PSYC 3082 Exam 2
0.0(0)
Card Sorting
1/117
Earn XP
Description and Tags
Last updated 6:51 PM on 11/9/22
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
118 Terms
1
New cards
How is it similar to other anxiety disorders with regard to criteria?
Requires exposure to an event resulting in extreme fear, helplessness, or horror
2
New cards
Symptoms of PTSD:
- Chronic worry
- inability to sleep
- exaggerated startle response
- hyper arousal
- hyper vigilance
- inability to sleep
- exaggerated startle response
- hyper arousal
- hyper vigilance
3
New cards
Criteria of PTSD:
• Criteria A: Requires exposure to an event resulting in extreme fear, helplessness, or horror (during the event and after)
• Criteria B: Person continues to re-experience the event (e.g.: intrusive memories, nightmares, night terrors, flashbacks)
• Criteria C: Avoidance of cues that serve as reminders of the traumatic event
• Criteria D: Emotional numbing and interpersonal problems are common. Anger, depression, detachment, etc...
• Criteria E: Physiological hyperarousal
• Criteria B: Person continues to re-experience the event (e.g.: intrusive memories, nightmares, night terrors, flashbacks)
• Criteria C: Avoidance of cues that serve as reminders of the traumatic event
• Criteria D: Emotional numbing and interpersonal problems are common. Anger, depression, detachment, etc...
• Criteria E: Physiological hyperarousal
4
New cards
Subtypes of PTSD:
• Acute PTSD: Diagnosed 1-3 months post-trauma
• Chronic PTSD: Diagnosed after 3 months post-trauma
• Delayed onset PTSD: Onset of symptoms 6 months or more post-trauma
• Chronic PTSD: Diagnosed after 3 months post-trauma
• Delayed onset PTSD: Onset of symptoms 6 months or more post-trauma
5
New cards
Treatment for PTSD:
• Cognitive-Behavior Therapies (highly effective): Prolonged Exposure, Cognitive Processing Therapy, EMDR
• Anxiety Medications
• Treatments/therapies also effect brain chemistry
• Anxiety Medications
• Treatments/therapies also effect brain chemistry
6
New cards
Causes of PTSD:
- Intensity of the trauma and one's reaction to it (i.e., true trauma)
- Uncontrollability and unpredictability
- Extent of social support, or lack thereof post-trauma
- Direct conditioning and observational learning
- Uncontrollability and unpredictability
- Extent of social support, or lack thereof post-trauma
- Direct conditioning and observational learning
7
New cards
Duration of symptoms is 1 to 3 months of post-trauma
Acute PTSD
8
New cards
Duration of post-trauma symptoms is more than 3 months
Chronic PTSD
9
New cards
Onset of symptoms 6 months or more post-trauma
Delayed onset PTSD
10
New cards
Most effective treatment/therapy for PTSD is:
effective brain chemistry
11
New cards
• Diagnosed immediately after trauma (0-1 month)
• Same symptoms as PTSD
• Symptoms go into remission on their own after several months
• Similar disorder to PTSD
• Same symptoms as PTSD
• Symptoms go into remission on their own after several months
• Similar disorder to PTSD
Acute Stress Disorder
12
New cards
Contributing Factors to Development of PTSD:
• Intensity of trauma
• Uncontrollability and unpredictability
• Extent of social support (or lack thereof)
• Direct conditioning and observational learning
• Uncontrollability and unpredictability
• Extent of social support (or lack thereof)
• Direct conditioning and observational learning
13
New cards
Intrusive and nonsensical thoughts, images, or urges that one tries to resist or eliminate; irrational and unwanted
Obsessions
14
New cards
Thoughts or actions to suppress the thoughts and provide relief
Compulsions
15
New cards
Anxiety disorder involving unwanted, persistent, intrusive thoughts and impulses, as well as repetitive actions intended to suppress them
Obsessive Compulsive Disorder (OCD)
16
New cards
Causes of OCD:
- Parallel the other anxiety disorders
- Early life experiences and learning that some thoughts are dangerous/unacceptable
- Thought-action fusion - Tendency to view the thought as similar to the action
- Early life experiences and learning that some thoughts are dangerous/unacceptable
- Thought-action fusion - Tendency to view the thought as similar to the action
17
New cards
Medical Treatment for OCD:
- Clomipramine
- Luvox
- Other SSRIs
- Psychosurgery (cingulotomy) is used in extreme cases
- Luvox
- Other SSRIs
- Psychosurgery (cingulotomy) is used in extreme cases
18
New cards
Pyschological Treatment for OCD:
• Cognitive-Behavior Therapy (exposure & response prevention
