Clinical Oncology - Head and Neck Cancer
1/196
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
197 Terms
Is head and neck cancer more common in females or males?
Incident rates for men are more than twice as high than for women
Which head and neck cancer is more common in females?
Post-cricoid cancer
What is the most common site for distant metastasis?
Lungs
What are the other sites of distant metastasis?
Bones, brain, mediastinal lymph nodes, liver
The incidence of distant metastasis is greatest with tumour of the:
Nasopharynx and hypo-pharynx

A direct correlation appears to exist between __________ and the development of of distant metastasis
the bulk of cervical lymph node disease
What are high grade parotid tumours known for?
To involve facial nerves and cause paralysis
What is the leading cause of death in early stage tumours of the head and neck? What research has come out regarding this cause?
Secondary primary tumours; research on adjuvant chemotherapy to prevent secondary primary tumours is ongoing
What cancer of the head and neck is increasing in incidence in white men and women?
Oropharyngeal cancer associated with HPV infection
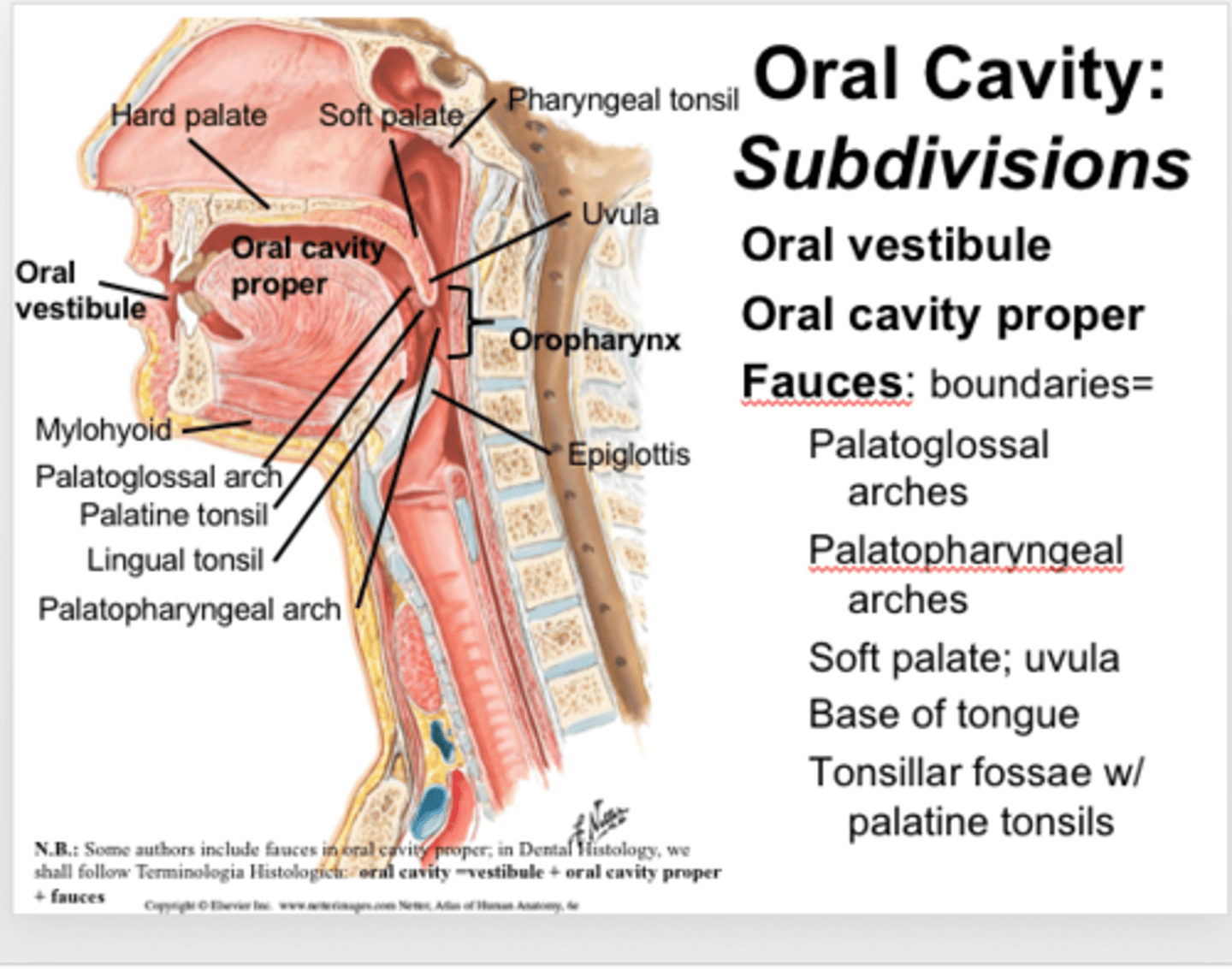
What is included in the oropharynx?
