Valvular regurgitation - mitral
1/80
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
81 Terms
Definition: MR
AKA
CAUSED BY
• Leaking of the mitral valve during systole from left ventricle to left atrium
• Also known as mitral insufficiency
• Due to incomplete closure of the mitral valve
decreased heart function causes what for regurge
decreased regurgitation but thick envelope
most common symptom of MR
MURMUR
Blowing
high pithed
holosystolic
cardiac apex radiates to axilla
MR can eventually lead to
Right heart failure due to backup in the pulmonary veins into the RA Increasing PAP
TOO MUCH VOLUME
Etiology MR: Causes (6)
• Primary Mitral Regurgitation
• Functional Mitral Regurgitation
• Flail mitral valve leaflet
• Papillary muscle rupture
• Left ventricle
- ischemia, infarction, cardiomyopathy
Mitral Valve Apparatus
MR Increases PRELOAD which causes the LV to become
hyperdynamic
WHAT VIEW IS MVP MITRAL VALVE PROLAPSE DIAGNOSED FROM ONLY!!!
PLAX!!! ONLY!!!
FLAIL MV
Severe regurgitation
leaflet fails to coap usually due to pap or chordae problem
leaflet goes back into LA
JET GOES IN DIRECTION OPPOSITE OF AFFECTED VALVE
Barlows syndrome
MV problems from fibrous disease
primary MR
Primary Mitral Regurgitation
problem with
problem with the leaflets
causes of primary MR (4)
o Mitral valve prolapse
o Endocarditis
o Rheumatic heart disease
o Mitral annular calcification
causes of Functional Mitral Regurgitation (4)
Ischemic mitral regurgitation due to ischemia or cardiomyopathy
Flail mitral valve leaflet
• Papillary muscle rupture
• Left ventricle - ischemia, infarction, cardiomyopathy
MV Apparatus
any problem with these will cause MR
• Left atrial wall
• Mitral annulus
• Anterior and posterior leaflets
• Chordae
• Papillary muscles
• Left ventricular myocardium underlying the papillary muscles (tenting)
• Normal closure of the valve is at the annulus
Auscultation / Heart sound MR
High-pitched, blowing holosystolic murmur
Diseases of MV (6)
Myxomastous Disease - MV Prolapse
Rheumatic Disease
Endocarditis
Marfan Syndrome
Ischemic MR
Pap muscle rupture
Myxomatous disease – Mitral Valve Prolapse (5)
o Thickened, redundant leaflets and chordae
o Excessive motion and sagging into the left atrium in systole
o Mitral valve prolapse – minimal leaflet displacement
o Flail mitral valve leaflet – severe leaflet displacement
o Mid systolic click and mid-to-late systolic murmur
Rheumatic Disease
Thickening of the leaflet tips and restricted motion
Endocarditis
Thickening of the leaflet tips and restricted motion
Marfan Syndrome
Long, redundant anterior leaflet that sags into the LA in systole
Ischemic MR
functional MR
Caused by
Relationship to MI
What happens with PAP rupture
what can happen to MV leaflets
due to:
results in _____ of leaflets
MR is due to:
MV
o Functional mitral regurgitation – the leaflets are normal – includes mitral regurgitation caused by ischemia and dilated cardiomyopathy
o Cause by papillary muscle displacement and dilation of the annulus
o Most common complication of an MI
o Severe mitral regurgitation can occur with papillary muscle rupture
o Tenting of the mitral valve leaflets (normal closure is at the annulus)
o Due to regional wall motion abnormalities or dysfunction
o Restricted leaflet motion – abnormal valve closure
o Results in apical displacement (“tenting”) and incomplete closure of the valve leaflets (normal mitral valve closure should be at the annulus)
