Lecture 26: Adenoviruses and Papillomaviruses
1/64
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
65 Terms
What is the structure of adenovirus?
non-enveloped, icosahedral capsid containing dsDNA linear genomes
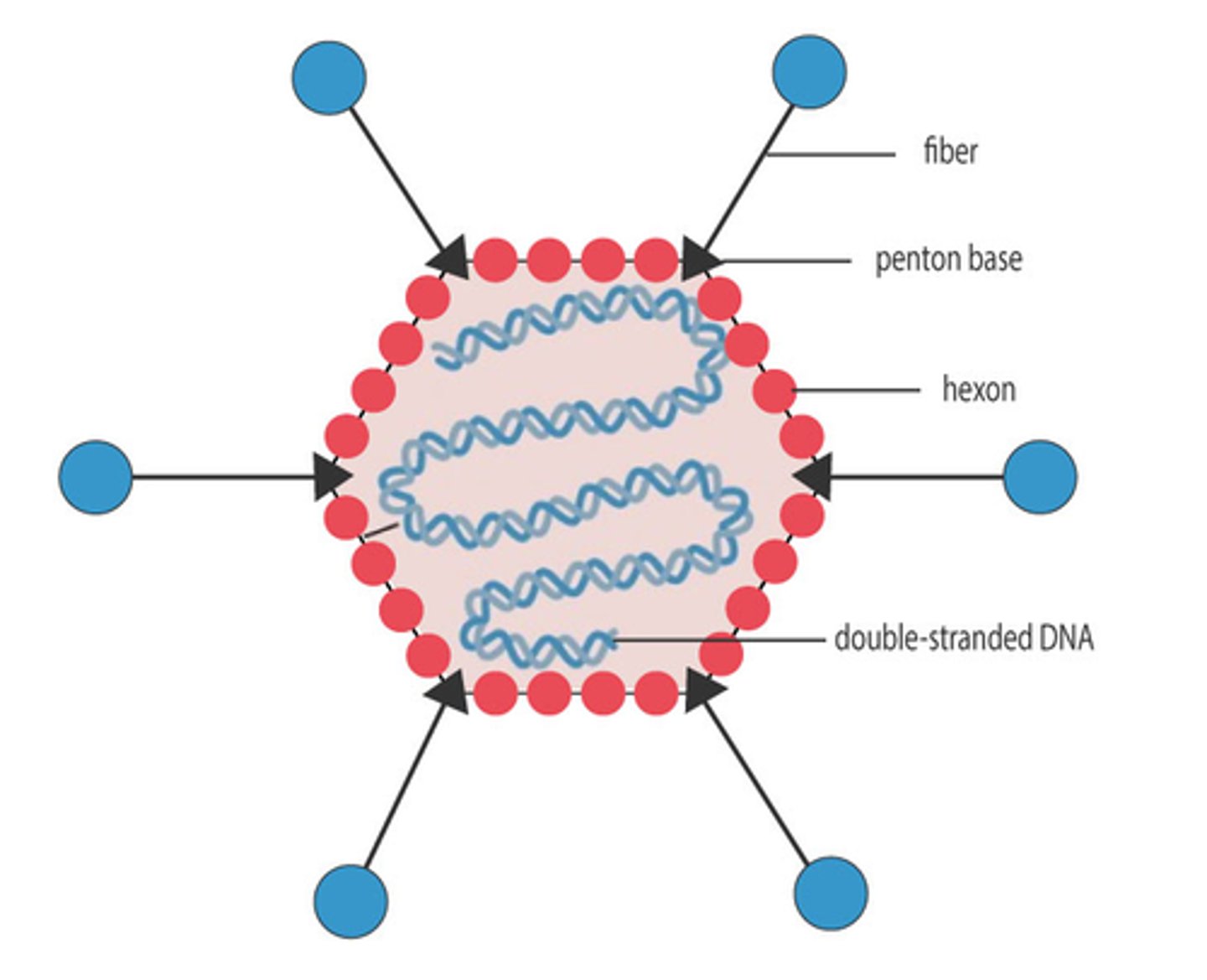
What do the projecting fiber proteins on adenoviruses bind to?
Coxsackie adenovirus receptor (CAR), which helps capsid proteins interact with the cell surface to initiate internalization
What do adenoviruses use for replication in the nucleus?
DDDP
What cell type does adenoviruses infect?
epithelial cells on mucous membranes
What sites do adenoviruses infect?
1)eyes
2)mouth
3)respiratory tract
4)urogenital tract
5)gastrointestinal tract
What determines the specificity of target cells for adenoviruses?
specificity of the virus fiber proteins
What are the symptoms of adenovirus infections?
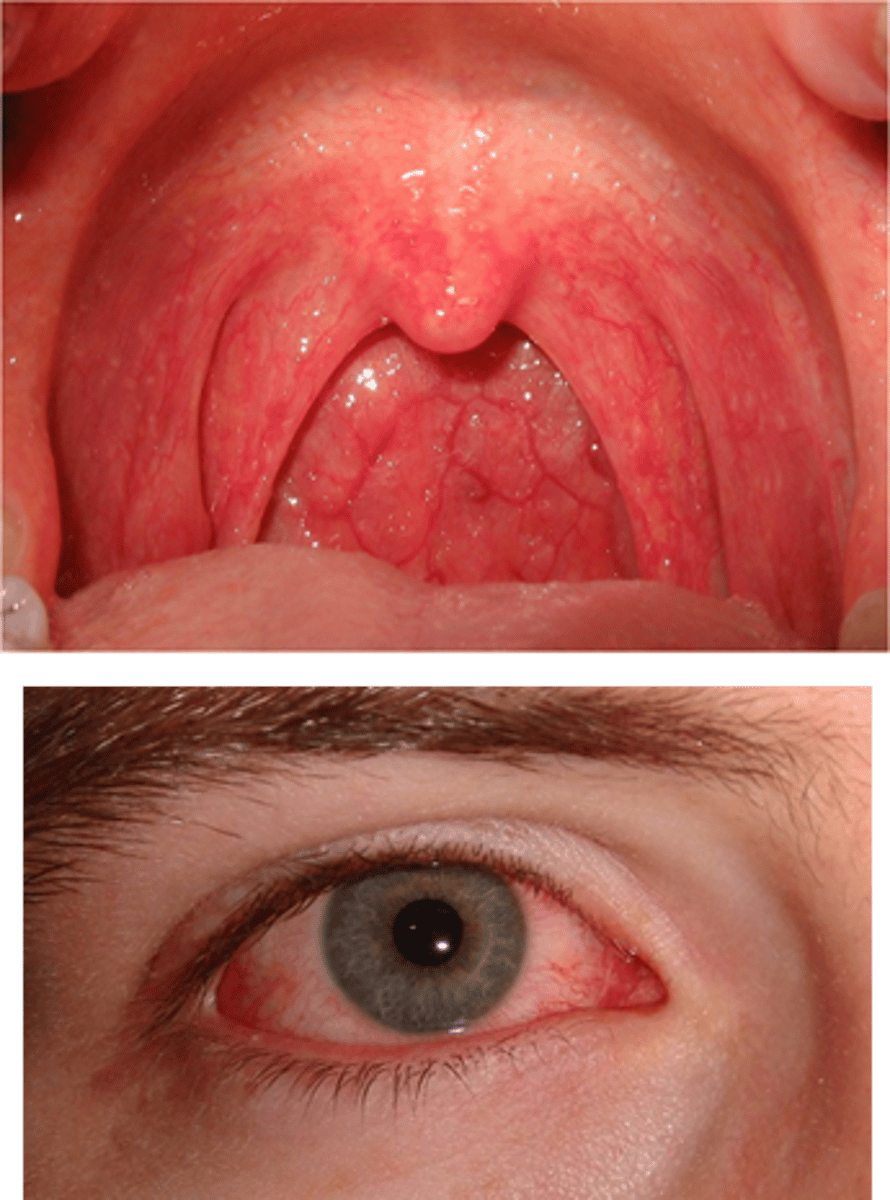
1)upper respiratory illness
2)keratoconjunctivitis
3)pharyngoconjunctival fever
4)diarrhea (most common in infants)
5)hemorrhagic cystitis (Inflammation of the bladder)
6)meningitis/encephalitis (rare)
7)myocarditis (rare)
Which serotypes of adenovirus cause pharyngitis? symptoms?
