Path Sciences 2 - Microbiology stolen
1/373
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
374 Terms
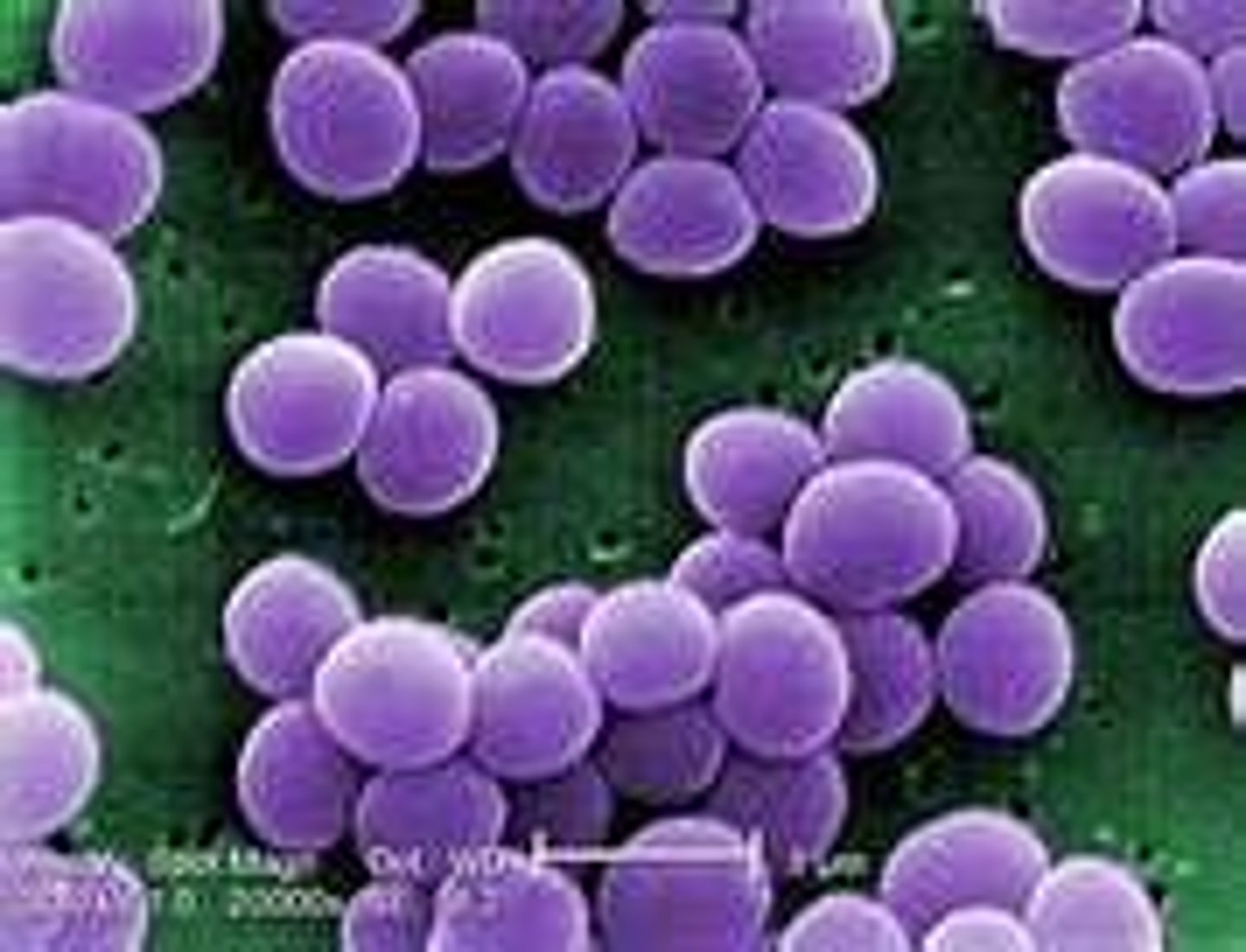
what are staphylococci?
Gram positive bacteria which form cocci arranged in grapelike clusters. There are 45 species, with S.aureus being the most recognised.
which cell wall has a thicker peptidoglycan layer?
gram positive
when observing a gram positive organism under the microscope, what colour would you expect the organism to be?
purple
do staphylococci possess the catalase enzyme?
yes
how many genera colonise humans?
16
what shape do gram positive cocci have?
spherical
do gram positive bacteria have endospores?
no
how can catalase differentiate between gram positive and gram negative bacteria?
