities with a scale and intensity that is proportionate to the level of disadvantage
-Marmot's approach- create conditions for people to take control of their own lives, involves local governments as well as NHS and private sector
6 policy objectives:
-giving every child the best start in life
-enabling all children, young people and adults to maximise their capabilities
-creating fair employment and good work for all
-ensuring a healthy standard of living for all
-creating and developing sustainable places and communities
-strengthening the role and impact of ill-health prevention
How can race contribute to health inequalities?
-may be at risk of certain diseases more than others
How can gender contribute to health inequalities?
-less well paid and secure jobs, pay gap, access to quality of care is different for women too as they may be less likely to have certain procedures done on them (myocardial infarction then revascularisation surgery)
What are relative health inequalities?
-measure inequality in terms of the ratio between the least advantages and the most advantaged groups
What are absolute health inequalities?
-measures inequality in terms of difference in health outcomes in the different groups
What are life course inequalities?
-investigates long term effects on health and chronic disease risk , incorporates time of exposure; socioeconomic inequalities accumulate throughout the life course
How can environmental factors determine health? Give examples + explain effect at a population + individual lvl
-exposure to physical, chemical, biological agents + social, economic and cultural factors
-e.g. urbanisation, development, energy production, factors
-pop lvl: certain regions have worse health
-individ lvl: depends on where you choose to live
How can nutritional factors determine health? explain effect at a population + individual lvl
-the food you eat
-pop lvl: eat well guide + food promotion
-individ lvl: making personal food choices
How can occupational factors determine health? Give examples + explain effect at a population + individual lvl
-the job you have
e.g. miners vs office workers
-pop lvl: some jobs more/ less competitive
-indiv lvl: think of health when choosing career
How can healthcare factors determine health? Give examples + explain effect at a population + individual lvl
-availability and cost of healthcare
e.g. having a well equipped hospital a 10 min walk away
-pop lvl: some regions have different mortality
-individ lvl: live somewhere close to improve health
How can genetic factors determine health? Give examples + explain effect at a population + individual lvl
-your genome
e.g. tumour markers passed down
-pop lvl: certain groups should have checks
-individ lvl: personal awareness
What is planetary health?
-health of human civilisation and the state of the natural systems on which it depends, interactions between natural systems and human health
Outline the changes in the quality of the natural environment (11)
-air pollution
-loss of forest -> people and wildlife in closer contact
-industrial areas
-seasons -> allergies
-home allergens - cats/dogs, cleanliness of the home
-occupation-> poor ventilation
-diet + what's available in the area
-climate change
-atmospheric aerosol loading
-ocean acidification
-water stress + ground water depletion
What is the effect on human health of the changes in the natural environment? (5)
-less healthy + good quality of food
-less hydrated
-passing diseases is easier (forest)
-preventable problems e.g. asthma
-carcinogenic chemicals in the environment
What are the three categories of challenges that humans face in relation to the natural environment?
-conceptual and empathy failures (rely on gross domestic products as measure of progress, don't think of future damage)
- knowledge failures (failure to address social and environmental drivers of ill health, not much funding or research, unwilling to work with decision making frameworks)
- implementation failures (governments and institutions don't recognise and don't respond to threats)
What is concordance?
A compromised agreement between a doctor and patient as to what the patient will do (whether, how and when medical treatment will be used)
What is compliance?
-extent to which patient's behaviour matches the prescriber's recommendations
What is adherence?
-extent to which a person's behaviour (taking amedication, following a diet, and/or executing lifestyle changes, corresponds with agreed recommendations from a healthcare provider
Describe the ideas presented by early studies on compliance
-idea that the 'problem' of non-compliance is situated within the context of the doctor-patient relationship and that patients are passive recipients of health care
-Parsons (1951) had a vision of the need to maintain social order through the adoption of specific social roles therefore patients who failed to 'comply' w/ medical instructions were viewed as 'deviant' or 'defaulting'
How did Stimson (1974) challenge the older views on compliance? (4)
-he questioned the notion that patients ought to receive instructions from the doctor + follow them -> he believed that patients had their own ideas about illness and the use of medicines
-he suggested that the focus of research should be on the social context in which illnesses are experienced + treatments used
-he carried out interviews: respondents often described that after consulting w/ doctor they sought furtehr info, speaking w/ friends & family members about their treatment i.e. rather than simply disobeying the doctor's instructions, patients were using information gathered over time to help inform decisions about their use of medicines
Why was the concept of concordance developed? (4)
-to recognise the doctor-patient interaction involved in the use of prescribed medicines
-concordance creates an open negotiation + subsequent agreement between doctors and patients about the use of medicines, treatment options which leads to an agreement about the way in which a condition will be treated
-acknowledges that both the doctor + patient have equally valid health beliefs
-concept reflects a shift towards a more equal relationshipp between the doctor and the patient
Why is the term 'compliance' problematic?
- it is built on the idea that it is rational for patients to adhere to medical advice
What is meant by lay knowledge? (2)
-refers to the ideas + perspectives employed by social actors to interpret their experiences of health and illness in everyday
-lay knowledge is integrative + holistic, drawing on multiple factors
What is the significance of lay knowledge in healthcare? (2)
-patients behaviours are influenced by their beliefs
-many instances of non-adherence are understandable from the point of view of what the patients believe, despite making no sense to the clinician
What does lay knowledge contribute to identifying? (5)
-ill health
-environmental factors
-health beliefs
-health behaviours
-understanding doctor-patient relationships
What is lay epidemiology? (2)
-process through which health risks are interpreted and understood by lay people
-observed as trends recognised by general public in a certain geographical area
In what way is lay epidemiology a challenge for public health?
