SALIVARY GLANDS
1/83
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
84 Terms
what provides defence for the oral cavity
the mucosa - physical barrier
palatine tonsils - lymphocyte and dendritic cells
salivary glands
how do salivary glands provide defence for the oral cavity
saliva washes away food particles that bacteria or viruses may use for metabolic support
the glands are surrounded by the lymphatic system and therefore have good blood supply - efficient delivery of immune cells
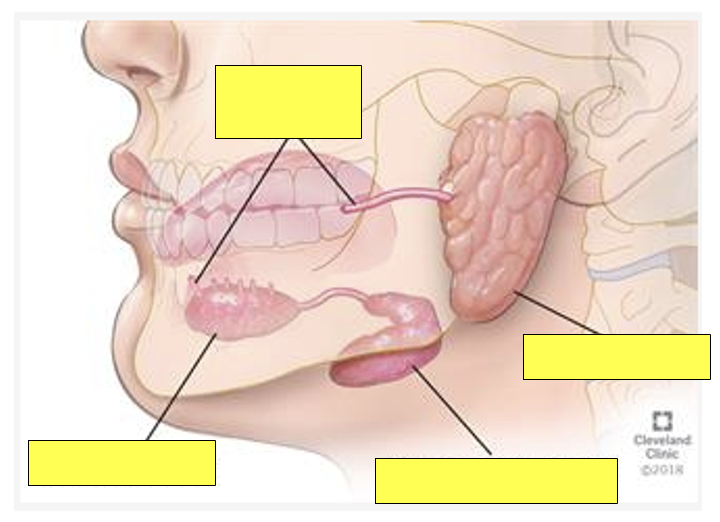
what are the major salivary glands
parotid
submandibular
sublingual
are the major salivary glands paired or unpaired
the major salivary glands are paired
what % of saliva do the major salivary glands collectively produce
the major salivary glands contributes to ≈ 80% of salivary flow
where are minor salivary glands located
submucosa of oral mucosa
lips
cheeks
hard palate
soft palate
tongue
what % of saliva do the minor salivary glands collectively produce
≈ 20%
which major salivary gland(s) are continuously active
submandibular
sublingual
UNSTIMULATED SECRETION
which major salivary gland(s) are not continuously active
parotid
becomes the main source of saliva when stimulated - thinking about eating/ eating something