Tonsils, base of tongue, soft palate, oropharyngeal walls and the uvula
Which cancer is uncommon in US but common in Asia (Hong Kong, China, southeast Asia)?
Nasopharyngeal cancer
Why is nasopharyngeal cancer more common in Asia?
It may be due to environmental factors, as there is a decreased incidence of nasopharyngeal cancer in generations of Chinese born Americans
What head and neck cancer is more common in India?
Tumours of the base of tongue and oral cavity, which indicates environmental and cultural factors
What are the etiological factors for head and neck cancer?
Tobacco and alcohol use
Viral infections
Ultraviolet light
Radiation exposure
Diet
Marijuana
Dentures, fillings, and poor oral hygiene
Genetics
Consumption of alcohol and tobacco incur the highest risk for cancers of the:
Oral cavity, oropharynx, hypopharynx, larynx
What are oropharynx tumours close to the esophagus associated with?
Pooling of saliva carrying carcinogens related to tobacco
Alcohol consumption is a risk factor for the development of:
Pharyngeal and laryngeal cancer
Etiology - Occupational Exposures
Nickel refining
Furniture and woodworking: larynx, nasal cavity, paranasal sinuses
Steel and textile work: oral cancer
Exposure to dust, fumes, formaldehyde: NPC
Carpenters and sawmill workers: adenocarinoma of nasal cavity and ethmoid sinuses
Etiology - Radiation Exposure
Exposure to radiation, especially in childhood, may be associated with thyroid and salivary gland tumours
What viruses are associated with the development of head and neck cancer?
Epstein-Barr virus, Herpes simplex virus (HSV-1), HPV
Carcinomas of the ___ have been found to have a high prevalence of HPV DNA
tonsil, tongue, and floor of mouth
Etiology - Diet
Nutritional deficiencies (A and E) may be associated with hypopharyngeal cancer, especially in alcoholics and females. Nasopharyngeal cancer has been associated with salted fish.
Etiology - Genetics
Bloom syndrome and Li-Fraumeni syndrome
Morbidity of treatment increases and prognosis decreases as affected area progresses from _____ to ______
back of lips to hypopharynx, excluding the larynx
What indicates poor prognosis?
Vascular invasion, non-SCCs, extent of lymph node involvement, presence of cervical metastases, endophytic growth (invasion of lamina propria and submucosa),
What can result from enlargement of adenoid/pharyngeal tonsil?
Obstruction of upper air passage and allows breathing only through the mouth
What is the function of tonsils?
1. Lymphoid tissue that provide protection against airway infections
2. Form barrier between respiratory tubes (nasopharynx) and digestive tubes (oropharynx, hypopharynx)
Where is the first cervical vertebrae (C1)?
Inferior margin of nasopharynx
What does C2 contain?
Oropharynx
What is C4 in line with?
True vocal cords
What can salivary gland tumours involve?
Facial nerves, major cranial nerves, arterial neck blood flow, several lymph node groups
Lymphatic drainage is mainly _____
ipsilateral
Which structures have bilateral drainage?
Soft palate, tonsils, base of tongue, posterior pharyngeal walls, nasopharynx
Which structures have few or no lymphatic vessels?
True vocal cord, paranasal sinuses, middle ear
What are endophytic tumours?
More aggressive in spread and harder to control locally
What are exophytic tumours?
Noninvasive neoplasms characterized by raised, elevated borders
What is a common symptom that head and neck patients report?
60% of patients report otalgia (ear pain)
What is a common symptom in oral cavity tumours?
