fluid and electrolytes
1/49
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
50 Terms
regulating fluids
shifts between intracellular fluid (ICF) and Extracellular fluid (ECF) for transports of nutrients gases and waste.
capillaries
filter out of vessels that increase hydrostatic pressure
and reabsorb back into vessel, which increases osmotic pressure
kidneys
kidneys are like water filters.
If you drink a LOT of water, it’s too watery, so your pee comes out clear.
If you don’t drink enough, your pee is more yellow because it’s more concentrated.
cardiovascular system
is a pump.
If it pumps faster, it pushes blood harder through your body.
That makes your blood pressure go up (like blowing harder into a balloon).
Third-spacing
is when the water leaks out into places it shouldn’t go — like into the walls or basement — where it can’t be used by the house anymore.
Thired spacing: What happens
Even though your body has water, it’s stuck in the wrong place.
That means the blood doesn’t have enough fluid, so your heart, kidneys, and blood pressure start to struggle.
signs of thrid spacing
Early sign
Less pee 🚽 → Even if you drink enough, your kidneys don’t get enough blood, so they make less urine to save water.
Other signs
You look and feel like you don’t have enough fluid in your blood:
Faster heartbeat ❤🔥 (heart works harder)
Lower blood pressure ⬇
Swelling (edema) 💧 in your body
Weight goes up ⚖ (because fluid is stuck in tissues)
Fluids in vs. fluids out don’t match (imbalance)
Third spacing occurs in
Ascites → fluid in the belly
Burns 🔥 → skin is damaged, fluid leaks out
Peritonitis 🦠 → infection in the belly lining
Bowel obstruction 🚫🥒 → blocked intestines cause fluid shift
Massive bleeding 🩸
dehydration
when your body loses more water than salt (electrolytes).
How your body tries to fix dehydration (compensatory mechanisms):
SNS (sympathetic nervous system) = makes you feel thirsty 🥤
ADH (antidiuretic hormone) = tells kidneys to hold onto water 🚱
Aldosterone = helps keep both water and salt 💦🧂
why older adults are at risk for dehydration
They have less body water to start with
They don’t feel as thirsty as younger people
Their bodies can’t adjust as quickly
Severe dehydration (fluid volume deficit) dangers
Your blood becomes too “empty” (low volume of blood)
Your heart has to work really hard to pump what little fluid is left
Eventually, your body can’t keep blood pressure up → hypovolemic shock 🚨
This can even cause seizures or be life-threatening
Recognize and Analyze Cues of Dehydration (Low Fluid Volume)
1. Low volume in the blood (not enough fluid in the pipes 🚰)
Fast heart rate = tachycardia ❤🔥
Weak, thin pulse = thready pulse
Low blood pressure = hypotension ⬇
Fast breathing = tachypnea 😮💨
Little urine = oliguria 🚽
Slow capillary refill (press nail → takes long to turn pink)
2. Low volume to the brain (brain not getting enough fluid 🧠💧)
Dizziness 🎢
Fainting (syncope) 😵
Confusion 🤔
3. Low water in tissues (body cells are thirsty 🌵)
Thirst 🥤
Dry mouth/mucous membranes 👅
Nausea & vomiting 🤢
Skin turgor down = pinch skin, it stays up like a tent ⛺
dehydration risk factors (what causes it)
Losing too much water (sweat, diarrhea, fever)
Third spacing = fluid stuck in wrong place (burns, ascites)
Blood or plasma loss (hemorrhage)
Not taking in enough (NPO, can’t swallow, anorexia)
Lab test for dehydration
Hematocrit (Hct) = high (unless bleeding, then low)
Blood osmolality = high (blood is concentrated)
Urine specific gravity = high (pee is dark & concentrated)
Sodium (Na+) = high
BUN = high (>25, blood too concentrated
deydration immediate actions
Check vital signs & labs
Breathing: rate & effort (RR) 😮💨
Oxygen: SpO₂
Urine output 🚽
Blood tests: CBC, electrolytes 🧪
Give oxygen if needed 🫁
Check the heart & brain
Level of consciousness (LOC) 🧠
Heart rhythm ❤