-catalase positive organisms fit in the staphylococci and micrococci groups
-catalase negative organisms sit within the streptococcus and enterococcus groups
-anaerobic gram positive cocci tend to be catalase negative as well
what are virulence factors?
properties of the pathogen that allow it to successfully invade and cause disease in a host
how can you differentiate between staphylococci and streptococci?
staphylococci are catalase positive
streptococci are catalase negative
how big are staphylococci bacteria?
0.5-1 um in diameter
are staphylococci motile?
no they are non-motile
what does facultatively anaerobic mean?
they can grow in the presence or absence of oxygen
what does halotolerant mean?
bacteria that can stand up to 10% salt content (NaCl)
what is the temperature range for staphylococci?
18-40°C
do staphylococci require simple or complex media to grow?
simple
how many species of staphylococcus are there?
32 (16 found on humans)
where in humans is staphylococcus found?
skin and mucous membranes
what is the most virulent staphylococcus bacteria?
S. aureus - it is the only species to produce enzyme coagulase
what colour are staphylococcus aureus bacteria?
golden - produce carotenoid pigments which can also act as a virulence factor
what colour are staphylococci bacteria in general?
whitish colour
what percentage of people carry S. aureus in nasal passages?
15%
why can staphylococcus infection be so prolific?
it can survive well in the environment and is easily spread from person to person
what are the virulence factors for staphylococcus aureus?
structural components, toxins, enzymes
what are the structural components of staph. aureus?
-capsule: loose fitting slime layer
-only seen occasionally in vitro
-inhibits: chemotaxis, phagocytosis
-facilitates adherence
-peptidoglycan layer
-teichoic acids aid attachment to host via fibronectin receptors
what is chemotaxis?
movement of an organism in response to a chemical stimulus
what are other structural components of staph aureus?
protein A:
coats surface, binds Fc receptor of IgG1,2 and 4.
extracellular protein A:
binds antibodies and forms immune complexes.
bound coagulase- clumping factor, binds fibrinogen and converts to fibrin.
cytoplasmic membrane:
-transport and anchorage
what are the staphylococcal toxins?
cytolytic:
membrane damaging toxins.
alpha, beta, delta, gamma and leukocidin. toxic for many cells:
leukocytes
erythrocytes
macrophages
platelets
fibroblasts
what is the exfoliative toxin?
exfoliatin, epidermolytic toxin. causes staphylococcal scalded skin syndrome. characterised by exfoliative dermatitis. two distinct forms, A and B, either can produce disease. both are associated with peeling blister skin formation. seen mostly in young children
what is toxic shock syndrome?
toxic shock syndrome toxin 1 (TSST1). fever, hypotension, rash, desquamation, multi organ system involvement. usually associated with female patients and tampons due to their absorbance. toxin secreted during growth of staph aureus. super antigen so immune system works against body and produces cytokines, secondary mediators, hypotension and rash, heart rate increase.
what is staphylococcal food poisoning?
intoxication rather than infection. most commonly infected foods are:
processed meats
salted pork
custard filled pastries
potato salad
ice cream
contamination by human carrier
toxin is heat stable
what are the symptoms of staphylococcal food poisoning?
rapid onset- about four hours
rapid course- <24 hours
severe:
vomiting
diarrhoea
abdo pain
nausea
treatment is relief of symptoms, rehydration, not antibiotics
what are bacteriaemia and endocarditis?
staph aureus is a common cause of bacteraemia so becomes a systemic infection. up to one third of patients have unknown focus of infection. common foci are:
skin infections
post operative
catheter related
causative agent in approx 15% septicaemias
what is pneumonia?
infection of the lungs. either after aspiration of oral secretions, or from blood spread
patients at risk:
cystic fibrosis
chronic obstructive disease
very young and very old
osteomyelitis. caused by haematogenous spread. secondary infection after trauma. spread from surrounding area
what is septic arthritis?
symptoms of localised pain over involved bone, high fever. s aureus is primary cause of septic arthritis in young children. painful red joint, purulent aspirate. usually large joints. good prognosis
what are staphylococcal enterotoxins?
