fluid and electrolyte balance - chapter 20
1/98
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
99 Terms
What are some routes the body uses to excrete ions and water?
feces
sweat
lungs — help remove H+ and HCO3- by excreting CO2
kidneys(primary route)
How can lost water be replaced?
by drinking water
Which substances are associated with fluid volume and osmolarity?
water and Na+
Water crosses most cell membranes freely. If the osmolarity of the extracellular fluid changes, water moves into or out of cells and changes intracellular volume.
How do renal tubule cells in the medulla regulate their intracellular osmolarity compared to other body cells?
the renal tubules cells in the medulla, synthesize organic solutes as needed to make their intracellular osmolarity match that of the medullary interstitial fluid.
other cells in the body, regulate their volume by changing their ionic composition
Why do the lungs and cardiovascular system respond more quickly than the kidneys in maintaining fluid and electrolyte balance?
adjustments made by the lungs and cardiovascular system are primarily under neural control. thus, can be made quite rapidly
the kidneys are primarily under endocrine and neuoendocine contol, and are thus slower
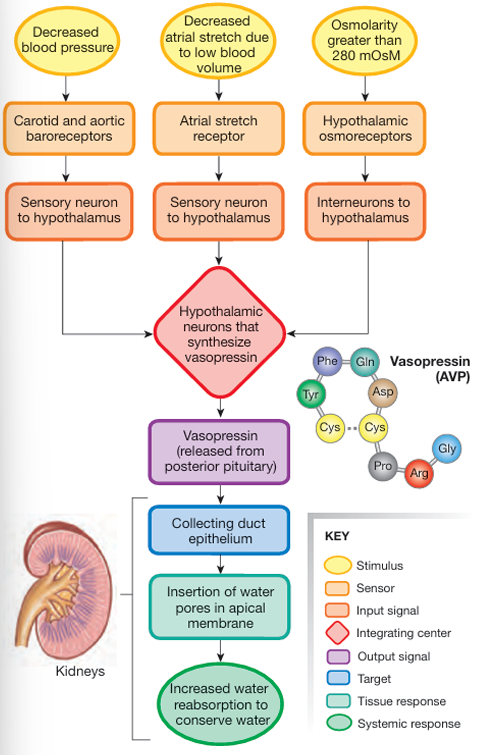
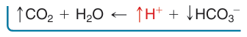
What is the response of the body to decreased blood pressure and volume?
decreased blood pressure and volume:
volume receptors in atria and corotid and aortic baroreceptors tirggers homeostatic reflexes;
cardiovascular system → increased cardiac output and causes vasoconstriction
behavior → thrist causes water intake, which causes the ECF and ICF volume to increase
this causes an increase in blood pressure
kidneys → conserve salt and water to minimize further volume loss
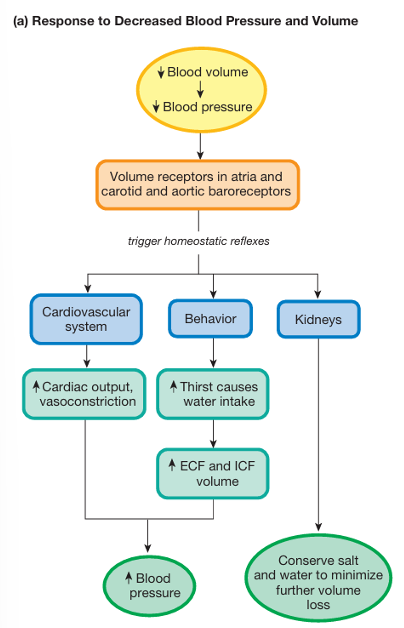
What is the response of the body to increased blood pressure and volume?
increased blood pressure and volume:
volume receptors in atria, endocrine cells in atria, and carotid and aortic barorecetors tigger homeostatic reflexes:
cardiovascular system → decreases cardiac output and causes vasodilation
kidneys → excrete salts and H2O in urine, causing a decrease in ECF and ICF volume
this decreases the blood pressure
How do we maintain a constant volume of water in the body?
by taking in the same amount of water that we excrete
In what ways do we gain water in the body?
ingested via food or drink —2L
normal metabolism, aerobic respiration —0.3L
In what ways do we lose watter in the body?
urine —1.5L
feces — 100mL
isnsensible water loss, it occurs across the skin surface and through exhalation of humidified air — 900mL
Which form of water loss can be regulated?
the water loss via urine
How does pathological water loss disrupt homeostasis?
volume depletion of extracellular compartment decreases blood pressure. if blood pressure cannot be maintained through homeostatic compensations, the tissues do not get adequate oxygen
if the fluid is hyposmotic to the body, the solute left behind in the body raise osmolarity, disrupting cell function
How does the kidney mainttain the body’s volume?
Fluid in the body enters the kidney and cycles back into the body to maintain the body’s volume.
If there is to much fluid, the fluid is allowed to drain out of the kidneys. If the small volume is lost from the body, fluid still flows through the handle, but fluid loss from the kidneys is turned of to prevent additional fluid loss.
If fluid loss is severe and volume falls below the dashed line, fluid no longer flows into the kidneys, just as a major fall in blood volume and blood pressure shuts down renal filtration.
The concentration, or osmolarity, of urine is a measure of what?
hwo much water is excreted by the kidneys
What is diuresis?
The removal of excess water in urine
How do the kisneys control the urine concentration?
By varying the amount of water and Na+ reabsorbed in the distal nephron
How is dilute urine produced?
the kidneys reabsorb solute without allowing water to follow by osmosis. this means that the apical tubule cell membranes and cell junctions must not be permeable to water
How is concentrated urine produced?
The kidney absorbs water without reabsorbing solute by making the collecting duct cells and the surrounding interstitial fluid more concentrated than the fluid inside the tubule.
