Neurologic and Psychotheraputic Agents
1/46
Earn XP
Description and Tags
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
47 Terms
status epilepticus
a continuous seizure state (15 minutes)
partial/focal seizure
one hemisphere of the brain
simple
complex
secondary generalized seizure
generalized seizure
both hemispheres involved
tonic-clonic (grand mal)
absence (petit mal)
atonic
myoclonic
status epilepticus
febrile seizure
treatments for epilepsy and seizures
vagus nerve simulator
ketogenic diet (low carb, high fat)
individually tailored
medication, surgery, focal resection, hemispherectomy, corpus callosotomy surgery
important to check in antiepileptic drugs
plasma levels for therapeutic range
Phenytoin (Dilantin)
MOA: decreases Na into cell
For: partial and tonic-clonic seizures, post neuro sx
off label antiarrythmic, severe preeclampsia
AE: nystagmus, ataxia, slurred speech, mental confusion, tremor, gingival hyperplasia (20% of pt’s), increased glucose level, teratogenic effects, purple glove syndrome
NC: therapeutic range is 10-20mcg/mL
take with food
is a vesicant, tears up the blood vessels
Carbamezapine (Tegretol)
MOA: blocks the sodium channels (delayed recovery of sodium channels from their inactivated state)
For: 1st drug of choice for focal seizures, generalized onset of tonic-clonic seizures, also for BPD and pain relief
AE: nystagmus and ataxia (muscle problems)
luekopenia, anemia, and thrombocytopenia, rash and photosensitivity
food and drug interactions: warfarin, oral contraceptives, phenytoin (dilantin), phenobarbital, and grapefruit juice
NC: monitor CBC and PLT, monitor serum blood levels of medications, educate food/drug interactions In solutions administered over 30 minutes
Valproate-divalproex (Depakote)
MOA: Increase availability or enhance the action of the GABA receptor site. This is a pre-curser of valproic acid that separates into valproic acid in GI tract
For: all seizure types, migraine HA and bipolar.
NC: take with food to avoid N/V, fatal hepatotoxicity (rare) avoid liver dysfunction patients.
Check LFTs
Highly teratogenic
Comes in Delayed Release, Extended Release and Immediate Release
Life-threatening pancreatitis
Oxcarbazepine (Oxtellar XR, Trileptal)
MOA: decreases Na into cells
Indications: mono and adjunctive therapy for management of focal seizures
Nursing considerations:
Altered renal function
AEs: dizziness, drowsiness, double vision, nystagmus, headache, ataxia, hyponatremia, hypothyroidism, Stevens-Johnson Syndrome, hypersensitivity
Take without regard to food
XR tablets – swallow whole
↓ effectiveness of oral contraceptives
Multiple drug interactions
Topiramate (Topamax)
MOA: blockade of NA+,CA + & glutamate; potentiation of GABA inhibition.
Indications: 2 yrs for adjunct therapy for focal seizures, primary generalized tonic-clonic seizures and associated with Leenox-Gastaut Syndrome.
Off label bipolar, migraine prophylaxis, neuropathic pain, essential tremors, binge-eating disorders.
Nursing Considerations: Dizziness, weight loss, drowsy,& cognitive effects.
Metabolic acidosis
Suicide risk
Kidney stones, glaucoma & paresthesias are rare
Gabapentin (Neurotin)
MOA: Unknown but may enhance GABA release, thereby increasing GABA inhibition of neuron firing.
Indications: Adjunctive therapy of focal-onset seizures
Off-label use: Neuropathic pain, prophylaxis of migraine, treatment of fibromyalgia, and relief of postmenopausal hot flashes, bi-polar disorder
Adverse Effects: Somnolence, dizziness, ataxia, fatigue, nystagmus, and peripheral edema.
Nursing Considerations: Advise the patient that gabapentin can be taken with or without food.
Instruct to swallow extended-release tablets without breaking, crushing, dissolving, or chewing.
Inform to take gabapentin at bedtime to minimize adverse effects.