which gland is more dominant in unstimulated saliva secretion
submandibular gland
what does ‘whole saliva’ consist of (5)
salivary gland secretions
blood
oral tissues
microorganisms
food remnants
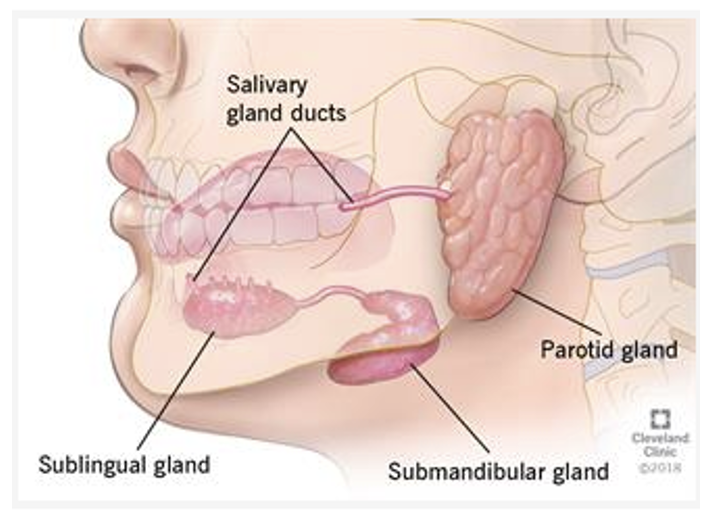
between which structures does the parotid gland lie
superficial triangular outline between
zygomatic arch
sternocleidomastoid
ramus of mandible
masseter muscle
medial pterygoid muscle
what is another term for the parotid duct
Stenson’s duct
describe the location of the parotid/ Stenson’s duct and state where it enters the oral cavity
crosses masseter
pierces buccinator and enters oral cavity at upper 7s
what structures pass through the parotid gland (3)
external carotid artery and its terminal branches
retromandibular vein
facial nerve and its branches to the muscles of facial expression
which major salivary glands are encapsulated and which are not
parotid + submandibular: encapsulated
sublingual: non-encapsulated
what are acini
secretory units mostly found in exocrine glands that produce saliva
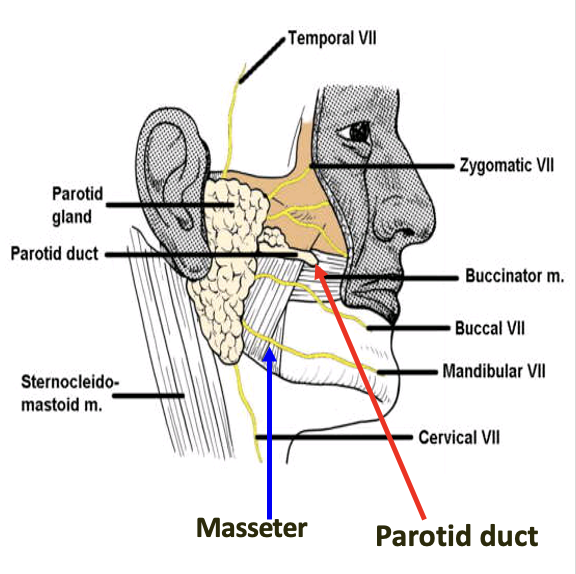
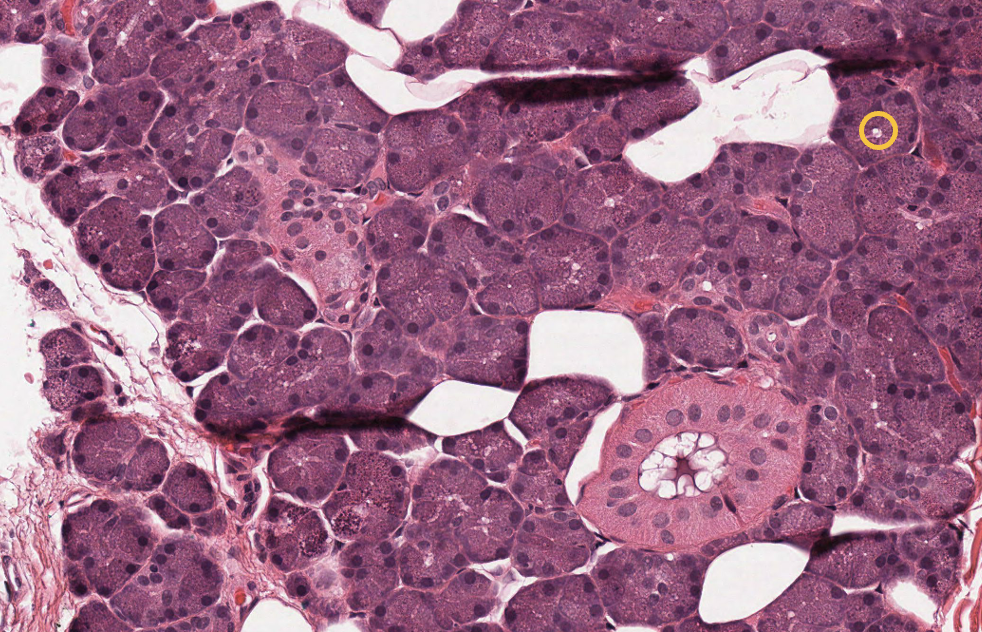
what type of acini are parotid glands made up of
parotid glands
entirely serous acini
with ducts interspersed (blue circle)
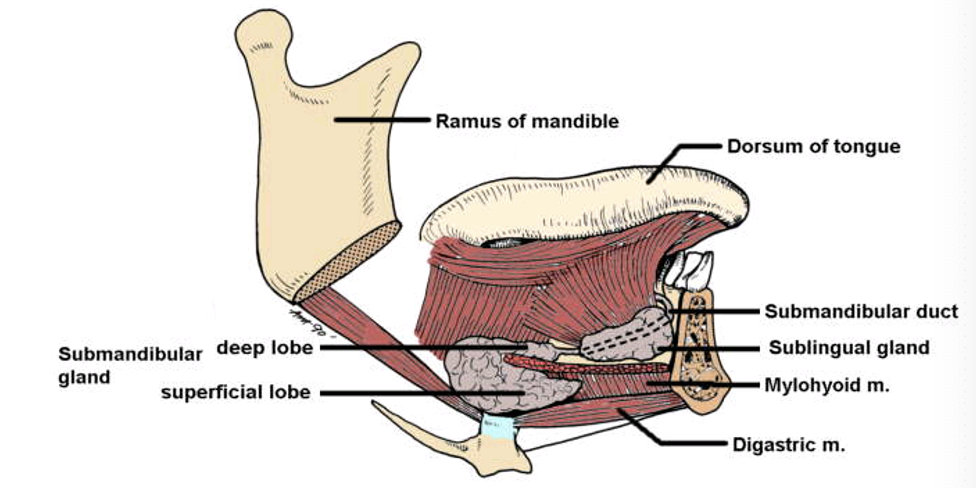
how is the submandibular gland divided