o Mitral regurgitation is due to left ventricular distortion and annular dilation
o Mitral valve bend is caused by the basal chord
Papillary muscle rupture (Partial rupture of the papillary muscle)
Comlication of :
results in
prognosis
o Complication of an acute myocardial infarction
o Acute, severe mitral regurgitation
o Poor survival
Ischemic MR caused by (6)
PAP Muscle displacement and dilation of the annulus
PAP rupture
regional WMA
Restricted leaflet motion-abnormal valve closure
LV Distortion
Annular dilation
What is the MC complication of MI
Ischemic MR
Pap muscle rupture can cause
severe MR
`Where is normal closure of MV leaflet tips
Annulus
What is it called when the MV closes distal to the annulus
tenting
tenting is _______ displacement which causes:
apicical displacement which causes incomplete closure
MV Bend is caused by what
basal chord
MR is due to
LV Distortion & annular dilation
The response to chronic volume overload on a chamber is
dilation with normal pressure
The response to acute volume overload on a chamber is
no dilation with marked increase in pressure
The initial response of the left ventricle to mitral regurgitation is
LV becomes hyperdynamic
Chronic mitral regurgitation
progression
wall thickness
affect on systolic function
LA
PAP
o Progressive left ventricular dilation
o Normal left ventricular wall thickness
o Irreversible decrease in systolic function in the absence of symptoms
o Left atrium gradually dilates with normal left atrial pressure
o Pulmonary artery pressure increases
intermitant MR
Due to ischemia
pap displacement
comes back to normal when ischemia is corrected
Acute mitral regurgitation
LA
Size/pressure
o Normal left atrial size
o Significant increase in left atrial pressure
can result in flail MV Leaflet
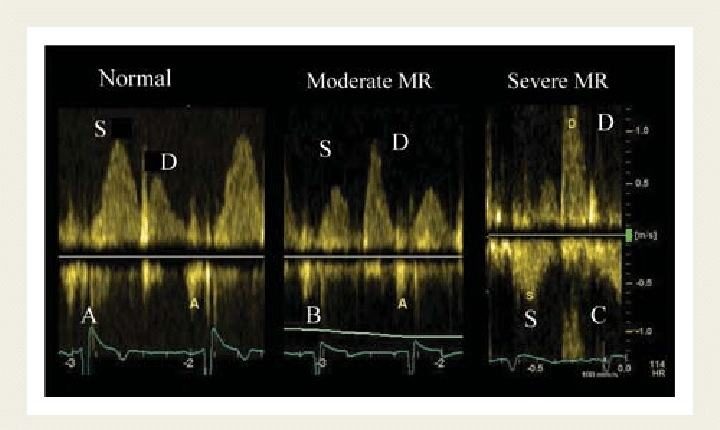
Two-Dimensional Evaluation: MR (5)
• Obtain careful, high-resolution imaging focusing on the mitral valve, chords and papillary muscles in both harmonics and fundamental modes in the parasternal and apical views
• Use magnification (zoom)
• Evaluate for flail mitral valve leaflet, mitral valve prolapse, mitral annular calcification
• Evaluate left atrial size
• Left Ventricle
How to evaluate LV 2D (3)
• Left Ventricle
o Evaluate left ventricular size and function - volume overload pattern
o Obtain end-systolic dimension
o Surgery needed with an end-systolic dimension greater than 45 mm and reduction in systolic function
Color Doppler Evaluation: (3)
color doppler jet
eccentric or central
vena contracta width
Color Doppler Jet Area
scale
settings
views
jet (2)
o Normal Color Doppler Nyquist Limit Setting: 50 – 60 cm/s
o Correct color Doppler gain
o Parasternal and apical views
o Length of mitral regurgitation jet
o Area of jet –
▪ Less than 20% of the left atrial area indicates mild mitral regurgitation
▪ Greater than 40% of the left atrial area indicates severe mitral regurgitation
o Area of jet –
▪ Less than 20% of the left atrial area indicates mild mitral regurgitation
▪ Greater than 40% of the left atrial area indicates severe mitral regurgitation
Eccentric or central
▪ The severity of mitral regurgitant jets that hug a wall is underestimated
– it is more severe than appears due to the Coanda Affect (the jet stays attached to the curved surface, i.e., left atrial wall).