serotypes 1-7; it presents as redness/blistering (3-5 days)

Which serotypes of adenovirus cause keratoconjunctivitis? symptoms?
serotypes 3 and 7; inflammation of both cornea and conjunctiva that is accompanied by pharyncojunctival fever
What is the most common cause of child gastroenteritis?
rotavirus
What is the most common cause of adult gastroenteritis?
Norwalk and Norwalk-like viruses
What serotypes of adenovirus cause gastroenteritis? symptoms?
serotypes 40 and 41; inflammation of the GI tract (childhood)
What serotypes of adenovirus cause hemorrhagic cystitis? symptoms?
serotypes 11 and 21; bladder inflammation, bleeding from bladder wall, and hospitalization (uncommon)
How do you treat and prevent adenovirus?
1)no antiviral treatment
2)immunization for military recruits for serotypes 4 and 7
3)handwashing (prevents transmission of fecal-oral route)
How is adenovirus transmitted?
fecal-oral route
Papillomaviruses are _________, which means they infect _____ and ______ epithelial cells
epitheliotropic, cutaneous, mucosal
How are most mucosal papillomaviruses transmitted?
sexual (not always)
How are most cutaneous papillomaviruses transmitted?
contact
Several papillomavirus types are associated with cancer (true/false)
True
Infections of papillomaviruses are easily cleared (true/false)
False, they are typically persistent and require years to be "cleared"
Which papillomaviruses are low-risk?
1, 2, 3, and 4
Which papillomaviruses are intermediate-risk?
6, 11, 5, and 8
Which papillomaviruses are high-risk?
16, 18, 33, 39, and 45
What disease do low-risk papillomaviruses cause?
1)skin warts
2)plantar warts
3)benign oral lesions
What disease do intermediate-risk papillomaviruses cause?
HPV 6 and 11:
1)anogenital warts
2)benign oral lesions
3)papillomatosis
HPV 5 and 8:
1)non-melanoma
2)skin cancer
What disease do high-risk papillomaviruses cause?
1)cervical cancer
2)vaginal cancer
3)other anogenital cancers
4)oral cancer
cutaneous warts
Varying morphological presentations that are caused by many HPV serotypes, long incubation, and are difficult to eliminate

What HPV subtypes cause verruca vulgaris?
HPV 2 and 4

How do you treat verruca vulgaris?
excision and/or cryotherapy (benign)

What HPV subtypes cause condyloma?
HPV 6 and 11
How do you treat condyloma?
excision, cryotherapy, trichloroacetic acid, and imiquimod (benign)
What HPV subtypes cause recurrent respiratory papillomatosis (RRP)?
HPV 6 and 11
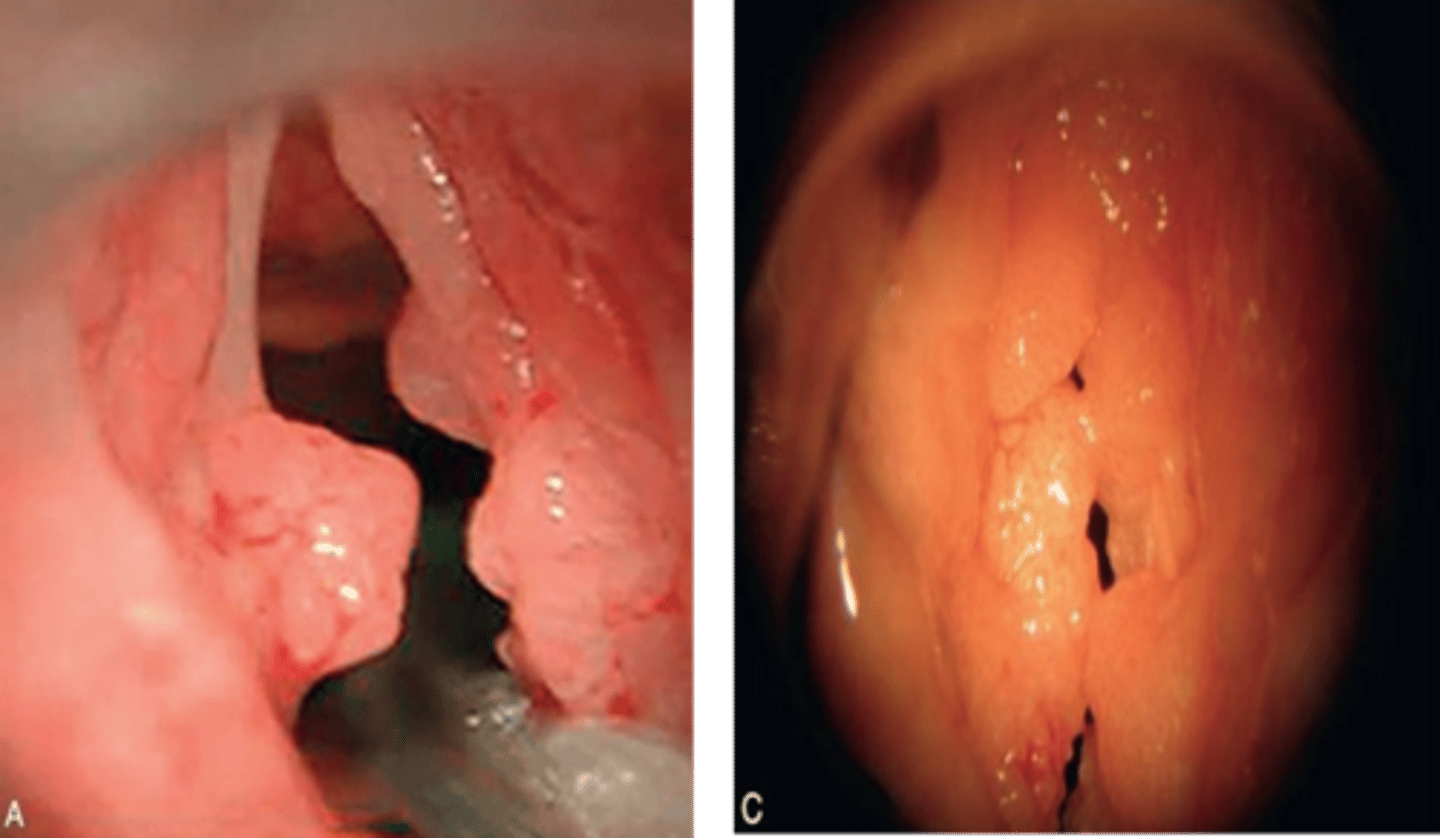
How do you treat recurrent respiratory papillomatosis (RRP)?