Do not suddenly stop gabapentin due to the increased risk of seizures
Levetiracetm (Keppra)
Unique agent that is chemically and pharmacologically different from all other antiseizure drugs
Mechanism of action: Unknown (PO or IV)
Indications: Adjunctive therapy for myoclonic, focal-onset, and generalized-onset tonic-clonic seizures
Adverse effects: drowsiness and asthenia
Neuropsychiatric symptoms (agitation, anxiety, depression, hallucinations)
Drug interaction: Does not interact with other antiseizure drugs
Nursing Considerations: IV infusion over 15 minutes Monitor RBC, WBC, and LFT
Paroxetine (Paxil)
MOA: inhibits neuronal reuptake of serotonin in the CNS-SSRI, thus potentiating the activity of serotonin has little effect on norepinephrine or dopamine.
Indications: GAD, OCD, and Major Depression Disorder
Adverse Effects: Neuroleptic malignant syndrome (fever, shakes, effects BP), suicidal thoughts, stevens johnson syndrome, serotonin syndrome, dizziness, drowsiness, anxiety, headache, insomnia, weakness, constipation, dry mouth, sweating
Nursing Inmplications: Assess for suicidal tendencies and Serotonin Syndrome
Monitor for development of neuroleptic malignant syndrome (fever, respiratory distress, tachycardia, seizures, diaphoresis, HTN or hypotension, pallor, tiredness)
Inform patient that frequent mouth rinses, good oral hygiene and sugarless gum or candy may minimize dry mouth
Advise patient to notify HCP if headache, weakness, anorexia, anxiety or insomnia persists
Buspirone (Buspar)
MOA: mechanism to relieve anxiety is unknown but it binds with high affinity to receptors for serotonin and lower affinity to receptors for dopamine.
Indications: Treatment of anxiety for patients who are known to abuse alcohol or other drugs.
Adverse Effects: Dizziness, nausea, headache, nervousness, lightheadedness, excitement, paresthesia, sleep disturbances, chest pain, tinnitus, nasal congestion, sore throat
Nursing Implications: Do not administer concurrently with MAOI or grapefruit juice
May lead to dizziness, drowsiness, fatigue, and weakness Patient may experience chest pain, palpitations, tachycardia Instruct patient to take as directed Instruct patient to avoid alcohol and other CNS depressants
Diazepam (Valium)
MOA: enhances the action of GABA (PO/IM/IV)
Indications: anxiety, sedation, muscle relaxation, decreased seizure activity with a few general type seizures-not all, and treatment of status epilepticus (Used with a long acting anti-convulsant)
AE: dizziness, drowsiness, depression, slurred speech, HA, N/V, constipation, rash, dry mouth, sexual dysfunction
Nursing Implications:
gradual withdrawal is recommended
avoid driving if drowsiness occurs
notify MD if pregnant
increase fluids consumed
rise slowly from a seated position
avoid caffeine
avoid other CNS depressant
Fluoxetine (Prozac) SSRI
MOA: blocks reuptake of serotonin increases serotonin in in the brain
Produces CNS excitation
Indications: major depression, bipolar disorder, panic disorder, OCD
~4 weeks to reach a steady state
Nursing implications:
Common AEs: weight gain, nausea, suicidal thoughts, sexual dysfunction, insomnia
Serotonin syndrome: begins w/in 2-72 hours
Concurrent use of MAOIs increases risk (shivers acronym)
Confusion, agitation, disorientation, anxiety, AMS
Spontaneous resolution when medication stopped
Venlafaxine (Effexor XR) SNRI
MOA: blocks reuptake of serotonin and norepinephrine, gives more serotonin and norepinephrine in the body
SSRIs may be better tolerated
Indications: GAD, major depression, social anxiety disorder, panic disorders
Nursing implications:
Common AEs: N/V, headache, HTN, nervousness, anorexia,insomnia
Taper over 2 weeks to avoid withdrawal
Serotonin syndrome
Imipramine (Tofranil) tricyclic antidepressant