If the tubule cells have aquaporins, this osmotic gradient allows water to be reabsorbed directly. The high osmolarity of the renal medulla enables this process and allows urine to be concentrated as it passes through the collecting duct.
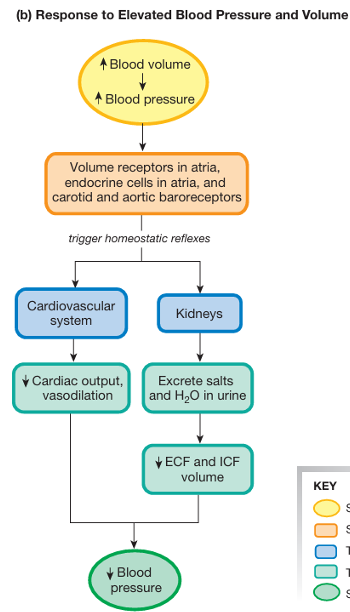
How does the kidney regulate urine concentration, and what role does the loop of Henle and distal nephron play in this process?
Filtrate enters the loop of Henle from the proximal tubule at ~300 mOsM (isosmotic).
As fluid moves down the descending limb, water is reabsorbed into the increasingly concentrated medullary interstitium; fluid becomes more concentrated. — 1200 mOsM
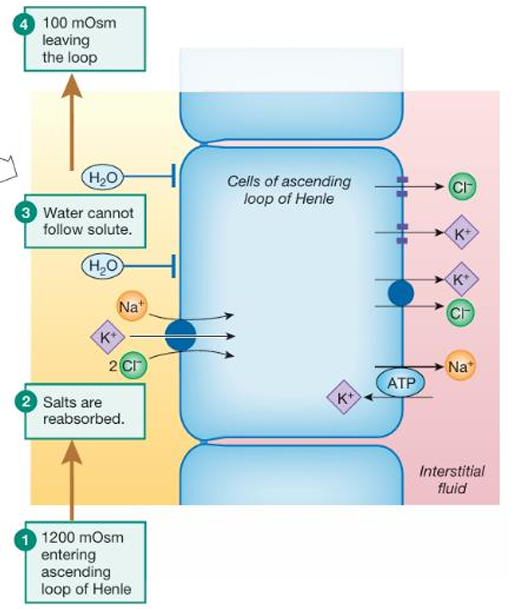
In the ascending limb, the tubule is impermeable to water but actively transports solutes out; this makes the fluid hyposmotic (~100 mOsM).
Hyposmotic fluid enters the distal nephron, where water permeability depends on hormonal control.
…
If no water pores are present: filtrate stays dilute, and urine can be as low as 50 mOsM.
If water pores are inserted: water is reabsorbed by osmosis into the concentrated medulla, concentrating the urine up to 1200 mOsM.
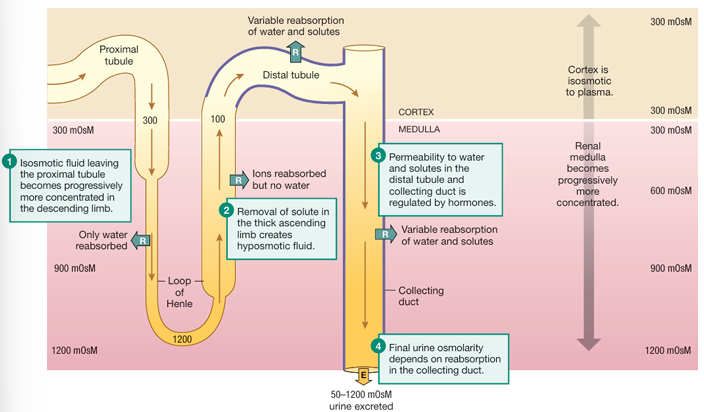
What is the function of vasopressin(ADH)?
a posterior pituatary hormone, that is involved in the process of adding or removing aquaporines in the apical membrane. it causes the body to retain water.
When vasopressin acts on target cells the collecting duct epithelium becomes permeable to water, allowing water to move out of the lumen. The water moves by osmosis because osmolarity of tubule cells and the medullary interstitial fluid is higher than osmolarity fluid in the tubule.
On What does the permeability of the collecting duct depent?
on how much vasopressin is present.
The graded effect of vasopressin allows the body to match urine concentration closely to the body’s needs.
Where are AQP2(regulated by ADH) found?
on the apical membrane facing the lumen
in the membrane of cytoplasmatic storage vesicles
What is the molecular mechanism of vasopressin, to increase water permeability in the collecting duct cells?
vasopressing arrives at the collecting duct
it binds to V2 receptors on the basolateral side of the cell
binding activates a Gprotein/cAMP 2nd messenger system
subsequent phosphorylation of the intracellular protein causes the AQP2 vesicles to move to the apical membrane and fuse with it
exocytosis inserts the AQP2 water pores into the apical membrane
now the cell is permeable to water
What is membrane recycling?
the process, in which parts of the cell membrane are alternately added by exocytosis and withdrawn by endocytosis
Which 3 stimuli control vasopressin?
plasma osmolarity → Monitored by osmoreceptors in the hypothalamus; vasopressin is released when osmolarity exceeds 280 mOsM.
blood volume → Detected by stretch-sensitive receptors in the atria; vasopressin is released when blood volume decreases.
blood pressure → Monitored by carotid and aortic baroreceptors; a drop in blood pressure stimulates vasopressin release.
How does plasma osmolarity regulate vasopressin release, and what is the threshold for activation?
Osmolarity is monitored by osmoreceptors, stretch sensitive neurons that increase their firing rate as osmolarity increases.
When the osmoreceptors shrink, cation channels linked to actin filaments open, depolarizing the cell.