5 serologically different distinct exotoxins. A to E. resistant to hydrolysis by gastric and jejunal enzymes. heat stable, 100C for 30 mins. 30-50% strains produce enterotoxins. enterotoxin A mostly associated with disease, strong inducers of cytokine response. fluid not absorbed, diarrhoea
what is staphylococcal enzyme coagulase?
coagulase - two forms bound and free.
bound directly converts fibrinogen to fibrin and causes visible clumping. causes fibrin clot. bacteria can hide in clot or coat themselves with fibrin so immune system doesnt recognise it. no phagocytosis.
cell free coagulase reacts with a globulin plasma factor -> staphylothrombin. this catalases conversion of fibrinogen to fibrin. clot still formed to help bacteria.
why is catalase important?
catalase catalyses the conversion of toxic H2O2 to water and oxygen. 2H2O2 --> 2H2O + O2
all staphylococci produce catalase.
hyaluronidase:
breaks down hyaluronic acids in connective tissue. helps spread of bacteria through tissues. >90% strains produce this enzyme
what is fibrinolysin?
staphylokinase, dissolves fibrin clots. attacks and inactivate fibrin.
what is staphylococcal enzyme lipase?
lipase. hydrolyses lipids and ensures survival in sebaceous areas. all S.aureus and 30% CNS produce lipids.
what is staphylococcal enzyme Dnase?
enzyme that cleaves DNA either within host cell to cause damage or in other bacteria cells to overcome those other bacteria.
what are beta lactinases or penicillinases?
enzymes that make it difficult to treat infections because they break down the structure of beta lactin antibiotics
what is the epidemiology of staph aureus?
ubiquitous. spread by: shedding, direct contact, fomites. major source of hospital acquired infection. lysozyme in tears etc forms natural barrier.
what are clinical syndromes caused by S.aureus?
staphylococcal scalded skin syndrome. described by ritter in 1878. redness and inflammation around the mouth covers entire body in 2 days. large blisters follow and then desquamation. blisters contain clear fluid, no WBC or bacteria
bullous impetigo, localised form of SSS
what are skin infections caused by staph aureus?
impetigo
folliculitis
furuncles
carbuncles
abscesses
wound infections- skin colonising bacteria entering wound
cellulitis and infection of ulcers.
what is methicillin resistant S.aureus (MRSA)?
altered penicillin binding protein under control of Mec A gene.
ranges from asymptomatic colonisation to life threatening septicaemia. treatment varies according to site. needs constant vigilance and control of infection.
why is MRSA so hard to treat?
the structure of peptidoglycan has two sugar units. NAG and NAM. multiple chains of each. cross linking bridge which helps to secure the chains together. target is penicillin binding proteins (PBP) target for penicillins, beta lactam antibiotics. they sit and bind to PBPS. cross linking bridge wont recognise it so will become rickety so cell wall bursts. cell wall inhibitors. MRSA altered PBP so called PBP2. instead of penicillin binding to PBP, penicillin wont recognise PBP2 so wont bind to it, so resists.
what is coagulase negative staphylococci?
cause of opportunistic infection in susceptible individuals. capsule enables them to adhere to:
intravenous lines, catheters
cause infection in:
prosthetic joints, heart valves
what are streptococci?
Gram-positive, catalase-negative cocci in pairs or chains
Most abundant group of bacteria in oral cavity
what are the types of streptococci?
non-haemolytic, alpha haemolytic and beta haemolytic
how are streptococci arranged?
chains or pairs
what properties do streptococci have?
they are facultative anaerobes but range from strictly anaerobic to capnophilic
do streptococci have simple or complex growth requirements?
complex. require blood or serum in the medium
what does capnophilic mean?
can survive in high levels in co2
how do you grow a streptococci colony?
put it on a blood plate
--> it is catalase negative so they use the catalase in the blood plate to break down the hydrogen peroxide to water and oxygen
How are streptococci classified?
Hemolysis (α, β, γ), Lancefield Antigens (A,B,C,D,E,F), Viridans (green characteristics)
what are the haemolytic patterns?
none- gamma
incomplete haemolysis - alpha
complete haemolysis - beta
what colour is alpha haemolytic streptococci?
green due to hydrogen peroxide produced by the bacteria- this oxidises the haemoglobin. incomplete haemolysis
what causes complete haemolysis in beta haemolytic streptococci?
streptolycin
what is lancefield grouping?
A method of grouping catalase-negative, coagulase-negative bacteria based on the carbohydrate composition of bacterial antigens found on their cell walls.
which alpha haemolytic streptococci can cause infections in humans?
streptococcus pneumoniae plus others
what is the process of a coagulase test?
slide coagulase test-
for bound coagulase
(clumping factor)
glass slides divided in two sections (test and control). put distilled water on both sides. put test organism on test side. put plasma in test side and mix. if clumping then coagulase positive staph aureus
tube coagulase test- for free coagulase
three tubes labelled negative, test and positive. put diluted plasma in all three. add broth to positive and negative. incubate. clot formations positive result so virulent staph aureus strain. more useful for confirmation of test.
both can be done by a tube test.