MOA: block reuptake of serotonin and norepinephrine – multiple pathways
Prolonged half-life = once daily dosing
Indications: depression, bipolar disorder, fibromyalgia syndrome
Nursing implications:
Common AEs: sedation, orthostatic hypotension, anticholinergic effects: dry mouth, blurred vision, urinary retention, constipation, tachycardia, photophobia
Serious AEs: cardiac toxicity, sudden death
Overdose: lethal dose = 8x average therapeutic dose
Treatment = gastric lavage, activated charcoal
Give suicidal patients 1-week supply = minimize overdose
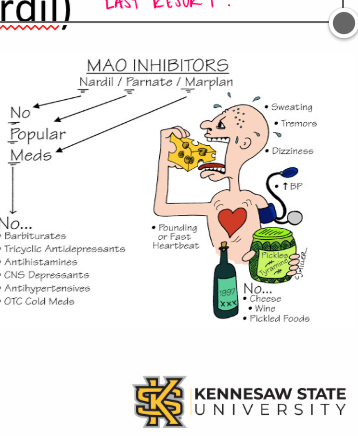
Phenelzine (Nardil) MAOI’s
MOA: block monoamine oxidase, ↑ NE, dopamine, serotonin, and tyramine
Indications: depression, bulimia nervosa, panic disorder, PTSD, OCD
Nursing implications: does not work well with other drugs, and is last resort for depression med
Common AEs: orthostatic hypotension, many drug interactions
Hypertensive crisis when tyramine-rich foods are consumed
MAO Inhibitors AE
sweating
dizziness
increased pounding HR
NO cheese, wine, pickled foods
Bupropion (Wellbutrin)
atypical antidepressants
MOA: blocks dopamine and/or NE reuptake
Effects seen 1-3 weeks
Indications: major depression, prevention of SAD, unlabeled ADHD
Zyban or Buproban (bupropion): smoking cessation
Nursing implications:
Common AEs: agitation, headache, dry mouth, constipation, weight loss, GI upset, dizziness, tremor, insomnia, blurred vision, tachycardia, seizures
NO sexual dysfunction all is wellbutrin
weight loss AE considerations
Look at patients BMI prior to administering, do not give if anorexic or if have risk of seizures
weight loss AE medications
Bupropion (Wellbutrin)
Venlafaxine (Effexor XR) SNRI
Topiramate (Topamax)
Amphetamine-dextroamphetamine (Adderall)
Alprazolam (Xanax)
•PO benzodiazepine
•MOA: Potentiates GABA’s effects by increased neuronal membrane permeability of chloride ions
•Indications:
Anxiety disorders and procedural anxiety; drug of choice for anxiety
Off-label for acute treatment of vertigo
•Adverse Effects:
Central nervous and respiratory system depression
Anterograde amnesia
Paradoxical effects, including excitation and euphoria
Abuse and misuse
•Nursing Considerations:
Adverse effects may often be worsened due to concurrent CNS depressant use
Antidote: IV flumazenil (Romazicon)
Monitor for anxiety signs and symptoms and progression while on pharmacotherapy along with non-pharmacological treatment measures
Zolpidem (Ambien)
•PO sedative-hypnotic
•MOA: Potentiates GABA’s effects via selective agonism at the benzodiazepine-1 receptor to increase chloride conductance to help with insomnia
•Adverse Effects:
Central nervous system depression, including next-day drowsiness and decreased mental alertness
Complex sleep behaviors
Other psychiatric and behavioral effects, including hallucinations, delirium, and worsening of depression
Withdrawal with chronic administration of supratherapeutic doses
Women need half the dose that men do
•Nursing Considerations:
Rapid onset (30 minutes) can help with people having difficulty falling asleep and duration (6 - 8 hours) can help with people staying asleep
Should only be used if insomnia cannot be managed by other means, including non-drug measures, and by addressing any underlying pathology
Acute Dystonia
Spasm of muscles of the tongue, face, neck, and back
Parkinson’s
Bradykinesia, masklike facies, tremor, rigidity, shuffling gait, drooling, stooped posture
Akathisia
Compulsive, restless movement, symptoms of anxiety, agitation
Tardive Dyskinesia
Oral-facial dyskinesiasthat develop after prolonged use of antipsychotic medications, characterized by involuntary movements of the face, tongue, and limbs.
Haloperidol
1st generation antipsychotic
•MOA: Blocking dopamine receptors in the brain.