▪ Henri-Marie Coanda – Romanian aerodynamicist
o Timing (early, mid, late) and duration
▪ Mitral valve prolapse will produce late systolic mitral regurgitation
Vena Contracta Width
where is the narrowest portion
what view
how to RES
mild
severe
o The narrowest portion of the color Doppler jet at the leaflet tips
o Parasternal long axis view - perpendicular to flow
o Magnify
o Mild = less than < 0.3 cm
o Severe = greater than 0.7 cm
Mitral Valve Inflow Doppler (LV Inflow)
o E velocity greater than 1.2 meters per second may indicate significant regurgitation with EF greater than 40%
o Deceleration time less than 150 milliseconds may indicate significant regurgitation
Continuous-Wave Doppler
o The jet is wider than the aortic stenosis jet – starts earlier
o More severe mitral regurgitation will produce a Doppler waveform that is complete and dark and triangular shaped
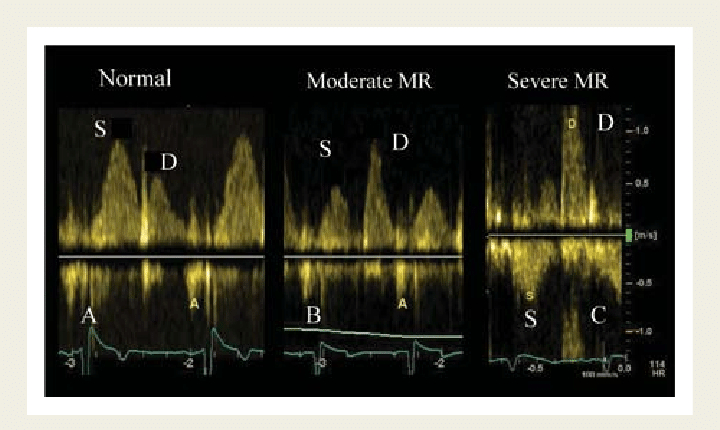
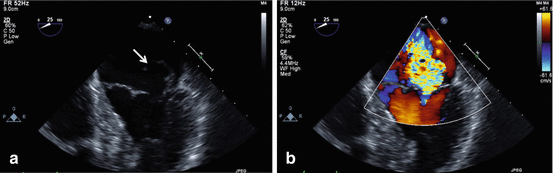
Pulmonary Venous Doppler
o Obtain color-guided pulsed-wave Doppler of the right upper (superior) pulmonary vein
o Lower color Doppler scale
o Increase color Doppler gain slightly
o Place sample volume
o Reduce wall filter
o Flow reversal in the right superior pulmonary vein is seen with severe mitral regurgitation
Proximal Iso-velocity Surface Area (PISA)
• Based on the concept that the flow proximal to the regurgitant orifice is equal to the flow through the regurgitant orifice
How to measure PISA
A4C or A3C
40 FPS
Zoom MV, Tight color box
Baseline towards jet
80 top #
30 bottom #
REMEMBER TO CHANGE IT BACK
Freeze mid systole 20 - 40 cm/s
Measure radius of aliasing velocity of vena contracta
scale set to ____ for MR Spectral doppler
6 m/s
What you need to measure: PISA
1. VTI of mitral regurgitation CW Doppler jet
2. PISA Radius
3. Aliasing Velocity
Procedure for PISA (5)
