chapter 14
1/56
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
57 Terms
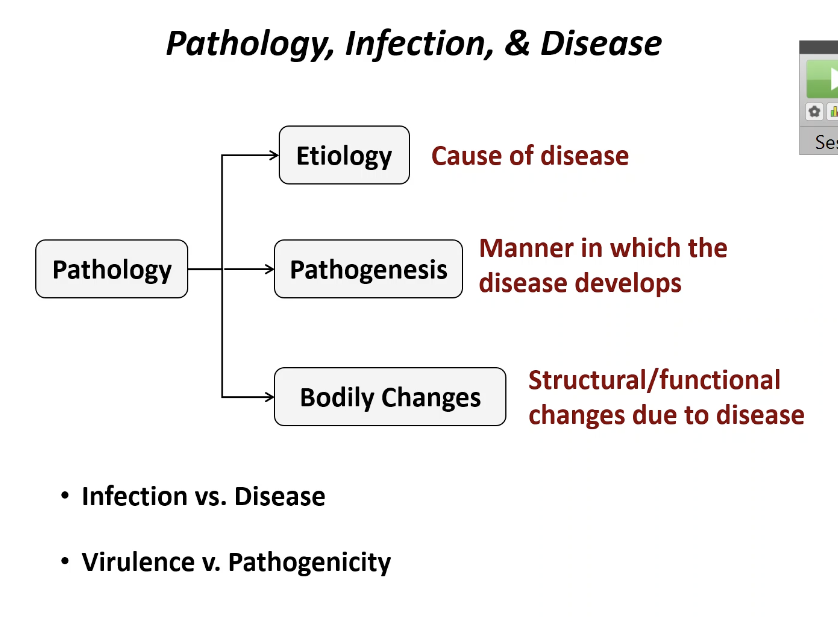
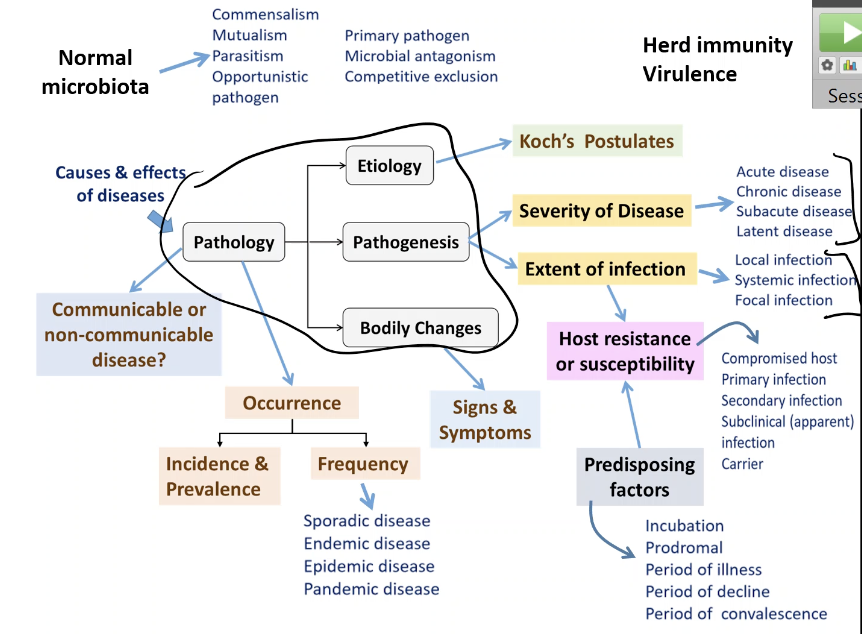
Pathology
is the study of disease; how they start, develop, and affect your body
Etiology
The cause of a disease
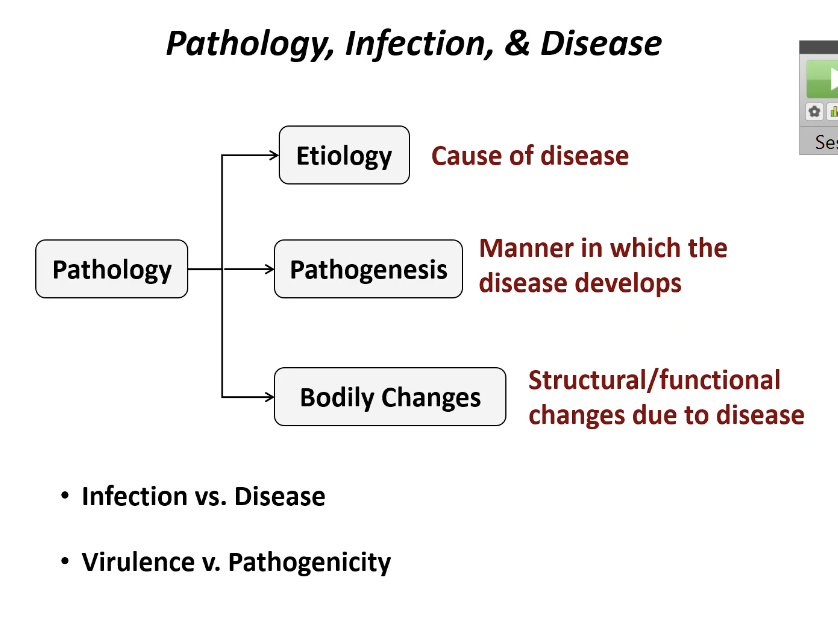
Pathogenesis
The manner in which a disease develops or progresses
Process of disease
How its transmitted, developed, entrance
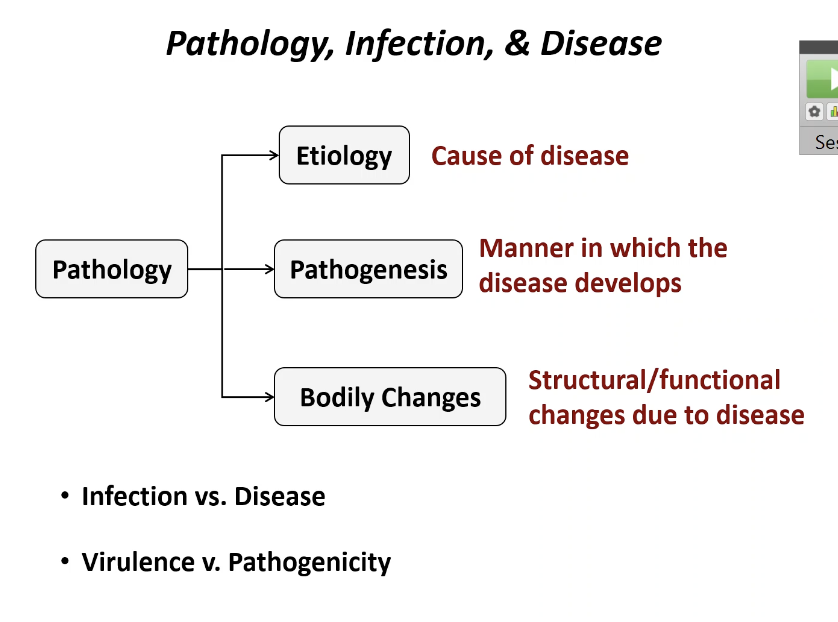
Bodily changes
The physical (structural ) and functional changes that result from the disease
