Normal Anatomy and Physiology of the Female Pelvis (Ch. 41)
1/121
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
122 Terms
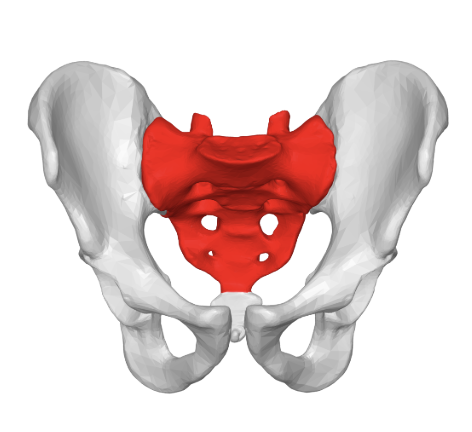
how many bones are in the bony pelvis?
4 bones
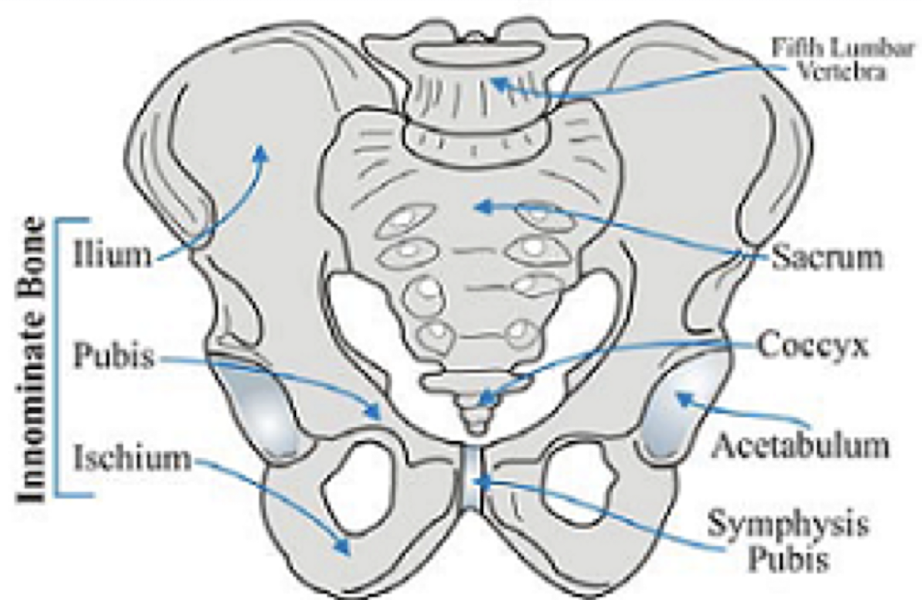
what are the bones in the bony pelvis?
sacrum
coccyx
innominate bones (2)
sacrum
forms part of posterior margin
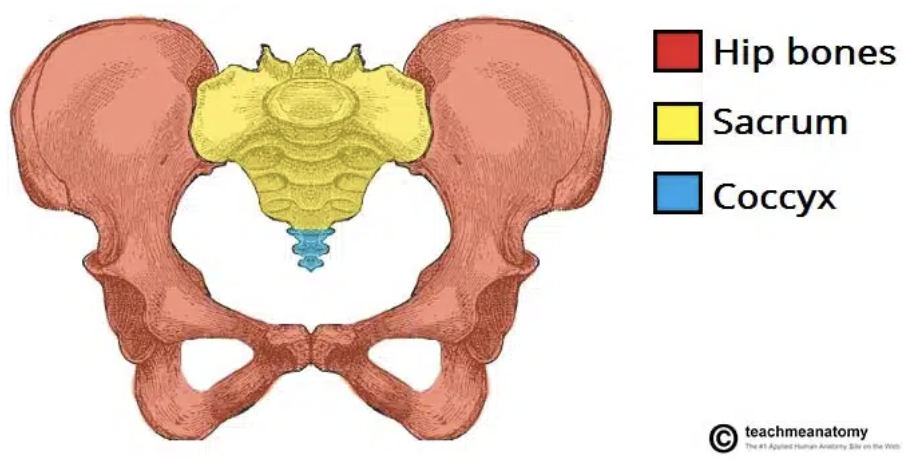
coccyx
forms part of posterior margin
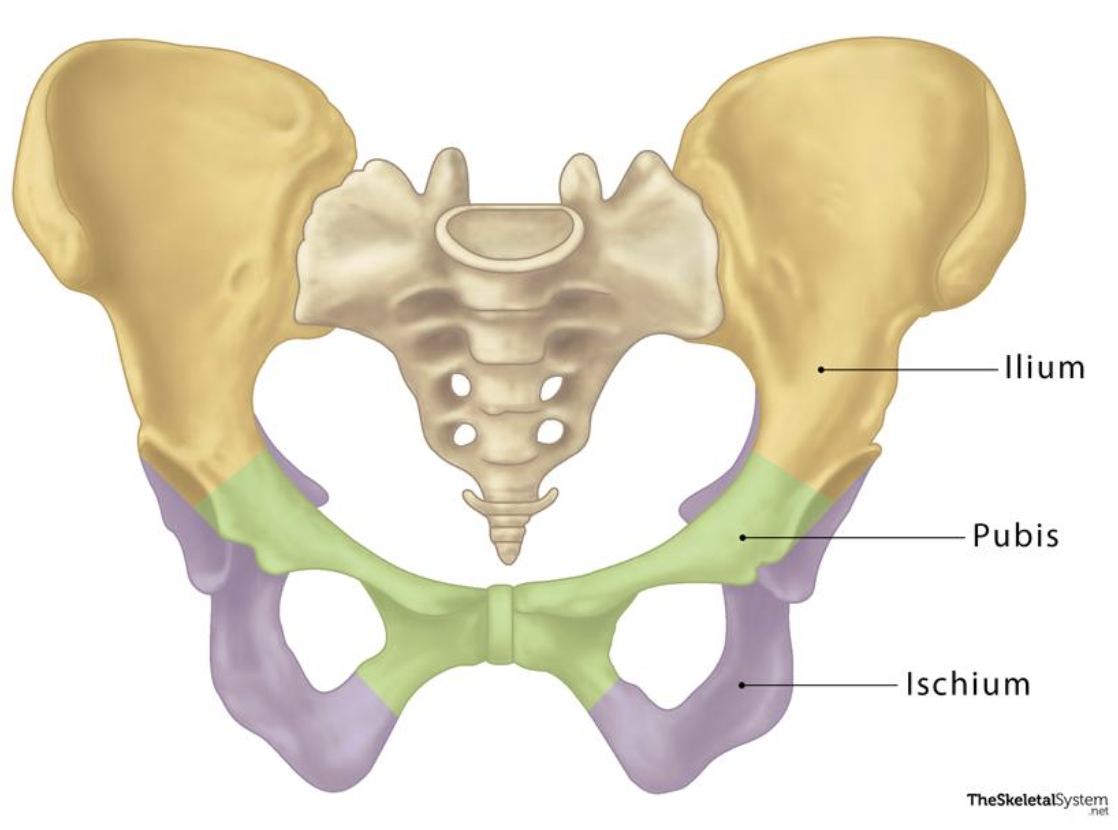
innominate bones
aka hip bones (consists of ilium, ischium, and pubis)
forms anterior/lateral margin
what are the 2 regions of the pelvis?
greater/false pelvis
lesser/true pelvis
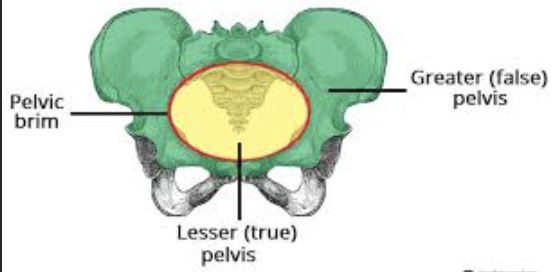
false pelvis
aka greater pelvis
above linea terminalis
contains mostly bowel
“bound posteriorly by the lumbar vertebrae, supported and bound laterally by the iliac fossae and iliacus muscles, and anteriorly by the lower anterior abdominal wall”
