Comprehensive Guide to Immunology and Serology Techniques
1/183
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
184 Terms
Immunology
The study of the body's immune system and its functions and disorders.
Serology
The in-vitro study of blood serum and its components to detect antigens and antibodies.
Antigen-antibody reactions in-vitro
Reactions that occur outside a living organism, typically in a laboratory setting, involving the interaction between antigens and antibodies.
Monoclonal antibodies
Antibodies that are made by identical immune cells that are all clones of a unique parent cell.
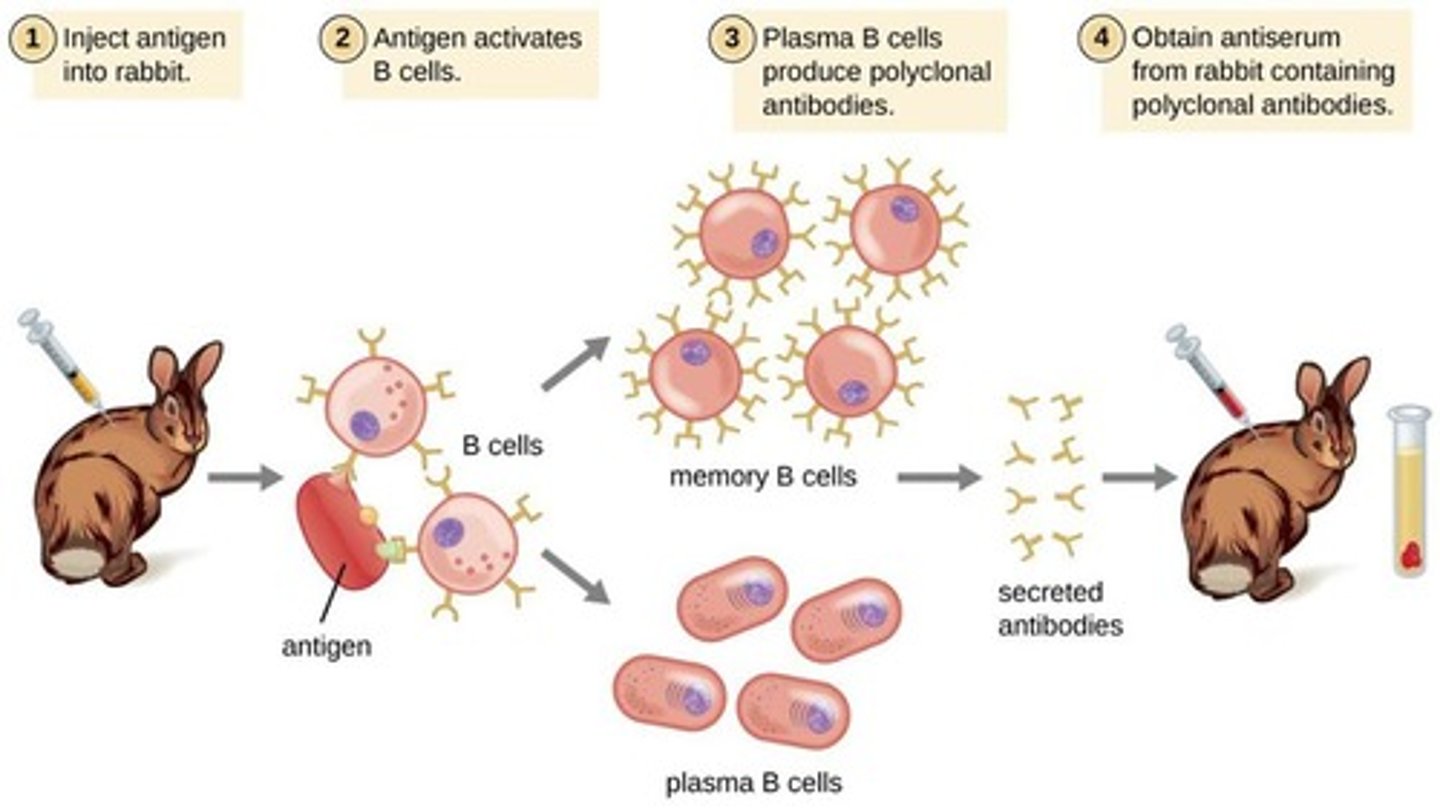
Polyclonal antibodies
Antibodies that are produced by different B cell lineages within the body.