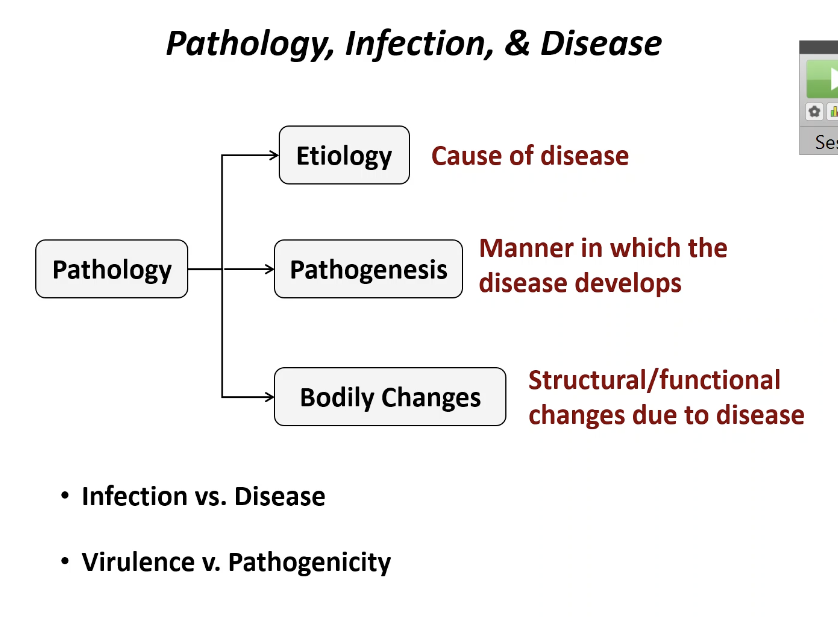
Infection VS Disease
When a microbe gets inside your body and starts to grow
You can be infected without feeling sick
Infection VS Disease
When that growth actually causes an abnormal state of health or noticeable illness
You can be infected but not have a disease yet
Pathogenicity VS Virulence
The ability of a microbe to cause disease at all
"Can it make you sick?"
Pathogenicity VS Virulence
How bad the microbe is - how severe the disease is
"how badly?"