“portion of pelvis found above the brim”

true pelvis
aka lesser pelvis
below linea terminalis
contains uterus, ovaries, and adnexa
“pelvic cavity found below the brim”

muscles of the false and true pelvis
false pelvis
rectus abdominis
psoas major
iliopsoas
iliacus
true pelvis
piriformis
obturator internus
levator ani and coccygeus (pelvic floor muscles)
what are the 4 false (greater) pelvis muscles?
rectus abdominis
psoas major
iliopsoas
iliacus
what are the 4 true (lesser) pelvis muscles?
piriformis
obturator internus
levator ani
coccygeus
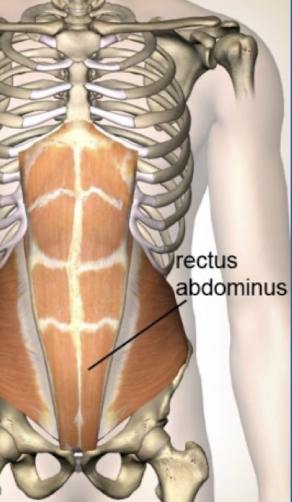
rectus abdominis
greater pelvis muscle
paired muscles that run vertically on side of anterior abdominal wall (6-pack)
extends from symphysis pubic to costal cartilages of ribs
controls pelvis tilt and curvature of lower spine
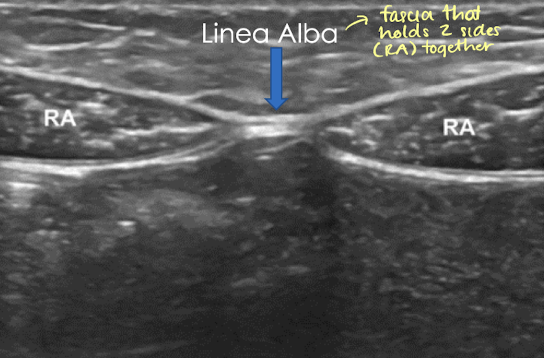
SONO: rectus abdominis
hypoechoic with echogenic striations in LONG