• Combining medication with CBT does not work as well as CBT alone
• Combining medication with CBT does not work as well as CBT alone
19
New cards
related to one's body or the perceptions of one's body or health, and there is noidentifiable medical condition causing the physical complaints
Somatization Disorder
20
New cards
meaning body
soma
21
New cards
• Strong disease conviction - convinced they have a disease (not concerned about develop
ing a disease)
• Severe anxiety (worry) focused on the possibility of having or developing a serious disease
• Medical reassurance does not help
ing a disease)
• Severe anxiety (worry) focused on the possibility of having or developing a serious disease
• Medical reassurance does not help
Hypochondriasis
22
New cards
Cause of Hypochondrias:
• Cognitive perceptual distortions - misinterpret bodily sensations of minor illness as threatening
• Family history of illness (People in family have developed serious illness before)
• Family history of illness (People in family have developed serious illness before)
23
New cards
Treatment for Hypochondrias:
- Challenge illness-related misinterpretations
- Provide more substantial and sensitive reassurance
- Treat anxiety (Stress management and coping strategies)
- Provide more substantial and sensitive reassurance
- Treat anxiety (Stress management and coping strategies)
24
New cards
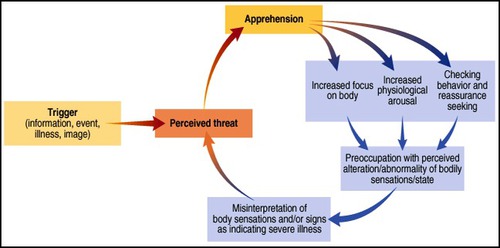
Integrative model of causes of hypochondriasis:
25
New cards
disorder involving extreme and long-lasting focus on multiple physical symptoms for which no medical cause is evident
Somatoform Disorder
26
New cards
Clinical Description for Somatization Disorder:
- Extended history of physical complains before age 30
- Concerned over the symptoms themselves, not what they might mean, as in the case with hypochondriasis
- Symptoms become the person's identity
- Numerous visits to physicians
- Substantial impairment in social or occupational functioning
- Concerned over the symptoms themselves, not what they might mean, as in the case with hypochondriasis
- Symptoms become the person's identity
- Numerous visits to physicians
- Substantial impairment in social or occupational functioning
27
New cards
Causes of Somatization Disorder:
• Familial history of illness
• Weak behavioral inhibition system
• Weak behavioral inhibition system
28
New cards
Treatment for Somatization Disorder:
- Stress management; pain management techniques
- Reduce the tendency to visit numerous medical specialists
- Assign "gatekeeper" physician
- Reduce supportive positive consequences of talk about physical symptoms
remove secondary gain (babying, staying home, sick leave, attention)
- Reduce the tendency to visit numerous medical specialists
- Assign "gatekeeper" physician
- Reduce supportive positive consequences of talk about physical symptoms
remove secondary gain (babying, staying home, sick leave, attention)
29
New cards
Physical malfunctioning, such as blindness or paralysis, suggesting neurological impairment but with no organic pathology to account for it. (Occurs more in females, triggered by a severe stressor such as loosing a loved one)
Conversion Disorder
30
New cards
Clinical Description of Conversion Disorder:
• Physical malfunctioning without any physical or organic pathology
• Malfunctioning often involves motor-sensory areas(sometimes involuntary)
• Person shows "la belle indifference" - little concern for their loss of functioning
• KEY: Unable to find physical cause
• Malfunctioning often involves motor-sensory areas(sometimes involuntary)
• Person shows "la belle indifference" - little concern for their loss of functioning
• KEY: Unable to find physical cause
31
New cards
Causes of Conversion Disorder:
- Freudian psychodynamic view: unconscious represses this trauma
- Emphasis on the role of trauma, conversion, and primary/secondary gain
- Detachment from the trauma and negative reinforcement seem critical
- Emphasis on the role of trauma, conversion, and primary/secondary gain
- Detachment from the trauma and negative reinforcement seem critical
32
New cards
Treatment for Conversion Disorder:
• Difficult to treat
• Attend to trauma
• Remove sources of secondary gain
• Reduce supportive consequences of talk about physical symptoms
• Attend to trauma
• Remove sources of secondary gain
• Reduce supportive consequences of talk about physical symptoms
33
New cards
Disorder in which as many as 100 personalities or fragments of personalities coexist within one body and mind.