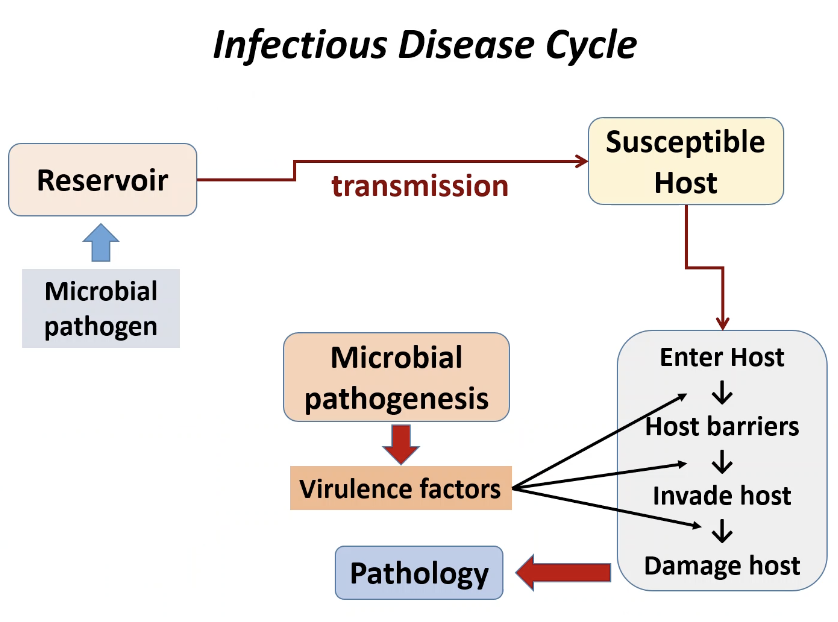
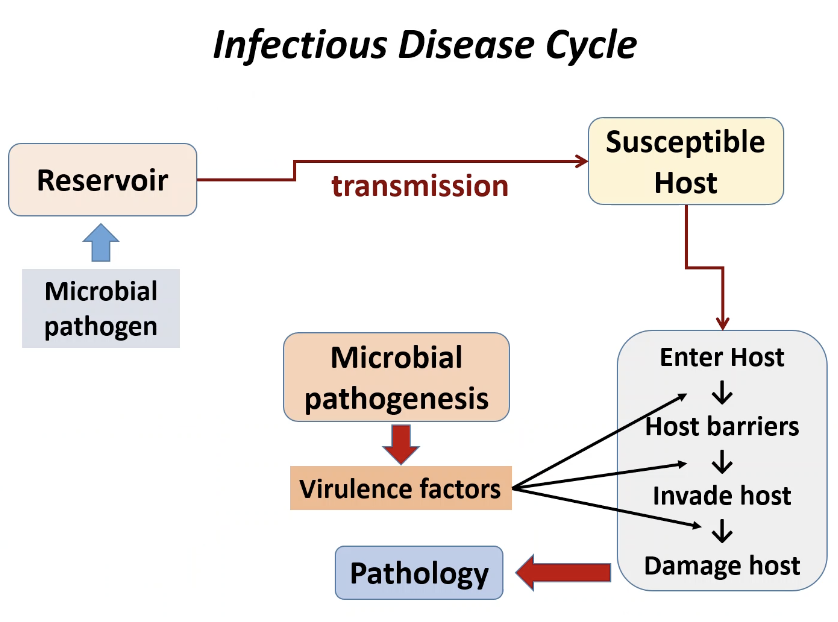
Infectious Disease Cycle
To cause disease, a microbe must follow these steps:
A microbial pathogen is stored in a reservoir (a source)
The pathogen uses transmission to reach a suspectable host
The pathogen must enter the host and overcome host barriers
The pathogen must use its virulence factors (tools it uses to harm you) to invade the host and damage the host
This damage results in pathology (the disease state)
Transmission of disease
Via contact, vehicles & vectors
contact
This means the disease spreads from touching or being near an infected source.
Contact: direct
Physical contact between source + host
Contact : indirect
Transmission via inanimate object -> fomite
Contact : droplet
Short distance
Sneezing, coughing
Travels < 1 meter
Vehicle
Congenital transmission
Vector
Vehicle
this means the disease spreads through a shared medium (something many people use/consume).
Transmit disease via water, food, or air; also blood, drugs
Waterborne
Contaminated (fecal) water treatment system compromised
Fecal-oral transmission
Airborne
Dust particles
Pet dander
Foodborne
Contaminated food storage @ improper temp
Undercooked food
Unsanitary handling of food
Congenital transmission
Mother -> child
Vector
This means the disease is spread by animals, usually insects.
Insects typically
Mechanical transmission:
The insect carries the pathogen on its body and passively spreads it.
Passive via body parts
Biological transmission
The pathogen grows or develops inside the insect before infecting you.
This involves the parasite's life cycle.