The primary osmoreceptors for vasopressin release are in the hypothalamus.
when the plasma osmolarity is below the threshold value of 280 mOsM, the osmoreceptors do not fire and vasopressin release from the pituitary ceases.
If plasma osmolarity rises above 280 mOsM, the osmoreceptors shrink and fire to stimulate release of vasopressin.
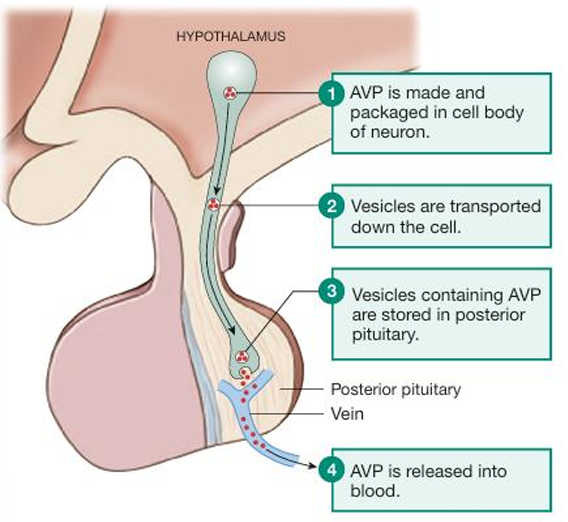
How does the hypothalamus cause secretion vasopressin when it is stimulated by low blood volume?
the vasopressin is amde and packed in the cell body of a neuron in the hypothalamus
vesicles are transported down the cell
vescicles containing vasopressin are then stored in the posterior pituitary
vasopressin is released into the blood
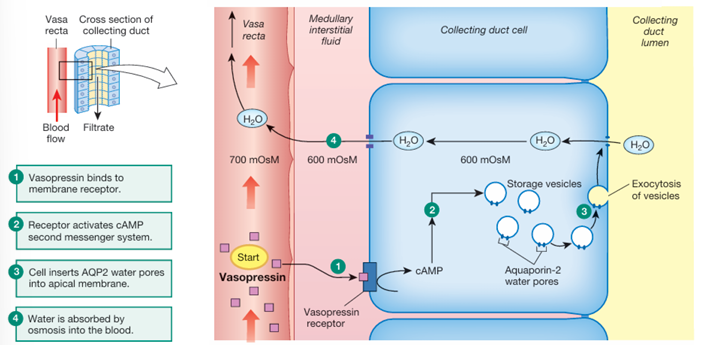
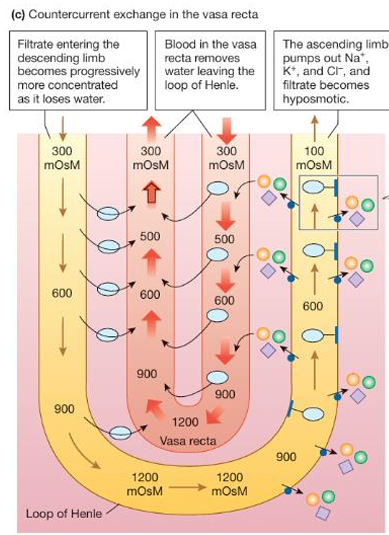
Whcih structures form the countercurrent exchange system?
the anatomical arrangement of the loop of Henle and its associated blood vessels, the vasa recta.
What does the countercurrent exchange system require?
it requires arterial and venous blood vessel that pass very close to each other, with their fluid moving in the opposite direction.
This arrangements allows the passive transfer of heat or molecules from one vessel to the other in tails and other limbs that are poorly insulated.
How does the countercurrent exchange system in the kidney contribute to solute concentration in the interstitium?
The countercurrent exchange system in the kidney transfers water and solutes, without losing them to the environment, since the kidney is a closed system. Solutes become concentrated in the interstitium, a process enhanced by the active transport of solutes out of the ascending limb of the loop of Henle, which increases extracellular fluid (ECF) osmolarity.
What is the countercurrent multiplier?
a countercurrent exchange system in which exchange is enhanced by actve transport
What are the 2 components of the countercurrent multiplier?
the loop of Henle
peritubular capillaries — vasa recta. they form a hairpin loop that acts as a countercurrent exchanger
How does filtrate concentration change as it moves through the loop of Henle, and what roles do the descending and ascending limbs play in this process?
Isosmotic filtrate (~300 mOsM) from the proximal tubule enters the descending limb of the loop of Henle.
The descending limb is permeable to water but not to solutes. Water leaves the tubule by osmosis into the increasingly concentrated medullary interstitial fluid.
As water exits, the filtrate becomes more concentrated, reaching up to 1200 mOsM at the tip of the loop.
Filtrate rounds the hairpin turn and enters the ascending limb, which is impermeable to water.
In the ascending limb, Na⁺, K⁺, and Cl⁻ are actively transported out of the tubule into the interstitial fluid.
As solutes are removed but water stays in the tubule, the filtrate becomes progressively more dilute, reaching about 100 mOsM by the time it enters the cortex.
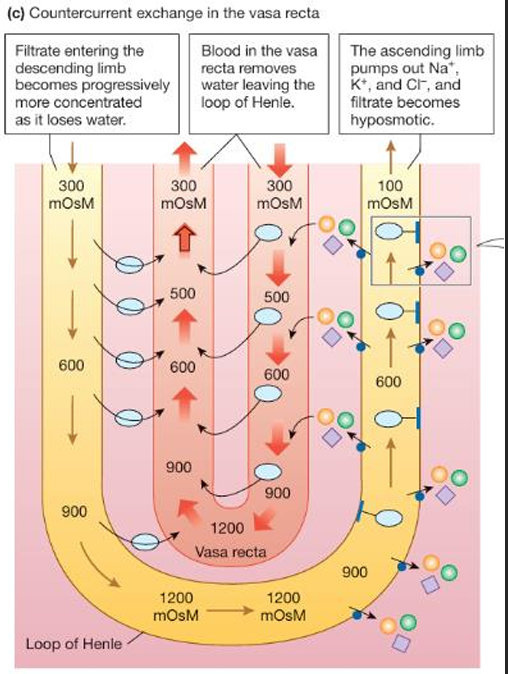
What is the net result of the countercurrent multiplier in the kidney?
to produce hyperosmotic interstitial fluid in the medulla and hyposmotic filtrate leaving the loop of Henle
How does the NKCC symporter function in the ascending limb of the loop of Henle?