submandibular gland
two lobes separated by mylohyoid muscle
larger superficial lobe
smaller deep lobe (in floor of mouth)
what is another term for the submandibular duct
Wharton’s duct
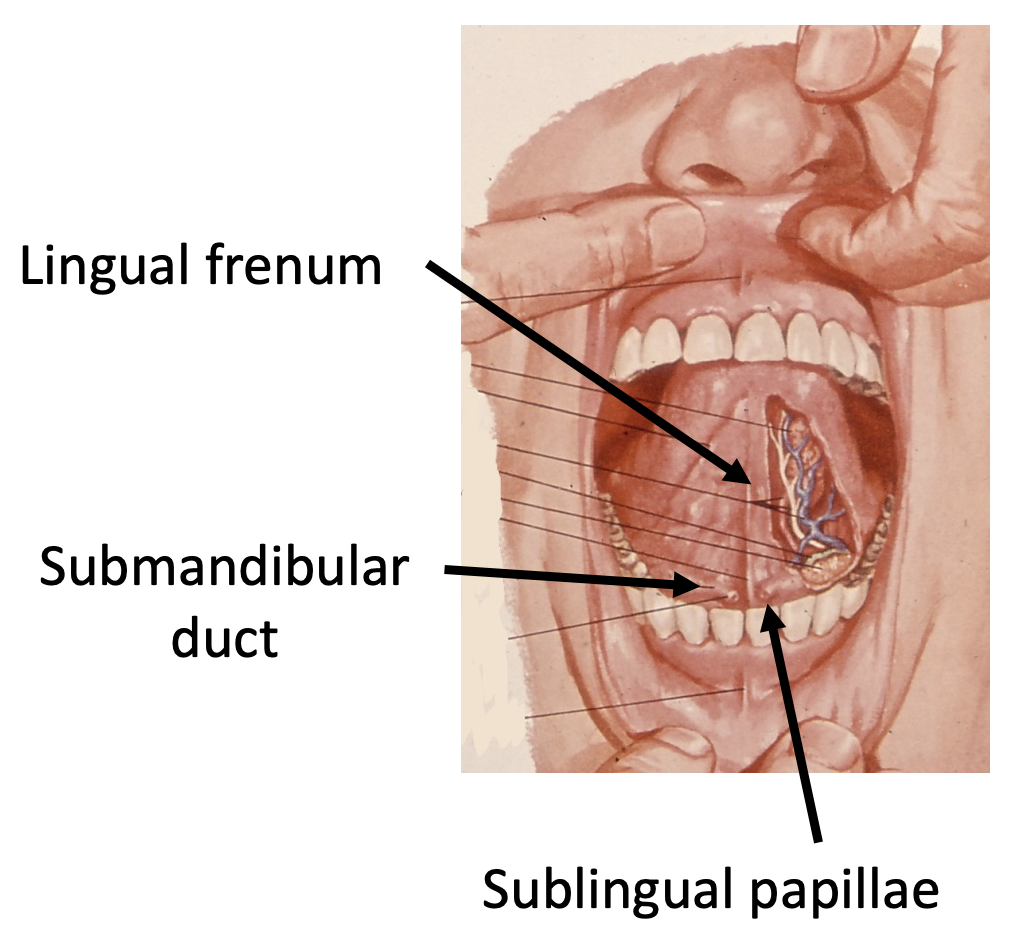
describe the course of the submandibular/ Wharton’s duct
begins in superficial lobe
wraps around free posterior border of mylohyoid muscle
runs along the floor of the mouth
the submandibular duct empties into the oral cavity at the sublingual papillae
diagram showing the lingual frenum, submandibular duct and sublingual papillae
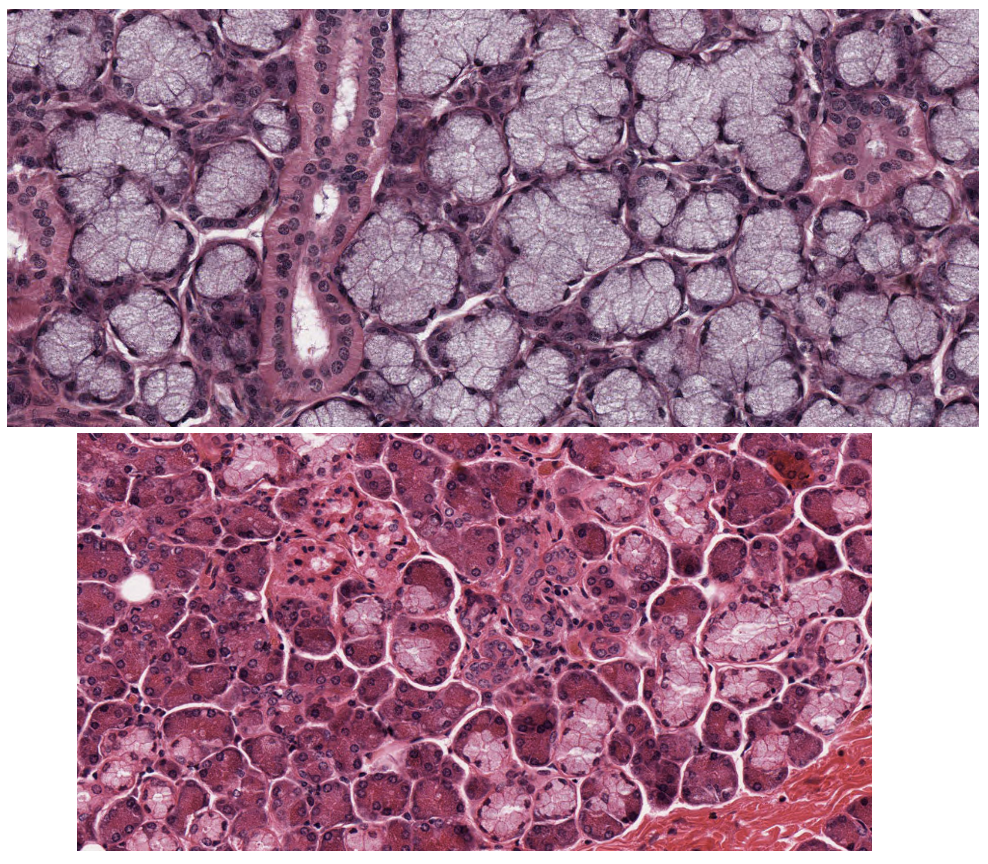
what type of acini are submandibular glands made up of
mixed gland
serous and mucous acini
referred to as seroumucous
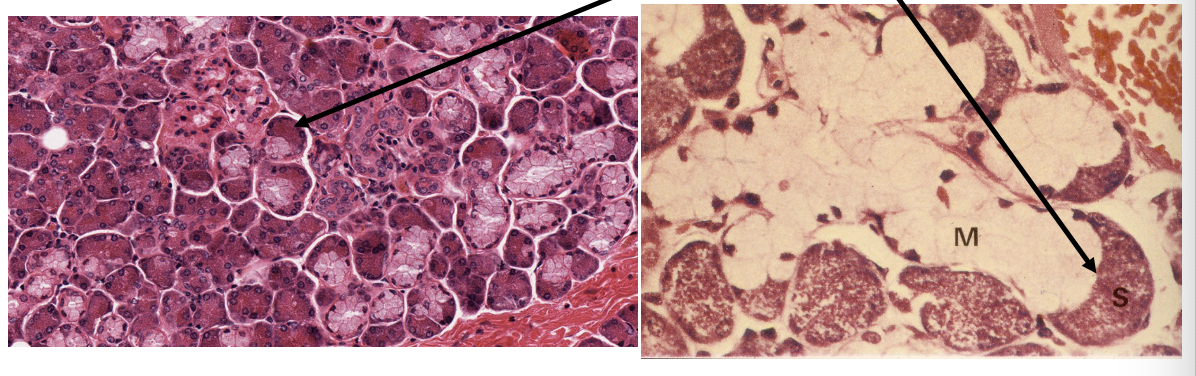
describe the serous acini in submandibular glands
the serous acini are arranged as crescent shaped groups of glandular cells at the base of mucous acini
serous demilunes
describe the location of the sublingual glands
in the floor of mouth between the mylohyoid muscle and oral mucosa of the FOM
what characteristic of the sublingual gland is variable
its size
what is another term for the sublingual duct
THE SUBLINGUAL GLAND DOES NOT HAVE A (LARGE) DUCT
if the sublingual gland has no duct, where does the saliva drain into?
