Exam 4: Conditions of the Equine Large Intestines and Rectal Tears
1/69
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
70 Terms
what is the function of the large intestine and its relation to colic
cecum functions in fluid resorption and initiation of microbial digestion
large colon further functions in fluid resoprtion and digestion
majority of large intestinal colics are caused by non-strangulating lesions
overall improved prognosis for large intestinal lesions compared to small intestines
what are the common clinical signs of large intestinal colic
abdominal pain
decreased or absent borborygmi
large intestinal gas distension
tachycardia/tachypnea
toxic/injected MM
prolonged CRT
dehydrated
± fever
how is NG intubation used in large colon colic
should be performed on all horses displaying signs of colic
>2L of net reflux abnormal
reflux is uncommon in horses with primary large intestinal disease
secondary simple obstruction of SI can occur, gastric impactions secondary
how is a rectal exam used for large colon colic
ingesta in pelvic flexure, impaction?
gas distension, cecum vs colon vs both
nephrosplenic space
tight colonic bands
displaced large colon
what can be seen on transabdominal ultrasound
spleen/kidney location
colonic gas or fluid
colon wall edema
colonic vasculature
how might abdominocentesis present with large colon colic
gas distention may prevent collection
increased protein with non-strangulating obstruction could indicate need for surgical intervention
increased lactate = strangulating lesion
how might bloodwork present with large colon colic
results can be consistent with dehydration with colonic fluid shifts and SIRS/septic shock
increased lactate with dehydration and strangulating lesion
what are the major cecal conditions
cecal Tympany
cecal impaction
cecocecal intussusception
what is primary cecal tympany
gas colic
rapid gas distension due to high grain diet or lush pastures
reduced cecal motility
what is secondary cecal tympany
outflow obstruction due to impaction, displacement or torsion of the large colon
what is the etiology of cecal impaction
dietary factors
decreased exercise
NSAIDs
motility disturbances
tapeworm
what are the clinical signs and and rectal presentation of cecal impaction
low grade, intermittent pain
acute onset severe pain
signs consistent with GI perforation
can occur without having any signs of colic prior to rupture
rectal reveals doughy to firm impaction, severe cecal distention with gas and fluid
what is type 1 cecal impaction
form, dry impaction of feed material
fluid and gass usually pass over the impaction
most common
what is type 2 cecal impaction
cecal dysfunction and fluid distention
soft ingesta and fluid filled cecum
what are the complications of cecal impaction
compromised cecal wall, peritonitis from leakage
perforation
recurrence → unless has cecal motility dysfunction, not likely if management changes are made
how can you prevent recurrence of cecal impaction
use caution in resuming feeding
wait 2-4 days after impaction resolved, begin with small amounts of feed with increased water and decreased fiber
clean, fresh water
adequate exercise
surgical → cecal bypass
what is the prognosis of cecal impaction
31% horses referred died <24hrs
short term 81% medical, 95% surgical if recovered
long term 95% medical, 89% surgical
what is the etiology of cecal intussusception
unknown, suspected to be related to motility alterations
parasites such as tapeworms and cyathostomes
Salmonella a
what are the 3 forms of cecal intussusceptions
acute - severe abdominal pain
subacute-severe abdominal pain
chronic wasting form- mild intermittent pain, fever, reduced fecal output, and chronic weight loss
how is cecal intussuceptions diagnosed
can be difficult
rectal exam for firm mass
ultrasound
what are the major large colon conditions
feed impactions
sand impactions
enteroliths
displacements
volvulus
what are the common locations of large colon impaction
pelvic flexure extending into LVC and LDC
transverse colon extending into RDC
what are predisposing factors to large colon impaction
coarse feed
poor dentition
foreign materials or bedding
motility disturbances
parasites
recent management changes
surgery >1hr
MSK pain, NSAIDs
what are the clinical signs and rectal exam for large colon impaction
mild to marked intermittent pain, usually controllable with analgesics
normal MM color
HR 40-0
mild dehydration
decreased Broborygmi
rectal showing doughy to firm impaction ± gas distension
what might diagnostics real for large colon impaction
ultrasound showing presence of gas in the large intestine
increased PCV and TP due to dehydration
abdominal fluid usually WNL but may have increased TP and WBC if longstanding
how can large colon impactions be prevented?