constant surgery removal (benign)

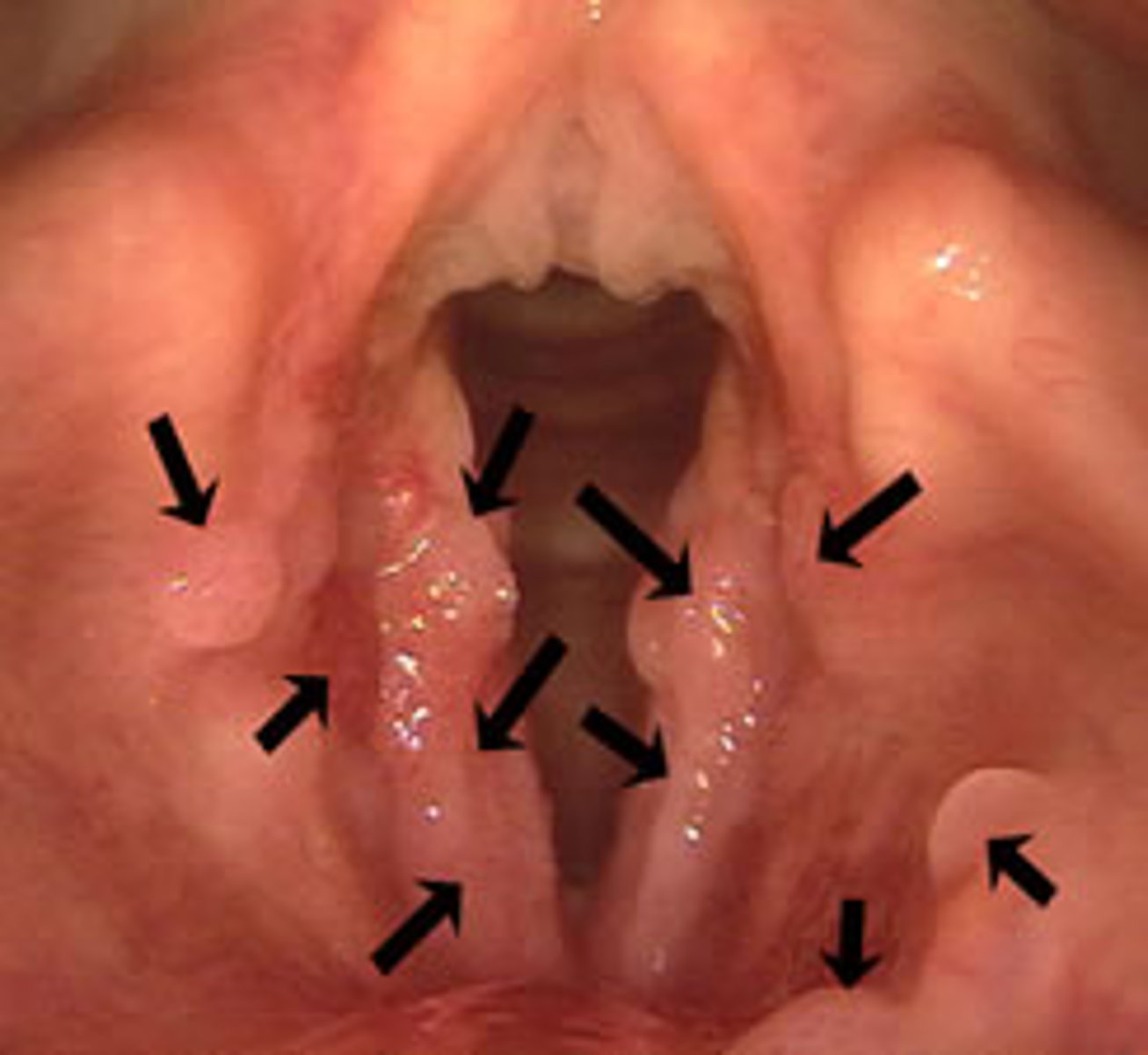
recurrent respiratory papillomatosis (RRP)
papilloma on the vocal cords, larynx, and respiratory tract that are transmitted from mother to child at birth (HPV 6 and 11)
What HPV subtypes cause oral papilloma?
HPV 6 and 11
How do you treat oral papilloma?
surgical removal or cryotherapy (benign)

What HPV subtypes cause head and neck cancer?
HPV 16 and 18

HPV head and neck cancer is more common in _________ than _________
men, women
What is second most common cancer in women?
cervical cancer
Which gender is at the greatest risk of HPV associated head and neck cancers?
men
What percentage of the sexually active population has/had anogenital HPV? high-risk HPV?