o Magnify on the color Doppler PISA
o Shift the color baseline downward (toward the jet) to decrease the color flow aliasing velocity (between 25 – 40 cm)
o Measure the radius of aliased region - the distance of the isovelocity shell from the orifice
o Note the alias velocity on the color bar (cm/s)
o VTI of mitral regurgitation continuous-wave Doppler jet (cm)
how to distringuish MR from Ao flow in Spectral doppler
TIMING!
MR ocurrs earlier than aortic flow
steep / fast deceleration time =
high pressure gradient
Regurgitant Volume (RV):
defintion
equations (3)
o the amount of blood that leaks back into the left atrium per beat o ml/beat
o RV = SVmr – SVlvot
o SV = CSA x VTI
o CSA = π(D/2)2 or 0.785 x (D)2
RV =
o RV = SVmr – SVlvot
SV =
SV = CSA x VTI
CSA = (2)
o CSA = π(D/2)²
or 0.785 x (D)²
Regurgitant Fraction (RF):
The percentage of blood that leaks back into the left atrium per beat
Regurgitant Orifice Area (ROA): def
The area (cm²) of the hole or defect through which the blood leaks
Regurgitant Orifice Area (ROA): eq
ROA = RV/VTIMR
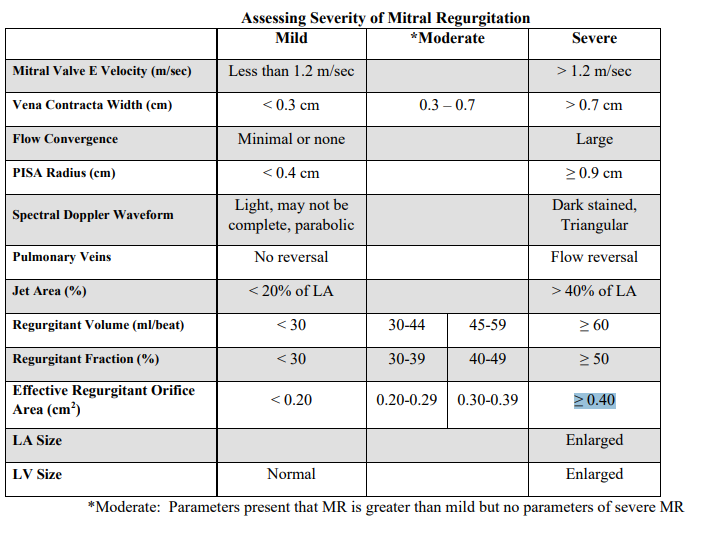
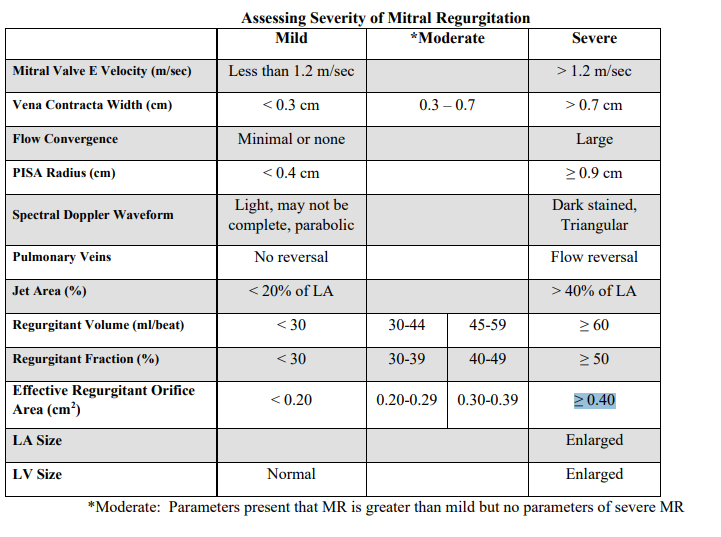
Mild Mitral Regurgitation:
• Jet area less than 20% of LA area
• Vena contracta width < 0.3 cm
• Very little or no flow convergence - PISA radius < 0.4 cm
• Light, not complete spectral Doppler signal
• Regurgitant Volume < 30 ml/beat
• Regurgitant Fraction <30% • Effective Regurg
Mitral E velocity (m/s)
mild
moderate
severe
mild
<1.3 m/s
moderate
severe
>1.2 m/s
Vena contracta width (cm)
mild
moderate
severe
mild
< 0.3 cm
moderate
0.3 - 0.7 cm
severe
>0.7 cm
Flow convergance
mild
moderate
severe
mild
minimal or none
moderate
severe
large
PISA Radius
mild
moderate
severe
mild
<0.4 cm
moderate
severe
≥ 0.9 cm
Spectral doppler waveform
mild
moderate
severe
mild
light, may not be complete, parabolic
moderate