Immunoglobulins production
The process by which antibodies are produced commercially, often involving hybridoma technology.
Precipitation
The process of combining soluble antigen with soluble antibody to produce insoluble complexes that are visible.
Agglutination
The process by which particulate antigens, such as cells, aggregate to form larger complexes when a specific antibody is present.
Serological tests
An in-vitro study of blood serum and its components to detect antigens and antibodies.
Quantitation of antigen and antibodies
The measurement of the amount of antigens and antibodies present in a patient sample.
Specific serological tests
Tests designed to diagnose specific viral and bacterial infections.
Non-specific serological tests
Tests that provide evidence for some diseases but are not definitive.
Qualitative tests
Tests that provide a yes or no answer regarding the presence of a substance.
Quantitative tests
Tests that measure how much of a substance is present in a sample.
Semi-quantitative tests
Tests that provide an estimate of the amount of a substance present, but not an exact measurement.
Detection of antibody
The process of identifying the presence of antibodies in a sample.
Detection of autoantibody
The identification of antibodies that mistakenly target and react with a person's own tissues.
Detection of offending drugs
The identification of drugs that may cause adverse reactions in patients.
Immunoassay of hormones
A test that can measure minute amounts of hormones in a sample.
Label-free immunoassays
Broadly classified as label-free immunoassays.
AG AB interaction
Based on physical change, it usually involves AG AB interaction.
Antibody
A glycoprotein produced by B lymphocytes which is capable of specifically binding antigen via an antigen binding site.
Antigen
A molecule which is capable of interacting with an antibody molecule (or T cell receptor) via the antibody molecule's antigen binding site.
Specific binding capacity
The ability of an antibody to bind specifically to its corresponding antigen.
Affinity
The strength of interaction between an antigen and an antibody.
Association
Ag + Ab forms an Ag-Ab complex.
Dissociation
The process where the antigen-antibody complex breaks apart.
Epitope binding site
The specific site on an antigen that is recognized and bound by an antibody.
Avidity
The collective affinity of multiple binding sites of an immunoglobulin.
Avidity formula
Avidity = Affinity + Valence.
Valence
The number of epitope binding sites in an antibody.
Heterogeneous mixture of antibodies
A mixture produced by different B cell clones.
Polyclonal antibodies production
Antibody responses differ from one individual to another.
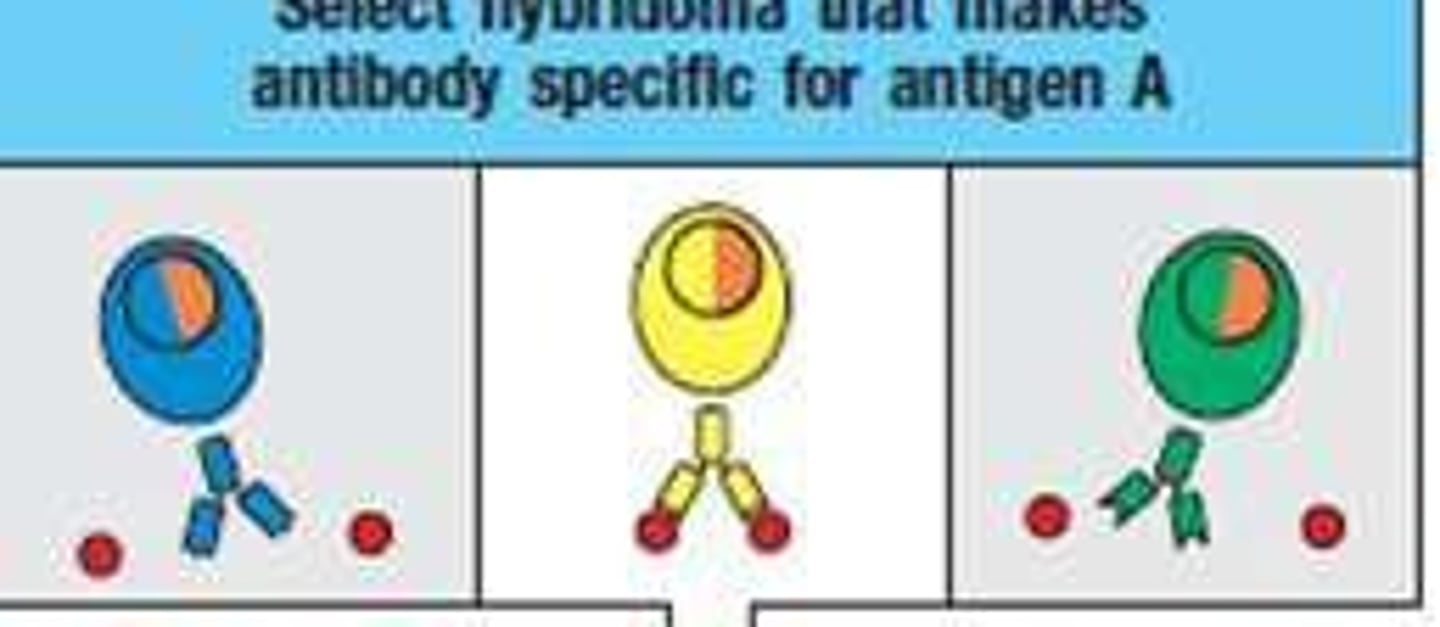
Hybridoma technology
A method used to produce monoclonal antibodies using hybridoma cells.
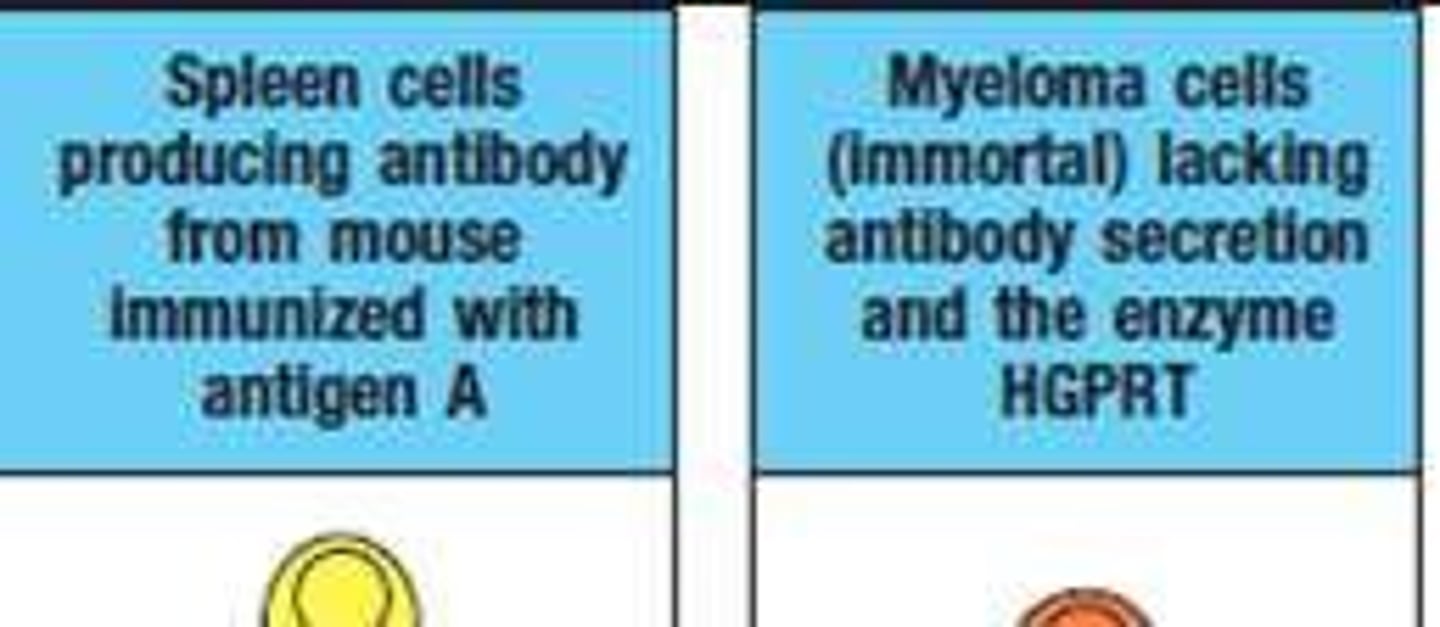
Cell Fusion
The process of fusing B cells with myeloma cells to produce hybridomas.