dental care
dietary management using small frequent feedings of good quality roughage, minimize feeding of grain
ensure water intake
appropriate exercise
deny access to sand
bulk laxative in diet
appropriate anthelmintics
wha are the potential complications and prognosis of large colon impaction
recurrent colic
colonic rupture
thromophlebitis
diarrhea
overall prognosis is good, 40% have at least 1 recurrent episode
what is the etiology of sand impaction
short of non-existent grass
insufficient roughage in diet
feed on ground with sandy soil
sand in stalls or paddocks
geographic area
what are the clinical signs of sand impaction
intermittent, mild to severe pain
± diarrhea
HR variable 40-60
may have toxic MM
± dehydration
abdominal auscultation, may hear sand pouring
sand in feces
how does sand impaction present on diagnostics
rectal = firm impacted viscous, may not feel due to gas distention
US- small hyperechoic particles may be seen
Rads may see sand
abdominal fluid- WNL to mild increase in TP and WBC, be careful that ventral colon can be heavy with sand and enterocentesis can occur
what is the prognosis of sand impaction
good to excellent in most cases, but poor if colon ruptures
how can sand impaction be prevented
feed off the ground
maintain good quality pasture
use bulk laxative
-psyllium hydrophilic muciloid
-bran in intermittent feedingsdo not use sand in stalls or paddocks
what is enterilithiasis
mineral concretions that form in the colon, usually found around a nidus
precipitation of minerals
magnesium, ammonium, phosphate
age >4yrs, alfalfa hay feeding
what are the common locations of enterolithiasis
right dorsal colon
transverse colon
small colon
what are the clinical signs of enterolithiasis
history of intermittent abdominal pain with mild to moderate discomfort
hr 40-60
may have diarrhea
rectal exam has variable findings, from normal to being able to palpate the enterolith
what is the treatment and prognosis of enteroliths
surgery necessary to remove via enterotomy, presence of polyhedron shaped stone indicates >1
good prognosis unless necrosis of the bowel wall occurs at site
what are the kinds of large bowel displacements
right dorsal displacement
left dorsal displacement
pelvic flexure retroflexion
what are predisposing factors for large colon displacement
large colon is highly mobile
motility disturbances
parasites
large breed horse
recent foaling
describe right dorsal colon displacement
colon moves into a position between the cecum ad body wall
what are the signs of right colon displacement
variable pain and hr
lab findings typically WNL ± increased GGT
large colon gas distention, taut bands coursing horizontally or diagonally across abdomen
what is the prognosis of right colon displacement
usually good with appropriate and timely surgical intervention
describe left dorsal displacement
aka nephrosplenic entrapment
left colon moves dorsally and becomes entrapped between spleen and left kidney and hangs over the NS ligament
simple obstruction develops
what are typical findings of left dorsal displacement
mild to moderate pain, variable HR
lab typically WNL
gastric impactions may occur secondary
rectal shows large colon gas distention, taut and coursing toward nephrosplenic space, LC within the nephrosplenic space
cannot ultrasound left kidney
what is large colon volvulus
twisting of colon around its long axis
>270 results in lumen and vascular occlusion = strangulation
what is the etiology and risk factors of large colon volvulus
exact cause unknown
alterations in GI motility
changes in VFA content
electrolyte abnormalities
broodmare, <100days post partum increases risk
what are the clinical signs of large colon volvulus
varies with magnitude, as <180 signs similar to displacement but >270 more severe
HR 40-100
MM pale to purple
dehydration occurs rapidly
extreme abdominal distention
how does large colon volvulus present on rectal exam
tight distended large colon
colon may felt transversing the abdomen horizontally in the pelvic inlet
colon wall thickening
may be too painful or too distended to palpate
how does large colon volvulus present on ultrasound or abdominocentesis
colon wall edema, vessel dilation (right side)
may be too distended to collect fluid without risk of enterocentesis
what is the prognosis for large colon volvulus
guarded to poor