what is streptococcus pneumoniae?
gram positive coccus: 0.5 -1.2 um in diameter. often oval or lancelate in shape. only grows on enriched media, such as blood. is catalase negative and needs catalase from blood. capsulated organisms from large mucoid colonies. non-capsulated are smaller and flat
what are some properties of streptococcus pneumoniae?
leading cause of morbidity and mortality particularly in <2 year olds. gram positive coccus. catalase negative. all colonies autolyse with age. alpha haemolytic when grown aerobically. virulent strains are covered with complex polysaccharide capsule. over 90 strains recognised by typing these polysaccharides. purified antigens used as polyvalent vaccine.
what are the cellular properties of streptococcus pneumoniae?
cell wall contains choline important for regulation of cell wall hydrolysis. choline must be present for the activity of the autolysin amidase during cell division. some teichoic acid in cell wall is exposed: called C substance, precipitates C reactive protein in the presence of calcium. regulates autolytic activity, also helps bacteria to adhere to host cells and it binds to choline binding receptors.
what are the virulence factors of streptococcus pneumoniae?
structural components. enzymes and toxins. carried asymptomatically: upper respiratory tract of 10-15% of adults as normal flora. has the ability to spread to:
lungs sinuses, middle ear, to other sites via blood.
colonisation mediated by binding to epithelial cells via a protein adhesin. a secretory IgA protease disrupts clearance from mucus.
what is pneumolysin?
a cytotoxin, binds cholesterol in the host membrane, creates pores to destroy the ciliated epithelial cells.
what is tissue destruction by pneumococcal infection caused by?
teichoic acid, peptidoglycan, pneumolysin
what is activated by virulence factors of strep pneumoniae?
classical and alternative complement pathways, producing C3a, C5a and also IL1 and TNF alpha - both pro inflammatory cytokines
what does infection of strep pneumonia cause?
inflammatory response, fever, tissue damage. production of hydrogen peroxide by bacteria causes further tissue damage. pneumococci enter a variety of cells by binding to receptors for platelet activating factor. facilitates spread through blood and CNS
what do pneumococci bind to?
choline, platelet activating factor
what are actual virulence factors for strep pneumoniae?
capsule gives protection from phagocytosis, pneumolysin suppresses oxidative burst. non-capsulated (rough) strains are avirulent
what are clinical syndromes of strep pneumoniae?
a result of spread of colonising organisms to different sites. significant cause of:
bacterial pneumonia, otitis media, sinusitis. bacteraemia septicaemia occurs in 25-30% of pneumonia cases, up to 80% of meningitis cases. pneumonia has rapid onset:
fever 39-41, pyrexia, localised to lower lobes. generalised bronchopneumonia . mortality rate higher with type 3
how is strep pneumoniae treated and controlled?
most are sensitive to: penicillin, erythromycin, clarithromycin, tetracycline. control by vaccine of capsular polysaccharide for 'at risk' patients.
2 effective vaccines: pneumovax- contains 23 serotypes, known to cause 90% of disease,
prevenar- contains 13 serotypes.
pneumovax now included in the childhood vaccination schedule
what are beta haemolytic streptococci?
classified by lancefield grouping system based on cell wall polysaccharides- groups A,B,C,F and G. lipoteichoic acid group D and enterococci
not all groups demonstrate beta haemolysis.
what is group F for beta haemolytic streptococci?
streptococcus milleri, sometimes does haemolysis sometimes not.
what are the properties of group A streptococcus?
colonies may appear: capsulated, non capsulated. capsule composed of hyaluronic acid is lost during the stationary phase. hyaluronic acid is found in connective tissue therefore is non immunogenic- antiphagocytic
what are the virulence factors of group A streptococcus?
M protein:
>80 types
antiphagocytic, degrades C3b
opacity factor produced by 29 M types. evades initial immune response. M like proteins bind the Fc protein of IgG and IgA and alpha2macroglobulin a protease inhibitor. F protein has a receptor for fibronectin. important for attachment to epithelial cells of:
pharynx, skin
adhesion factor in a way
what toxins do group A streptococci contain?
pyrogenic exotoxins (induce a fever): (Spe) SpeA, SpeB and SpeC. act as superantigens
what streptolysins do group A streptococci produce?
S and O
what is streptolysin S?
cell bound haemolysin, lyses erythrocytes, leukocytes and platelets. destroys phagocytes. oxygen stable, non-immunogenic
what is streptolysin O?
haemolysin activity. inactivated by oxygen irreversibly and reversibly by cholesterol but will stimulate an antibody response.
what enzymes are produced in type A streptococci?
streptokinases- A and B lyse blood clots
Dnase- depolymerises cell free DNA in purulent material.