right and left rectus abdominis muscles join linea alba (echogenic) which courses along abdominal midline
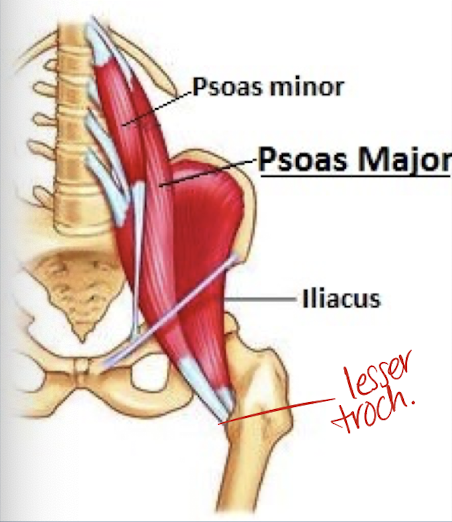
psoas major
greater pelvis muscle
origin: lumbar spine
insertion: lesser trochanter (posterior femur)
courses inferiorly
DOES NOT ENTER true pelvis
joins iliacus muscle to form iliopsoas muscle
“paired muscles that originate at transverse process of lumbar vertebrae and extends inferiorly through false pelvis on pelvic sidewall, where it unites with iliacus muscle to form iliopsoas muscle before inserting into lesser trochanter of the femur; serves to flex the thigh toward the pelvis”
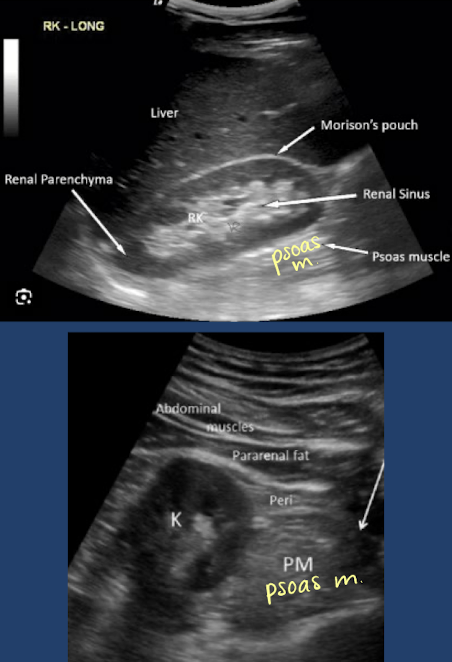
SONO: psoas major
visualized while imaging kidneys
hypoechoic muscle tissue with echogenic striations
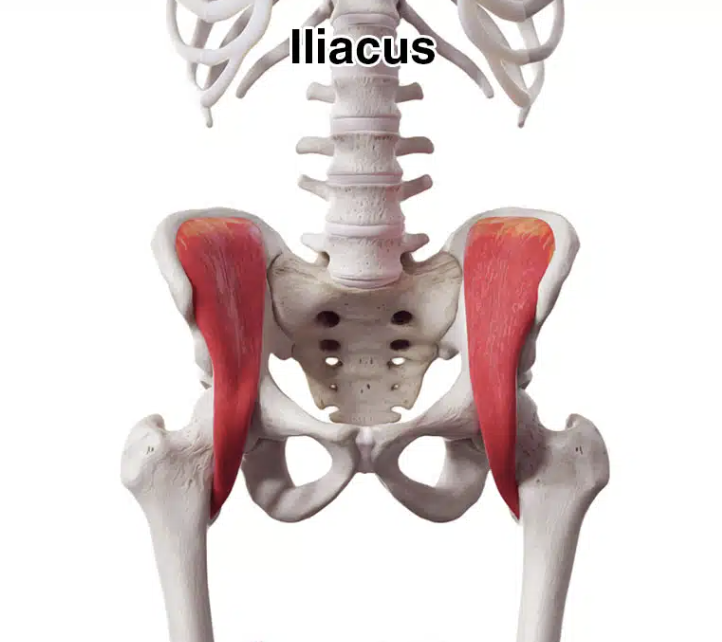
iliacus muscle
greater pelvis muscle
origin: inner iliac crest/fossa and sacrum
insertion: lesser trochanter (posterior femur)
courses inferiorly
DOES NOT ENTER true pelvis