the saliva drains into the submandibular duct/ Wharton’s duct and/ or small ducts that pierce the oral mucosa on the FOM
what is the result of the Wharton’s duct draining both submandibular and sublingual saliva
pure submandibular/ sublingual saliva cannot be collected because both come out of Wharton’s duct
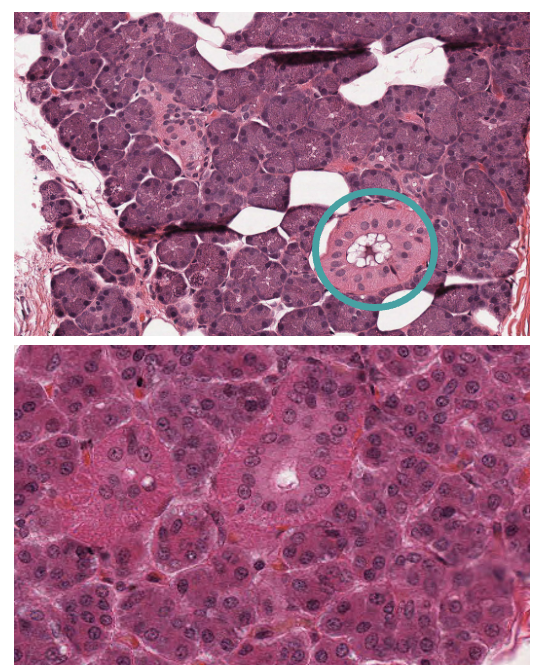
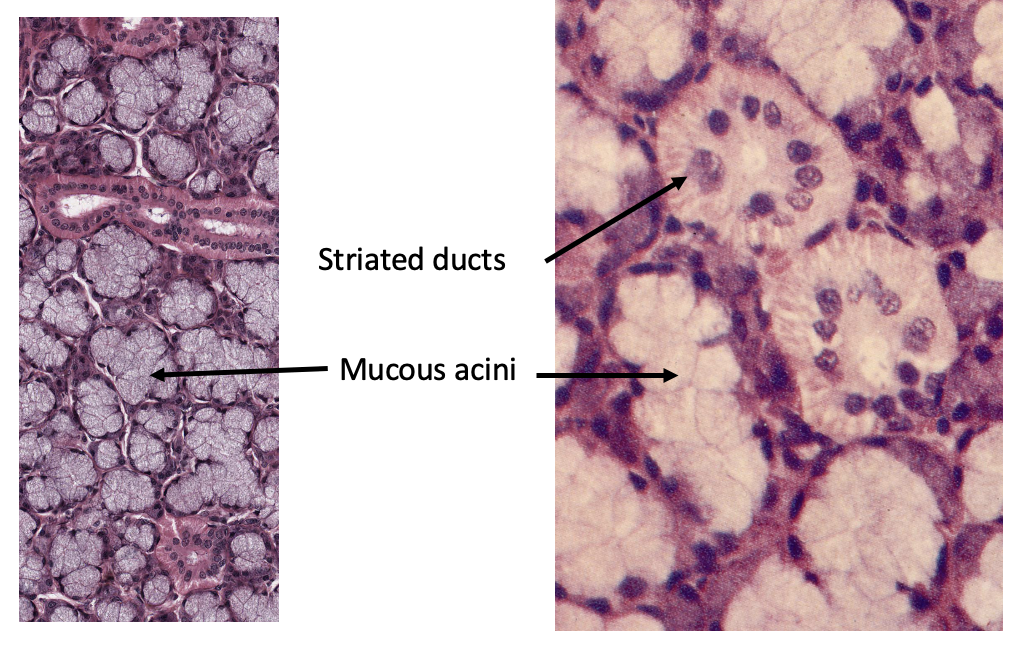
what type of acini are sublingual glands made up of
mixed gland
serous and mucous acini
mainly mucous acini
histological image of sublingual gland
sublingual has intercalated ducts but NOT striated
where are minor salivary glands concentrated
minor salivary glands are concentrated in the:
buccal
labial
palatal
lingual
regions
where else are minor salivary glands also found
superior pole of tonsils (Weber’s glands)
tonsillar pillars i.e. palatoglossal and palatopharyngeal arches
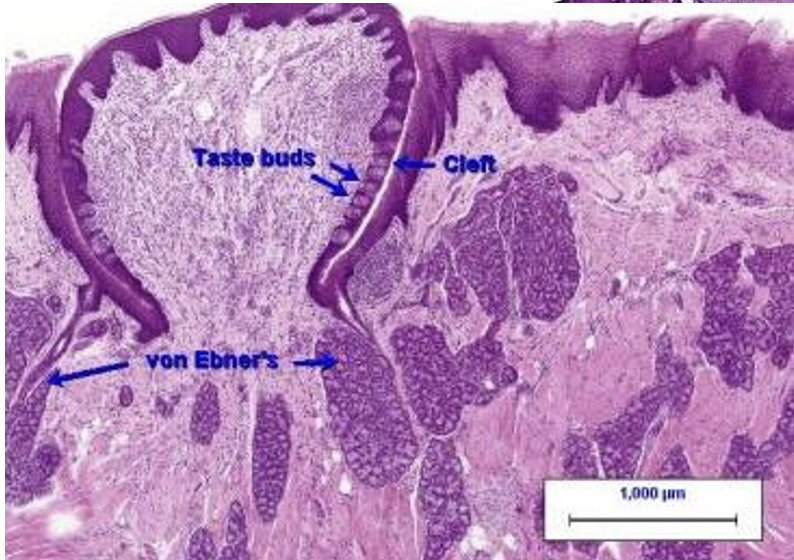
base of the tongue (von Ebner’s glands - underlying circumvallate papillae)
describe the acini of minor salivary glands
all minor salivary glands are mucous
except serous glands of von Ebner
histological image of taste buds and von Ebner’s glands
what structure do minor salivary glands lack and what is the result of this
minor salivary glands lack a branching network of draining ducts
each salivary unit has its own simple duct
what is the effect of parasympathetic stimulation on saliva production
stimulation of parasympathetic nerves causes the production of a copious flow of saliva
what does sympathetic stimulation cause production of
sympathetic stimulation selectively causes secretion of protein and glycoprotein
what is the basic structure of salivary glands
composed of two morphologically distinct epithelial tissue
acinar cells
ducts - collect to form large duct entering the mouth
what other features do salivary glands have
equipped with channels and transporters in the apical and basolateral membranes
this enables transport of fluid and electrolytes
describe serous acini