HAT Medium Selection
A selection medium containing Hypoxanthine, Aminopterin, and Thymidine used to select hybridomas.

HGPRT enzyme
An enzyme inherited from B cells that allows hybridomas to survive in HAT medium.
Specificity
The ability of an antibody to bind to a specific epitope, with monoclonal antibodies having high specificity and polyclonal antibodies having lower specificity.
Sensitivity
The ability of an antibody to detect its target, with polyclonal antibodies generally having higher sensitivity.
Reproducibility
The consistency of antibody production across batches, with monoclonal antibodies being highly reproducible and polyclonal antibodies showing low reproducibility.
Cost
Monoclonal antibodies are expensive, while polyclonal antibodies are more cost-effective.
Production Time
Monoclonal antibodies take longer to produce using the hybridoma method, whereas polyclonal antibodies can be produced in a shorter time through animal immunization.
IgM
An antibody that appears first after infection, detectable around 1-2 weeks, peaks quickly, and is an early marker of recent/acute infection.
IgG
An antibody that rises more slowly than IgM, detectable around 2 weeks, reaches a higher sustained level, and provides longer-term immunity.
IgA
An antibody that appears around the same time as IgM/IgG, important for mucosal immunity, and increases in levels but not as strongly sustained as IgG.
Neutralising Antibodies
Antibodies that provide functional protection by blocking the pathogen and follow a similar pattern to IgG.
Uncertainty in Antibody Response
Reflects variability between individuals in terms of antibody levels, timing, or persistence.
Polyclonal Response
The body's natural production of a variety of antibodies (IgM, IgG, IgA) from different B-cell clones after infection.
Monoclonal Antibody Use
Lab-made antibodies that mimic one specific antibody and are often used for therapy or diagnostics.
Serum
Clotted blood collected using a Serum Separator Tube, commonly used for serological testing.