joins psoas muscle to form iliopsoas muscle
“paired triangular, flat muscles that cover the inner curved surface of iliac fossae; arise from iliac fossa and join psoas major muscles to form lateral walls of the pelvis”
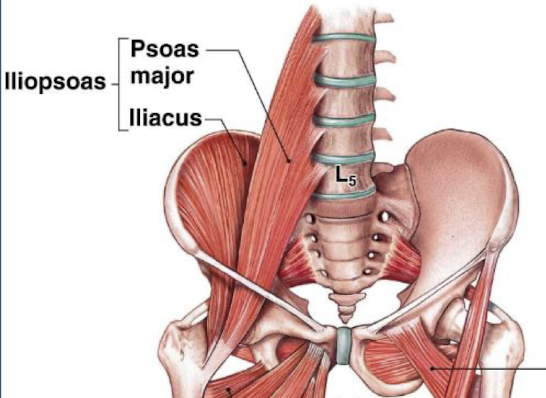
iliopsoas muscle
greater pelvis muscle
group of muscles:
psoas major
psoas minor
iliacus
origin: lumbar, sacrum, iliac crest and fossa
insertion: lesser trochanter (posterior femur)
functions:
hip flexor
stabilize lower back and core
exits pelvis posterior to inguinal ligament
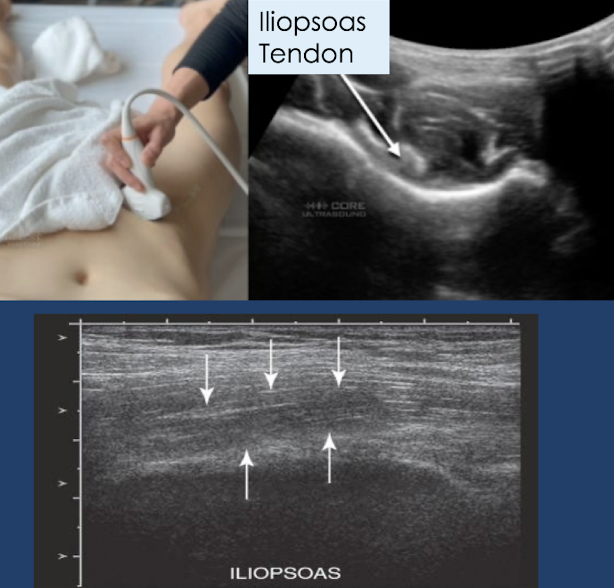
SONO: iliopsoas muscle
hypoechoic with echogenic linear striations in LONG
distal iliopsoas tendon is echogenic
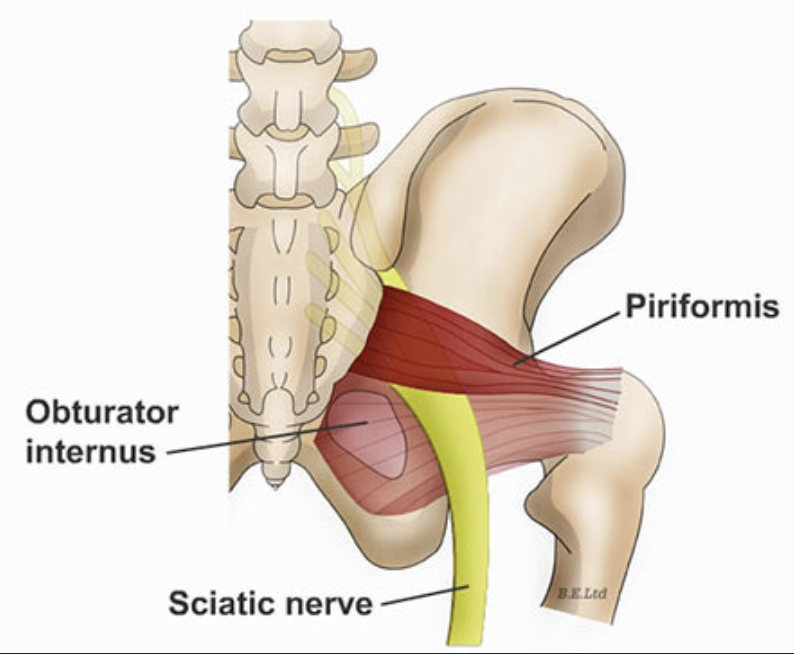
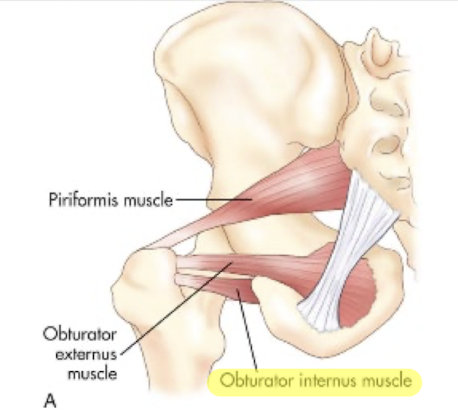
piriformis muscle
lesser pelvis muscle
origin: sacrum
insertion: greater trochanter (lateral femur)
