Lesson 7 - Recording and Documentation
1/82
Earn XP
Description and Tags
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
83 Terms
Discussion
Informal oral exchange to identify and resolve issues
Report
Oral, written, or digital communication to convey information
Record (Chart/Client Record)
Formal legal document providing evidence of care
Recording/Charting/Documenting
The process of entering data into client records
Restrict access
Ethical codes and legal responsibility
Policies and procedures to ensure privacy and confidentiality
Security for Computerized Records
Passwords required and should not be shared
Never leave the computer terminal unattended after logging on
Do not leave client information displayed
Shared all unneeded computer-generated worksheets
Know the facility’s policy and procedure for correcting an entry error
Follow agency procedures for documenting sensitive material
Firewalls
11 ways of Maintaining Confidentiality of Records
Communication
Planning client care
Auditing health agencies
Research
Education
Reimbursement
Legal documentation
Health care analysis
8 purposes of client record
Source-Oriented Record
Problem-oriented medical record
PIE Model (Problems, Interventions, Evaluation)
Focus Charting
Charting by Exception (CBE)
Computerized Documentation
Case Management
7 types of documentation systems
Source-Oriented Records
Traditional client record
Each discipline makes notations in a separate section
Information about a particular problem distributed throughout the record
Narrative charting used
Admission Sheet: Demographic, allergies
Initial Nursing Assessment: Nsg Hx and PE
Medical History and Physical Examination: PMHx FMHx, HPI
Physician’s Order Form: Medical orders for medications, treatments
Physician’s progress notes: Medical observations, treatments, client progress
Nurse’s notes; Pertinent assessment of client Specific nursing care including teaching and client’s responses
Medication record: Name, dosage, route, date of regularly administered medications
Name or initals of individual administering the medication
Special flow sheets VS Sheet: Fluid balance record, skin assessment
Diagnostic reports: Lab and Diagnostic reports
Consultation Records
Client discharge plan and referral summary
11 Components of the Source-Oriented Record
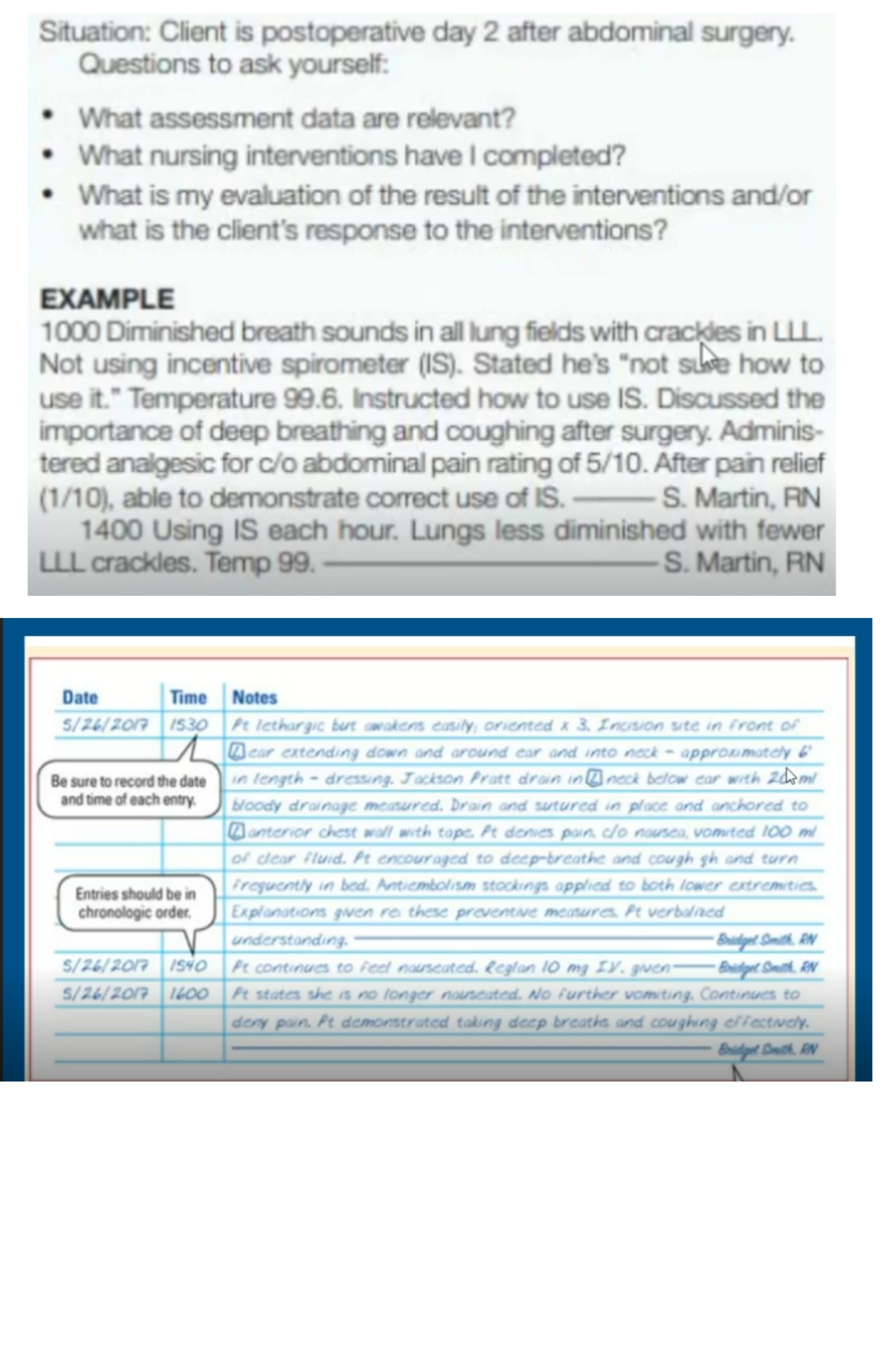