75% and 40%
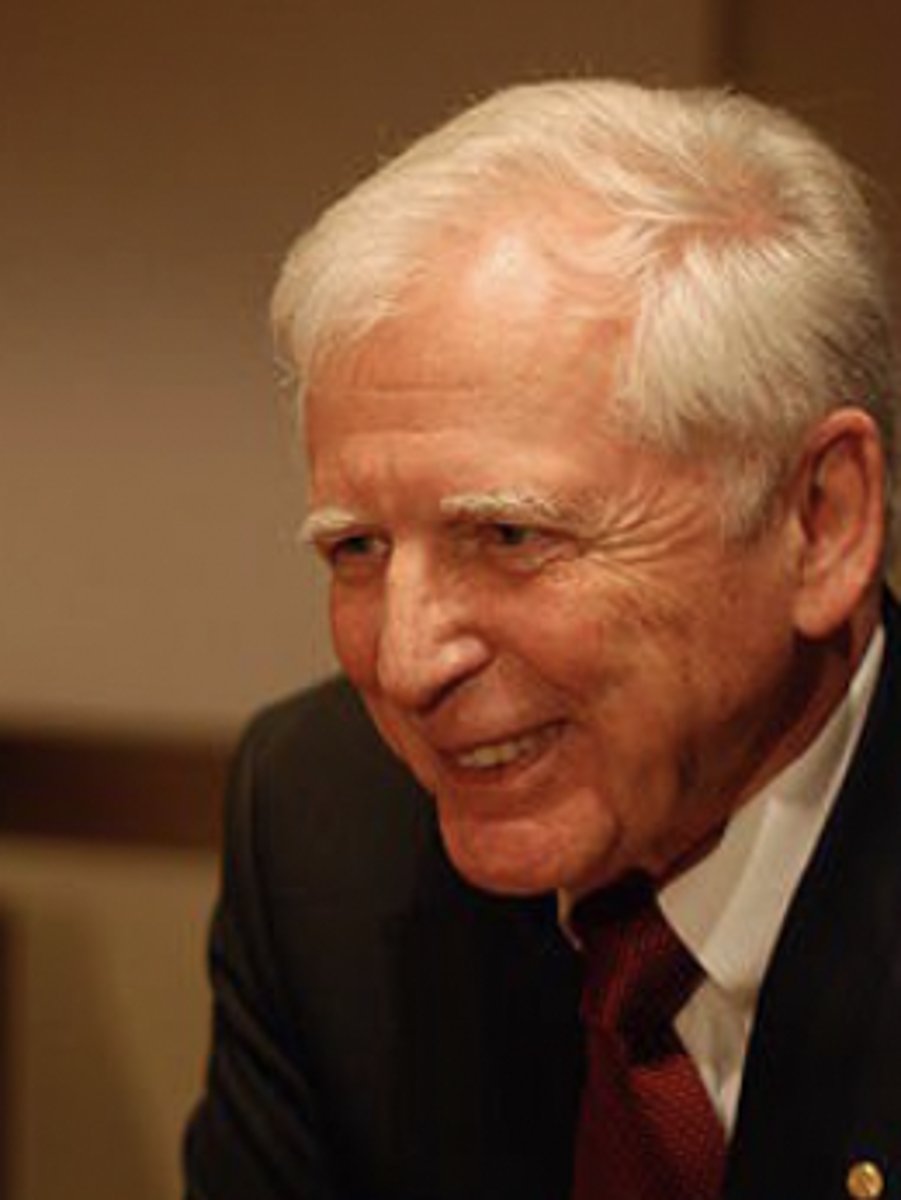
What did Harald zur Hausen do?
He discovered that HPVs cause genital warts (HPV 6) and cervical cancer (HPV 16 and 18)
What is the structure of papillomaviruses?
non-enveloped, icosahedral with circular dsDNA viral genome inside the capsid
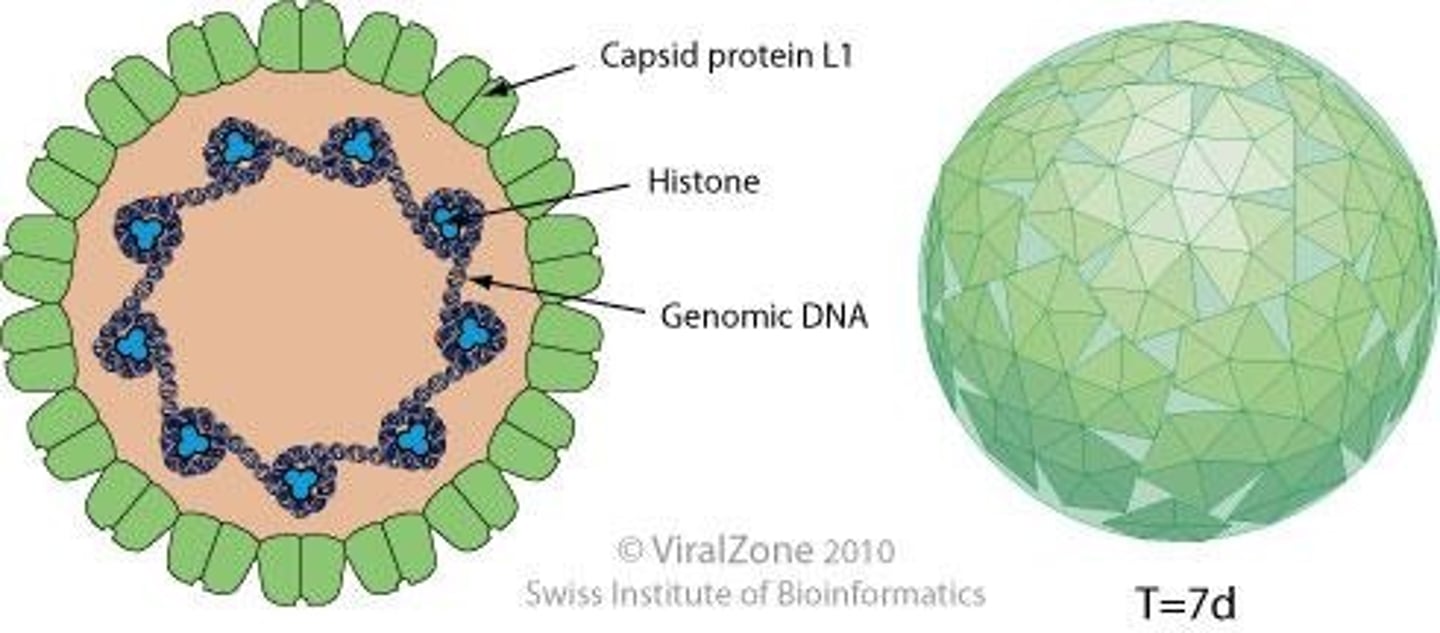
What are L1 and L2?
They are major capsid (L1) and minor capsid proteins (L1) that help with attachment and help form the outer shell of the virus
How does HPV infect epithelium?
