2.6 Resp general pathology (INCOMPLETE)
1/19
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
20 Terms
How are alveolar macrophages distributed in the lung?
Normally 1 sentinel macrophage per alveolus
At what age is partial atelectasis in the lungs normal?
Up to 24-48h
Parts of lung have not expanded
Was this animal stillborn or did it die shortly after birth?
Stillborn = total primary atelectasis
lung has no air
3 compression causes of secondary atelectasis
Pmeumothorax/hydrothorax
Prolonged recumbency or abdominal distension (large animals) → presses on diaphragm
Pulmonary/mediastinal mass → presses on lungs
Why are cattle especially prone to secondary atelectasis caused by obstructions?
Fibrous septae between lung lobules → lack of communication between lobes
Therefore if one lobe blocked = no air goes into it
3 types of emphysema
Alveolar (e.g. emphysema = alveolar destruction, RAO in horses)
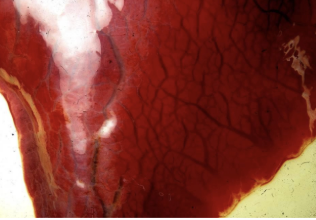
Interstitial (e.g. cattle pneumonia = air forced into interstitium)
Compensatory (emphysema adjacent to area of consolidation)
Emphysema definition
Excess air in lungs
Most common cause and 2 pathological findings of this
Alveolar emphysema
Neutrophils secrete elastase → alveolar wall destruction
Lung feels like bubble wrap
Alveoli rupture and merge together
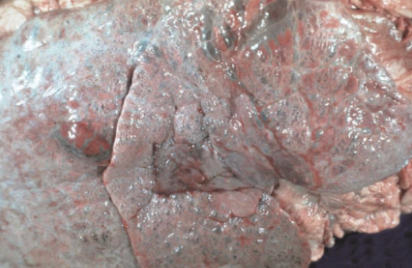
If severe emphysema (in general) = lungs do not deflate when thoracic cavity opens
Imprints of ribs present on pleural surfaces
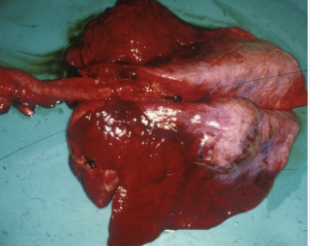
Aspiration pneumonia
Cranioventral lung lobes are hyperaemic = gravity
Why may previously healthy animals exhibit post mortem pulmonary congestion?
Effect of barbiturate euthanasia
Why is pulmonary oedema often hard to remove?
Mixes with surfactant → foams up like detergent
3 factors resisting pulmonary oedema
Tight junctions between alveolar + capillary endothelium
Intra-alveolar pressure > interstitial pressure
Interstitial lymphatic drainage removes fluid escaping from blood
4 causes of oedema
Damage to endothelium/epithelium (inflammation, toxins)
Cardiogenic (pressure overload)
Neurogenic (pressure overload → excess sympathetic drive)
Volume overload (excess fluids, renal failure)
Thrombosis
Obstruction of vessels by coagulated blood components during life within the body
Not outside body =
5 predisposing factors for pulmonary thrombosis/embolism/infarction
DIC
Liver abscess (esp cows)
Valvular endocarditis
Lung lobe torsion → abrupt infarction
(Jugular thrombosis from catheterisation)
6 morphological subtypes of rhinitis/sinusitis
Serous
Catarrhal (mucoid)
Purulent
Necrotising
Ulcerative
Haemorrhagic
5 subtypes of bronchopneumonia
Purulent bronchopneumonia (cranioventral)
Fibrinous bronchopneumonia (cranioventral)
Interstitial pneumonia (diffuse)
Embolic pneumonia (diffuse, multifocal)
Granulomatous pneumonia (diffuse, multifocal)
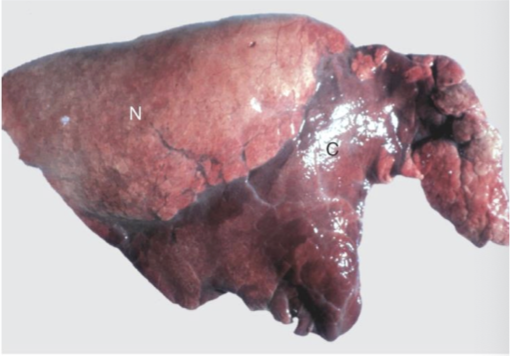
Bronchopneumonia = cranioventral consolidated tissue
3 sequelae in bronchopneumonia
Resolution
Mild inflammation = 7 days
Return to normal = 3 weeks
Deterioriation
Abscess formation (if pyogenic)
Pleuritis (severe fibrinous pneumonia) → adhering visceral/parietal pleura
Fulminating cases → hypoxaemia, toxaemia, death
Persistence
Becomes chronic with fibrosis and bronchiectasis
Describe the mechanism of bronchiectasis.