serous acini
dark staining
nucleus in basal third
small central duct (orange circle in histological image)
secrete water and alpha amylase
describe mucous acini
mucous acini
pale staining - ‘foamy’
nucleus at base
large central duct
secrete mucous and glycoproteins
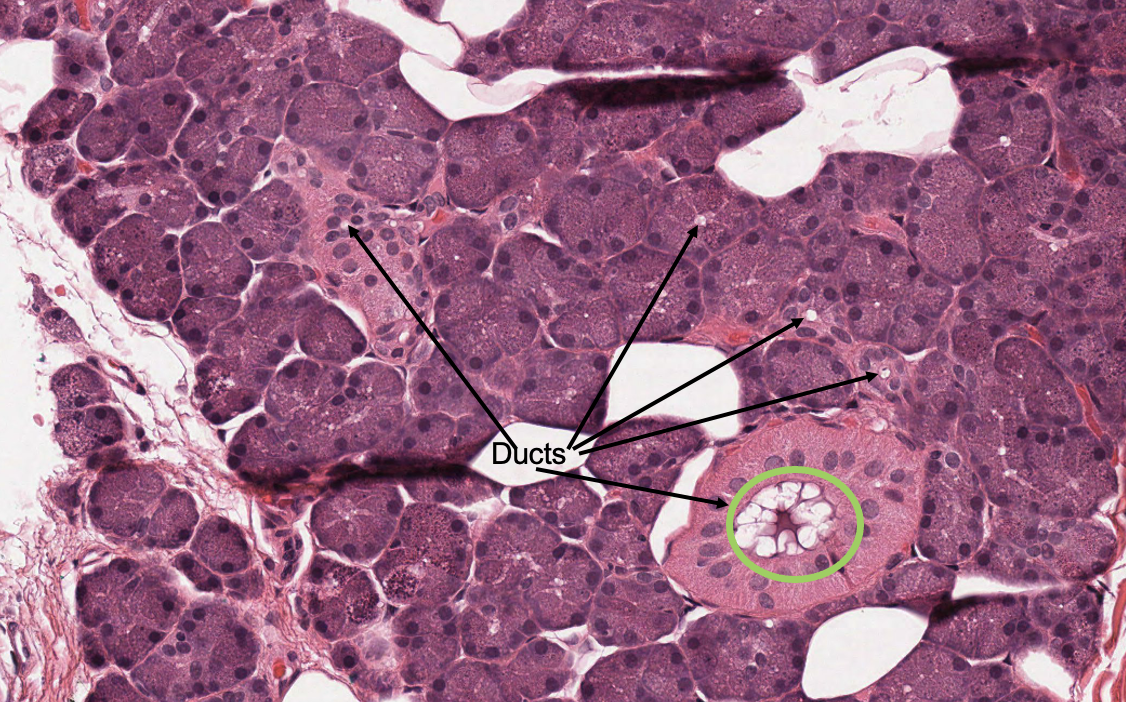
identify the type of acini shown and state what the green circle represents
serous acini
green circle: large striated duct
what are intralobular ducts
intralobular ducts: small duct within an exocrine gland that drains the secretions from the acini and transport them towards the interlobular ducts
what are intralobular ducts divided into
intercalated
striated
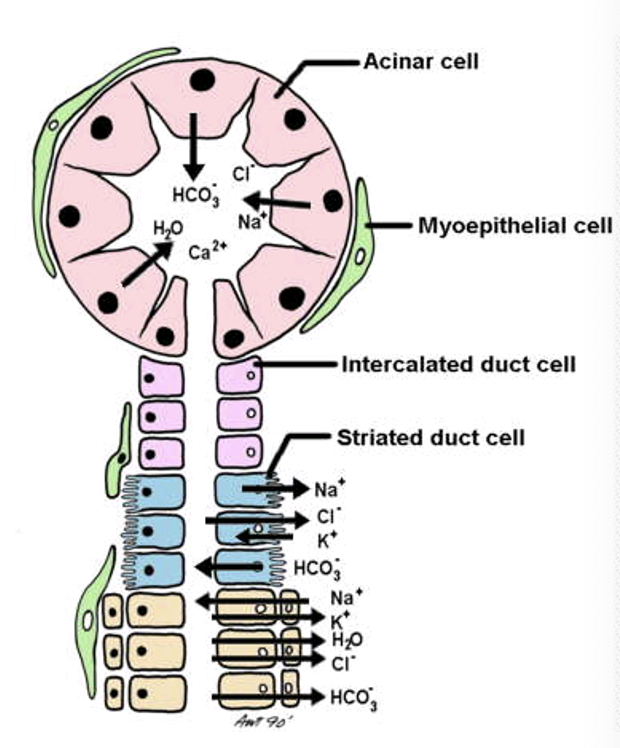
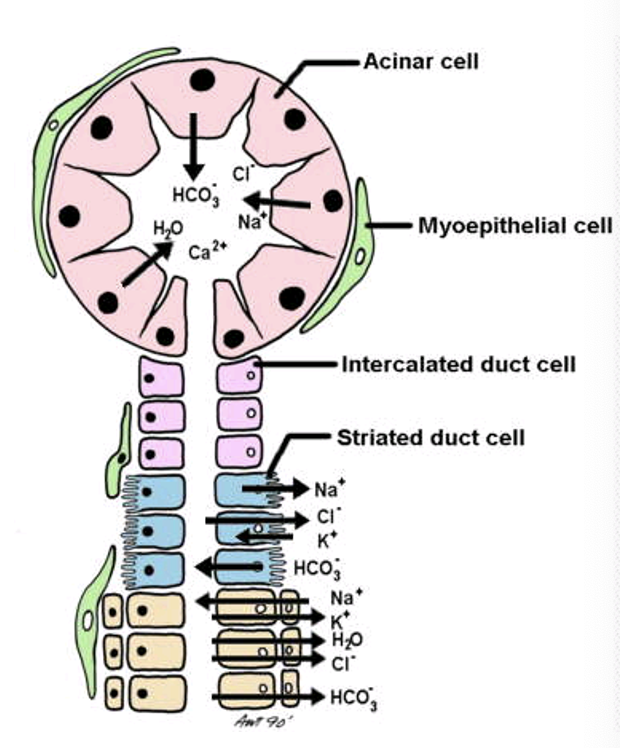
outline intercalated ducts
intercalated ducts: short narrow duct segments with cuboidal cells that connect acini to larger striated ducts
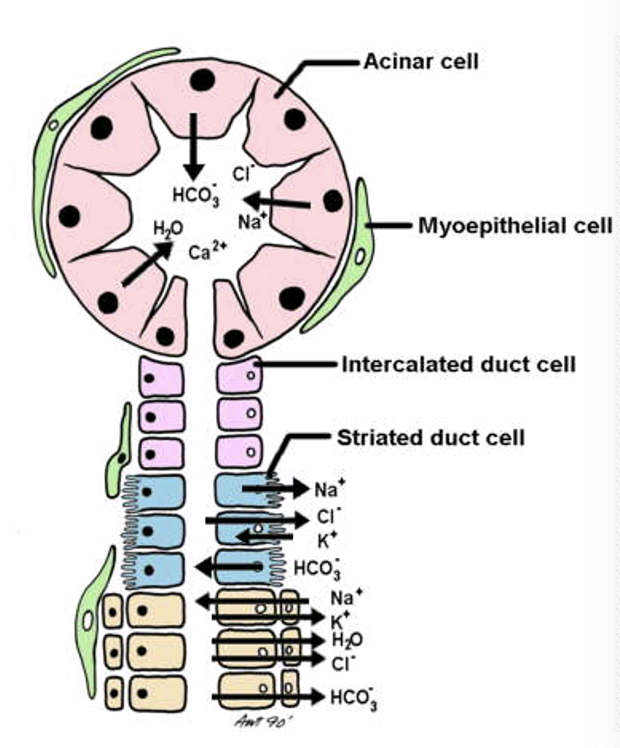
outline striated ducts
appear striated at the basal end because…
basal membrane is highly folded into microvilli for active transport of HCO3 against the concentration gradient
microvilli are filled with mitochondria that produce energy to facilitate the active transport of salts
what is the function of striated ducts
striated ducts: major site for reabsorption of NaCl, this movement of salt alters the final composition of saliva
what is the composition of primary saliva
NaCl rich
isotonic
plasma-like fluid secreted by acini
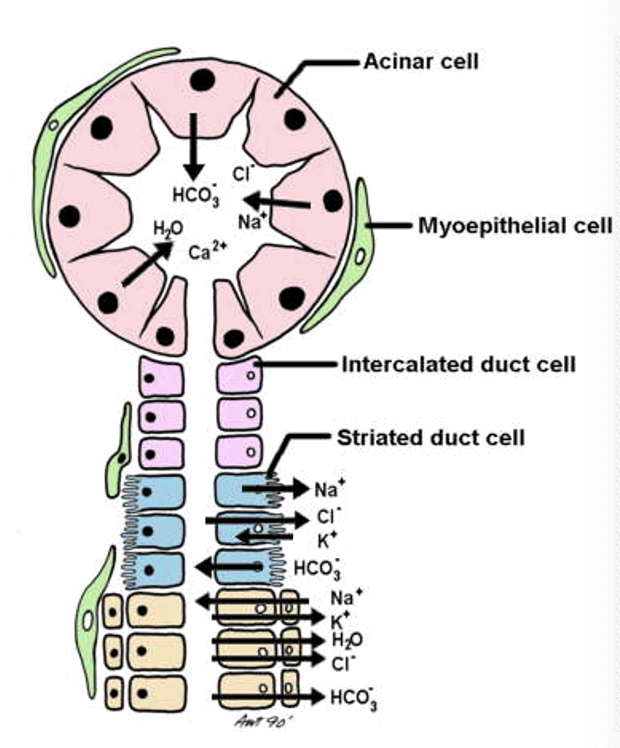
how does the composition of primary saliva change
the composition of primary saliva changes as it moves down the striated duct
K+ and HCO3- are secreted
Na+ and Cl- are reabsorbed
the final saliva becomes hypotonic
why is the final saliva hypotonic
because the epithelium of the duct does not allow any water movement
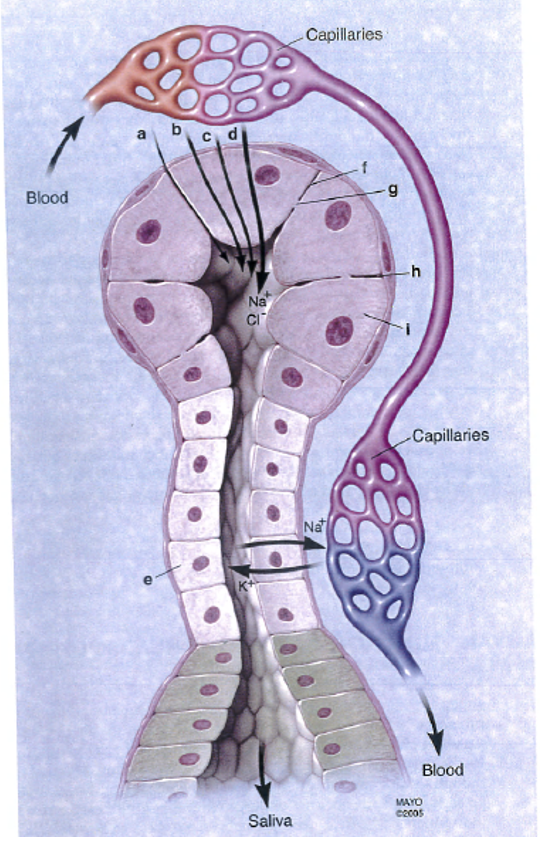
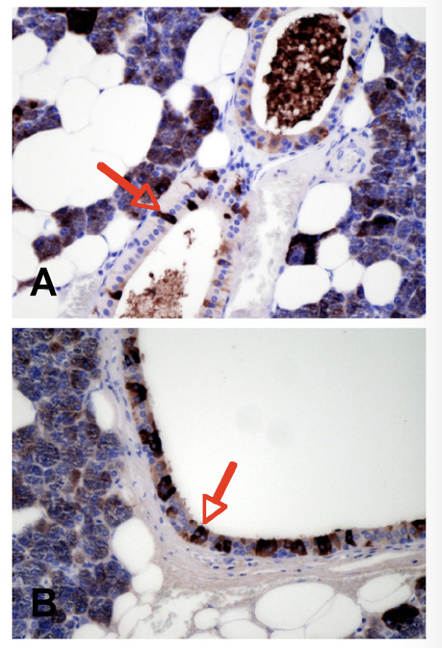
what does this diagram show
the close proximity of the acinar cells to the lymphatic/ blood system