Swelling or ulcer that fails to heal. Localized pain is considered a symptom of advanced disease.
What are common symptoms in oropharynx tumours?
Painful swallowing, sore throat and referred otalgia
What are common symptoms of nasopharynx tumours?
Bloody discharge, difficulty with hearing, neck mass from metastatic adenopathy
What are common symptoms of laryngeal tumours?
Persistent sore throat, hoarseness and stridor
What are common symptoms of hypoharynx tumours?
Sore throat, odynophagia, and painful neck nodes. Up to 25% of cases present with a neck mass only. Dysphagia and weight loss are common symptoms of advanced disease.
What are common symptoms of tumours of nose/sinuses?
Obstruction, discharge, facial pain, diplopia, local swelling
What is a common site of metastases from the oral cavity, oropharynx or hypopharynx?
Subdigastric nodes
What nodes frequently arise from tumours found in the salivary glands?
Preauricular nodes
What is associated with tumours of the hypopharynx, base of tongue, and larynx?
Midcervical neck mass
During a physical examination, what are characteristics of metastasis?
Nodes that are hard, greater than 1 cm, nontender, nonmobile, and raised
What is the most common pathology of head and neck cancer?
Squamous cell carcinoma
What is stage IVA, IVB, IVC?
Advanced resectable disease
Advanced unresectable disease
Advanced metastatic disease
What are contrast enhanced CT and MRI scans for?
To determine size and shape of tumour, better than a clinical evaluation
Why is the volume of irradiated fields large?
Due to risk of nodal spread
How common is recurrence in head and neck cancers?
High. More than 75% of all head and neck cancers recur locally or regionally.
How common is hematogenous spread?
Hematogenous spread below neck is rare, except in nasopharyngeal or parotid gland cancer
In nasopharyngeal cancer, which nodes are commonly positive?
Inferior cervical nodes are clinically positive in 6% to 23% of cases
How does metastatic spread occur in nasopharyngeal cancer?
Nasopharyngeal cancer with bilateral cervical node involvement has a 25% chance of spreading via blood to bone then lung
What are the goals of treatment?
Eradication of disease, maintenance of physiologic function, preservation of cosmetics
What are the major curative modalities for head and neck cancer?
Radiation therapy and surgery, with adjuvant chemotherapy for advanced stages
What treatment modality is typically indicated?
Radiation therapy, as tumours in the head and neck area are often inaccessible via surgery
What is the treatment modality for small lesions with negative nodes?
One modality - surgery or radiation therapy
What is the treatment modality for small lesions with involved nodes?
Surgery and radiation therapy for control
What is the treatment modality for large lesions (T3/4), extensive cervical node disease, or both?
Surgery, radiation therapy and chemotherapy
What is the use of surgery as treatment correlated to?
Possibility of en bloc resection, as partial resections involve high risk of recurrence. Wide margins (>2 cm) are usually needed.
What is also performed during surgery?
Biopsy of cervical nodes and lesions
When would surgery be the modality of choice?
Early stage oral cavity or floor mouth cancers with no clinically positive nodes or if risk of deep cervical node involvement is low
What are conventional curative surgeries?
Laser therapy, cryotherapy, electrocautery
What is an ideal case for surgery as palliative salvage therapy in the event of failure after radiation therapy?
If conventional treatment was done, as accelerated treatments result in severe acute toxic effects that often require feeding tube and mucosal healing that take months
What is the modality of choice for disease that has invaded bone? Why?
Surgery, as radiation therapy doses have high risk of necrosis
What is a radical neck dissection?
Removes lymph nodes from level I to V, sternocleidomastoid muscle, internal jugular vein, spinal accessory and 11th cranial nerve
What is the modified radical neck dissection?
Decreases morbidity by sparing sternocleidomastoid muscle, internal jugular vein, and 11th cranial nerve, depending on location of metastatic spread
What is wound healing impacted by?
Diminished blood supply, impaired collagen formation and increased risk of infection due to decreased leukocyte function
Why is there more caution with radiation and neck dissections?
High doses from radiation can cause decreased vascularity and fibrosis, and may likely result in healing complications
What is the role of chemotherapy in head and neck cancer?