The NKCC symporter uses the energy from the Na⁺ concentration gradient to transport Na⁺, K⁺, and 2 Cl⁻ ions from the tubule lumen into epithelial cells of the ascending limb. On the basolateral side, the Na⁺-K⁺-ATPase pumps Na⁺ out of the cells, while K⁺ and Cl⁻ exit through cotransport proteins or channels.
What role does the vasa recta play in maintaining the concentration of the medullary interstitial fluid?
The vasa recta, closely associated with the loop of Henle, acts as a countercurrent exchanger.
It removes water that leaves the tubule when there is an osmotic gradient, preventing the medullary interstitial fluid from being diluted. By carrying away this water, the vasa recta helps maintain the high solute concentration in the medulla, which is essential for concentrating urine.
How does urea contribute to the high osmolarity of the medullary interstitium, and what mechanisms facilitate its movement?
Urea contributes nearly half of the solute concentration in the medullary interstitium, increasing its osmolarity.
Its movement is facilitated by membrane transporters in the collecting duct and loops of Henle, including facilitated diffusion carriers and Na⁺-dependent secondary active transporters, which help concentrate urea in the medullary interstitium.
How does the body keep the ECF Na+ concentration at 140 mOsM?
by adding water when the mOsM is higher than 140 mOsM, and removing water when the mOsM is lower than 140 mOsM.
We would have to add 0.1 liter of water for each liter of ECF volume to compensate for the addition of Na+. So if normal ECF volume is 14 liters, we would have to add 1.4L.
for example:
155 mOsM / X liters = 140mOsM/ liter
X = 1.1 liters
What happens to body cells when NaCl is added to the extracellular fluid (ECF) and plasma osmolarity increases?
The higher osmolarity draws water out of the cells and into the ECF, causing the cells to shrink and disrupting their normal function.
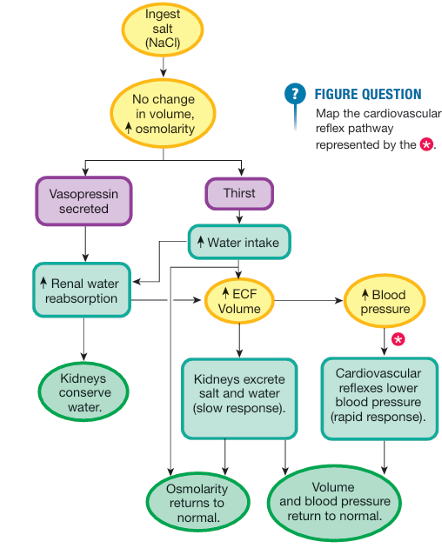
What is the homeostatic pathway for Na+?
addition of NaCl raises the osmolarity
two responses are triggered:
(1) vasopressin secretion → the kineys conserve water and concentrate the urine
(2) thirst → increases fluid intake, decreases osmolarity.
these increases then trigger another series of control pathways,w hich bring the ECF volume, blood pressure, and total body osmolarity back into a normal range by excreting extra salt and water
What happens to sodium and chloride balance during conditions like vomiting, diarrhea, or heavy sweating, and how does the body respond?
During vomiting, diarrhea, or heavy sweating, the body loses significant amounts of Na⁺ and Cl⁻ through nonrenal routes.
The stimuli that set the Na+ balance pathway in motion are more closely tied to blood volume and blood pressure than to Na+ levels.
The kidneys respond by regulating Na⁺ reabsorption, Chloride typically follows Na⁺ during reabsorption, either through electrochemical gradients or specific transporters like the NKCC in the loop of Henle and the Na⁺-Cl⁻ symporter in the distal tubule.
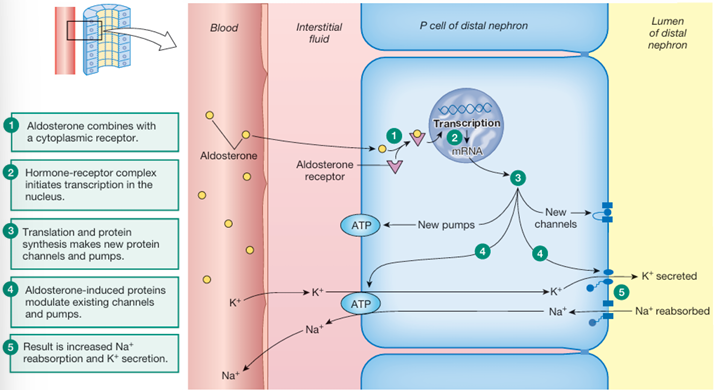
What is the function of aldosterone?
regulated the reabsorption of Na+ in the distal tubules and collecting ducts of the kidney.
The more aldosterone the more Na+ reabsorption.
Aldosterone is synthesized in the adrenal cortex and secreted in the blood and transported on a protein carrier to its target.
What is the primary site and target of aldosteron?
The primary site for aldosterone action is the last third of the distal tubule and the portion of the collecting duct.
The primary target of aldosterone is principal cells(P cells), with Na+-K+-ATPase, pumps on the basolateral membrane and various channels and transporters on the apical membrane(leak channels for Na+ and K+).