in what field are salivary glands a target tissue for
gene therapeutics - gene transfer technology
what are advantages of salivary glands (4)
well-encapsulated - limits undesirable spread of vectors
luminal membranes (membrane orientated towards the lumen) are easy to access in a relatively non-invasive manner
one single salivary gland is not crucial for life and can therefore be removed with little morbidity
salivary glands normally make large amounts of protein for export
less relevant and ? advantages of salivary glands (2)
salivary epithelial cells are well differentiated and very slowly dividing, providing a stable cell population for non-integrating vectors
ductal access of salivary glands use a limited fluid volume that is not diluted or disseminated following delivery, enabling use of low vector doses
how can salivary flow be restored
use the AQP gene that codes for a water channel
water channel is inserted into the membrane of the duct
duct becomes more permeable therefore increased salivary flow
which salivary gland is the most affected (gland) by radiation and why
parotid gland
it is often in the radiation pathway
» dry mouth
what are the two general pathways for protein secretion
regulated exocrine pathway
major regulated
minor regulated
constitutive endocrine pathway
outline the regulated pathway
external stimulus dependent
proteins stored in secretory granules prior to stimulation with secretion being directed apically into saliva
what is exocrine secretion triggered by
primarily triggered by sympathetic nervous system
secondarily triggered by parasympathetic nervous system
outline the constitutive and constitutive-like pathway
non-directional
continuous secretion of protein
not modulated by external stimuli
outline xerostomia
dry mouth
may be a consequence of cystic fibrosis or Sjogrens syndrome
most common causes: medication and irradiation for head and neck cancers
high prevalence of dental caries and candida infections in those with xerostomia
—
NOT A DISEASE MORE A CONSEQUENCE/ SYMPTOM