Involves parasite life cycle
Human Microbial Flora
Normal microbiota (or flora)
Millions of microbes (mostly bacteria) that live naturally and permanently on your body without causing disease
Skin
Mouth
Nose
Gut
Lungs
They colonize based on
Physical factors
Temp
Moisture
Chemical factors
pH
Oxygen levels
Normal vs transient microbiota
Microbes that are only present for a short period (days or week) before they disappear
Sterile areas
If microbes are found in areas that should normally be microbe-free (like blood or internal organs), it signals true infection
Host-Microbiota Relationship (Symbiosis)
Symbiosis is the relationship between the host and the microbes
Microbiota exhibit Microbial antagonism (competitive exclusion)
Prevents colonization of pathogenic microbes
The normal, healthy bacteria precent pathogenic bacteria from settling down. They do this by competing for nutrients and space, or by producing substances that kill or inhibit the pathogens
Normal biota protect you by:
Competing with pathogens
Taking up space
Using nutrients
Making toxins to kill bad microbes
If the balance is upset -> disease
Types of symbiosis
Commensalism (+/0)
Microbes benefit; host unaffected
Normal skin bacteria
Mutualism (+/+)
Both benefit
Gut bacteria making vitamins
Parasitism (+/-)
Microbes benefits/ host is harmed
Pathogens
Opportunistic pathogens
Normal microbiota that turn harmful when
Immune system weak
Balance disrupted
Microbes enter wrong location
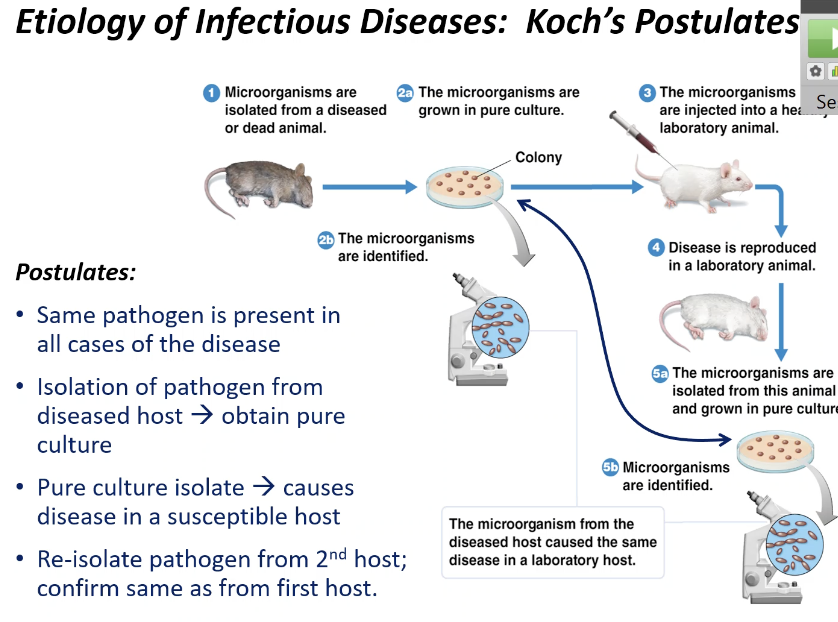
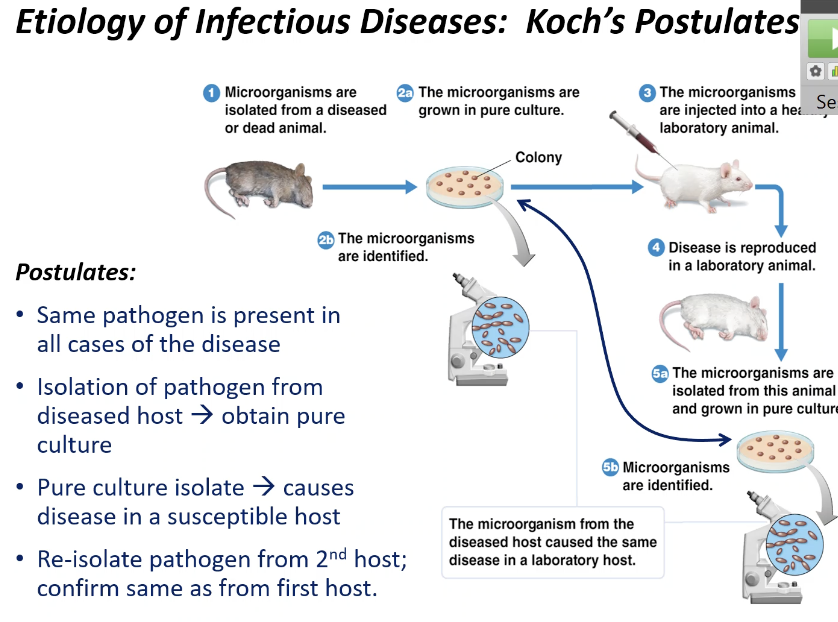
Koch's Postulates
4 steps used to prove a specific microbes is the cause (etiology) of a specific infectious disease
Same pathogen must be found in every single case of the disease
The pathogen must be isolated from the diseased host and grown in a pure culture (container w/ only one type of microbe)
The isolated microbe from the pure culture must cause the same disease when injected into a healthy suspectable animal host