Dissociative Identity Disorder
34
New cards
Clinical Description of Dissociative Identity Disorder:
- Involves adoption of several new identities- a different personality, name, eating habits, style of dress, sexual orientation, likes/dislikes, different gender
- Identities display unique sets of behaviors, voice, and posture
- Defining feature is dissociation of certain aspects of personality
- Identities display unique sets of behaviors, voice, and posture
- Defining feature is dissociation of certain aspects of personality
35
New cards
Unique Aspects of DID:
- Alters
- Host
- Switch
- Host
- Switch
36
New cards
Refers to the different identities or personalities in DID
Alters
37
New cards
The identity that seeks treatment and tries to keep identity fragments together
Host
38
New cards
Often instantaneous transition from one personality to another
Switch
39
New cards
Causes of Dissociative Identity Disorder:
• History of horrible unspeakable child abuse
• Evolves as a coping mechanism
• Evolves as a coping mechanism
40
New cards
Treatment for Dissociative Identity Disorder:
• Focus on reintegration of identities
• Aim is to identify and neutralize cues/triggers that provoke memories of trauma/dissociation
• Aim is to identify and neutralize cues/triggers that provoke memories of trauma/dissociation
41
New cards
Average age of onset for Major Depression:
25 years old
42
New cards
Average length of Major Depressive episode if left untreated is about:
9 months
43
New cards
Up to _______ will experience an episode of Major Depressive Disorder.
1 in 5
44
New cards
About _______ of the adult population will experience Major Depressive Disorder.
5-7%
45
New cards
________people who experience a single episode of major depressive disorder go on to experience a recurrent episode
80%
46
New cards
group of disorders involving severe and enduring disturbances in emotionality ranging from elation to severe depression
Mood disorders
47
New cards
Loss of pleasure/interest in usual activities
Anhedonia
48
New cards
Defining Features of Major Depression:
• Must experience major depressive episode: extremely depressed mood state lasting at least two weeks
• Must have 6 of 8 additional symptoms:
o Cognitive Symptoms
• Excessive crying/feelings of wanting to cry, difficulty concentrating and forgetfulness, changes from previous functions, difficulty making decisions, emotions, thoughts of death, dying, or suicide
o Vegetative or somatic symptoms
• Eating patterns: significant increase or decrease in appetite
• Changes in sleep patterns: mainly insomnia or hyper insomnia
o Anhedonia - loss of pleasure/interest in usual activities
• Loss of energy or excessive lethargy; decreased motivation
• Must have 6 of 8 additional symptoms:
o Cognitive Symptoms
• Excessive crying/feelings of wanting to cry, difficulty concentrating and forgetfulness, changes from previous functions, difficulty making decisions, emotions, thoughts of death, dying, or suicide
o Vegetative or somatic symptoms
• Eating patterns: significant increase or decrease in appetite
• Changes in sleep patterns: mainly insomnia or hyper insomnia
o Anhedonia - loss of pleasure/interest in usual activities
• Loss of energy or excessive lethargy; decreased motivation
49
New cards
Etiology of Depression:
• Neurobiological Influences
o Low serotonin levels
o Elevated cortisol levels
• Stressful Life Events
o Low serotonin levels
o Elevated cortisol levels
• Stressful Life Events
50
New cards
Relates to a perceived lack of control over negative life events; perception that one doesn't have control over these events and therefor they are depressive; leads to a depressive attributional style: internal, stable, global negative attribution
Learned Helplessness
51
New cards
negative outcomes are one's own fault
Internal attributions
52
New cards
belief or perception that future negative events will continue to be one's own fault
Stable attributions
53
New cards
belief that negative events will disrupt many life activities
Global attributions
54
New cards
Treatment for Major Depression:
• SSRIs
• Therapy
• Therapy
55
New cards
Alternations between full manic episodes and depressive episodes
Bipolar I Disorder
56
New cards
Defining Features of Bipolar I Disorder
• Alternations between full manic episodes and depressive episodes
• Person must experience a manic episode