•High potency —> give less
•Peaks 2-6 hrs
•Indications: Schizophrenia, acute psychosis, & Tourette's syndrome
•Nursing implications:
•Common AEs: acute dystonia, parkinsonism, akathisia.
•Uncommon AE: sedation, hypotension, and anticholinergic effects.
•Caution with dysrhythmias causes long QT syndrome.
•Neuroleptic malignant syndrome-high fever, BP fluctuation, dysrhythmias, muscle rigidity, diaphoresis, tachycardia, & change in LOC.
•Stop antipsychotic medication!
Neuroleptic Malignant Syndrome Acronym
FEVER
Fever
Encephalopathy
Vs unstable
Elevated CPK Rigidity
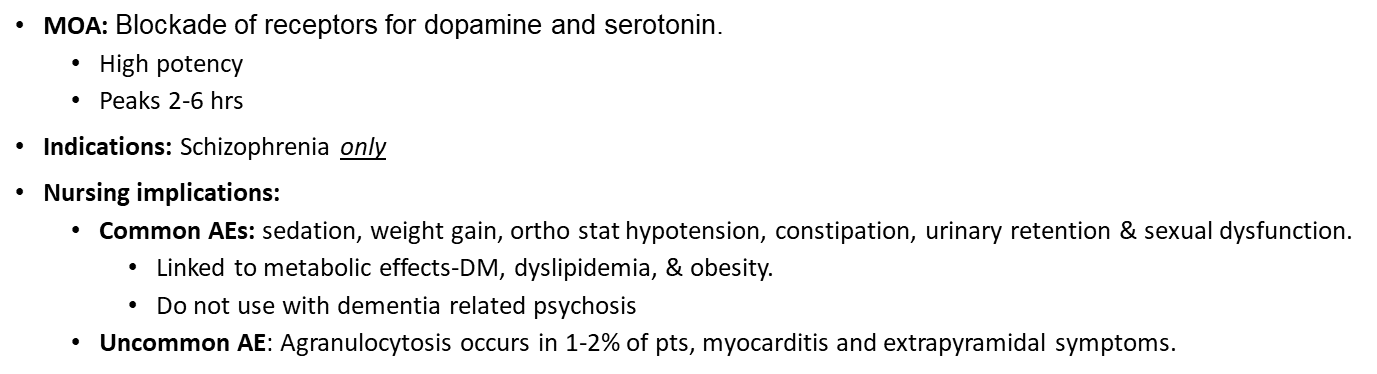
Clozapine (Clozaril)
2nd generation antipsychotic
MOA: Blockade of receptors for dopamine and serotonin.
•High potency
•Peaks 2-6 hrs
•Indications: Schizophrenia only
•Nursing implications:
•Common AEs: sedation, weight gain, ortho stat hypotension, constipation, urinary retention & sexual dysfunction.
•Linked to metabolic effects-DM, dyslipidemia, & obesity.
•Do not use with dementia related psychosis
•Uncommon AE: Agranulocytosis occurs in 1-2% of pts, myocarditis and extrapyramidal symptoms.
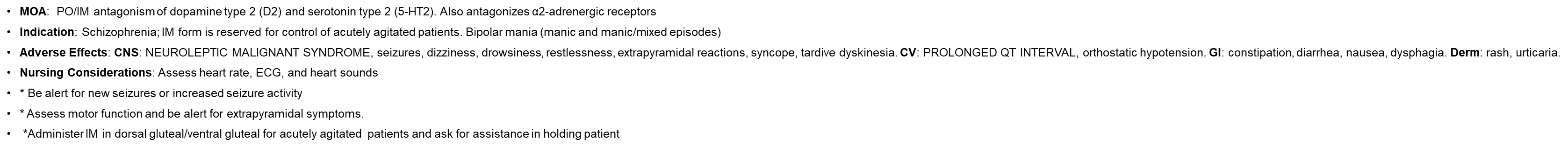
Ziprasidone (Geodon)
•MOA: PO/IM antagonism of dopamine type 2 (D2) and serotonin type 2 (5-HT2). Also antagonizes α2-adrenergic receptors
•Indication: Schizophrenia; IM form is reserved for control of acutely agitated patients. Bipolar mania (manic and manic/mixed episodes)
•Adverse Effects: CNS: NEUROLEPTIC MALIGNANT SYNDROME, seizures, dizziness, drowsiness, restlessness, extrapyramidal reactions, syncope, tardive dyskinesia. CV: PROLONGED QT INTERVAL, orthostatic hypotension. GI: constipation, diarrhea, nausea, dysphagia. Derm: rash, urticaria.