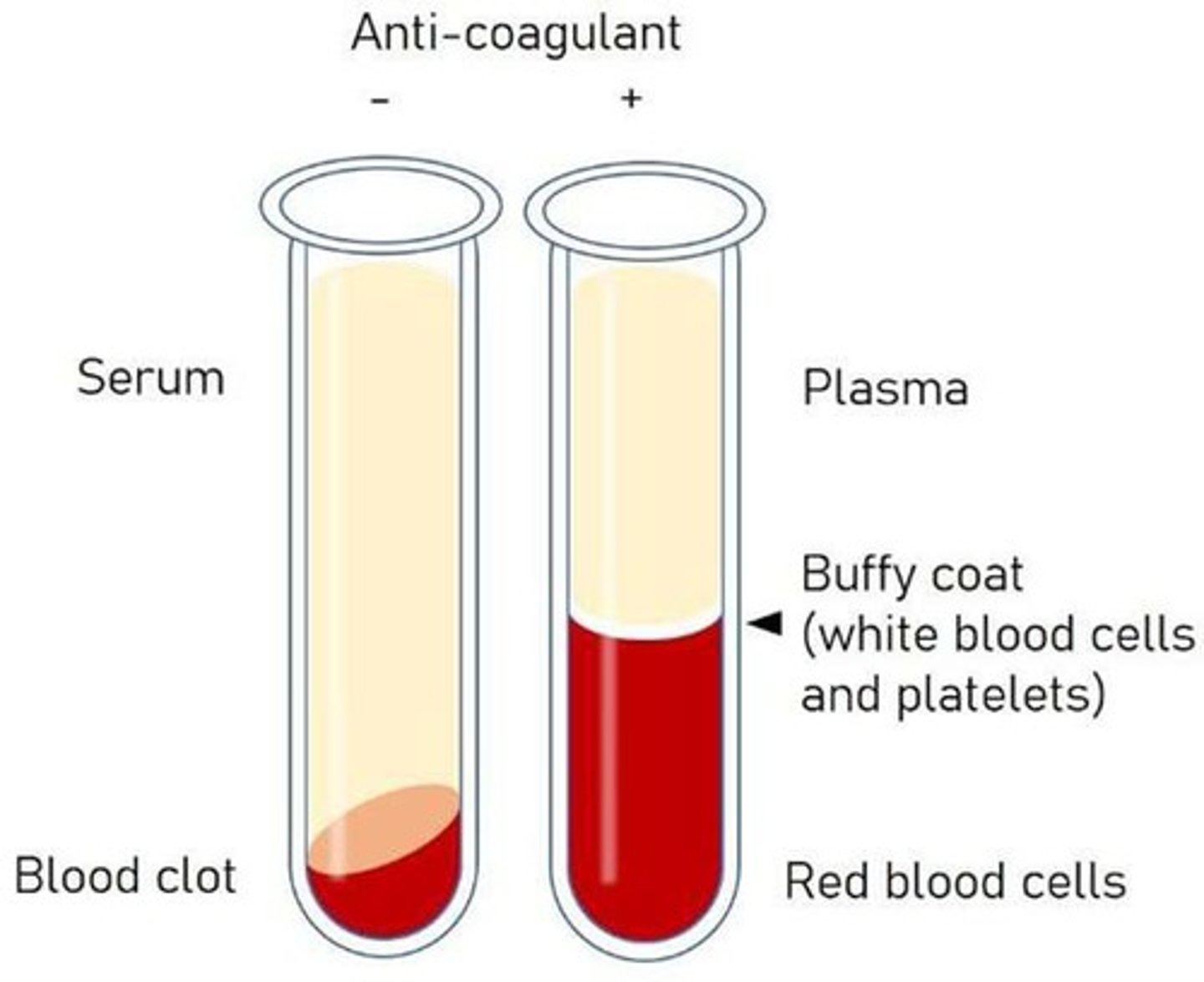
Plasma
Anticoagulated blood used for various serological tests.
Whole Blood
Blood collected with anticoagulants like EDTA or Heparin, used in flow cytometry and HLA typing.
Cerebrospinal Fluid (CSF)
Fluid collected via lumbar puncture, used for testing neurosyphilis and viral encephalitis.
Bronchoalveolar Lavage (BAL)
Fluid collected via bronchoscopy, used for testing Pneumocystis jirovecii.
Synovial Fluid
Joint fluid collected via arthrocentesis, used for testing rheumatoid factors and autoimmune markers.
Urine
Collected midstream, used for testing Bence Jones Protein and Legionella antigen.
Stool
Sample collected for testing Clostridium difficile and Rotavirus.
6 main uses of serological test
1. identification of microorganisms
2. detection of antibodies
3. detection of autoantibodies
4.detection of offending drugs
5.immunoassay of hormones (measure minute amount of hormones)
6.detection of immunologic abnormalities
Nasopharyngeal Swab
Swab collected from the nose/throat, used for testing Influenza and COVID-19 Antigen.