Used for metastatic disease, locally recurrent disease, or salvage therapy when surgery and radiation therapy can no longer be used
What is the role of chemotherapy in nasopharyngeal cancer?
For advanced NPC, neoadjuvant chemotherapy can be used as a radio-sensitizer, or used adjuvantly after treatment
Which chemotherapy drug has the highest overall and complete remission rates?
Cisplatin containing drug combinations
What is the most common chemotherapy drug combination?
Cisplatin and 5-FU
What is a reason why chemotherapy may not be used?
When used concurrently with RT, it can increase severity of toxicities and complication rates - which is why it may not be used
How do we determine whether a patient receives concurrent or adjuvant chemotherapy?
For a fit patient, concurrent chemoradiation may be offered to maximize the chance to skip surgery and neoadjuvant chemotherapy may be used for borderline fit patients, as acute toxicity during RT is lower
How does proton beam radiation therapy minimize dose to surrounding tissues?
Protons deposit low energy when they enter the body and then there is a rapid increase in the deposit of energy (Bragg Peak), followed by a steep decrease in energy
How is PBRT beneficial for head and neck cancer?
It can spare OARs, contralateral areas, such as salivary glands, and can be used to irradiate recurrent disease
What is the standard course of treatment in the event of recurrence?
Surgery or chemotherapy. Radiation therapy is not used due to the higher rate of toxicities.
Can electron beams be used for head and neck cancers?
May be used to boost doses to superficial regions
What fractionation is used for SCCs with longer doubling times?
Standard fractionation (200 cGy, 5 days/week)
What fractionation is used for SCCs with shorter doubling times?
Accelerated hyperfractionation (120 cGy, twice daily)
What would the patient position be for treatment of the maxillary sinus/antrum?
Chin is extended to include the anterior aspect of maxillary sinus/antrum in the anterior field, without including the eyes
What techniques and immobilization would be used for post-operative patients? Why?
An electron boost field or bolus may be used, as tumour cells in surgical beds are less oxygenated and more radioresistant. Hence, higher doses are necessary.
What is the purpose of a tongue blade as an immobilization device?
Tongue blade may be inserted between incisor teeth to depress tongue if tumour invasion includes tongue to reduce superior border, displace tongue from treatment field (lesion is at anterior floor of mouth), or displace palate
What are the subdivisions of the oral cavity?
Anterior two-thirds of tongue, lips, buccal mucosa, lower and upper alveolar ridge, retromolar trigone, floor of mouth, hard palate
How is the clinical target volume defined in oral cavity cancer?
Pre-op diagnostic images, surgical and pathological findings, post-op changes on post-op CT scan
Is nodal and metastatic spread common in oral cavity cancer?
No, cervical lymph node involvement at time of presentation is uncommon and oral cavity cancers have the lowest incidence of nodal metastasis. Hematogenous spread occurs in fewer than 20% of patients.
What is the treatment for early stage and pre-malignant lesions in oral cavity cancer?
Surgery alone
When is surgery and radiation therapy indicated in oral cavity cancer?
Inadequate surgical margins and neck nodal involvement
In oral cavity cancer, is irradiation of the neck nodes involved?
If lesion has high rate of spread or history of bilateral spread via lymphatics
When do lesions of the oral cavity typically recur?
Most sites typically recur within 2 years and rarely after 5 years
What dose does gross disease of the oral cavity receive?
70 Gy
What volumes receive 64 Gy in oral cavity irradiation?
High risk of microscopic disease
High risk lymph nodes
What volumes receive 60 Gy in oral cavity irradiation?
Contralateral neck or low neck
What is included in the low-risk CTV in oral cavity irradiation?
Contralateral neck or low neck
How much dose does each volume receive if the patient is receiving 72 Gy in oral cavity irradiation?
72 Gy to primary lesion
66 Gy to high risk CTV
60 Gy to low risk CTV
Final 6 Gy delivered via electron beam
For patients who had neo-adjuvant chemotherapy for oral cavity cancer, what are the target volumes for radiation therapy?
Target volumes are defined from the original extent of the tumour
Describe the lymphatic drainage of the upper lips
Drain into buccal, parotid, upper cervical and submandibular nodes. It may cross midline to the submental and submandibular nodes of contralateral side.