•Nursing Considerations: Assess heart rate, ECG, and heart sounds
•* Be alert for new seizures or increased seizure activity
•* Assess motor function and be alert for extrapyramidal symptoms.
• *Administer IM in dorsal gluteal/ventral gluteal for acutely agitated patients and ask for assistance in holding patient
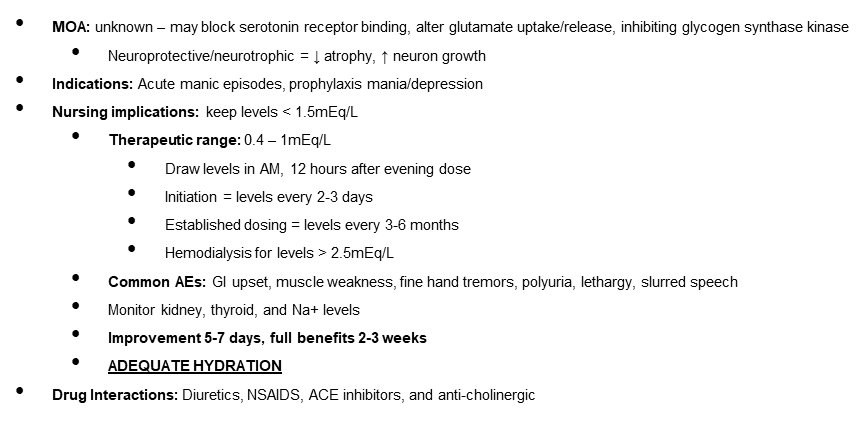
Lithium (Lithobid) - mood stabilizer
•MOA: unknown – may block serotonin receptor binding, alter glutamate uptake/release, inhibiting glycogen synthase kinase
•Neuroprotective/neurotrophic = ↓ atrophy, ↑ neuron growth
•Indications: Acute manic episodes, prophylaxis mania/depression
•Nursing implications: keep levels < 1.5mEq/L
•Therapeutic range: 0.4 – 1mEq/L
•Common AEs: GI upset, muscle weakness, fine hand tremors, polyuria, lethargy, slurred speech
•Monitor kidney, thyroid, and Na+ levels
DO NOT DRINK ALCOHOL!
•Improvement 5-7 days, full benefits 2-3 weeks
•ADEQUATE HYDRATION
•Drug Interactions: Diuretics, NSAIDS, ACE inhibitors, and anti-cholinergic
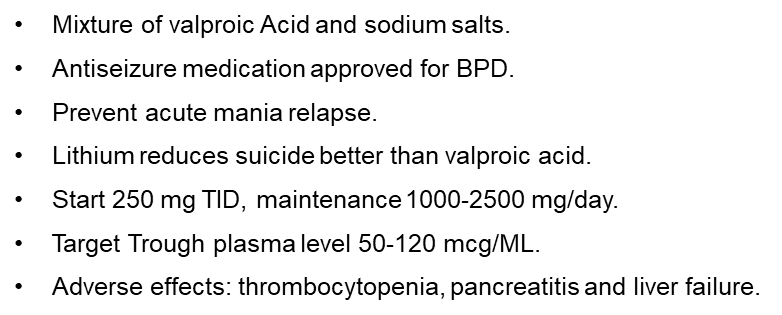
Divalproex sodium (Valproate)
Antiepileptic Drug
•Mixture of valproic Acid and sodium salts.
•Antiseizure medication approved for BPD.
•Prevent acute mania relapse.
•Lithium reduces suicide better than valproic acid.
•Start 250 mg TID, maintenance 1000-2500 mg/day.
•Adverse effects: thrombocytopenia, pancreatitis and liver failure.