depended upon duration prior to surgical correction
improved prognosis if diagnosed and treated quickly, up to 80%
what are the most common small colon conditions
impactions
fecaliths/enteroliths
strangulating lipomas
mesenteric rents
what are the risk factors and predilections of small colon impactions
poor dentition
poor hay quality
lack of water
parasites
submucosal edema
motility problems
older horses and yearlings, miniature horses, ponies, Arabians, fall and winter
what are the clinical signs of small colon impaction
abdominal pain that is initially mild with slow progression
straining to defecate, intermittent cramping
infrequent diarrhea
history of decreased manure production
gross abdominal distension may be present
fever
how might small colon impactions present on diagnostics
bloodwork- leukopenia is not uncommon, dehydration
rectal exam- impaction at the small colon, gas distention of the large colon, rough rectal mucosa
occasional gastric reflux, with severe distension
abdominocentesis usually WNL
what are the indications for surgery with small colon impactions, prognosis and complications
increasing abdominal pain
increasing abdominal distension
abnormal abdominocentesis
deteriorating CV
presence of refllux
prognosis generally good
complications include re-impaction, diarrhea, Salmonella
what is the presenting complaint with small colon fecaliths or enteroliths
miniature and young horses
straining to defecate may have infrequent diarrhea, history of no recent manure production, gross abdominal distension
how does small colon enterolith present on diagnostics
abnormal abdominocentesis suggestive of small colon wall compromise
abdominal Rads low yield
surgery is indicated
what are the differentials for small colon strangulating
mesenteric rents
pedunculated lipoma
intussusception
volvulus
clinical findings similar to non-strangulating lesion except abnormal abdominocentesis and perhaps level of pain
what are the causes of rectal tears
iatrogenic during rectal palpation or transrectal ultrasound
dystocia
enema administration
breeding accident
passage of fecalith/enterolith
idiopathic in aged geldings
what are the signalment risk factors for rectal tears
arabians and minis
older horses
mares due to more frequent palpation and breeding/foaling
stallions/geldings due to lack of palpation
what is the etiology of rectal tears
failure of the rectal wall to relax during rectal palpation
weakening of rectal musculature
trauma to the rectal mucosa
10-2o clock, 15-20cm oral to sphincter
how are rectal tears diagnosed
history
sudden decrease in pressure around an examiners arm during the examination
blood on palpation sleeve, though could be mucosal irritation only
palpable defect
rectal scoping
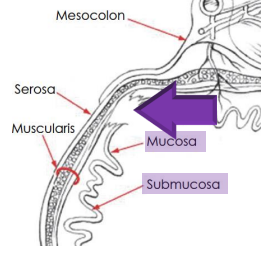
what grade rectal tear
grade 1- through mucosa and submucosal only
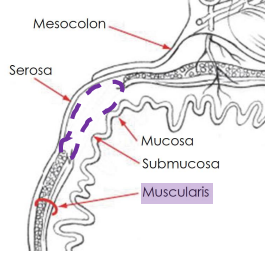
what grade rectal tear
grade 2- torn muscularis with intact mucosa and submucosal
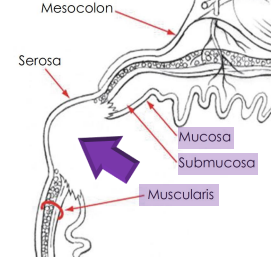
what grade rectal tear
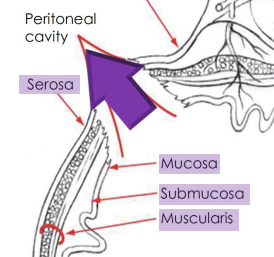
grade 3a, serosa only intact layer
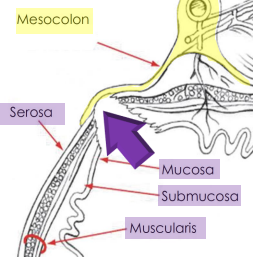
what grade rectal tear
grade 3b, mesocolon only intact layer
what grade rectal tear
grade 4, entrance to peritoneal cavity
how are rectal tears prevented
well restrained- handler on lead, twitch, in stocks
sedation- alpha-2 adrenergic gonist like xylazine, butorphanol
n-butylscopolammonium bromide that decreases peristaltic waves
lidocaine per rectum
generously lubricated rectal sleeve
remove feces before exam
do not move forward while horse is straining
how should liability be handled for rectal tears
cause of malpractice claims
not required to inform client of risk, but doing so can protect
inform owner → provide appropriate emergency treatment → offer referral → maintain detailed records including client communication → notify professional liability insurance
vets should not admit liability
what are potential sequelae of rectal tears
periana fistula
dissecting cellulitis
formation of rectal diverticulum with grade 2
rectal stricture
septic peritonitis with grade 4 → tachycardia, ileus, pyrexia hyperhidrosis, reluctance to move, colic, pain on rectal palp
what is the prognosis for rectal tears
1= good
2= considered incidental
3= fair to guarded
4= poor to grave