Dried Blood Spot (DBS)
Blood collected via heel or finger prick, used for newborn screening and HIV/Hepatitis testing.
Collection Tube
Container used to collect blood samples for testing.
EDTA (Purple)
Anticoagulant used in blood collection that prevents clotting.
Heparin (Green)
Anticoagulant used in blood collection that prevents clotting.
Citrate (Blue)
Anticoagulant used in blood collection that prevents clotting.
Type of blood collection tube used for serum collection.
Red-top, serum separator tube - SST (Gold/Tiger-top)
Clotting Factors
Proteins in blood that help control bleeding.
Processing Time
Duration required to prepare blood samples for testing.
Antibody Testing
Testing method to detect the presence of antibodies in the blood.
Complement System Testing
Testing method to evaluate the complement system's function.
Acute Serum
Serum collected from a patient with a current infection.
Convalescent Specimen
Blood sample collected during the recovery phase of an infection.
Paired Sera
Two serum samples tested together, one from acute and one from convalescent phase.
Seroconversion
The change of an antibody test from negative to positive over time.
Confirming a Recent or Active Infection
Using paired serology to detect rising IgG titers to confirm an infection.
Retrospective Diagnosis of Viral or Bacterial Infections
Using paired testing to detect past infections when recovery occurs before diagnosis.
Diagnosing Diseases That Require Seroconversion Detection
Identifying diseases by observing the change in antibody presence over time.
Confirming Immunity or Vaccine Response
Measuring antibody development after vaccination or post-infection.
what is the acute sample, convalescent sample and diagnosis for dengue Fever
acute sample: high IgM/ low IgG
convalescent sample: low IgM/ high IgG (4x increase)
diagnosis: recent infection
COVID-19 IgG Serology
Example of retrospective diagnosis using paired testing.
Hepatitis A, B, C Serology
Examples of diseases that may require seroconversion detection.
Hepatitis B (Anti-HBs IgG response)
Example of confirming immunity post-vaccination.
Measles, Mumps, Rubella (MMR vaccine response)
Example of confirming vaccine response.
Varicella-Zoster Virus (Chickenpox Immunity Testing)
Example of testing for immunity against chickenpox.
The Early Phase of infection will use what sample of patients serum?
acute serum
when should convalescent specimens be followed up?
2-4 Weeks Later
Criteria for diagnosis of Primary Infection
4-fold or more increase in titre of IgG or total antibody between acute and convalescent
IgM present
Recent infection
Presence of IgM
Typhoid (Widal Test)
4× rise in titers
what is the acute sample, convalescent sample and diagnosis for Typhoid Fever
acute: Low O & H agglutinin titers
convalescent: 4x rise in tires
diagnosis: typhoid fever
name 2 Criteria's for reinfection
4-fold or more increase in IgG antibody or total
IgM absecent/ slight increase
what is the acute sample, convalescent sample and diagnosis for Syphilis (RPR/VDRL)
acute sample: Low titer
convalescent sample: 4x increase/ decrease (post-treatment)
diagnosis: active or resolving infection
Presence of IgM
Similar to reinfection
7 examples of UNLABELLED IMMUNOASSAYS
Examples include Precipitation, Agglutination, Complement fixation, Neutralisation, Antibody dependent cell mediated cytotoxicity (ADCC), Opsonisation
Formation of an antigen-antibody lattice
Depends on the valence of both the antibody and antigen.
Bivalent antibody
A precipitate will not form with monovalent Fab fragments.
Zone of Equivalence
The optimal ratio of antigen and antibody affects the amount of precipitation.
Zone of antibody excess
Initially, there is not enough antigen to produce visible lattice formation.
Equivalence zone
Where both the optimal antigen-antibody interaction and maximal precipitation occur.
Zone of antigen excess
If even more antigen were added, the amount of precipitation would decline.
Prozone Effect (Antibody Excess Zone)
A phenomenon in which visible agglutination or precipitation does not occur in mixtures of specific antigen and antibody because of antibody excess.