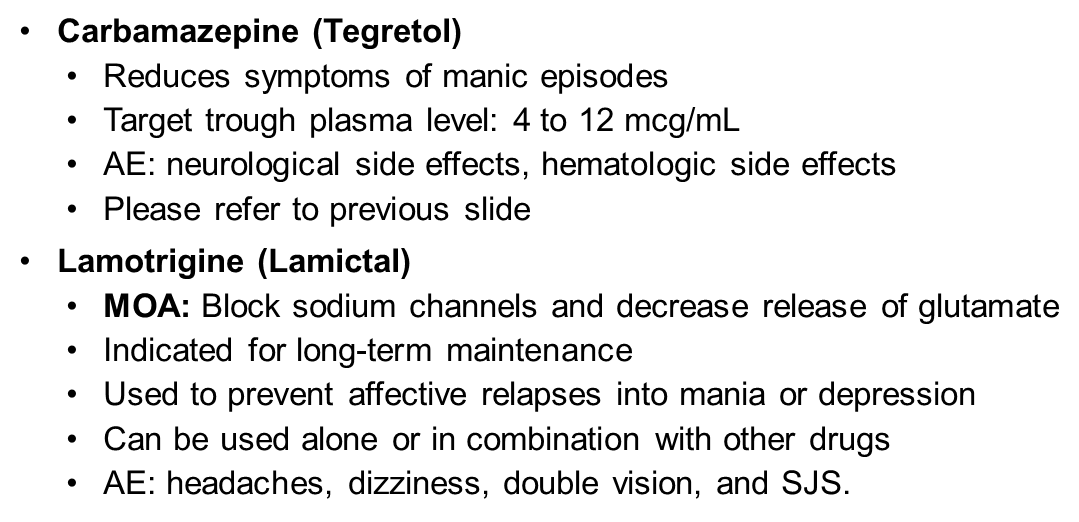
Antiepileptic drugs used for Bipolar
•Carbamazepine (Tegretol)
•Reduces symptoms of manic episodes
•Target trough plasma level: 4 to 12 mcg/mL
•AE: neurological side effects, hematologic side effects
•Please refer to previous slide
•Lamotrigine (Lamictal)
•MOA: Block sodium channels and decrease release of glutamate
•Indicated for long-term maintenance
•Used to prevent affective relapses into mania or depression
•Can be used alone or in combination with other drugs
•AE: headaches, dizziness, double vision, and SJS.
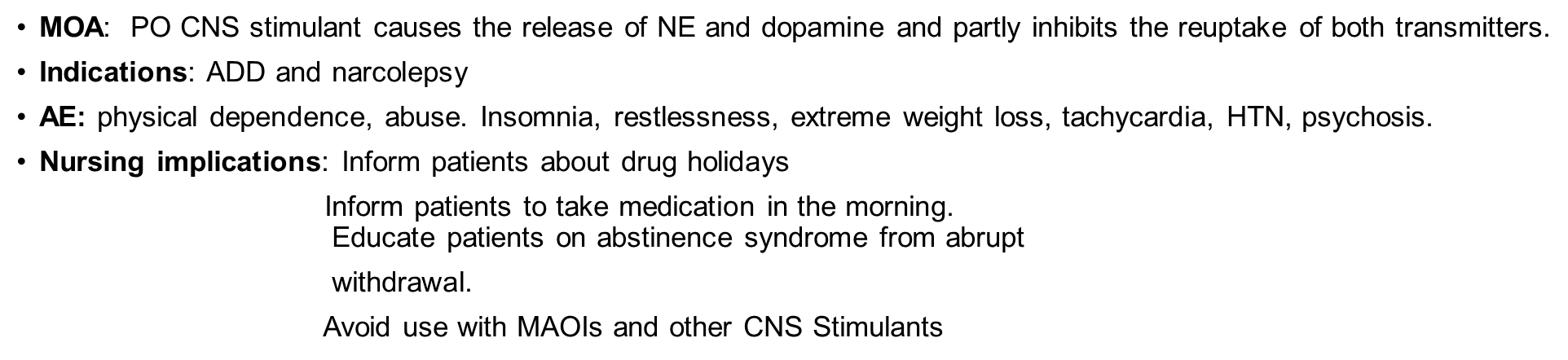
Adderall
•MOA: PO CNS stimulant causes the release of NE and dopamine and partly inhibits the reuptake of both transmitters.