Narrative Charting
A traditional form of documentation in source-oriented records of written notes that describe routine care, normal findings, and client problems
There is no strict order, but entries are often recorded chronologically
Although less common today, narrative charting is still used alongside modern systems like charting by exception or focus charting for describing abnormal findings
Problem-oriented Medical Records (POMR)
Data arranged according to client problem
Four Components of POMR:
Database
Problem List
Plan of Care
Progress Notes
Health team contributes to the problem list, plan of care, and progress notes for each problem
Database
Problem List
Plan of Care
Progress Notes
Four Components of POMR
Subjective Data (S)
Information obtained from what tje client says. In relation to the problem.
“I feel lightheaded and nauseous.”
Objective Data (O)
Measurable and observable information collected through assessment
Includes vital signs, laboratory results, imaging findings, and physical exam results
Example: BP 88/60 mmHg, HR 110 bgm, pale skin.
Assessment (A)
Interpretation of subjective and objective data
During the initial assessment, the problem list is created
In subsequent notes, this section describes progress and condition
Example: Hypotension secondary to dehydration
Plan (P)
The care plan to address the identified problem
Includes treatment, interventions, and follow-ups
Example: Administer IV fluids, reassess BP in 30 minutes
SOAPIE
SOAP that adds Interventions and Evaluations
Interventions (I)
Actions performed by the caregiver.
Example: Administered *1L normal saline IV bolus.)
Evaluation (E)
Client’s response to interventions
Example: BP improved to 100/70 mmHg, dizziness resolved
SOAPIER
SOAPIE that adds Revision
Revision (R)
Adjustments to the care plan based on evaluation
Continue IV fluids at maintenance rate; monitor BP hourly.
AP(Assessment & Plan)
Combines subjective and objective data into the assessment
APIE/APIER
Includes interventions, evaluation, and revision but eliminates separate subjective/objective sections
PIE Documentation
Groups information into 3 categories:
Problem, Interventions, Evaluation
Consists of client assessment, flow sheet, and progress notes
Flow Sheet Overview
Uses specific assessment criteria (e.g., human needs, health patterns).