o Manic Episode
• High energy levels
• Euphoric, extremely positive mood
• Racing thoughts
• Easily excited
• Pressured (rapid) speech
• Spontaneous/impulsive
• May be reckless
o HAVOC on the person's life
• Person must experience a manic episode
o Manic Episode
• High energy levels
• Euphoric, extremely positive mood
• Racing thoughts
• Easily excited
• Pressured (rapid) speech
• Spontaneous/impulsive
• May be reckless
o HAVOC on the person's life
57
New cards
Alternations between major depressive episodes and hypomanic episodes; Typically able to function but causes slight problems
Bipolar II Disorder
58
New cards
similar to mania but less severe
Hypomania
59
New cards
Chronic (at least 2 years) mood disorder characterized by alternating mood elevation and depression levels that are not as severe as manic or major depressive episodes.
Cyclothymic Disorder
60
New cards
Defining features for Cyclothymic Disorder:
• Chronic low grade bipolar disorder
• Chronic, Long Lasting, Low Grade mania or hypomania with depression.
• Pattern must last for at least 2 years (1 year for children and adolescents) People should be treated for fear of developing a more severe bipolar disorder.
• Chronic, Long Lasting, Low Grade mania or hypomania with depression.
• Pattern must last for at least 2 years (1 year for children and adolescents) People should be treated for fear of developing a more severe bipolar disorder.
61
New cards
Mood disorder involving persistently depressed mood, with low self-esteem, with-drawl, pessimism, or despair, present for at least 2 years, with no absence of symptoms for more than two months
Dysthymia
62
New cards
Defining Features for Dysthymia:
• Chronic, low-grade depressed mood
• Defined by persistently depressed mood that continues for at least 2 years
• Early Onset: Before age 21 (early 20s), greater chronicity, poorer prognosis
• Late Onset: Typically in the early twenties, but AFTER 21
• Defined by persistently depressed mood that continues for at least 2 years
• Early Onset: Before age 21 (early 20s), greater chronicity, poorer prognosis
• Late Onset: Typically in the early twenties, but AFTER 21
63
New cards
Most ____________ Persons are ___________, Not All __________ Persons are ___________.
Most Depressed Persons are Anxious, Not All Anxious Persons are Depressed
64
New cards
Sleep and Circadian Rhythms:
o Hallmark of most mood disorders
o Those who are depressed enter REM sleep much faster than those who are not.
o Those who are depressed experience less deep sleep, if any.
o Those who are depressed enter REM sleep much faster than those who are not.
o Those who are depressed experience less deep sleep, if any.
65
New cards
- Type of Cognitive Error
- Overemphasize the negative
- Overemphasize the negative
Arbitrary Inference
66
New cards
- Type of Cognitive Error
- Generalize negatives to all aspects of a situation
- Generalize negatives to all aspects of a situation
Overgeneralization
67
New cards
Medication Treatments for Mood Disorders:
• Tricyclics - rarely used (very lethal); Block reuptake or norepinephrine and other neurotransmitters
• MAO Inhibitors - Block Monoamine Oxidase
• Monoamine oxidase is an enzyme that breaks down serotonin/norepinephrine
• Slightly more effective than tricyclics
• SSRIs
• Lithium - most commonly used for mania (drug of choice for bipolar disorder)
• MAO Inhibitors - Block Monoamine Oxidase
• Monoamine oxidase is an enzyme that breaks down serotonin/norepinephrine
• Slightly more effective than tricyclics
• SSRIs
• Lithium - most commonly used for mania (drug of choice for bipolar disorder)
68
New cards
• RARE and for SEVERE depression for those who are treatment resistant
• Side effects: few and include short-term memory loss
• Side effects: few and include short-term memory loss
Electroconvulsive Therapy (ECT)
69
New cards
Psychosocial Treatment for Mood Disorders:
•Cognitive Therapy
- Addresses cognitive errors in thinking
- Also includes behavioral components
• Interpersonal Psychotherapy
- Focuses on problematic interpersonal relationships
- Addresses cognitive errors in thinking
- Also includes behavioral components
• Interpersonal Psychotherapy
- Focuses on problematic interpersonal relationships
70
New cards
Eighth Leading Cause of Death in the United States
Suicide
71
New cards
What races participate in suicide the most?