1)tear/wound of the epidermis
2)HPV infects basal cells
3)tear/wound heals
4)basal cells differentiate into squamous cells and move up
5)HPV virions amplify as cells are pushed from the basal layer and differentiate
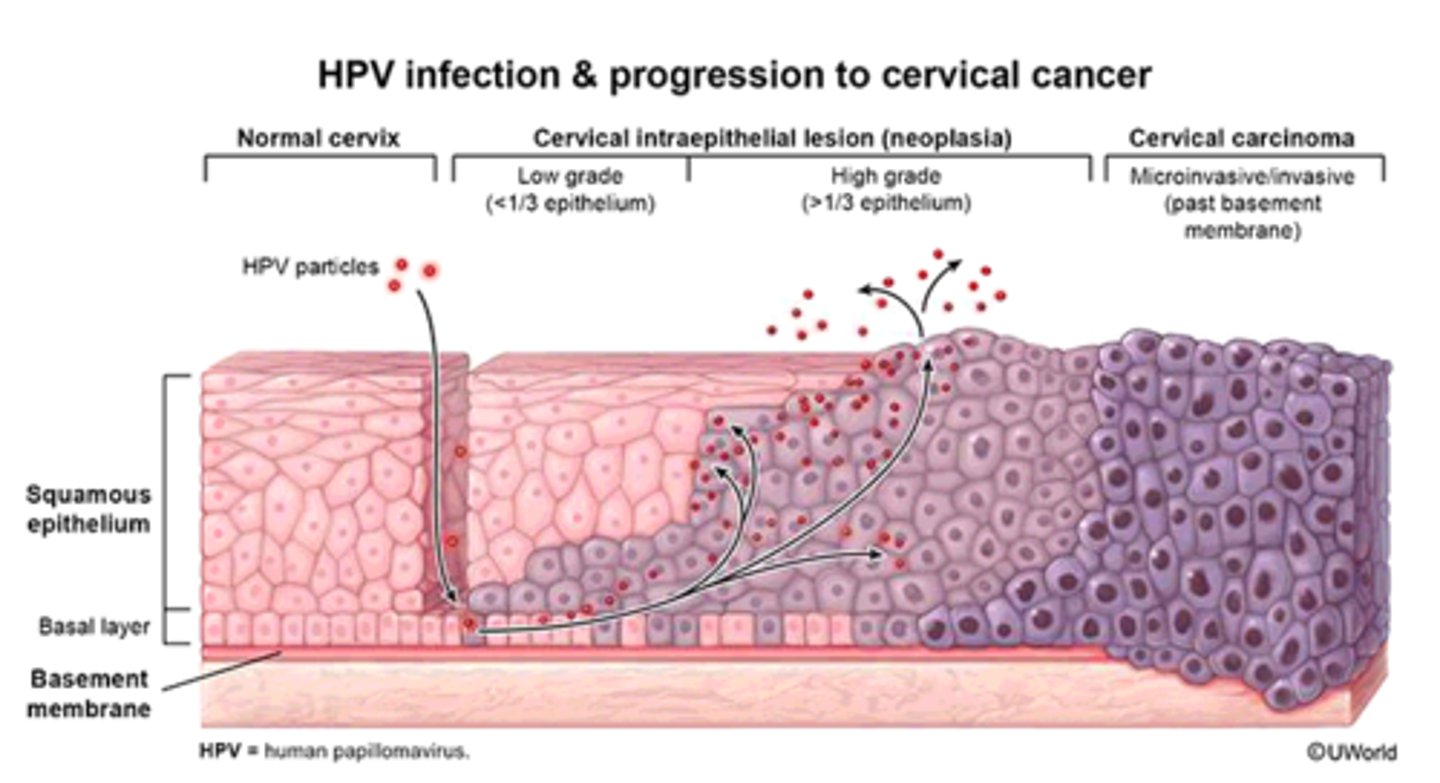
There are no infectious virions produced in the lower basal layer of the epidermis (true/false)
True, the virions are produced by basal cells differentiating into squamous cells and moving up toward the surface.
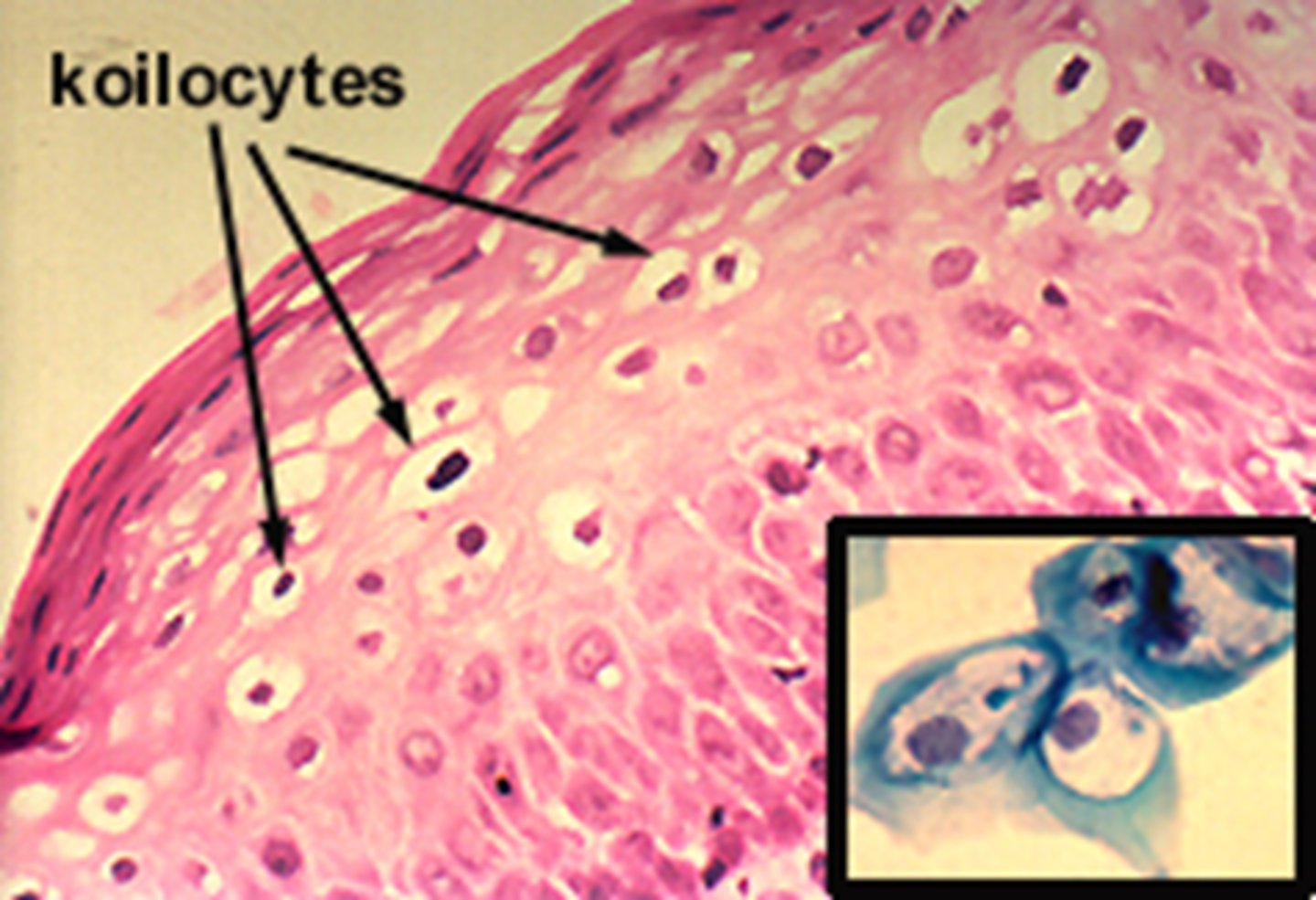
HPV infection results in ________ proliferation and development of _________
aberrant, koilocytes
What are koilocytes?