severe
Dark stained, triangular
Pulmonary vein
mild
moderate
severe
mild
no reversal
moderate
severe
Flow reversal
Jet area %
mild
moderate
severe
mild
<20% of LA
moderate
severe
>40% of LA
Regurgitation volume (mL/beat)
mild
moderate (2)
severe
mild
<30 mL/beat
moderate
30 - 44 mL/beat
45 - 59 mL/beat
severe
>60 mL/beat
Regurgitation fraction (%)
mild
moderate (2)
severe
mild
< 30%
moderate
30 - 39%
40 - 49%
severe
≥ 50%
Effective regurgitation oriface area (cm²)
mild
moderate
severe
mild
< 0.20 cm²
moderate
0.20 - 0.29 cm²
0.30 - 0.39 cm²
severe
≥ 0.40 cm²
LA size
mild
moderate
severe
mild
moderate
severe
enlarged
LV Size
mild
moderate
severe
mild
Normal
moderate
severe
Englarged
Severe MR
• Increased inflow velocity – E wave greater than 1.2 meters per second
• Reversed systolic flow in pulmonary veins
• Dilated left atrium and left ventricle
• Hyperdynamic left ventricle
• Eventually will develop left ventricular dilation
• Color Doppler jet area greater than 40% of LA area
• Vena contracta width greater than 0.7 cm
• Large flow convergence (PISA radius) ≥ 0.9 cm (aliasing velocity at 40 cm/s)
• Dense spectral Doppler waveform, triangular-shaped spectral Doppler waveform
• Regurgitant Volume ≥ 60 ml/beat
• Regurgitant Fraction ≥ 50%
• Effective Regurgitant Orifice Area ≥ 0.40 cm2
when is surgery required for MR
End-systolic dimension >45 mm
AND
Reduced systolic function
surgical options for MR
Valve replacement
angioplasty / revascularization
valve repair
annular ring / annuloplasty
mitra clip
like a staple in the middle of the valve
2 jets but less regurgitation
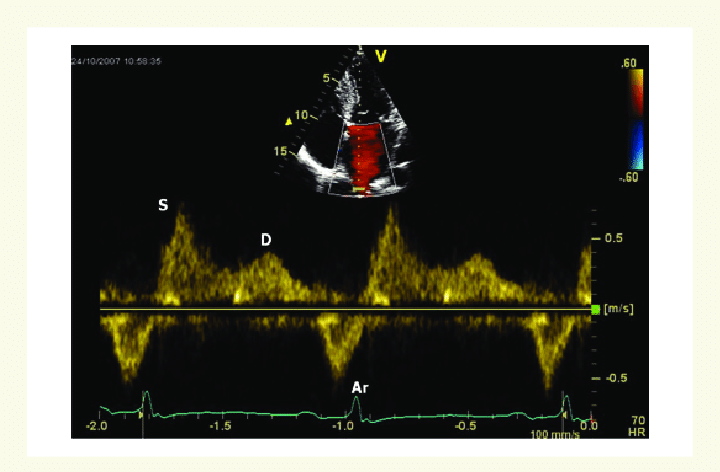
Normal PW doppler of pulmonary vein
systolic dominance
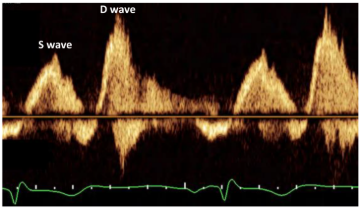
blunted systolic pulm vein flow
moderate
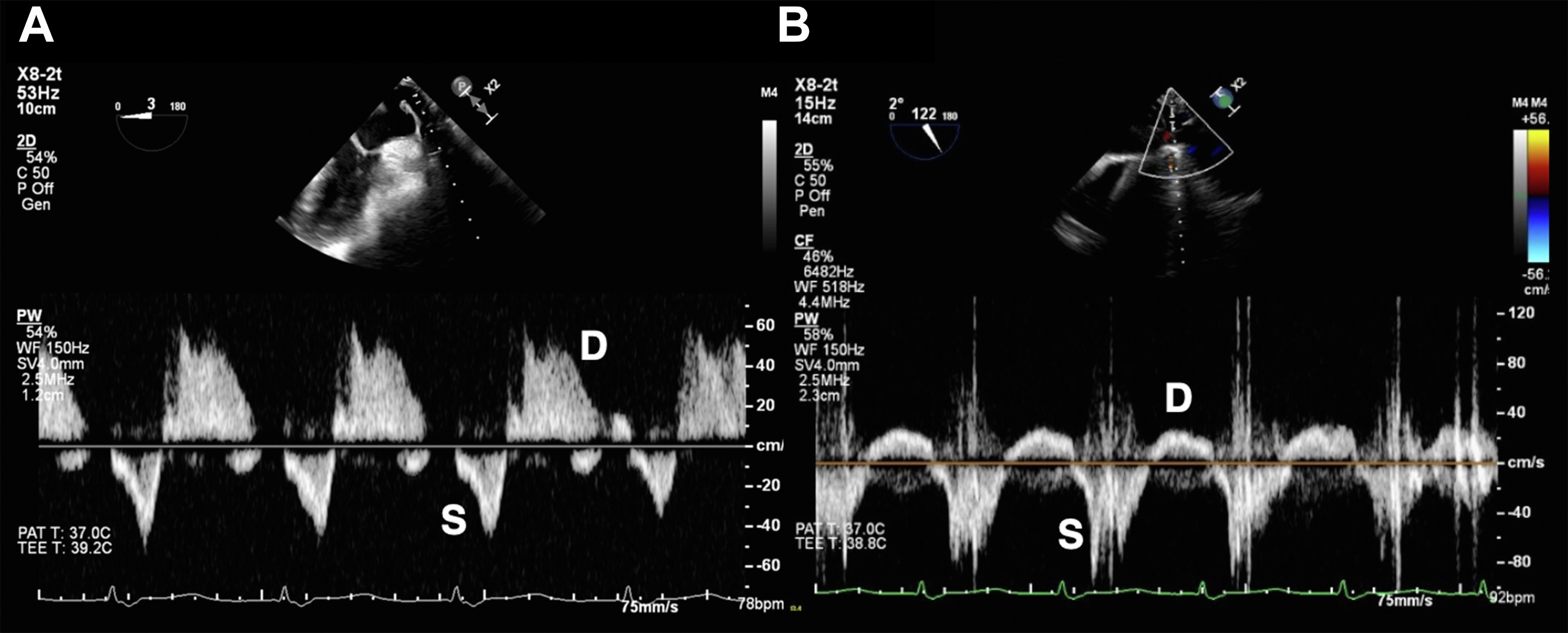
superior pulm vein flow reversal
BAD