Time intervals vary from minutes to months.
Problems (PIE documentation)
Identified based on client assessment
Often written using nursing diagnosis
If no approved diagnosis exists, a problem statement is formulated with:
Client’s response
Probable causes
Manifested characteristics
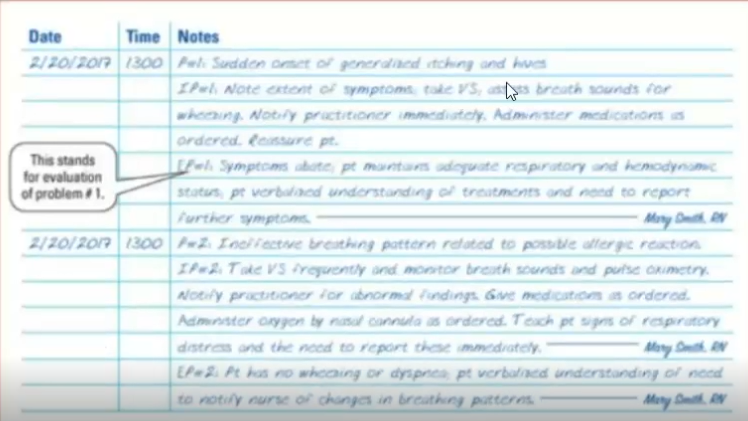
Interventions (PIE documentation)
Actions taken by the nurse to address the problem.
Recorded with a corresponding problem number
Evaluation (PIE documentation)
Assesses effectiveness of interventions
Determines whether modifications are needed
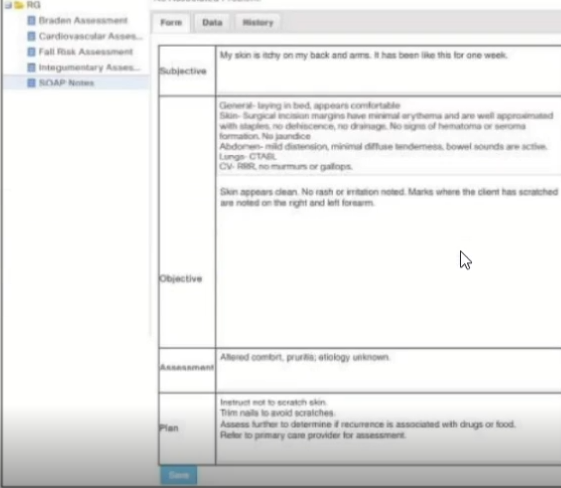
Focus Charting
Focus on client concerns and strengths
Holistic perspective of client and client’s needs
Nursing process framework for the progress notes
Uses three columns:
Date/TIme
Focus: The Focus can be a condition, nursing diagnosis, behavior, symptom, acute change, or client strength
Progress notes: DAR (DATA , ACTION, RESPONSE)
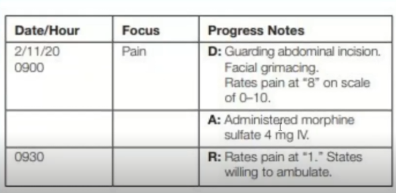
Data
Action
Response
3 progress notes follow the DAR format:
Data (Focus Charting)
Observations of client status and behaviors (subjective & objective data, flow sheet info)
Action (Focus Charting)
Nursing interventions, planning, and any care plan adjustments
Response (Focus Charting)
Client’s reaction to nursing and medical care.
Charting by Exception (CBE)
A documentation system in which only abnormal or significant findings or exceptions to norms are recorded
Saves time by reducing unnecessary documentation and highlighting significant client changes
May pose legal risks due to incomplete records, and some nurses feel uneasy about the “not charted, not done” concern
Flow Sheets
Standards of Nursing Care
Bedside Access to Chart Forms
Key Elements of CBE
Flow Sheets
Used to record vital signs, assessments, and risk evaluations in a structured format
Standards of Nursing Care
Routine care is documented by reference to pre-set standards, with only deviations fully described in nursing notes
Bedside Access to Chart Forms
Flow sheets are kept at the bedside for immediate recording, eliminating transcription delays.