Abnormal cells created by HPV infection that present with nuclear enlargement, irregularity of nuclear membrane contour (raisin-like), hyperchromasia (darker nucleus), and perinuclear halo (clear area around nucleus)
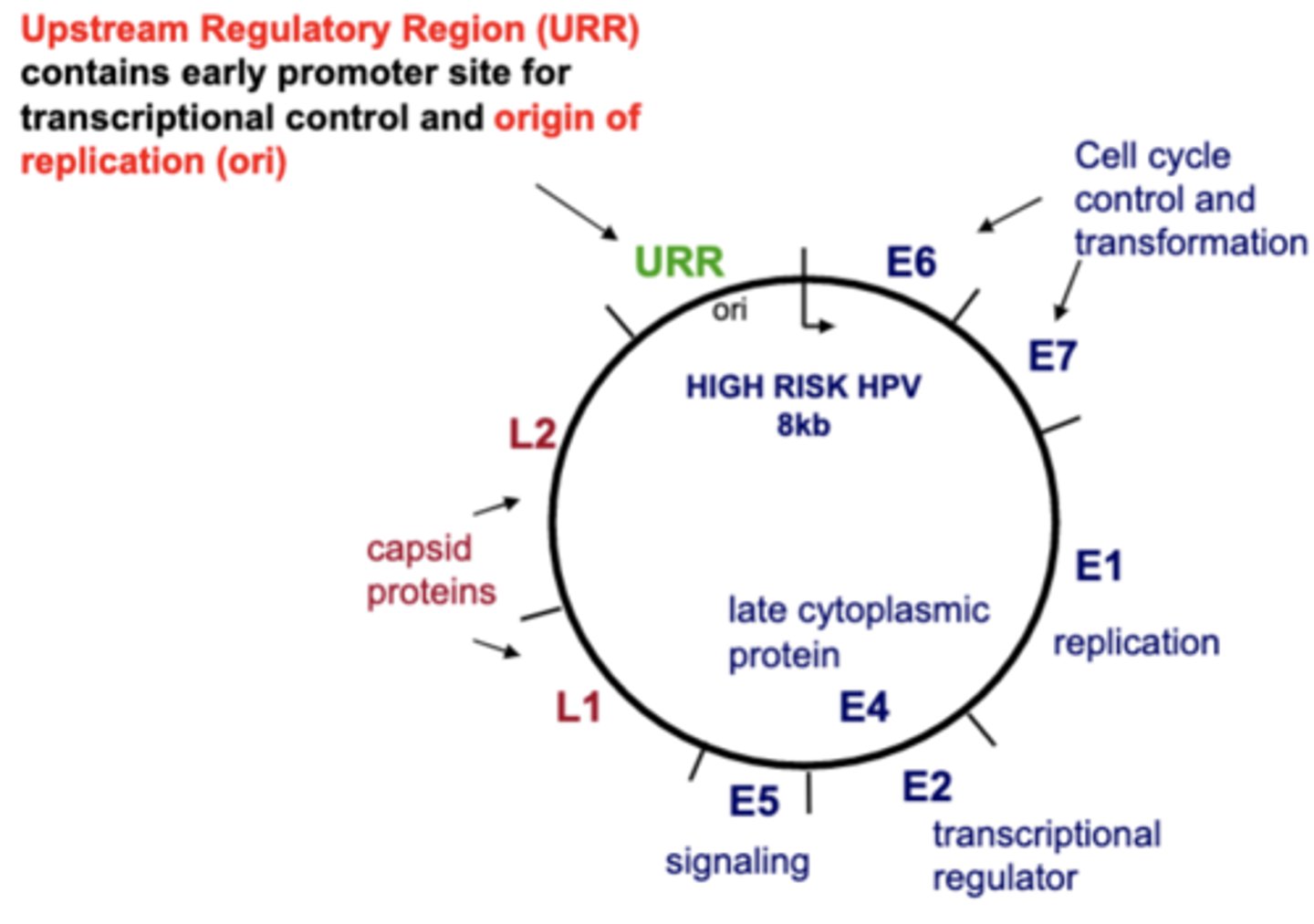
How does HPV cause aberrant cell proliferation?
HPV produces proteins (E6 and E7) that drive cell synthesis and initiate continuous proliferation by removing cell check point proteins.