What is the molecular mechanims aldosterone elicits?
aldosterone enters P cells by diffusion
aldosterone comines with a cytoplasmatic receptor
there are 2 phases:
early response phase → apical Na+ and K+ channels increase their open time and existing channels are inserted into the apical membrane
slower response → newly synthesized channels and pumps are inserted into the epithelial cell membranes
intracellular Na+ levels rise from apical entry. Na+ -K+ -ATPase pump speeds up the transporting of cytoplasmic Na+ into the ECF and bringing K+ from the ECF into the P cells
this results in a rapid increase in Na+ reabsorption and K+ secretion
Why does water not automatically follow Na+ reabsorption in the distal tubule?
because vasopressin must be present to make the distal nephron permeable to water.
Which 2 stimuli increase aldesterone secretion?
increased extracellular K+ concentration — acts directly on the adrenal cortex
decreased blood pressure — initiates a complex pathway that results in the release of angiotensin II, which stimulates aldosterone secretion

How does the The RAS(renin-angiotensin) pathway maintain blood pressure?
low blood pressure:
Juxtaglomerular granular cells in the afferent arterioles of a nephron secrete renin
renin converts angiotensinogen into angiotensin I
ANG encounters enzyme angiotensin-converting enzyme(ACE), and ANG I is converted into ANG II
ANG II in the blood reaches the adrenal gland, which causes synthesis of aldosterone
at the distal nephron, aldosterone initiates the intracellular reactions that cause the tubules to reabsorb Na+
What are the stimuli that begin the RAS pathway?
granular cells that are directly sensitive to blood pressure — they respond to low blood pressure in the renal arterioles by secreting renin
sympathetic neuons — activated by the cardiovascular control center when blood pressure decreases, terminate on the granular cells and stimulate renin secretion.
paracrine feedback — stimulates renin release
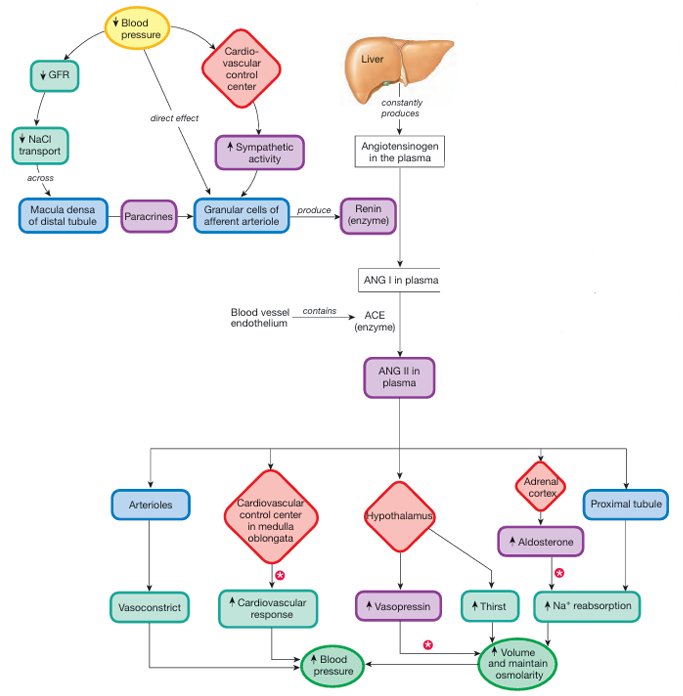
explain this pathway
Trigger: Low Blood Pressure
Initial Responses:
↓ Blood Pressure → ↓ GFR (Glomerular Filtration Rate)
→ ↓ NaCl transport across the macula densa in the distal tubuleMacula densa cells signal nearby granular cells (in afferent arteriole) via paracrines
Simultaneously, baroreceptors detect ↓ blood pressure → activate the cardiovascular control center in the brainstem
→ ↑ Sympathetic activity → stimulates granular cellsGranular cells release renin, an enzyme
Hormonal Cascade:
Renin converts angiotensinogen (constantly produced by the liver) into Angiotensin I (ANG I)
ANG I is converted to Angiotensin II (ANG II) by ACE (angiotensin-converting enzyme) found in blood vessel endothelium
Actions of Angiotensin II (ANG II):
Arterioles: → Vasoconstriction → ↑ blood pressure
Cardiovascular control center (medulla): → ↑ sympathetic output → ↑ cardiac output → ↑ BP
Hypothalamus:
↑ Vasopressin (ADH) → water reabsorption in kidneys
↑ Thirst → ↑ water intake → ↑ blood volume
Adrenal cortex:
Releases aldosterone, which acts on the proximal tubule to ↑ Na⁺ reabsorption
→ water follows → ↑ volume
Final Outcome:
Increase blood pressure
Restore fluid volume
Maintain osmolarity
ANG II increases blood pressure both directly and indirectly through which 6 pathways?
stimulating aldosterone secretion
increases vasopressin secretion — ANG II receptors in the hypothalamus initiate this reflex. Fluid retention in the kidney under the influence of vasopressin helps conserve blood volume, thereby maintaining blood pressure.
stimulates thirst
vasocontriction — causes blood pressure to increase without a change in blood volume
Activation of ANG II receptors in the cardiovascular control center, increases sympathetic output to the heart and blood vessels. Sympathetic stimulation increases cardiac output and vasoconstriction, both of which increase blood pressure.
ANG II increases proximal tubule Na + reabsorption. ANG II stimulates the apical Na+ H+ exchanger (NHE). Sodium reabsorption in the proximal tubule is followed by water reabsorption, so the net effect is reabsorption of isosmotic fluid, conserving volume.
What is the effect of ACE inhibitors?