Recorded
A documentation system in which only abnormal or significant findings or exception to norms are ___
saves time by reducing unnecessary documentation and highlighting significant client changes
May pose legal risks due to incomplete records, and some nurses feel uneasy about the “not charted, not done” concern.
Computerized Documentation
EHR integrate all client information into one system
Developed to manage volume of information
Use of computers to store the client’s database, new data, crete and revise care plans and document client’s progress
Information easily retrieved.
Possible to transmit information from one care setting to another
Case Management Model
Focuses on quality, cost-effective care within a set timeframe.
Critical pathways outline expected outcomes and interventions for specific client groups.
CBE is often used, requirinf documentation only when goals are unmet (variance)
Variance refers to deviations from the expected care plan, requiring documentation of cause and action taken.
Uses of CBE
Documentation of variance include:
Actions taken to correct the situation
Justify the actions taken
Documenting the Nursing Process
Admission Nursing Assessment
A comprehensive assessment is conducted upon admission and documented based on health patterns, body systems, or healthcare settings, with updates recorded in flow sheets or progress notes.
Nursing Care Plans
Required by the Joint Commission, care plans can be traditional (individualized) or standardized (Institution-based but customizable) and must include assessments, interventions, and expected outcomes.
Kardexes
A quick-reference record for healthcare professionals that contains essential client information, including medications, treatments, and care needs, and may be temporary or permanent.
Kardex
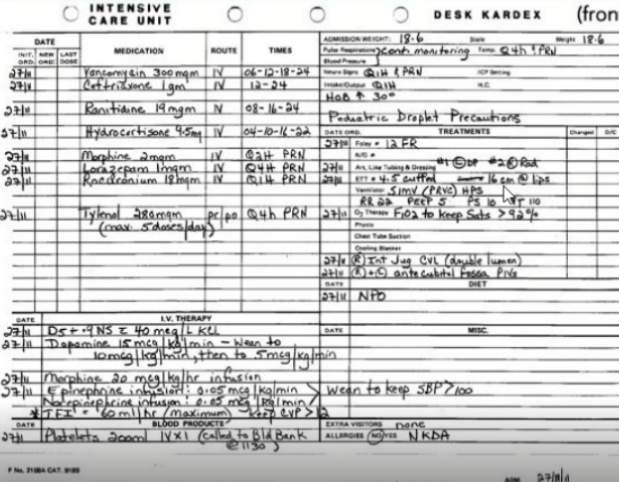
Flow Sheets
Concise records that track various aspects of patient care, such as vital signs (graphic record), fluid balance (intake/output), medications (MAR), and skin integrity (assessment records)
Progress Notes
Used to document client status, interventions, and responses, following the institution’s preferred format.
Nursing Discharge & Referral Summaries
These summaries ensure continuity or care by documenting the client’s condition, ongoing needs, treatments, restrictions, support systems, and follow-up care in clear, understandable language.
Date and Time
Essential for legal and clinical accuracy to track interventions and patient progress
Must be documented with each entry using either
12-hour format (e.g., 0900, 1515) to avoid confusion
Never pre-record entries before performing care
Timing
Follow the healthcare facility’s documentation frequency policy
Adjust documentation based on the patient’s condition (e.g., unstable vital signs require more frequent recording)
Document immediately after providing care or making an assessment.
Legibility
Entries must be clear and readable to prevent misinterpretation
Permanence
Use dark ink for written records to ensure clarity and prevent alterations
Corrections in EHRs must follow the software’s tracking and correction policies
Accepted Terminology
Use standardized medical abbreviations to prevent errors
Avoid ambiguous abbreviations that may have multiple meanings.