what are the types of salivary gland diseases and dysfunctions (4)
obstructive
inflammatory
degenerative
drug side effects
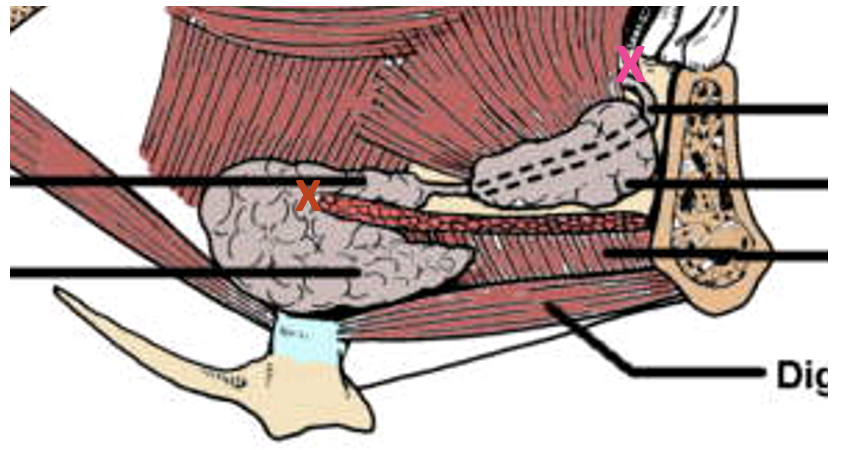
outline obstructive salivary gland disease
saliva contains calcium and phosphate ions that can form salivary calculi (stones)
most often found in submandibular glands (80%)
block duct at the bend around the mylohyoid muscle (red X) OR the exit at the sublingual papillae (pink X)
what is the name given to the condition of having salivary stones
sialolithiasis
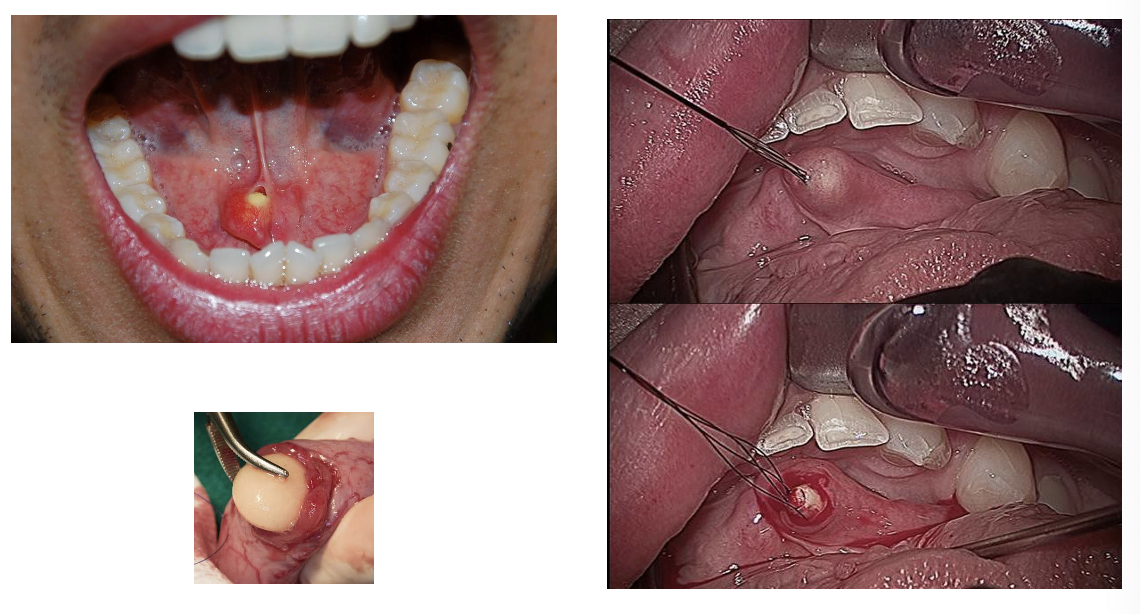
what are the treatment options for sialolithiasis
laser directed at salivary calculi to break them into smaller pieces
oral surgeons can excise the salivary gland stone
outline inflammatory salivary gland disease
infection secondary to blockage i.e. on the other side of the blockage
example of inflammatory salivary gland disease is mumps
viral infection
causes inflammation, swelling and pain - particularly the parotid gland
pain is due to the capsule
fever, malaise
outline degenerative salivary gland disease
complication of radiotherapy to head and neck for cancer treatment
example of degenerative salivary gland disease is Sjogren’s syndrome
mainly affects post-menopausal females
affects salivary and lacrimal glands » dry mouth + dry eyes
rheumatoid arthritis may also be present
outline drug side effects in relation to salivary gland disease
≈ 500 prescription drugs have a sympatheticomimetic effect
act on noradrenaline receptors (SNS)
OR
inhibit parasympathetic action at ACh receptors
» dry mouth
if salivary output falls to < __% of normal flow the patient will experience xerostomia
if salivary output falls to < 50% of normal flow the patient will experience xerostomia
what are the effects of salivary gland dysfunction (4)
low lubrication
low natural oral hygiene - poor pH control
accumulation of plaque - rampant dental caries, gingivitis and periodontal disease
opportunistic infections - esp. fungal infections e.g. oral thrush