Blood pressure lying & standing (orthostatic BP)
Rehydrate the body 💦
Oral fluids if possible 🥤
IV fluids if ordered 💉
Keep IV access ready
dehydration ongoing actions
Track fluid balance
Daily weight ⚖
Input & output (I & O)
Alert the doctor if urine <30 mL/hr 🚨
Watch for nausea & vomiting 🤢
Safety first
Help with walking / changing positions slowly 🚶♂
Prevent falls
Hypotonic fluid
0.45% Normal Saline (half-normal) | More water than particles → water moves into cells | Dehydration inside cells; watch for swelling 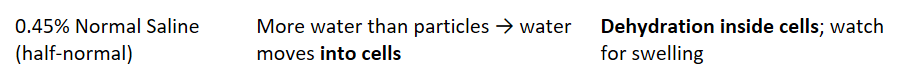 |
isotonic fluid
0.9% Normal Saline (NSS), Lactated Ringers | Expands blood volume → stays mostly in blood vessels | Replace fluid loss, maintain IV access 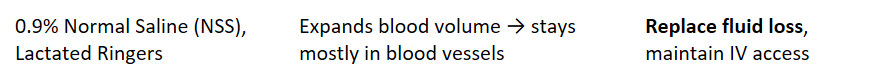 |
hypertonic fluid
3% NaCl, Mannitol | Pulls water out of cells into blood | Cerebral swelling (brain), very concentrated; use carefully |
Dextrose fluid
D5W (5% dextrose in water) | Starts isotonic → becomes hypotonic after glucose is used | Can cause fluid overload; not for nutrition |
Hypervolemia
Your body has too much water or fluid.
The electrolytes (salts, minerals) are usually still normal, but they get diluted because there’s too much water.
Hypervolemia causes
Drinking or receiving too much fluid
Fluid overload from IVs or heart/kidney problems
Body can’t remove fluid properly (kidney issues)
Hypervolemia complications
Severe cases → heart and lungs affected
CHF (congestive heart failure)
Pulmonary edema (fluid in lungs)
hypervolemia body compensation
Kidneys try to get rid of extra salt and water (natriuresis)
Less aldosterone is released → body holds onto less water
Hypervolemia Recognize the Cues
Body System | What You Might See |
Vitals | Fast heart rate (tachycardia), strong pulse, high blood pressure (HTN), fast breathing |
Neuro / Muscles | Confusion, muscle weakness, seizures, tingling, vision changes |
GI | More active gut (increased motility), fluid in belly (ascites) |
Respiratory | Trouble breathing (dyspnea), crackles in lungs, shortness of breath when lying down (orthopnea) |
Other | Swelling (pitting edema), jugular vein distention (JVD), weight gain, pale and cool skin |
💧 Hypervolemia risk factors
1. Hypervolemia (too much fluid + sodium)
Kidney disease 🚽 (can’t get rid of fluid)
CHF ❤ (heart too weak to pump fluid forward)
Cirrhosis 🍺 (liver disease → fluid buildup in belly)
Older age 👵 (less effective heart & kidneys)
Excessive sodium intake 🧂 (salt pulls in water)
2. Overhydration (too much water, not enough electrolytes)
Drinking/replacing only water 💧 (no electrolytes)
SIADH (too much ADH → body keeps water)
Too much IV D5W or hypotonic fluids
Hypervolemia lab test
Hematocrit (Hct) ↓ (blood is watered down)
Blood osmolality ↓ (less concentrated)
Urine specific gravity ↓ (pee more diluted)
Exception: SIADH → urine concentrated
Sodium (Na⁺) ↓ (too much water makes sodium look low)
BUN ↓ (blood looks diluted)
Other electrolytes ↓ in overhydration
ABG → Respiratory alkalosis (from fast breathing, trying to blow off CO₂)
💧 FVO – Immediate actions
Monitor breathing 🫁
Respiratory rate & effort
Breath sounds (crackles, wheezes)
Shortness of breath / dyspnea
SpO₂ (oxygen level)
Check labs & diagnostics 🧪
Urine output
CBC, electrolytes
ABG
Chest X-ray (CXR for pulmonary edema)
Interventions
Give oxygen as needed
Give diuretics (to help pee out excess fluid) 💊
Keep IV access ready
Restrict fluids & sodium intake 🚫🥤🧂
FVO Ongoing actions
Track fluid balance
Daily weight ⚖ (best indicator of fluid changes)
Input & output (I & O)
Protect skin & comfort
Reposition every 2 hours (prevent skin breakdown from edema)
Monitor for swelling (edema)
Elevate/support arms & legs 🛏
Safety
Monitor for weakness, confusion, or fall risk
Ensure safe mobility 🚶♂
⚖ Acid-Base Balance (ABG Basics) Why it matters
Keeps the body in homeostasis (stable internal balance).