“flat, pyramidal muscle arising from anterior sacrum, passing through greater sciatic notch to insert into superior aspect of greater trochanter of femur; serves to rotate and abduct the thigh”
associated with piriformis syndrome (baby pressing on pelvis —> piriformis compressing on nerve, causing nerve injury)
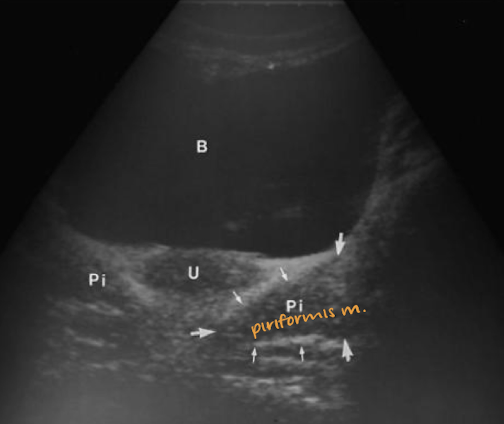
SONO: piriformis muscle
flat
triangular-shaped
hypoechoic
** can be mistaken for ovary—so elongate transducer to see if “ovary” elongates
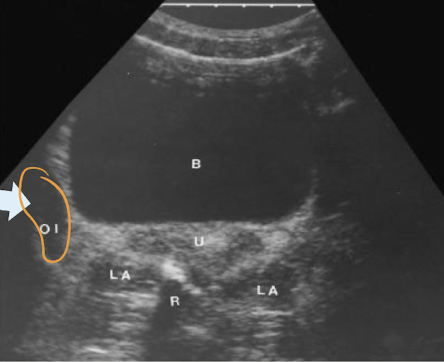
obturator internus muscle
lesser pelvis muscle
origin: anterolateral pelvic wall/pubic ramus/obturator foramen
insertion: greater trochanter (lateral femur)
“triangular sheet of muscle that arises from anterolateral pelvic wall and surrounds obturator foramen; passes through lesser sciatic foramen and inserts into medial aspect of greater trochanter of femur; serves to rotate and abduct the thigh”
SONO: obturator internus muscle
hypoechoic elongated, vertical, ovoid structure

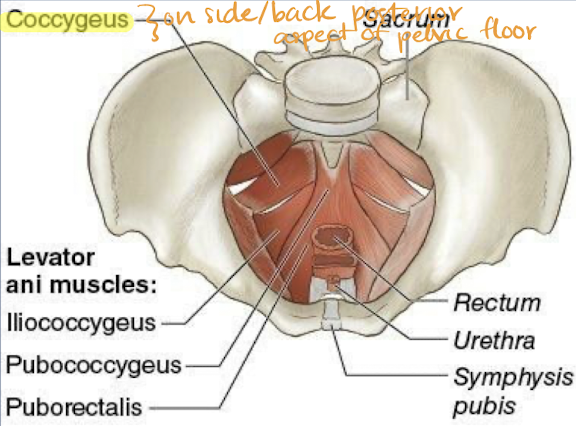