what % of salivary gland neoplasms occur in the:
a) parotid gland
b) submandibular gland
c) sublingual and minor salivary glands
a) parotid gland: 80%
b) submandibular gland: 15%
c) sublingual and minor salivary glands: 5%
what % of salivary gland tumours are benign
nearly 80% of salivary gland tumours are benign
malignant salivary gland tumours are rare
6% of all head and neck malignancies
< 0.5% of all cancers
what % of salivary gland tumours are malignant in the:
a) parotid gland
b) submandibular gland
c) sublingual and minor salivary glands
a) parotid gland: 20%
b) submandibular gland: nearly 50%
c) sublingual and minor salivary glands: > 60%
what are risk factors for salivary gland cancers (5)
exposure to radiation
low nutrition diet
history of childhood benign salivary gland tumours
infection
genetics
what characteristics of salivary gland cancers makes them difficult to diagnose
very heterogenous i.e. varied
clinically diverse
complex histology
histological sections of salivary gland cancers
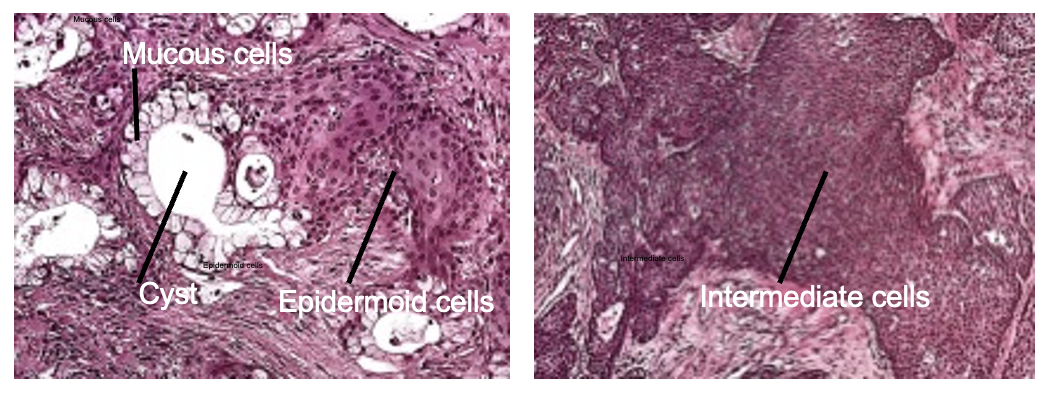
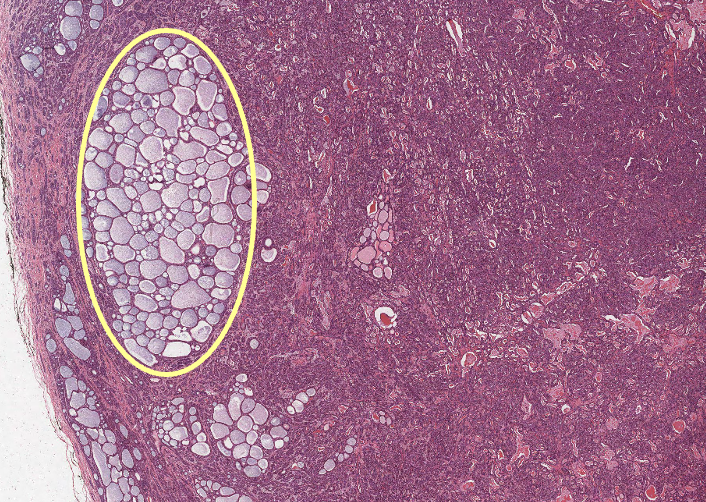
what does the yellow circle indicate
cyst
what is a fusion gene
fusion gene: a part of two genes that inappropriately join together to create a new gene
relevancy of fusion genes to salivary gland cancers
some benign and malignant tumours have the same fusion gene - abnormal
fusion genes are expressed in 34-81% of salivary gland mucoepidermoid carcinomas (MEC) - most common malignant salivary gland tumour
not all cells in a tumour will express the fusion gene associated with it
fusion genes are associated with better survival rates in some studies
outline adenoid cystic carcinoma (ACC)
relatively rare but life threatening cancer that occurs mainly in salivary glands
can also occur in the breast, lacrimal gland, lung, vulva, skin
outline characteristics of salivary gland adenoid cystic carcinoma (SGACC)
slow growing
commonly grows down nerves
absence of regional metastasis