Controlled by lungs (respiratory) and kidneys (metabolic).
Imbalances → Acidosis (too much acid) or Alkalosis (too much base).
pH
normal range: 7.35-7.45
acid or basic
overall balance
PaCO2
normal range: 35-45
CO2 in blood
respiratory
PaO2
normal range: 80-100
O2 level in aterial blood
respitory gas exchange
HCO3
normal range: 22-26
bicarbonate
metabolic
SaO2
normal range: 95-100%
% of hemoglobin carrying O2
O2 status
Clinicians Use ABG To:
Check respiratory efficiency (ex: COPD, asthma, respiratory failure)
Assess metabolic function (ex: kidney disease, diabetes, shock)
Diagnose/manage acid-base imbalances
Guide treatments: oxygen therapy, ventilation, electrolyte replacement, meds
Metabolic Acidosis
ABG Pattern: ↓ pH, ↓ HCO₃⁻
Risk Factors (Causes):
Diarrhea 🚽 (loss of bicarb)
Fever 🌡
Hypoxia (low O₂)
Starvation / ketoacidosis 🍽
Seizures ⚡
ASA (aspirin) overdose 💊
Renal failure 🩺
DKA (diabetic ketoacidosis)
Dehydration
Clinical Manifestations (Signs):
Bradycardia ❤🩹
Weak pulses
Hypotension ⬇
Tachypnea (fast breathing, Kussmaul respirations) 😮💨
Flaccid paralysis
Confusion
Metabolic Alkalosis
ABG Pattern: ↑ pH, ↑ HCO₃⁻
Risk Factors (Causes):
Too many antacids 🍼
GI suction (loss of stomach acid)
Hypokalemia (low K⁺)
TPN (Total Parenteral Nutrition)
Blood transfusions
Prolonged vomiting 🤮
Clinical Manifestations (Signs):
Dizziness 🎢
Paresthesia (tingling) ✨
Muscle cramps/spasms (hypertonic muscles) 💪
Slow/shallow breathing (respiratory compensation)
Interventions (Both Metabolic Acidosis & Alkalosis)
Treat the underlying cause 🩺
Give fluids + electrolytes as needed 💧🧂
Monitor vital signs, neuro status, and ABGs
⚖ Compensation for Metabolic Imbalances
1. Metabolic Acidosis (↓ pH, ↓ HCO₃⁻)
Problem: Too much acid / not enough base
Compensation:
Lungs hyperventilate (breathe fast & deep)
This blows off CO₂ (acid)
Helps raise pH back toward normal
Example: Kussmaul respirations in DKA
2. Metabolic Alkalosis (↑ pH, ↑ HCO₃⁻)
Problem: Too much base / not enough acid
Compensation:
Lungs hypoventilate (slow breathing)
This retains CO₂ (acid)
Helps lower pH back toward normal
Limited by O₂ needs — the body won’t let you stop breathing too much
Respiratory Acidosis
ABG Pattern: ↓ pH, ↑ CO₂
Risk Factors (Causes):
Respiratory depression (opioids, anesthesia, trauma)
Pneumothorax (collapsed lung)
Airway obstruction (asthma, choking, mucus plug)
Inadequate ventilation (neuromuscular disease, hypoventilation)
Clinical Manifestations (Signs):
Dizziness, headache
Palpitations
Muscle twitching
Convulsions/seizures
Interventions:
Maintain a patent airway
Administer naloxone if opioid-induced
Support ventilation (bag-mask, intubation, mechanical ventilation if severe)
Give bronchodilators (open airways)
Give mucolytics (thin mucus)
Respiratory Alkalosis
ABG Pattern: ↑ pH, ↓ CO₂
Risk Factors (Causes):
Hyperventilation (anxiety, panic attack)
Hypoxemia (low O₂ → breathing too fast)
Altitude sickness ⛰
Asphyxiation
Asthma
Pneumonia
Clinical Manifestations (Signs):
Tachypnea (rapid breathing)
Anxiety / panic
Tetany (muscle spasms)
Paresthesia (tingling in hands/feet)
Palpitations, chest pain
Interventions:
Regulate oxygen therapy (don’t over-oxygenate)
Reduce anxiety (calm environment, meds if needed)
Rebreathing techniques (paper bag, rebreather mask → increases CO₂)
Compensation for Respiratory Imbalances
1. Respiratory Acidosis (↓ pH, ↑ CO₂)
Problem: Too much acid (CO₂ buildup from hypoventilation).