ACE inhibitors, block the ACE-mediated conversion of ANG I to ANG II, thereby helping to relax blood vessels and lower blood pressure. This also means less aldosterone release, a decrease in Na+ reabsorption and a decrease in ECF volume. Contributing to lowering blood pressure.
What is the effect of renin inhibitors?
decrease plasma activity of renin, which in turn block production of ANG I and inhibits the entire RAS pathway.
What is natriuresis?
the urinary Na+ loss
What is Atrial natriuretic peptide(ANP)?
a peptide hormone that is produced in specialized myocardinal cells primarily in the atria.
ANP is synthesized a part of a large prohormone that is cleaved into several active hormone fragments.
What is brain natriuretic peptide(BNP)?
an hormone synthesized by ventricular myocaridal cells and certain brain neurons
What is the function of ANP?
it enhances the Na+ and water excretion, to decrease blood volume
What triggers the release of natriuretic peptides like ANP, and what is their systemic effect?
Natriuretic peptides are released when myocardial cells stretch due to increased blood volume (especially atrial stretch). They work via a cGMP second messenger system to promote Na⁺ and water excretion, reducing blood volume.
On which sites does ANP act?
in the kidney it dilates the afferent arterioles(increasing GFR), and decreases Na+ reabsorption in the collecting duct
act indirectly to increase Na+ and water secretion by supressing the release of; renin, aldosterone, and vasopressin
act directly on the cardiovascular control center of the medulla to lower the blood pressure
K+ is reabsorbed in the … and the … of the loop and may be secreted in the … .
K+ is reabsorbed in the proximal tubule and the ascending limb of the loop and may be secreted in the collecting duct.
How does the body compensate when its in hyperkalemia(increased K+ plasma concentration)?
Hyperkalemia acts directly on the adrenal cortex to promote aldosterone secretion, which act on the P cells in the distal nephrons. these ceel keep the cell's apical ion channels open longer and speeds up the Na+ -K+-ATPase, increasing the renal excretion of K+
If plasma K+ concentrations decrease, the concentration gradient between the cell and the ECF becomes … , … K+ leaves the cell, and the resting membrane potential becomes more … .
If plasma K+ concentrations decrease, the concentration gradient between the cell and the ECF becomes larger, more K+ leaves the cell, and the resting membrane potential becomes more negative.
If ECF K+ concentrations increase, the concentration gradient … and more K+ … in the cell, … it.
If ECF K+ concentrations increase, the concentration gradient decreases and more K+ remains in the cell, depolarizing it.
Why does hypokalemia cause muscle weakness?
hypokalemia causes muscle weakness because it is more difficult for hyperpolarized neurons and muscles to fire action potentials.
Why is hyperkalemia a dangerous potassium disturbance?
Because in this case depolarization of excitable tissues makes them more excitable initially.
Subsequently, the cells are unable to repolarize fully and actually become less excitable. In this state, they have action potentials that are either smaller than normal or non-existent.
Cardiac muscle excitability affected by changes in plasma K+ can lead to life-threatening cardiac arrhythmias.
What is thirst?
the urge associated with fluid balance.
it is the only way to restore lost water
What is salt appetite?
the craving for salty food that occurs when plasma Na+ concentrations drop.
salt appetide is linked to aldesterone and angiotensin, hormones that regulate the Na+ balance
What is the homeostatic response to increased osmolarity and increased volume?
excretion of hypertonic urine
What is the homeostatic response to increased volume and no change in osmolarity?
excretion of isotonic urine whose volume equal that of ingested fluid
What is the homeostatic response to increased volume and decreased osmolarity?
excrete very dilute urine to maximize water loss while conserving salts — this compensation is imperfect, because the urinary output cannot match the input
What is the homeostatic response to no change in volume and increased osmolarity?
intense thirst, whcih prompts ingestion of water to dilute the added solute.
the kidneys help by creating concentated urine of minimal volume, conserving water while removing excess NaCl
What is the homeostatic response to no change in volume and decrease in osmolarity?
the decreased volume resulting from the dehydration is corrected, but the replacement fluid has no solutes to replace those lost.
What is the homeostatic response to decreased volume and increased osmolarity?
blood volume is decreased to the point that the heart can no longer pump blood effectively to the brain. cell shrinkage is caused by increased osmolarity, which disrupts cell function
in severe dehydration the cortex gets 2 opposing signals:
secrete aldosterone
do not secrete aldosterone
What is the homeostatic response to decreased volume and no change in osmolarity?
no homeostatic response
blood loss represents the loss of isosmotic fluid from the extracellular compartment. If a blood transfusion is not immediately available, the best replacement solution is one that is isosmotic and remains in the ECF, like NaCl
What is the homeostatic response to decreased volume and decreased osmolarity?
is uncommon, but might be the result from incomplete compensation of dehydration.
no homeostatic response
In severe dehydration(decrease in volume and increase in osmolarity), compensatory mechanisms are aimed at restoring normal blood pressure, ECF volume and osmolarity by?