C5a peptidase.
Hyaluronidase 'spreading factor'
diphosphopyridine nucleotidase
what is the anti streptolysin O test?
identify serum concentration of anti streptolysin. see if patient has a current or past infection
what are clinical conditions associated with group A strep?
suppurative and non suppurative (pus forming)
what is the presentation of pharyngitis?
sore throat, grey white exudate on tonsils, fever, headache, malaise, abdominal pain. 2-4 days after exposure. complications are scarlet fever. lysogenised with a temperate bacteriophage. stimulates production of pyrogenic exotoxin.
what are the skin infections caused by group A strep?
soft tissue infections: erysypelas, skin rash to face or legs, preceded by respiratory tract or skin infections. cellulitis, involves deeper tissue. infected wounds, ulcers, insect bites etc. pyoderma, impetigo
what is necrotising fasciitis?
infection becomes established in the fascial tissue below the skin, spreads rapidly causing tissue necrosis. Spe A and B involved. follows entry of bacteria to skin or wounds, cellulitis, high mortality, not a new disease
treatment for NF involves surgical removal of dead tissue and antibiotic therapy.
what are treatments of toxic shock syndrome?
streptococci toxic shock syndrome. may follow throat and soft tissue infections. severe multi organ symptoms. Spe A,B and C implicated.
soft tissue inflammation at the site of infection with non-specific symptoms: fever, chills, nausea etc. increased pain as disease progresses to multi-organ failure and shock. bacteriaemic and often have necrotising fasciitis. predisposing factors HIV, cancer, diabetics, alcohol and drug abuse
what are examples of non-suppurative diseases?
often a complication of initial streptococcal infection. rheumatic fever- associated with pharyngeal infection, 2-5 weeks after initial infection. inflammation involves heart valves, joints and blood vessels. can cause chronic damage to heart valves. caused by specific M groups- antibodies formed to cell wall antigens cross react with the sarcolemma of the heart.
rheumatic heart disease- repeated attacks with different M types can lead to hear valve disease
what is diagnosis and treatment of a group A strep condition?
gram stain and growth characteristics. lancefield grouping. sensitive to bacitracin. treatment - sensitive to penicillin. prompt treatment prevents rheumatic fever. does not influence progression to glomerulonephritis. prophylaxis necessary in some cases. beta haemolysis will be gram positive
what are group B streptococci S.agalactiae?
grow as buttery appearing colonies on nutritionally enriched medium. small zone of beta haemolysis. group specific polysaccharide cell wall antigen. nine serotypes. produce several enzymes, Dnases, hyaluronidase, neuraminidase, proteases, hippurase, haemolysins. useful for identification rather than pathogenesis. colonisers of lower gastrointestinal and genitourinary tract.
what do group B streptococci cause?
neonatal disease, urinary tract infection, wound infections etc, occasionally bacteraemia, 29.5% of reported neonatal bacterial meningitis.
what are the risk factors of group B streptococci?
heavily colonised mother lacking specific antibody. premature rupture of membranes. pre-term delivery. prolonged labour and obstetric complications.
<5% mortality. 15-30% of those with meningitis have neurological sequelae
what serotype is meningitis caused by?
type 111 but all serotypes
what do group C and G streptococci cause?
S.equilisimilis and S.angionosus associated with human disease. cause pharyngitis, found in wound infections. S.anginosus also has polysaccharide antigens for group G. group G: part of normal flora, can cause wound and throat infections. cases of bacteraemia reported for both C and G
what are group F streptococci?
milleri group. caramel smell and colour. growth conditions: CO2, minute colonies on blood agar. normal flora of vaginal area. involved in deep infections, eg abscesses
what are group D streptococci?
18 species. most common: E.faecalis, E.faecium. E.faecalis responsible for 80-90% human infections. E.faecium 10-15%
part of normal flora of bowel. facultatively anaerobic cocci- growing optimally at 35C. range 10-45C
grow as non haemolytic colonies - tolerate 6.5% salt and 40% bile salts
what are enterococci and their virulence factors?
few virulence factors but can cause life threatening disease.
virulence factors include:
-aggregation substance, carbohydrate adhesins, bacteriocin, gelatinase.
most important is antibiotic resistance:
-aminoglycosides, beta-lactams, vancomycin (mediated by VanA, VanB and VanC genes)
what are bacillus and clostridia?
two clinically important genera of spore forming bacteria (gram positive) from family Bacillaeae