levator ani
lesser pelvis muscle
pelvic floor muscles
group of muscles:
pubococcygeus
puborectalis
iliococcygeus
spans pelvic floor like hammock to support internal organs
plays important role in rectal and urinary incontinence
forms pelvic diaphragm with coccygeus muscle
kegel exercises strengthen the muscle
“one of the two muscles of the pelvic diaphragm that stretch across the floor of the pelvic cavity like a hammock, supporting the pelvic organs and surrounding the urethra, vagina, and rectum; a broad thin muscle that consists of pubococcygeus, puborectalis, and iliococcygeus muscles”
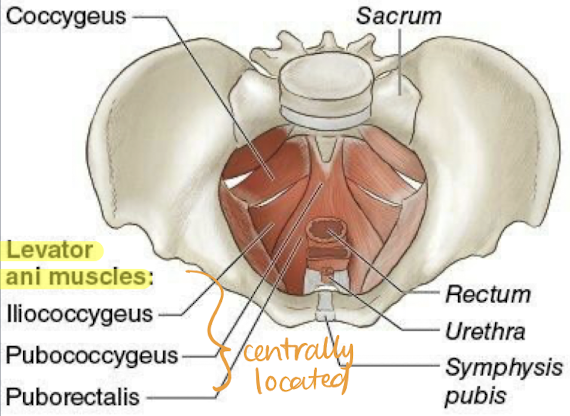
coccygeus
lesser pelvis muscle
located on posterior pelvic floor
triangular sheet of muscle
posterior aspect of pelvic diaphragm
not usually evaluated on US
“one of the two muscles in pelvic diaphragm; posterior pelvic floor muscle that support the coccyx”
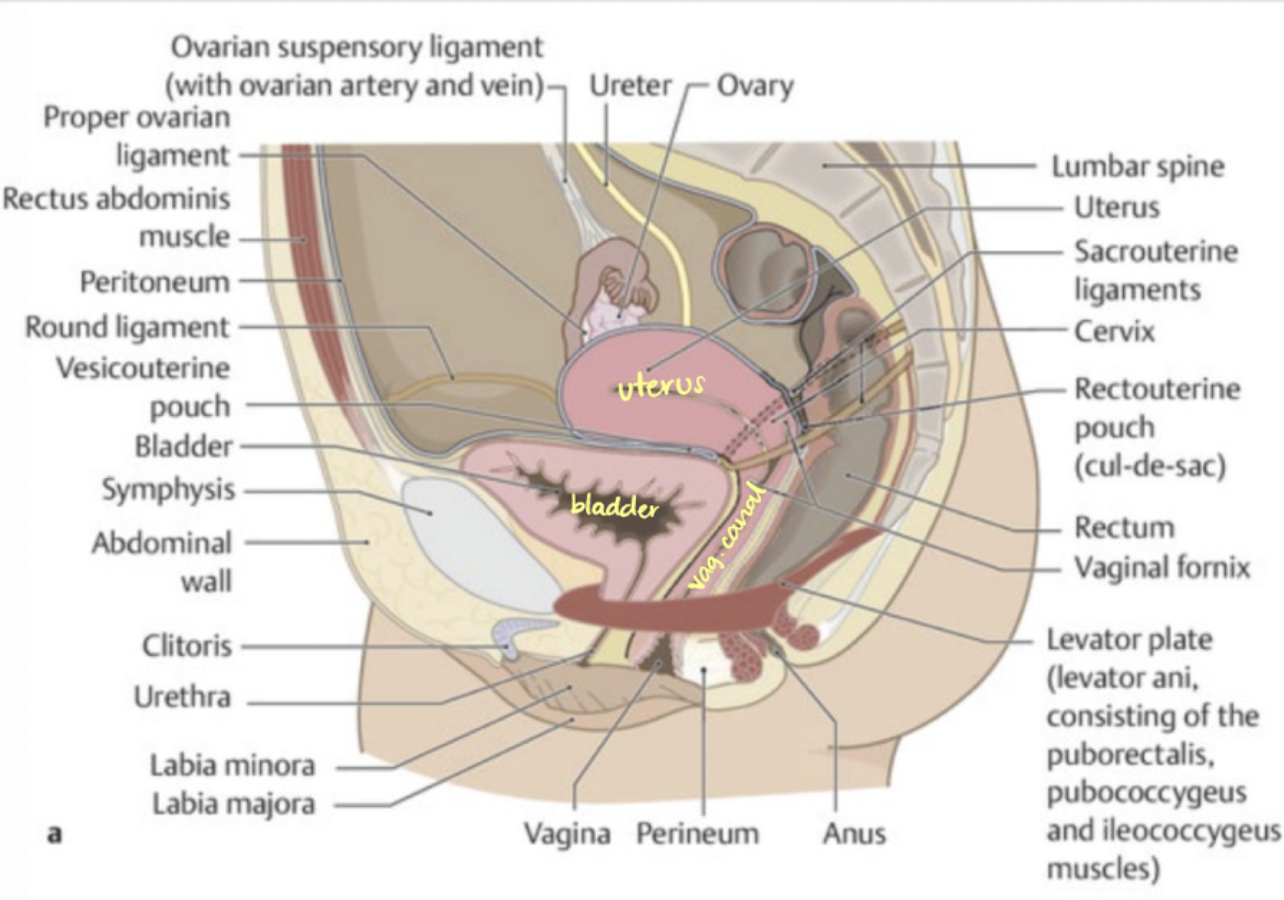