Correct Spelling
Spelling errors can lead to serious medical mistakes, especially with medication names (e.g., Fosamax vs. Flomax)
Signature and Identification
Each entry must be signed with the nurse’s full name and credentials (e.g., “Jane Doe, RN”).
Accuracy
The patient’s full name and ID must appear on each page of the medical record
Verify the correct chart before making an entry
Document only objective facts, avoiding assumptions or opinions.
Correcting Errors
Do not erase, use correction fluids, or overwrite mistakes
To correct a handwritten mistake:
Draw a single line through the error
Write “error” above it, initial, and date the correction
Sequence
Record events in the order they occur (e.g., assessment → interventions → patient response).
Appropriateness
Only document information relevant to patient care.
Conciseness
Entries should be brief but complete to save time while maintaining clarity. Omit the patient’s name in each entry (it is assumd from the record).
Legal Prudence
Accurate and complete documentation protects the nurse, patient, and facility in legal cases.
Example of Proper Documentation in a Fall Incident:
1100 - Patient complained of dizziness. Raised side rails and instructed patient to stay in bed.
1130 - Found patient on the floor. Patient stated, “I climbed out of bed all by myself.” Assisted back to bed. BP 100/60, HR 90, RR 24
1135 - Physician Dr. Nadem notified. Signed: Rs Woo, RN
Chart a change in a client’s condition and show that follow-up actions were taken
Read the nurse’s notes prior to care to determine if there has been a change in the client’s condition
Be timely. A late entry is better than no entry; however, the longer the period of time between actual care and charting, the greater the supicion
Use objective, specific, and factual descriptions
Correct charting erors.
Chart all teaching
Record the client’s actual words by putting quotes around the words
Chart the client’s response to interventions
Review your notes - are they clear and do they reflect what you want to say?
Do’s for Practice Guidelines: Documentation
Leave a blank space for a colleague to chart later
Chart in advance of the event (e.g., procedure, medication).
Use vague terms (e.g., “appears to be comfortable,” “had a good night”).
Chart for someone else
Record “patient” or “client” because it is their chart
Alter a record even if requested by a superior or a primary care provider.
Record assumptions or words reflecting bias (e.g., “complainer,” “disagreeable”).
Don’t for Practice Guidelines: Documentation
Guidelines for Reporting Client Data
Reporting is essential in healthcare to ensure effective communication of patient information among healthcare professionals.
A well-structed report should be:
Concise - Contain only relevant details.
Accurate - Based on factual data and observations.
Timely - Delivered promptyl to maintain continuity of care.
Organized - Presented logically to facilitate understanding.
Change-of-shift report
Telephone reports
Care plan conference
Nursing rounds
types of reporting
Handoff Communication (Change-of-shift report)
It is a process of sharing client care information
A standardized approach is critical for client safety during transitions of care
Healthcare institutions must define the elements of handoff communication to prevent adverse outcomes.