conserving fluid to prevent additional loss
triggering cardiovascular reflexes to increase blood pressure
stimulating thrist so that normal fluid volume and osmolarity can be restored
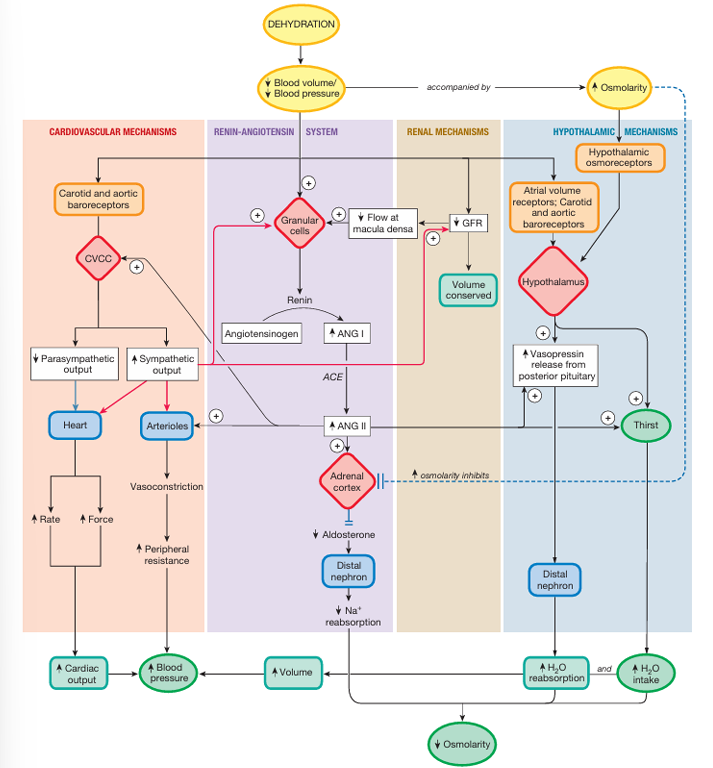
explain this pathway
The carotid and aortic baroreceptors signal the cardiovascular control center(CVCC) to raise blood pressure: sympathetic output from the CVCC increases while parasympathetic output decreases.
(1) The heart rate goes up as control of the SA node shifts from predominantly parasympathetic to sympathetic
(2) The force of ventricular contraction also increases under sympathetic stimulation. The increased force of contraction combined with increased heart rate to increase cardiac output.
(3) Simultaneously, sympathetic input causes arteriolar vasoconstriction increasing peripheral resistance.
(4) Sympathetic vasoconstriction of afferent arterioles in the kidneys decreases GFR, conserving fluid
(5) Increased sympathetic activity at the granular cells of the kidneys increases renin secretion.
Decreased peripheral blood pressure directly decreases GFR. A lower GFR conserves ECF volume by filtering less fluid into the nephron
Paracrine feedback causes the granular cells to release renin. Lower GFR decreased f luid flow past the macula densa. This triggers renin release
Granular cells respond to decreased blood pressure by releasing renin. The combination of decreased blood pressure, increased sympathetic input onto granular cells, and signals from the macula densa stimulated renin release and ensures increased production of ANG II.
Decreased blood pressure, decreased blood volume, increased osmolarity, and increased ANG II production all stimulate vasopressin and the thirst centers of the hypothalamus.
What is the function of diuretics?
decrease the ion reabsorption in the ascending limb of the loop of Henle or in the distal concoluted tubule, causing additional water excretion along with the un-reabsorbed ions.
What are the 3 mechanims the body uses to cope with pH changes?
buffers → Buffers are the first line of defense, always present and waiting to prevent wide swings in pH
ventilation → Ventilation, the second line of defense, is a rapid, reflexively controlled response that can take care of 75% of most pH disturbances
renal regulation → They are slower than buffers or the lungs but are very effective at coping with any remaining pH disturbance under normal conditions.
of H+ and HCO3-
Why are proteins sensitive for pH changes?
Intracellular proteins are particularly sensitive to pH because the function of these proteins depends on their three-dimensional shape.
Changes in H+ concentration alter the tertiary structure of proteins by interacting with hydrogen bonds in the molecules, disrupting the proteins’ three-dimensional structures and activities.
Abnormal pH may significantly affect the activity of the nervous system.
What is acidosis, and what is its result?
the pH is too low
neurons become less excitable and CNS depression results
What is alkalosis, and what is its result?
The pH is too high
neurons become hyperexcitable, firing action potenitals at the slightest signal
Why are disturbances inn Acid-base associated with disturbances in K+ balance?
this is partly due to the renal transporter that moves K+ and H+ ions in an antport fashion.
In acidosis, the kidneys excrete H+ and reabsorb K+ using an H+-K+-ATPase.
In alkalosis, the kidneys reabsorb H+ and excrete K+ .
What are the reflex pathways and cellular machanims involved in respiratory compensation of pH changes?
high plasma H+(carotid and aortic chemoreceptors) and PCO2(central chemoreceptors)
activate the respiratory control centers in the medulla, increasing the action potentials in somatic motor neurons
this works on the muscles of ventilation — increasing the rate and depth of breathing
this decreases PCO2, which causes a decrease in H+
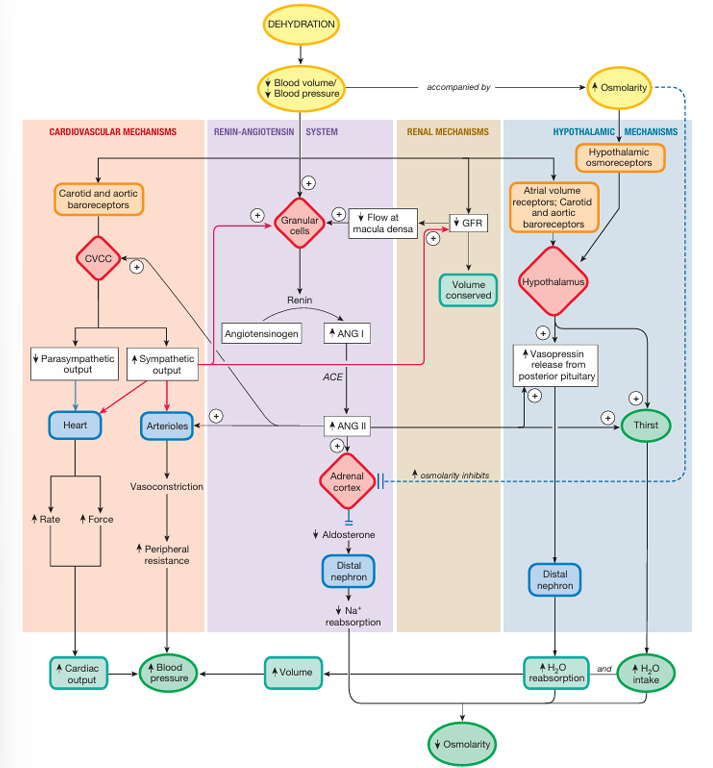
What does carbonic anhydrase do?
it catalyzes the conversion of CO2 and H2O to H2CO2, which then falls apart in H+ and HCO3-
What is a buffer?
a molecule that moderates but does not prevent changes in pH by combining with or releasing H+.