anatomy of female pelvis
** filled bladder pushes uterus back —> better acoustic window
anatomy of female reproductive system
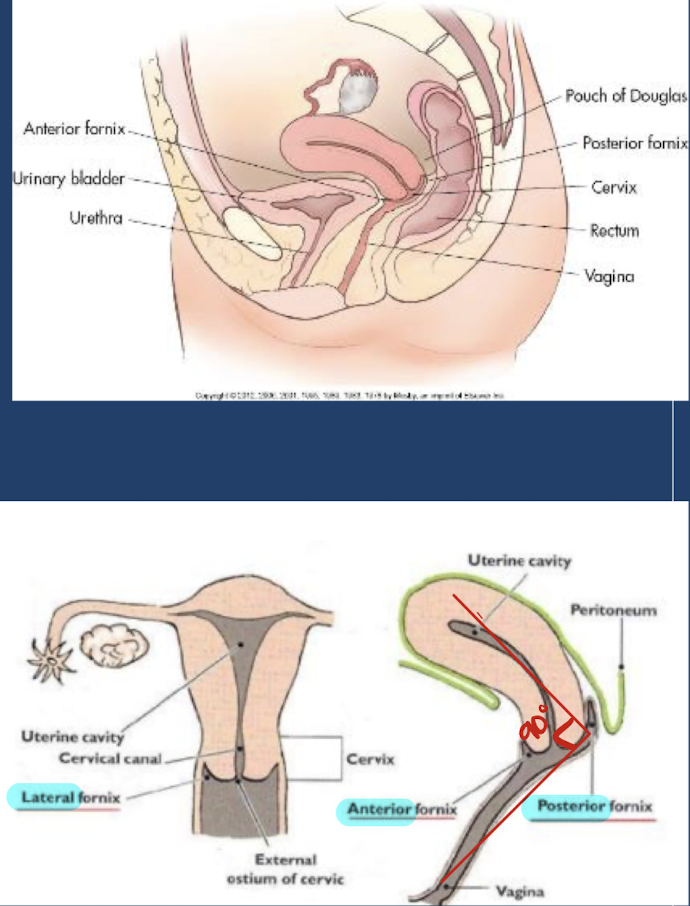
vagina
collapsed muscular tube that extends from external genitalia to cervix of uterus
posterior to bladder and urethra
anterior to rectum and anus
forms 90-degree angle with uterine cervix
vaginal lumen surrounding cervix is divided into 4 fornices:
anterior
posterior
lateral (x2)
inner walls from vaginal canal
outer walls form muscular layer
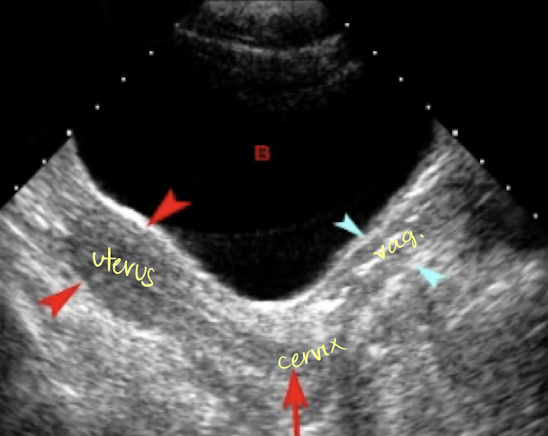
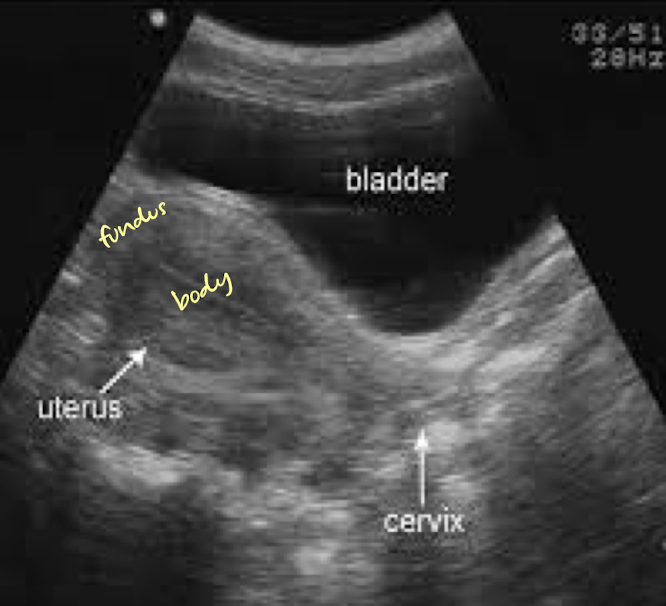
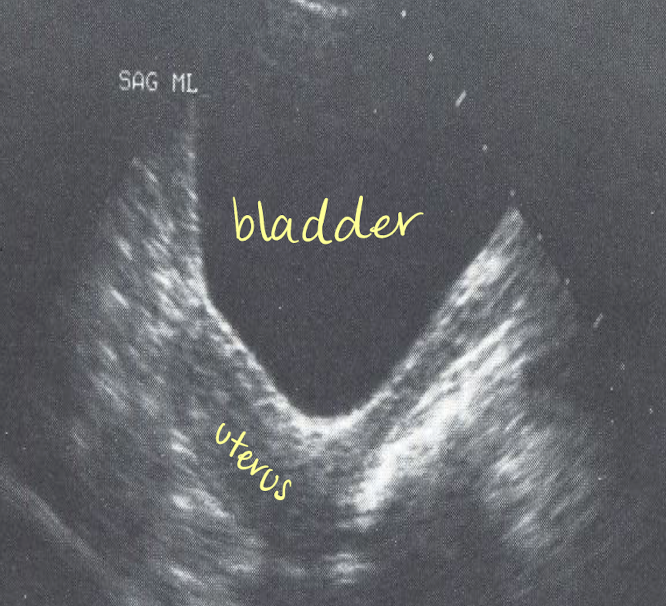
SONO: vagina, cervix, uterus
uterus
located in lesser (true) pelvis
posterior to bladder in vesicouterine pouch
anterior to colon/rectum in rectouterine pouch (aka Pouch of Douglas)
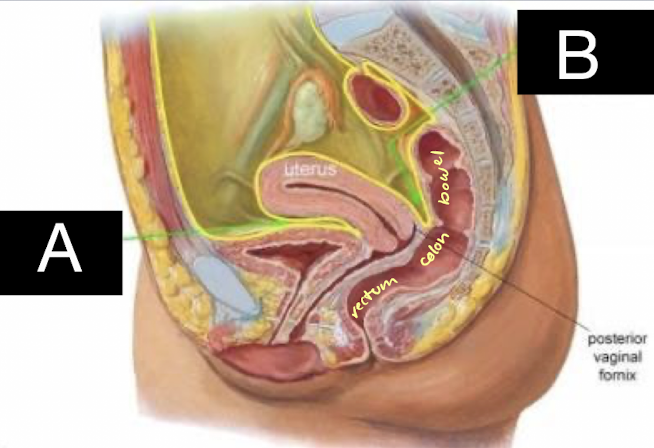
what is A pointing to?
vesicouterine pouch
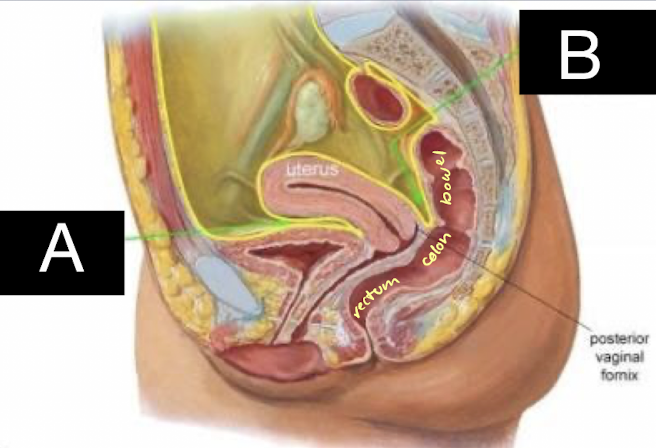
what is B pointing to?