Whites and Native Americans
72
New cards
Suicide rates are increasing particularly in?
Adolescents and elderly
73
New cards
________ are more successful at committing suicide than ___________.
Males are more successful at committing suicide than females
74
New cards
_________ attempt suicide more often than __________.
Females attempt suicide more often than males
75
New cards
50% of people with _____________ attempt suicide
Bipolar disorder
76
New cards
________ have been linked with suicide in adolescents
SSRIs
77
New cards
Factors that Increase the Risk for Suicide:
- Suicide in the Family
- Low Serotonin Levels
- A Psychological Disorder
- Alcohol Use and Abuse
- Past Suicidal Behavior
- Experiencing a Shameful/Humiliating Stressor
- Publicity About Suicide and Media Coverage
- Low Serotonin Levels
- A Psychological Disorder
- Alcohol Use and Abuse
- Past Suicidal Behavior
- Experiencing a Shameful/Humiliating Stressor
- Publicity About Suicide and Media Coverage
78
New cards
• Shared Biological Vulnerability
- Overactive neurobiological response to stress
• Exposure to Stress
- Stress activates hormones that affect neurotransmitter systems
- Stress turns on certain genes
- Stress affects circadian rhythms
- Stress activates dormant psychological vulnerabilities (i.e., negative thinking)
- Stress contributes to sense of uncontrollability
- Fosters a sense of helplessness and hopelessness
• Social and Interpersonal Relationships/Support are Moderators
- Overactive neurobiological response to stress
• Exposure to Stress
- Stress activates hormones that affect neurotransmitter systems
- Stress turns on certain genes
- Stress affects circadian rhythms
- Stress activates dormant psychological vulnerabilities (i.e., negative thinking)
- Stress contributes to sense of uncontrollability
- Fosters a sense of helplessness and hopelessness
• Social and Interpersonal Relationships/Support are Moderators
Integrative Theory
79
New cards
Out-of-control eating episodes, or binges, followed by self-induced vomiting, excessive use of laxatives, or other attempts to purge
Bulimia Nervosa
80
New cards
Most common subtype of bulimia (e.g., vomiting, laxatives, enemas)
Purging subtype
81
New cards
Bulimia subtype (e.g., excess exercise, fasting)
Nonpurging subtype
82
New cards
Defining Features of Bulimia Nervosa:
• Binge Eating - hallmark of bulimia
o Binge: eating excess amounts of food at one sitting
• Eating is perceived as uncontrollable
• Compensatory behaviors
o Purging - self-induced vomiting, diuretics, laxatives, enemas, etc.
o Excessive exercise (non-purging type)
• Most are within 10% of their target body weight
o Body image isn't nearly as distorted as with anorexia
o Binge: eating excess amounts of food at one sitting
• Eating is perceived as uncontrollable
• Compensatory behaviors
o Purging - self-induced vomiting, diuretics, laxatives, enemas, etc.
o Excessive exercise (non-purging type)
• Most are within 10% of their target body weight
o Body image isn't nearly as distorted as with anorexia
83
New cards
- Anorexia subtype
- Limit caloric intake via diet and fasting
- Limit caloric intake via diet and fasting
Restricting subtype
84
New cards
- Anorexia subtype
- About 50% of anorexics; Engage in binge eating and purging like bulimia, but also severely underweight and have a distorted bodily view
- About 50% of anorexics; Engage in binge eating and purging like bulimia, but also severely underweight and have a distorted bodily view
Binge-eating-purging subtype
85
New cards
Treatment for Bulimia Nervosa:
• Antidepressants can help reduce binging and purging behavior
• Cognitive-behavior therapy (CBT) is the treatment of choice; focuses on changing eating habits and changing attitudes about weight and shape
• Interpersonal psychotherapy results in long-term gains similar to CBT
• Cognitive-behavior therapy (CBT) is the treatment of choice; focuses on changing eating habits and changing attitudes about weight and shape
• Interpersonal psychotherapy results in long-term gains similar to CBT
86
New cards
Person eats nothing beyond minimal amounts of food, so body weight sometimes drops dangerously.