The pathogen must be re-isolated from the second host and confirmed to be identical to the original pathogen
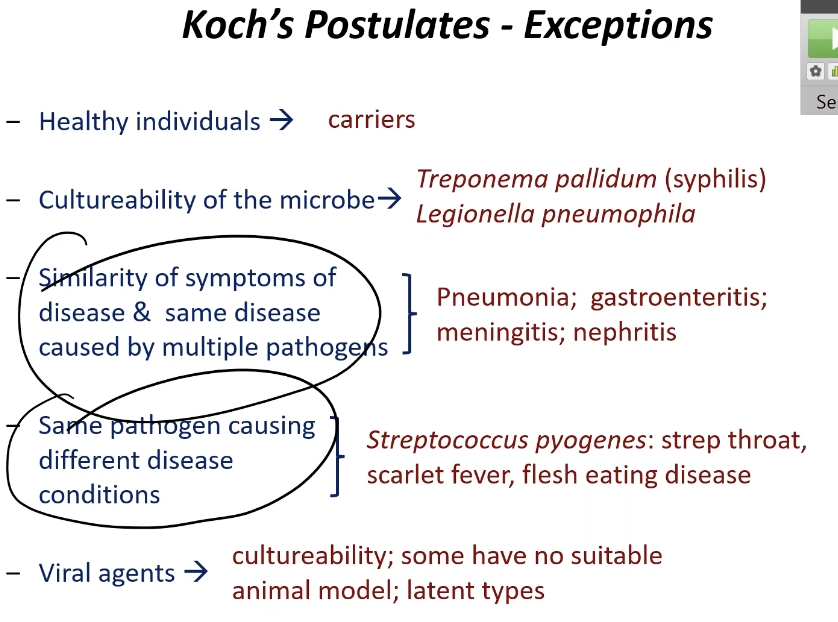
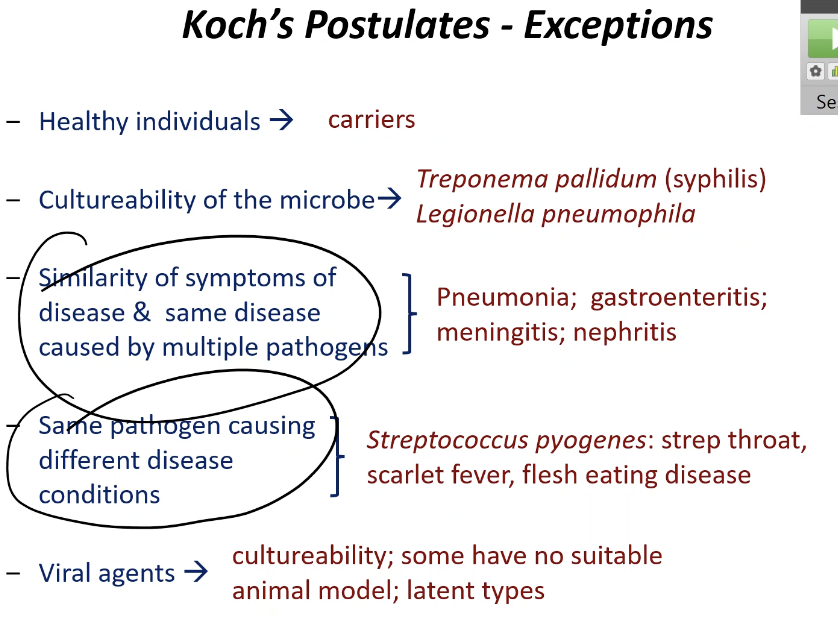
Koch’s Postulates Exceptions:
There are healthy carriers - people who carry the pathogen but don’t show any symptoms
Some microbes cant be grown in labs (pure culture)
Treponema pallidum
Viruses
One diseases can be caused by many microbes
Pneumonia
One microbe can cause multiple diseases
Streptococcus pyogenesis
Strep throat, scarlet fever, flesh eating disease
Viruses need host cells - cannot grow in pure culture normally
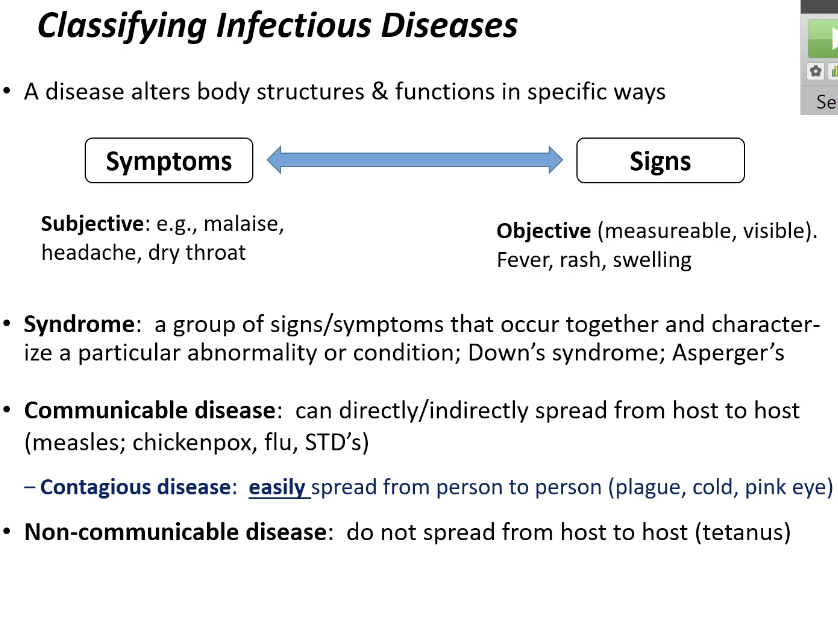
Classifying infectious disease
By spread (transmission)
By occurrence (frequency)
By severity or duration
By extent of infection
By spread (transmission)
Communicable disease
Disease that can spread direclty or indirectly from one host to another
Contagious disease
A communicable disease that is very easily and rapidlt spread
Cold, pink eye
Non communicable disease
A disease that cannot be spread from host to host
Tetanus; caused by bacteria in the soil
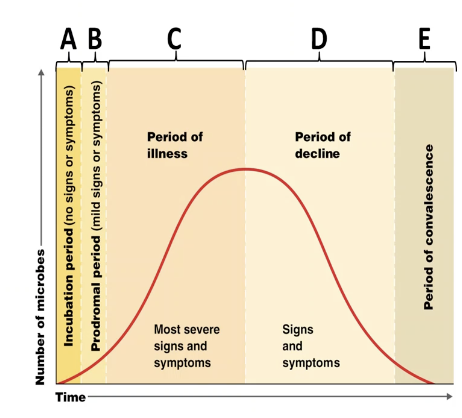
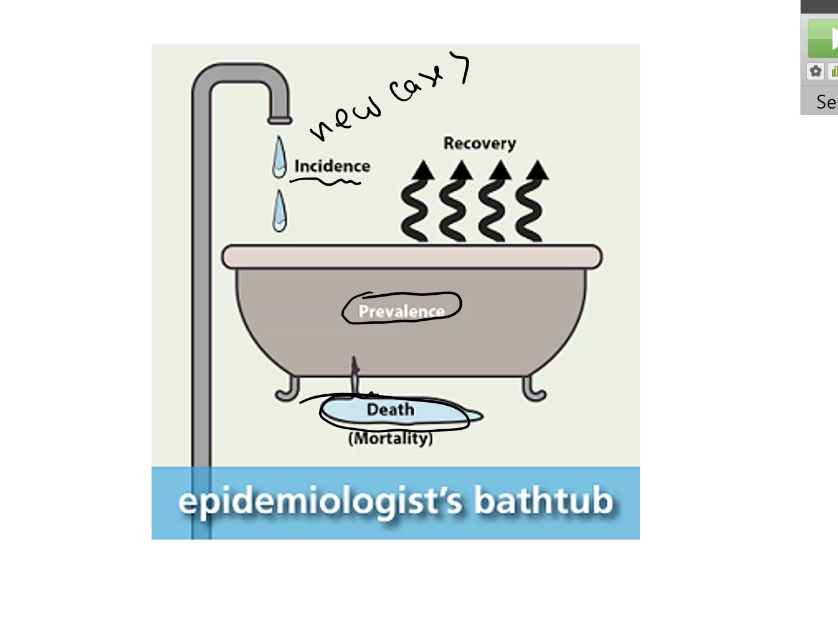
By occurrence (frequency)
Incidence
Number of new people who get a disease in a given time period
Shows the spread of the disease
Prevalence
The total number of people who have a disease in a given time period
It shows the spread of the disease
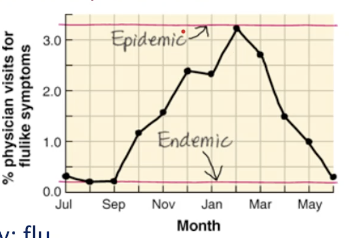
By occurrence (frequency): TYPES
Frequency Type | Definition | Example |
Sporadic | Disease occurs infrequently (randomly and rarely)41. | Isolated cases of typhoid fever. tetanus |
Endemic | Disease is always present in a population at a certain level42. | Common cold, cholera. |
Epidemic | Disease develops rapidly and affects many people in a specific area43. | A large regional flu outbreak. |