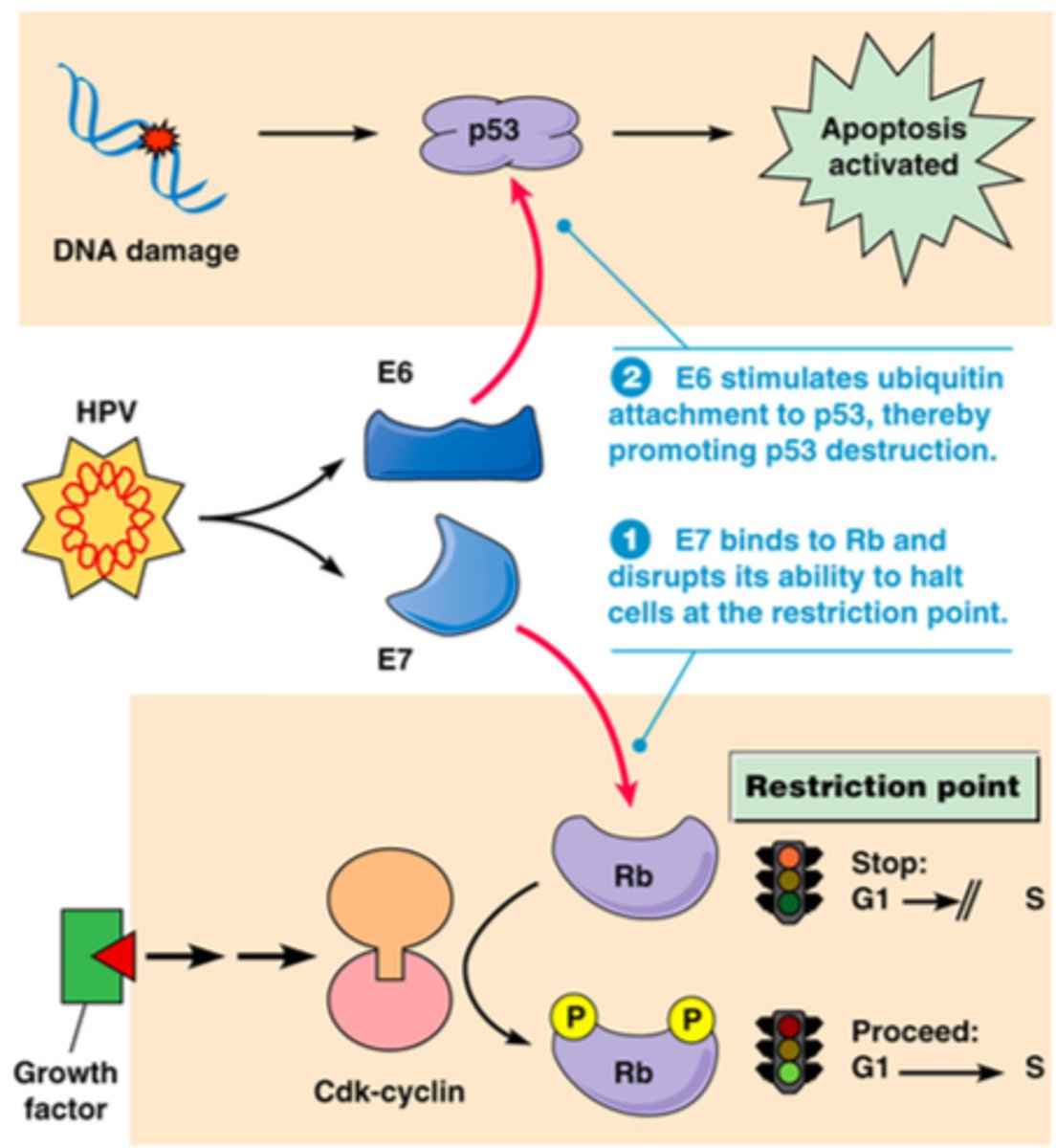
What are the functions of the E6 protein for HPV cancer?
1)degradation of p53 (guardian of the genome) to release cell cycle control
2)activation of hTERT (telomerase that helps with the immortalization of cells)
3)degradation of other cellular proteins important for controlling cellular growth
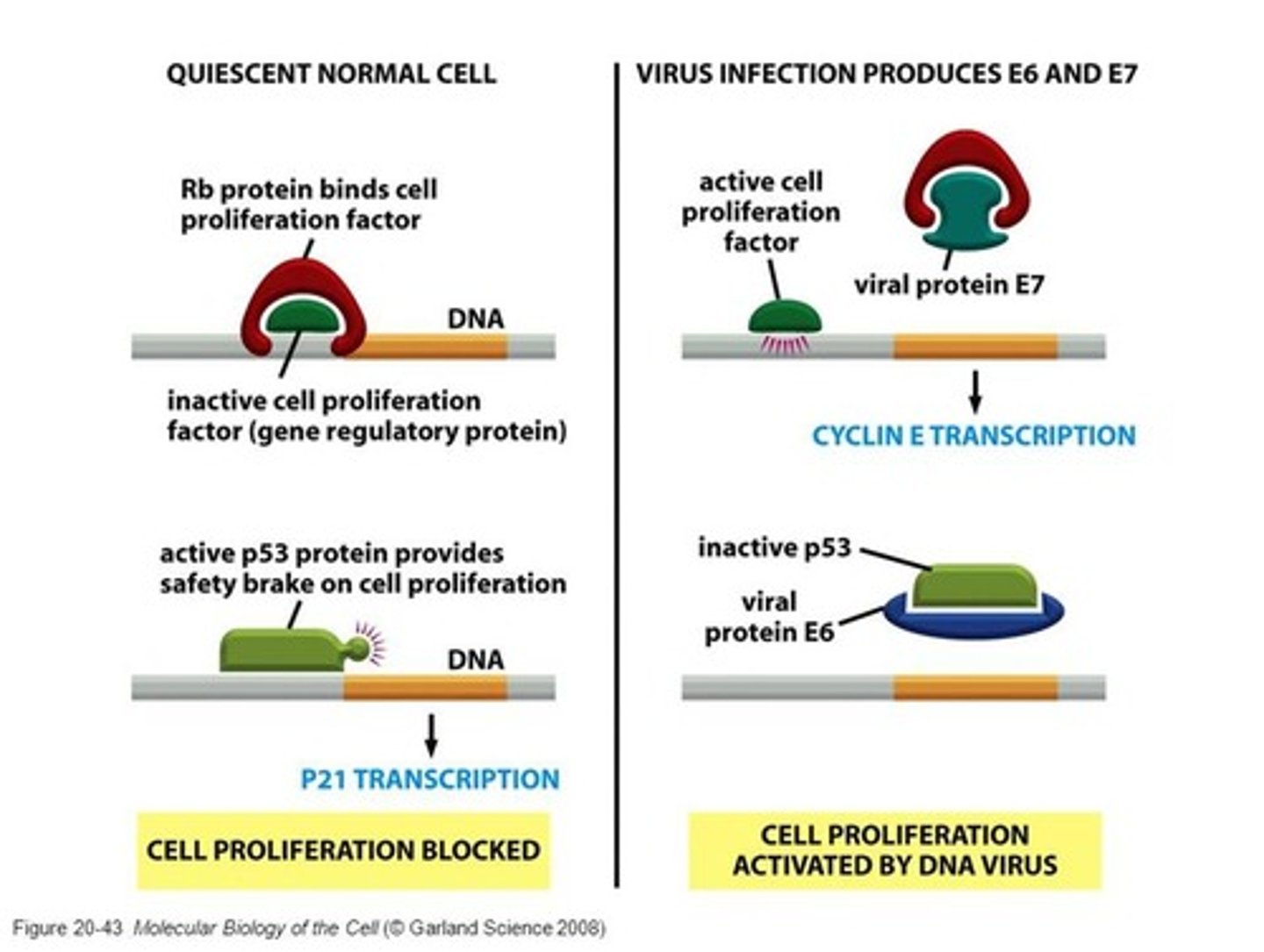
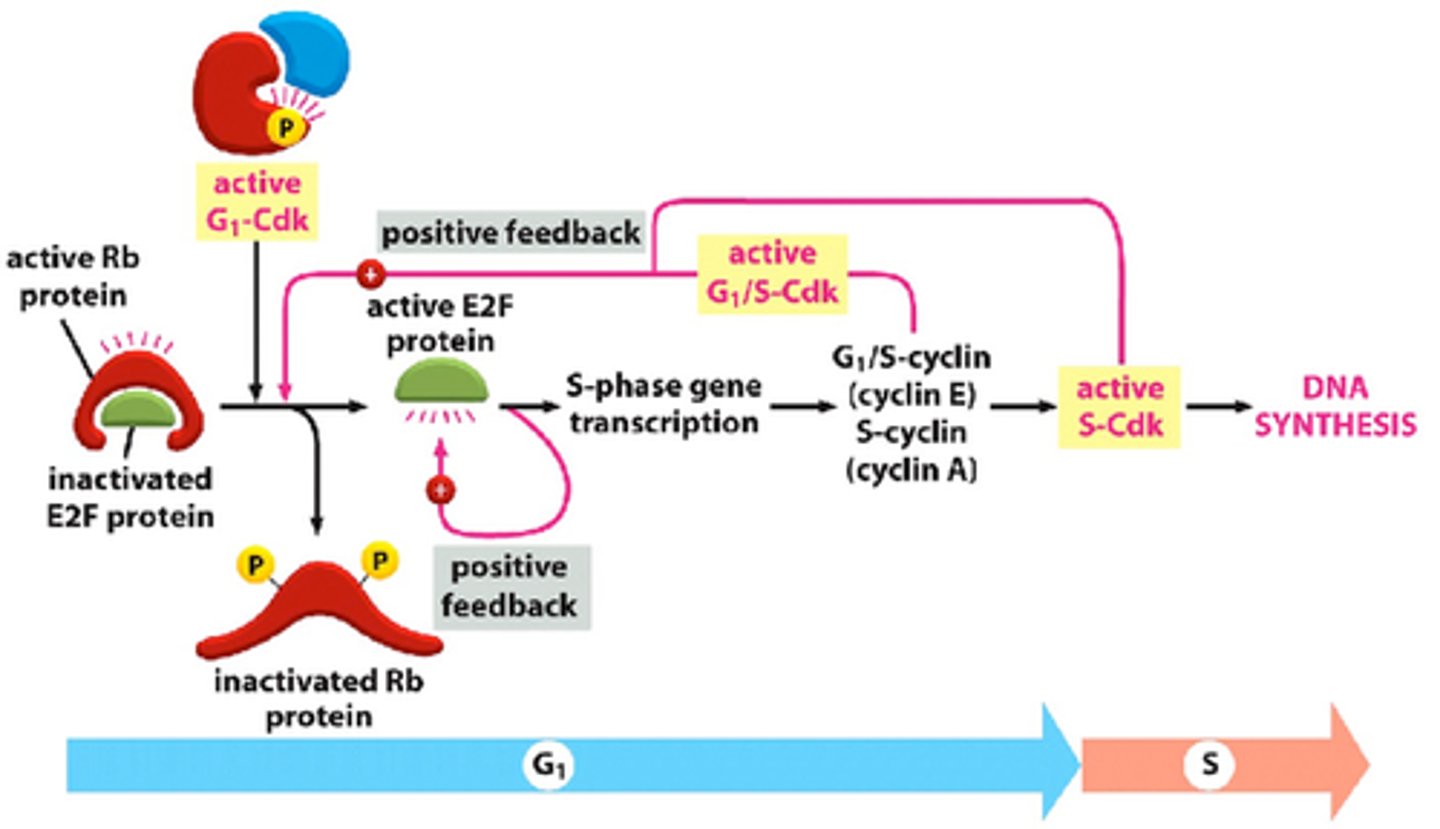
What is the function of the E7 protein for HPV cancer?
inactivation of Rb (cellular tumor suppressor protein) that causes the release of E2F (transcription factor) to stimulate DNA synthesis (S) genes
How does HPV progress to malignant cancer?
1)HPV upregulates the expression of E6 and E7
2)Virus integrates into the cell's DNA genome (progression to cancer)
HPV can still produce virions once it integrates into the cell genome (true/false)
False, once it integrates, it no longer produces virions and progresses to malignant tendencies (cancer)
How are HPV-associated cervical cancers detected?
PCR and pap smears (HPV 16, 18, and 31)
How do you treat HPV-associated cervical cancers?
early lesions: surgery or cryotherapy
late lesions: surgery, radiation, or chemotherapy
What is the presentation of an abnormal pap smear test?
1)increased nuclear cytoplasm ratio
2)hyperchromatic nuclei
3)pleiomorphic nuclei
4)lack of squamous cell differentiation