Anorexia Nervosa
87
New cards
Treatment for Anorexia Nervosa:
• Psychological Treatment:
o Weight restoration
o Education, behavioral, and cognitive interventions
o Often Involves Family
• Nutritional counseling, out-patient CBT (preferred one)
o Weight restoration
o Education, behavioral, and cognitive interventions
o Often Involves Family
• Nutritional counseling, out-patient CBT (preferred one)
88
New cards
Defining Features of Anorexia Nervosa:
• Severe Weight Loss (15% or more below expected weight)
• Intense Fear of Obesity and losing control over eating
• Show relentless pursuit of thinness, often beginning with dieting
• Intense Fear of Obesity and losing control over eating
• Show relentless pursuit of thinness, often beginning with dieting
89
New cards
Causes of Bulimia and Anorexia:
• Cultural imperative for thinness translates into dieting
• Standards of ideal body size change as much as clothes
• Low sense of personal control and self-confidence
• Food restriction often leads to a preoccupation with food
• In addition to sociocultural pressures, casual factors include possible biological and genetic vulnerabilities (run in families), psychological factors (low self-esteem), social anxiety (fear of rejection), and distorted body image (relatively normal weight individuals view themselves as fat and ugly).
• Standards of ideal body size change as much as clothes
• Low sense of personal control and self-confidence
• Food restriction often leads to a preoccupation with food
• In addition to sociocultural pressures, casual factors include possible biological and genetic vulnerabilities (run in families), psychological factors (low self-esteem), social anxiety (fear of rejection), and distorted body image (relatively normal weight individuals view themselves as fat and ugly).
90
New cards
Repetitive eating of inedible substances; Both occur more in people with developmental disabilities.
Pica
91
New cards
Chronic regurgitation and re-swallowing of partially digested food; Both occur more in people with developmental disabilities.
Rumination Disorder
92
New cards
Who typically suffers from Anorexia?
• Females and
• White
• From middle-to-upper middle class families
• Average intelligence
• White
• From middle-to-upper middle class families
• Average intelligence
93
New cards
Psychological dissatisfaction with biological gender, or a disturbance in the sense of identity as a male or female. The primary goal is not sexual arousal but rather to live the life of the opposite gender.
Gender Identity Disorder
94
New cards
Clinical Overview of Gender Identity Disorder:
• Person feels trapped in the body of the wrong sex
• Assume the identity of the desired sex
o Has to do with physical identity, not sexual behavior
• Assume the identity of the desired sex
o Has to do with physical identity, not sexual behavior
95
New cards
Treatment for Gender Identity Disorder:
• Sex Reassignment - 30% report satisfaction
• Involve realigning the persons psychological gender with their biological sex
• Involve realigning the persons psychological gender with their biological sex
96
New cards
Long-term recurring, intense sexually arousing urges, fantasies, or behavior involving the use of nonliving, unusual objects, which cause distress or impairment in life functioning.
Fetishism
97
New cards
Defining Features of Fetishism:
• Sexual attraction to nonliving objects
- Required to become physically aroused
• Numerous targets of fetishistic arousal, fantasy, urges, and desires
- Required to become physically aroused
• Numerous targets of fetishistic arousal, fantasy, urges, and desires
98
New cards
Sexual arousal with the act of cross-dressing
Transvestic Fetishism
99
New cards
Inflicting pain or humiliation to attain sexual gratification
• Pain not desired by other person
• May be unable to maintain an erection without causing harm to another
• Pain not desired by other person
• May be unable to maintain an erection without causing harm to another
Sexual Sadism
100
New cards
Suffer pain or humiliation to attain sexual gratification
Sexual Masochism