Intracellular buffers include;
cellular proteins,
phosphate ions (HPO4 2- ),
hemoglobin → buffers the H+ produced by the reaction of CO2 with H2O. Each H+ ion buffered by hemoglobin leaves a matching bicarbonate ion inside the red blood cell. This HCO3 - can then leave the red blood cell in exchange for plasma Cl- , the chloride shift.
What is the chloride shift?
The movement of HCO3- out of the red blood cell in exchange for plasma Cl-.
What is the cause respiratory acidosis?
occurs when alveolar hypoventilationr esults in CO2 retention and elevated plasma PCO2.
Plasma CO2 levels increase, leading to elevated H+ and HCO3-. this causes a decrease in pH
How is respiratory acidosis compensated?
by renal mechanisms that excrete H+ and reabsorb HCO3-

What is metabolic acidosis?
a disturbance of mass balance that occurs when the dietary intake and metabolic input of H+ exceeds H+ excretion.
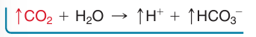
How is metabolic acidosis compensated?
via respiratory compensation, which causes PCO2 to decrease to normal or even below-normal levels du to hyperventilation.
via renal compensation, which causes secretion of H+ and reabsorption of HCO3-
What is Respiratory Alkalosis?
occurs as a result of hyperventilation, when alveolar ventilation increases without a matching increase in metabolic CO2 production.
How does the body compensate for Respiratory Alkalosis?
via renal compensation, by not reabsorbing HCO3- in the proximal tubules and secreting it in the distal nephron.
The combination of HCO3- excretion and H+ reabsorption in the distal nephron decreases the body’s HCO3- buffer load and increases its H+
What are the 2 common causes for metabolic alkalosis?
excessive vomiting of acidic stomach contents
excessive ingestion of bicarbonate-containing antacids
in both cases H+ concentration is reduced
How does the body compensate for metabolic alkalosis?
resperitory compensation — via hypoventilation, which increases the PCO2 and so creating more H+ and HCO3-. This respiratory compensation helps correct the pH problem but elevates HCO3- levels even more.
renal response → HCO3- is excreted and H+ is reabsorbed
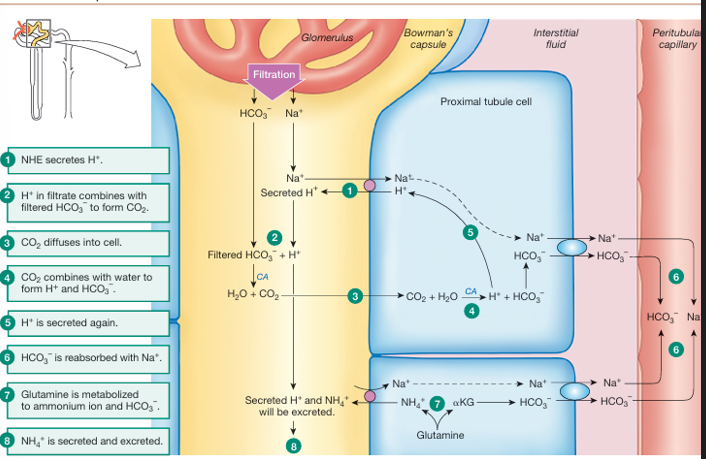
How does the kidney compensate for a too low pH?
the apical Na+-H+ exchanger(NHE) secretes H+ into the tubule
H+ in the filtrate combines with filtered HCO3- to form CO2
CO2 diffuses into the cell
CO2 combines with water to form H+ and HCO3-
H+ is secreted again
HCO3- is reabsorbed with Na+ (basolateral Na+-HCO3 - symporter)
in another (linked) pathway:
glutamine is metabolized to ammonium ion and HCO3-
NH4+ is secreted and excreted
Which two urinary buffers trap large amounts of secreted H⁺?
Ammonia (NH₃) from amino acids → forms NH₄⁺
Phosphate (HPO₄²⁻) → forms H₂PO₄⁻
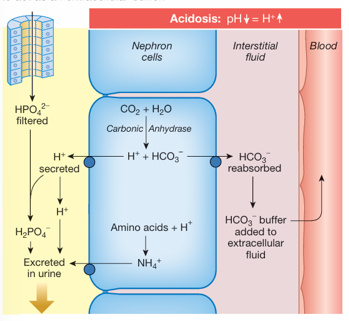
While excreting H⁺, what new ion do kidneys generate and reabsorb, and why?
They make new HCO₃⁻ from CO₂ and H₂O and reabsorb it into the blood to buffer H⁺ and raise systemic pH.
When are Type A intercalated cells active and what is their function?
during acidosis
they secrete H+ and reabsorb HCO3-
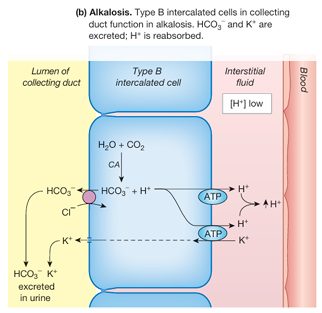
When are Type B intercalated cells active and what is their function?
during alkalosis
they secrete HCO3- and reabsorb H+