Kidney Compensation:
Excrete H⁺ (acid) into urine 🚽
Retain HCO₃⁻ (bicarbonate, base) in blood
Helps raise pH back toward normal
2. Respiratory Alkalosis (↑ pH, ↓ CO₂)
Problem: Too much base (CO₂ blown off from hyperventilation).
Kidney Compensation:
Excrete HCO₃⁻ (base) in urine 🚽
Retain H⁺ (acid) in blood
Helps lower pH back toward normal
🧂 Sodium (Na+)
Normal range: 135–145 mEq/L
It lives mostly outside the cells 🏠 and helps with water balance 💧 and nerve signals ⚡.
⬇ Hyponatremia (<135)
Causes: Too much water 🚰, vomiting 🤮, diarrhea 💩, sweating a lot 🏃💦, diuretics 💊, SIADH.
Signs:
Weak, tired 🛏
Headache 🤕
Confused brain 🌀
Swelling (edema, crackles in lungs, JVD) 💦
Seizures ⚡
Fix:
Give sodium back 🧂
Limit water 🚫💧
Nursing:
Track intake/output 📝
Daily weights ⚖
Watch brain function 🧠
Safety 🛑
⬆ Hypernatremia (>145)
Causes: Not enough water 🚱, too much sodium 🧂, diarrhea 💩, kidney failure 🚫🩸, diabetes insipidus.
Signs:
Thirsty 😫
Restless/anxious 😵💫
Dry mouth 👅
Red/flushed skin 🌶
Swelling 💦
Muscle twitches 💪
Fix:
Give hypotonic solution (slowly) 💧🐢 to avoid brain swelling
Limit salt 🧂🚫
Diuretics (to dump sodium) 💊
Nursing:
Track fluids 📝
Offer water 💧
Keep safe 🛡
🍌 Potassium (K+)
Normal range: 3.5–5.0 (or 5.2) mEq/L
Mostly lives inside the cells 🏠 and helps with muscles 💪 and the heart ❤ (ECG rhythm).
⬇ Hypokalemia (<3.5)
Causes: Diuretics 💊, vomiting 🤮, diarrhea 💩, suction, not eating enough 🍽, NPO, alcoholism 🍷, alkalosis.
Signs:
Weak muscles 💪
Leg cramps 🦵
Constipation 🚫💩
Tingling (paresthesia) ✨
Irregular heartbeats ❤ (flat/inverted T wave, U wave)
Fix:
Give K+ back (PO or IV 💊💉)
Eat potassium-rich foods 🍌🥔🍊
Nursing:
Monitor heart ❤
Watch kidneys 🩺
Replace K+ as ordered ✅
⬆ Hyperkalemia (>5.0/5.2)
Causes: Too much K+ intake 🍌, potassium-sparing diuretics 💊, ACE inhibitors, kidney failure 🚫, burns 🔥, trauma 🚑, acidosis.
Signs:
Heart changes ❤ (peaked T wave, wide QRS)
Weak muscles 🪫
Paralysis 🚷
Nausea 🤢, diarrhea 💩
Fix:
Limit potassium foods 🚫🍌
Kayexalate 💊 (pulls K+ out)
If dangerous ⚠ → Calcium gluconate, insulin with glucose, sodium bicarb, loop diuretics, beta-2 agonists 💉
Nursing:
Check brain 🧠, heart ❤, gut 🍽
Avoid K+ foods 🚫🍌🥑