•Indications: ADD and narcolepsy
•AE: physical dependence, abuse. Insomnia, restlessness, extreme weight loss, tachycardia, HTN, psychosis.
•Nursing implications: Inform patients about drug holidays
Inform patients to take medication in the morning.
Educate patients on abstinence syndrome from abrupt
withdrawal.
Avoid use with MAOIs and other CNS Stimulants
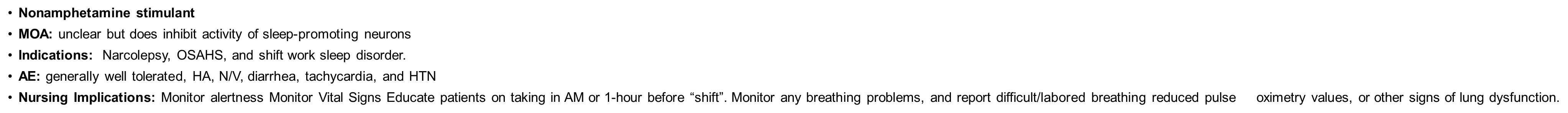
Modafanil (Provigil)
•Nonamphetamine stimulant
•MOA: unclear but does inhibit activity of sleep-promoting neurons
•Indications: Narcolepsy, OSAHS, and shift work sleep disorder. Those who work night shift, take one hour before shift starts.
•AE: generally well tolerated, HA, N/V, diarrhea, tachycardia, and HTN
•Nursing Implications: Monitor alertness Monitor Vital Signs Educate patients on taking in AM or 1-hour before “shift”. Monitor any breathing problems, and report difficult/labored breathing reduced pulse oximetry values, or other signs of lung dysfunction.
Methylphenidate (RItalin)
MOA: promotion of NE and DA release, inhibition of NE and DA reuptake
works different than the others, leaves more in the body
For: ADHD and narcolepsy
AE: insomnia, reduced appetite, emotional liability, and abuse liability
NC: same as amphetamines
The nurse identifies the mechanism of action of the amphetamines as what? (Select all that apply.)
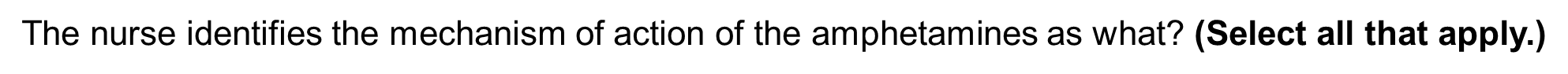
A. causing the release of norepinephrine
C. causing the release of dopamine
D. inhibiting the reuptake of norepinephrine
E. inhibiting the reuptake of dopamine release
Which medication should the nurse question prescribed to a patient taking lithium?
Furosemide (Lasix)
Renal function should be evaluated before the administration of Lithium, patients with reduced renal function are at risk for lithium toxicity
What are the s/s of lithium toxicity?
polydipsia, slurred speech, and fine hand tremors
Think of a person getting pulled over and they seem drunk - however it is just lithium toxicity
T/F: older patients require smaller doses of antipsychotics?
True; typically 30-50% of older patients require a smaller dosage
A patient is diagnosed with type 2 diabetes mellitus and schizophrenia. The nurse will closely monitor the blood sugar if the patient receives which medication for the treatment of schizophrenia?

Clozapine (Clozaril)
2nd generation antipsychotics carry a higher risk of serious metabolic effects (such as diabetes and dyslipidemia) than 1st generations (loxapine, thioxene, haloperidol). Clozapine should be used with caution in patients with diabetes.
What are manifestations are associated with tardive dyskinesia?
Twisting, worm-like movements of the tongue and face
2nd & 3rd generation antipsychotics
MOA: 2nd blocks serotonin & < dopamine receptors
3rd stabilize dopamine system both agonist and antagonist.
1st generation antipsychotics
MOA: blocks dopamine, acetylcholine, histamine and norepinephrine receptors in the brain and periphery