Pandemic | An epidemic that is worldwide44. | The global spread of COVID-19. |
By severity or duration
Acute disease
Symptoms develop rapidly but last only a short time
The flu
Chronic disease
Disease develops slowly and last a long time
Tuberculosis
Subacute disease
Symptoms fall somewhere in between acute and chronic
Latent disease
A disease with a period where the pathogen is inactive and there are no symptoms
It can reactivate later
Shingles, cold sores
By extent of infection
Local infection
The pathogen is limited to a small, specific are
Systemic infection
The pathogen spreads throughout the entire body, usually via the blood or lymph systems
Focal infection
Starts as a local infection but then spreads to specific areas of the body
Infection spreading from a tooth/tonsil
Primary infection
The illness that causes the first infection
The initial sickness
Secondary infection
An infection caused by an opportunistic pathogen after the body has been weekended by the primary infection
Sepsis
A dangerous inflammatory condition caused by toxins or bacteria spreading in the blood from a focus of infection
Ex: Septicemia (bacteria multiplying in the blood)
Subclinical (inapparent) infection
Infection that occurs without any noticeable signs or symptoms of illness
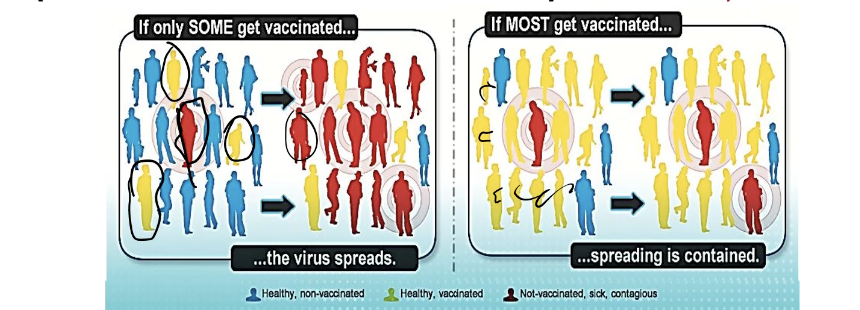
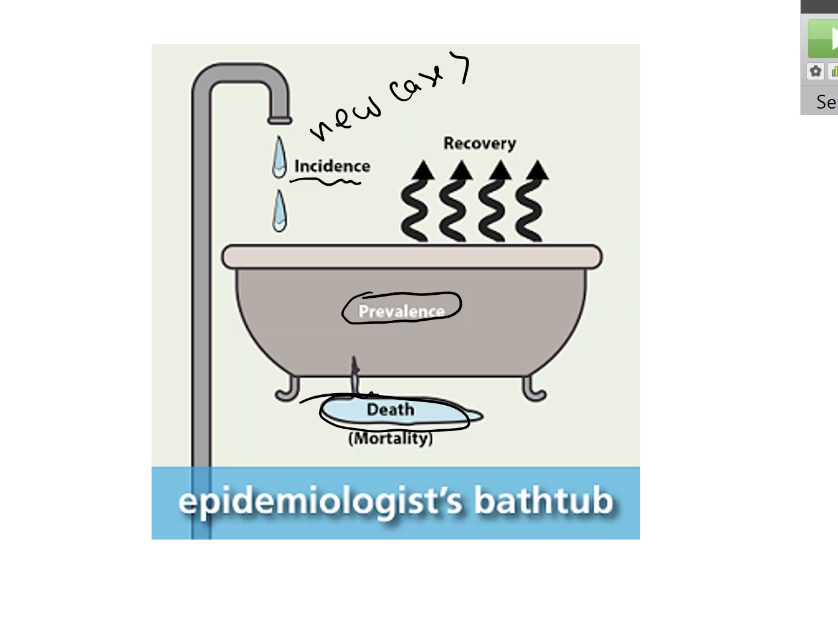
Herd immunity
Immune individuals (vaccinated or recovered from the disease) act as a barrier to the spread of infection
This protects non-immune individuals
Like infants or Immunocompromised
Threshold
The specific percentage of population that must be immune to stop the disease from spreading
R0 (reproduction number)
The average number of people who will catch a contagious disease from one person who is sick
Diseases with higher R0 (like measles R0=18) require a higher vaccination threshold (up to 94%) to achieve herd immunity
Patterns of Development of Disease: Predisposing factors