How are HPV-associated oral cancers detected?
1)visual presentation (dentists)
2)PCR test (biopsy)
How do you treat HPV-associated oral cancers?
surgery and radiation
Which is easier to treat, HPV oral or non-oral cancers?
HPV oral cancers are more treatable than non-oral cancers
____% of oropharyngeal cancers are caused by HPV
50
How were HPV vaccines developed?
HPV vaccines were developed using recombinant technology (yeast and baculovirus) to produce the virus's L1 protein, which self-assembles into virus-like particles that safely trigger an immune response without containing viral DNA.
What are the three commercially available HPV vaccines?
1)Gardasil (HPV 6, 11, 16, 18)
2)Gardasil 9 (HPV 6, 11, 16, 18, 31, 33, 45, 52, and 58)
3)Cervarix (HPV 16 and 18)
How successful are HPV vaccines?
1)high antibody titers after vaccination
2)97-100% efficacy in preventing HPV infections/lesions
3)64% reduction in vaccine-type HPV infections among teen girls since vaccination started
What are the adverse effects of HPV vaccines?
headache, aches, fever, and fainting (rare)
What is the "challenge of HPV vaccines"?
1)not curative (if previously infected)
2)distribution and recommendation of the vaccine
3)cost (without insurance)
4)multiple types (not all covered by vaccine)
5)acceptance (religion, social, misinformation, low compliance in boys)