Every hospital and healthcare system must implement a standardized approach to handoff communication
Handoff occurs at multiple levels in healthcare settings, such as:
Nurse to nurse/ Nurse to physician/ Physician to physician/ Other healthcare providers
Change-of-Shift Report Process
The report is given to all nurses on the next shift
Face-to-face communication allows the incoming nurse to:
Ask questions
Gain confidence in client care
Incoming and departing nurses establish care priorities for the next hours
Reviewing checklists and medical records ensures a smooth transition
Report content includes: Client problems and interventions for client care
Methods of Change-of-Shift Reporting
Written
Oral (face-to-face or audiotape recording)
Face-to-face bedside reporting allows the oncoming nurse to:
Meet the client and family
Ask questions and address concerns
Involve the client in their care
A designated room
The nurses’ station
At the client’s bedside
Face-to-face reports can also occur in
I PASS the BATON
I-SBAR
PACE
Five-P’s
Standardized Handoff Communication Tools
I PASS the BATON
Introduction, Patient, Assessnent, Situation, Safety Concerns, Background, Actions, TIming, Ownership, Next
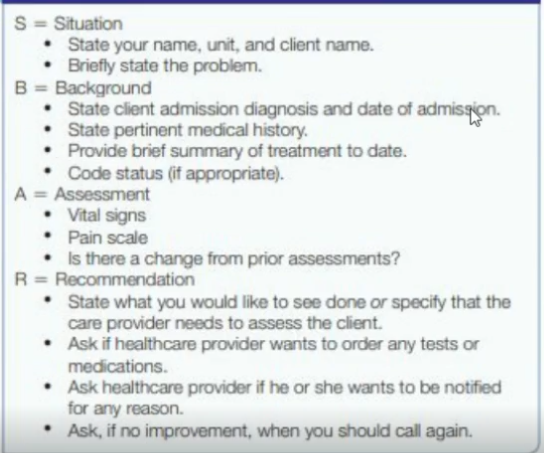
I-SBAR
Introduction, Situation, Background, Assessnent, Recommendation
PACE
Patient/Problem, Assessment/Actions, Continuing (treatments)/Changes, Evaluation
Five-P’s
Patient, Plan, Purpose, Problem, Precautions, Physician (assigned to coordinate)
Key Elements for Effective Handoff Communication
The communication should include the following":
Up-to-date information
Interactive communication allowing for questions between the giver and receiver of client information
Method for verifying the information (e.g., repeat-back, readback techniques)
Minimal interruptions
Opportunity for receiver of information to review relevant client data (e.g., previous care and treatment),
Guidelines for Change-of-Shift report
Follow a particular order
Provide basic identifying information
For new clients provide the reason for admission or medical diagnosis/es, surgery, diagnostic tests and therapies in the past 24 hours
Significant changes in client’s condition
Provide exact information
Report client’s need for emotional support
Include current nurse and physical-prescribed orders
Provide a summary of newly admitted clients, including diagnosis, age, general condition, plan of therapy, and significant information about the client’s support people
Report on clients who have been transferred or discharged
Clearly state priorities of care and care due after the shift begins
Be concise
Telephone reports
Health professionals frequent;y report client information via telephone.
Nurses inform primary care providers about changes in a client’s condition
A radiologist may report x-ray results
A nurse may report to another nurse regarding a transferred client
Guidelines for Receiving a Telephone Report
Document date and time
Record the name of person giving the information
Record the subject of the information received
Repeat information to ensure accuracy
Sign the notation
The individual receiving the information should repeat it back to the sender to ensure accuracy
Guidelines for Giving a Telephone Report
Be concise and accurate
When giving a telephone report to a primary care provider, it is important that the nurse to be concise and accurate. The SBAR communication tool is often used for telephone
Have chart ready to give any further information needed
Document the date, time. and content of the call
SBAR communication tool
Telephone and Verbal Orders
Primary care providers may order therapy (e.g., medication) by telephone or verbally (face-to-face).
Most agencies have specific policies regarding these orders
Many agencies allow only registered nurses (RNs) to take these orders
Many acute care hospitals require the provider to sign the order within 24 hours as per policy.
While receiving the order:
Write the complete order on the physician’s order form.
Read it back to the primary care provider to ensure accuracy
Clarify any ambiguous, unusual, or controindicated orders, such as:
Abnormally high medication dosafes
Orders that contradict the client’s condition
The primary care provider must verbally acknowledge the read-back of the order
Indicate on the physician’s order form it is a Telephone Order (TO) or Verbal Order (VO)
Care Plan Conference
A meeting where nurses discuss solutions to a client’s problems, such as coping difficulties or lack of progress
Other health professiona;s, like social workers or dietitians, may provide expertise
Effective conferences require, nonjudgemental acceptance, and active lsitening
Nurses visit clients bedised to gather information, allow client input, and evaluate care
The assigned nurse gives a brief summary of the client’s needs and interventions
Benefit include client participation and direct observation of the client and equipment
Nurses should use simple language to ensure client understanding.