Predisposing factors
Factors more susceptible to disease
- Age
- Fatigue
- Lifestyle
Diet, exercise, stress
- Climate and weather
- Inherited traits
Sickle cell gene
- Gender
- Chemotherapy
Or other immunosuppressive treatment
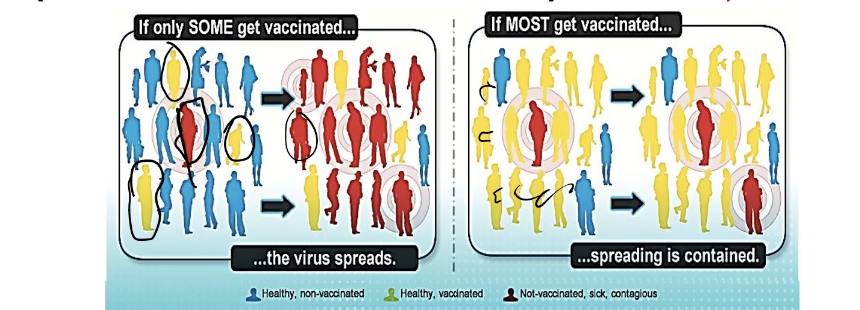
Patterns of Development of Disease: Development of disease stages
The disease follows strict sequential pattern over time
Incubation period
The time from initial infection until the first signs or symptoms appear
Prodromal period
A short time when mild signs or symptoms begin
Period of illness
The disease is at its peak intensity; the most severe signs and symptoms are present
Period of decline
The signs and symptoms subside
Period of convalescence
The body returns to its normal state
Epidemiological studies
Form basis for disease control and prevention through tracking
Prevalence of disease
Identifying determinants/causes of disease
Defines risk factors
Only 1 in 10 reported
150/100,000 more realistic
REVIEW P1
How Infection spreads
The infection cycle is the route an organism takes to get from one person/source to another
The starting point is:
A. Reservoir of infection
How Infection spreads: Reservoir of infection
The place where the disease causing microbe normally lives
3 types
Human reservoir
Animal reservoir
Non living reservoirs
Human reservoir
People who carry the microbe
2 types
People with symptoms
Carriers
Carry disease but show no symptoms
Inapparent infections (hidden infections)
Or latent diseases (inactive)
Animal reservoir
Diseases that animals give to humans called zoonoses
Rabies
Lyme
Ebola
Non living reservoirs
Are soil, water, or other environmental sources
Tetanus (soil)
Cryptosporidiosis (water)
Cholera (water)
Legionella (water systems)
How Infection spreads: Modes of Transmision
How diseases move between people
Three main ways: contact, vehicles, and vectors
Contact Transmission
Vehicle transmission
Vector transmission
Other ?