-when the public disbelieves or fails to act on public health messages
How can a clinician maximise adherence?
-help the patient understand treatment recommendations
What are the laws of control (internal + external)? (2)
-internal locus: individuals who believe that they are in control of what happens to them
-external locus: individuals who believe that what happens to them is controlled by outside factors
Outline the OCEAN personality structure
-variable, but harder to change in an adult
Openess
Conscientiousness -> careful, diligent; linked to good health + long life as more likely to make good decisions, eat well + exercise
Extrovert -> increased immunity, less likely to have social diseases like depression, may be more likely to take part in risk taking activities like drinking
-Agreeableness -> more cooperative
-Neuroticism -> tendency toward anxiety, depression, self doubt and negative feelings
List some other personality traits and how they can link to an individual's health (7)
-Optimistic: may boost overall physical health; if you get ill more likely to accept their illness
-Pessimistic: less likely to take medicine but in some cases if you expect the worse you may be more careful about your wellbeing and live longer
-Stoic: can cause problems if you try to tough it out instead of getting help for a health issue
-Impulsive: can lead to many unhealthy activities including alcohol and drug abuse
-Anxious: higher risk of certain conditions, including stroke & heart disease
-Empowered: a feeling that you're in control and can be good for your health eg. more likely to take medicine the way the doctor prescribed it but on the downside if you feel emboldened to make decisions about your care when you don't necessarily have good info, that causes problems
-Hostile: linked to health problems e.g. heart disease, increased likelihood of getting certain types of migraines, bulimia, high BP & type 2 diabetes
What are some sociological factors that can impact the way in which an individual may respond to illness? (3)
-some groups are socialised to go to the doctor often/ not often
-culture
-family experiences + opinions on ilness + how to respond
What is statute law? Give an example + describe the nature of this law
-law passed by a legislative body (parliament)
e.g. theft is a statutory crime as there is a Theft Act (1968)
-always binding
What is a common/case law? Give an example + describe the nature of this law
-law derived from previous judicial decisions/ cases in court
e.g. murder- there is no statutory definition of murder so it falls under common law
-not always binding
What is public law? Give an example
-made up of both statute & common law
- largest part is criminal law= behaviour forbidden by the state, normally the state is the prosecutor not the victim(s)
e.g. man slaughter via negligence, notify GMC
What is private/ civil law? Give an example
-concerned w/ disputes between private individuals and businesses
e.g. vicarious liability (hospital covers what happens in them- NHS are vicariously liable for the negligent acts + omissions of their employees), MDU
What is a law of contract?
-legally binding agreement
What is a law of tort?
-a civil (not criminal) harm that inflicts harm upon person
-covers battery (unlawful physical contact) and negligence in medical practice
What is the civil court?
-two independent parties- tort/contract law. Aiming to fairly compensate the injured person/ people
-most within the civil system, under tort of negligence
What are the criminal courts?
-one independent party against the state
-broken the law of the state, and deciding if they need punishment
What is a right?
- a moral or legal entitlement to have or do something
What is a human right?
-rights inherent to all human beings whatever our nationality, place of residence, sex, national or ethnic origin, colour, religion, language, or any other status
Describe universal human rights
-often expressed and guaranteed by law
-international human rights law lays down obligations of governments to act in certain ways or refrain from certain acts, in order to promote and protect human rights & fundamental freedoms of individuals or groups
What is the difference between rights and interests?
-rights= what is owed to the patient (intrinsically, legally)
-interests= acting in the patient's favour- what will benefit them the most?
Outline the relevant human rights for medicine and the implications they have for medical practice
-right to life (article 2): no one should be deprived of life intentionally and there is an obligation to protect life, excludes the withdrawal of life support (artificial nutrition & hydration) in patients in a persistent vegetative state
-prohibition of torture (article 3): adequate medical treatment for everyone, including detained patients
-right to liberty (article 5): being free from restrictions, making informed decisions free of restrictions, bias or influence
-right to respect for private and family life, home and correspondence (article 8): underpinning laws concerning confidentiality
What is an absolute right? Example
Can never be limited, unqualified (w/o limitation), can be legally enforced
e.g. right not to be tortured or treated in an inhuman or degrading way
What is a limited right? Example
Rights w/exceptions, can be lawfully restricted
e.g. right to liberty
What is a qualified right? Example
Government can interfere if it is lawful and necessary
e.g. national security
What is a moral law? Example
Under ethics, grounded in humanity, not everyone believes in them
e.g. fairness, rights to privacy
What is a legal right? Example
Recognised and protected by law, can be created or abolished
e.g. free healthcare, education
What is a negative right? Example
other people must abstain from interfering w/ your actions
e.g. freedom of speech
What is a positive right? Example
Other people must provide you w/ a good or service
e.g. minimum wage, free education
What is a universal law? Example
Moral rights we all possess because we are all human
e.g. life, liberty, estate
What are special rights? Example
Rights possessed by some but not all
e.g. contracts, social relationships
Give examples of moral rights in medical practice
-informed consent: be honest, tell the truth, don't withhold important information because patient must be aware of any procedures, side effects and diagnoses
-access to treatment: always do the best you can for your patient
Give examples of legal rights in medical practice
-informed consent: if you don't tell your patient all the information they need, and they come to harm, you are responsible
-access to treatment: do not withhold treatment, don't be biased, if you inflict your personal views you are removing your patient's autonomy