Contact Transmission
Requieres contact between source and the host
Direct contact:
Physical contact between source and host
Indirect contact
Transmission via inanimate object called fomite
Fomite = contaminated object
Droplet contact
Transmission via droplets (sneezing/coughing) that travel a short distance <1 meter
Not same as airborne because it travels farther
Vehicle transmission
Transmission via inanimate reservoir like water, food, or air
Microbes spread through a medium
Airborne
Transmission via dust particles or pet dander
Foodborne
Transmission through contaminated, undercooked, or improperly stored food
Other vehicles
Disease can also be transmitted via blood or drugs
Congenital (vertical) transmission
Mother to child
Vector transmission
Animals, typically insects
Mechanical transmission
No biting required
The insect passively carries the microbe on its body
Biological transmission
The insect is an active part of the disease cycle, as the parasite/microbes must go through part f its life cycle inside the vector before it can be transmitted
Usually bites you and injects pathogen
Other ?
Fecal-oral transmission
Infection from swallowing contaminated feces traces
Healthcare-Associated Infections (HAI)
Infections you get while receiving medical care
Not illness you came in for
Affect 4-5% of hospital patients
Healthcare-Assocated Infections (HAI): WHY ?
Microbes in hospitals
Hospital environment is a reservoir
Lots od opportunistic pathogens
Lots of drug resistant microbes (MRSA , etc.)
Compromised host
Someone whose defenses are weakened sue to underlying disease, burns, or therapy
This can be due to a suppressed immune system or having broken skin/mucous membrane (from surgery or IV lines)
Chain of transmission
The ways infection spreads inside hospitals
Direct contact
Staff to patient or patient to patient
Indirect contact
Fomites
Equipment, bedding, clothing
Airborne
The use of devices (like catheters or reparatory devices) to assist patients is a major source of infection
Control of HAI's
Universal
General rules to prevent spread
Standard precautions
Transmission based precautions
Standard precautions
Applies to all patients
Basic, minimum precautions applied to all levels of patient care
Includes, frequent handwashing, aseptic techniques, proper handling of contaminated materials, and educating staff
Use of isolation and wards
Use of ppe
Transmission based precautions
Used to supplement standard precautions when dealing wth individuals who have a known or suspected infection that is highly transmissible
Contact precautions
Droplet precautions
Short distance
Airborne precautions
Long distance
Emerging infectious diseases (EID)
Disease that is
New
Changing
Increasing in numbers
Likely to increase soon
Caused by bacteria, viruses, fungi, protozoa, or worms
75% are zoonotic, mainly of viral origin , and often vector borne
Criteria to identify an EID
- -Disease might be considered emerging if:
Distinctive disease symptoms
Symptoms are new or unusual
Improved diagnostic techniques that allow identification of a new pathogen
A rare disease becoming common
A local disease becoming widespread
A mild disease becoming more severe
Factors contributing to EIDs
Genetic recombination/evolutions
Microbes changing
Misuse of antibiotics/pesticides
Resistance
Climate change
New habitats for vectors
Increased human transportation
Ecological changes
Affecting animal/human contact
Public health failures
Poor vaccination rates
Poor sanitation
Epidemiology:
Where and when diseases occur
How they are transmitted
How to control them
Epidemiology: Study of
Where and when diseases occur
How they are transmitted
How to control them
Epidemiology: Helps determine
Cause of diseases
Patterns of spread
Risk factors
Age, race, income, lifestyle
How well prevention methods work
Epidemiology: Important for
Determining the etiology (cause) of disease
Identifying other important factors concerning the spread of disease
Demographic data, socioeconomic status, etc
Developing methods for controlling disease
(control of reservoirs, food inspection, vaccination)
Assembling data and graphs to outline the incidence of disease
Determine disease frequency
Test effectiveness of disease control (vaccination)
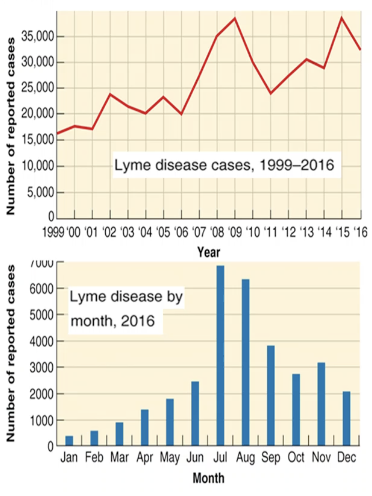
Case reporting
Healthcare workers are required to report specific diseases (like aids, meningitis, or tetanus) to local, state, and national offices
Establishes the chain of transmission
Nationally notifiable Infectious diseases
Diseases that physicians are legally required to report when they occur
CDC
National organization that collects and analyzes epidemiological information in the us and publishes the morbidity and mortality weekly report
Morbidity vs Mortality
Morbidity
The incidence (new cases) of specific notifiable disease
Morbidity rate
Rate at which diseases occurs
Mortality
the deaths form notifiable diseases
Mortality rate
The rate at which death occurs