rectouterine pouch (aka Pouch of Douglas)
potential spaces where fluid may accumulate
anterior cul-de-sac (vesicouterine pouch)
in front of uterus
posterior cul-de-sac (pouch of Douglas/rectouterine space)
behind uterus
FF often accumulates here b/c of gravity and bigger space
Space of Retzius (retropubic space)
in front of bladder
“between anterior bladder and pubic symphysis”
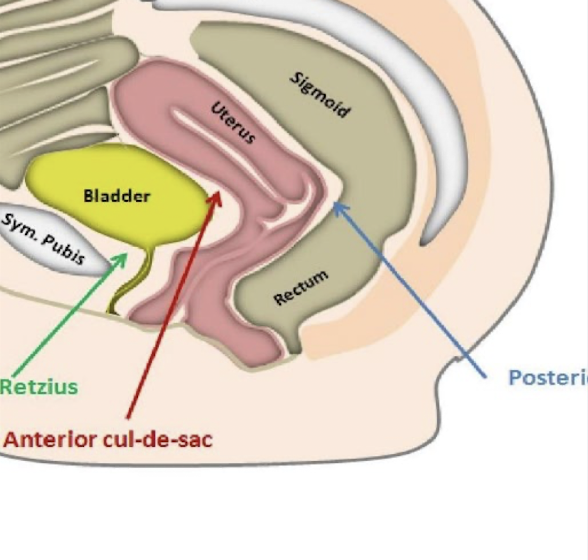
another name for anterior cul-de-sac
vesicouterine space
another name for posterior cul-de-sac
pouch of Douglas or rectouterine space
another name for space of Retzius
retropubic space
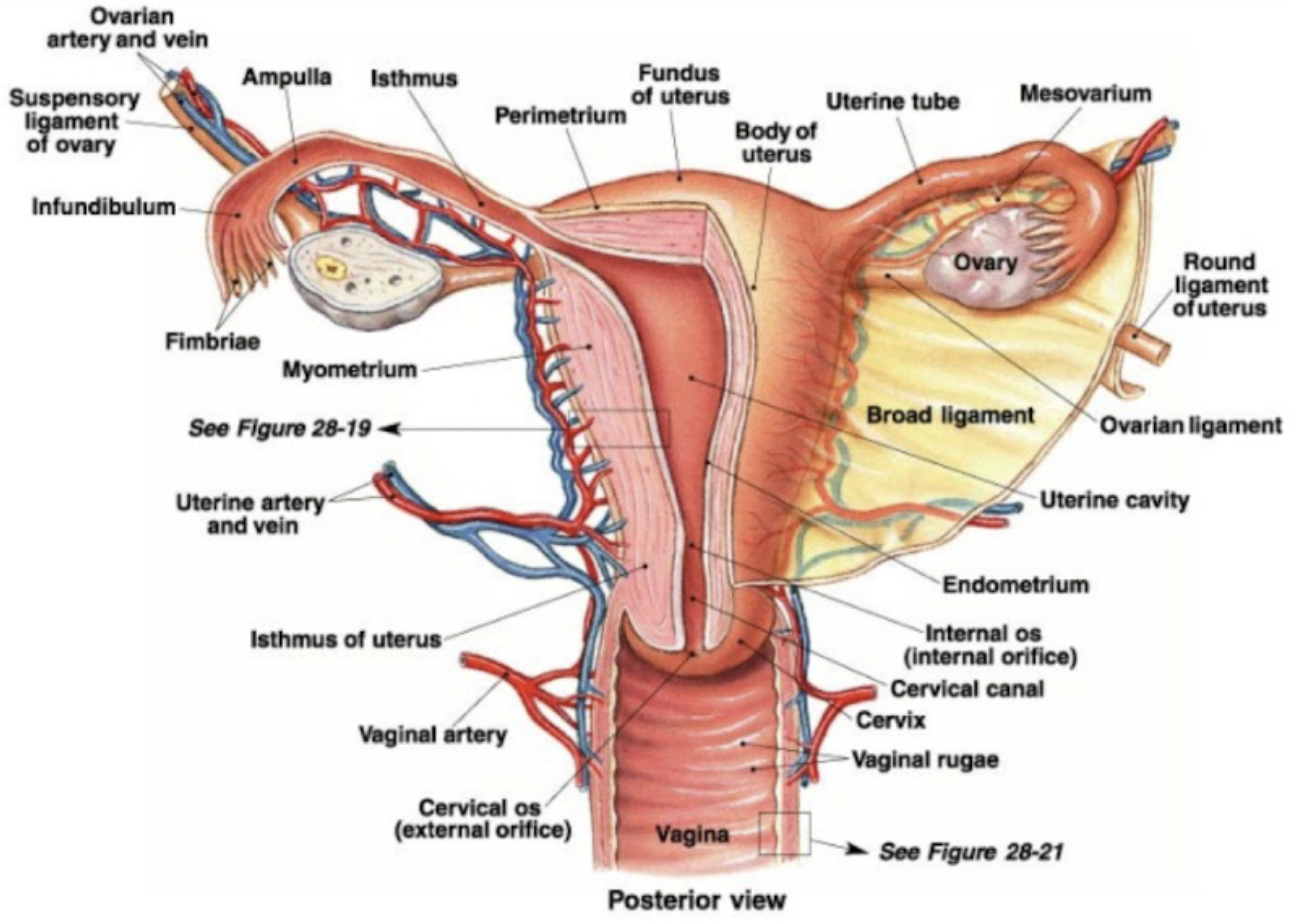
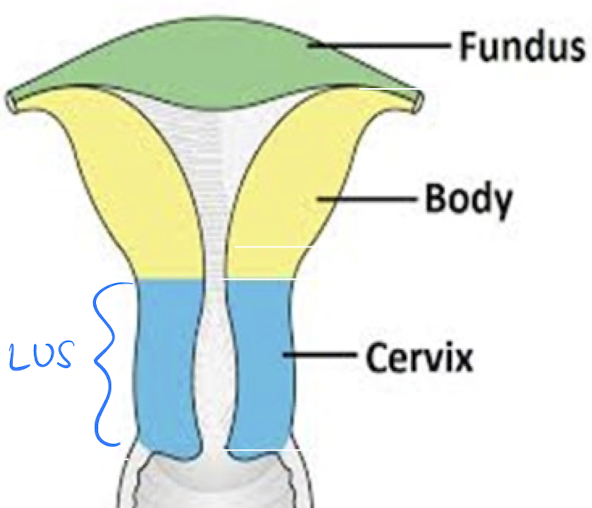
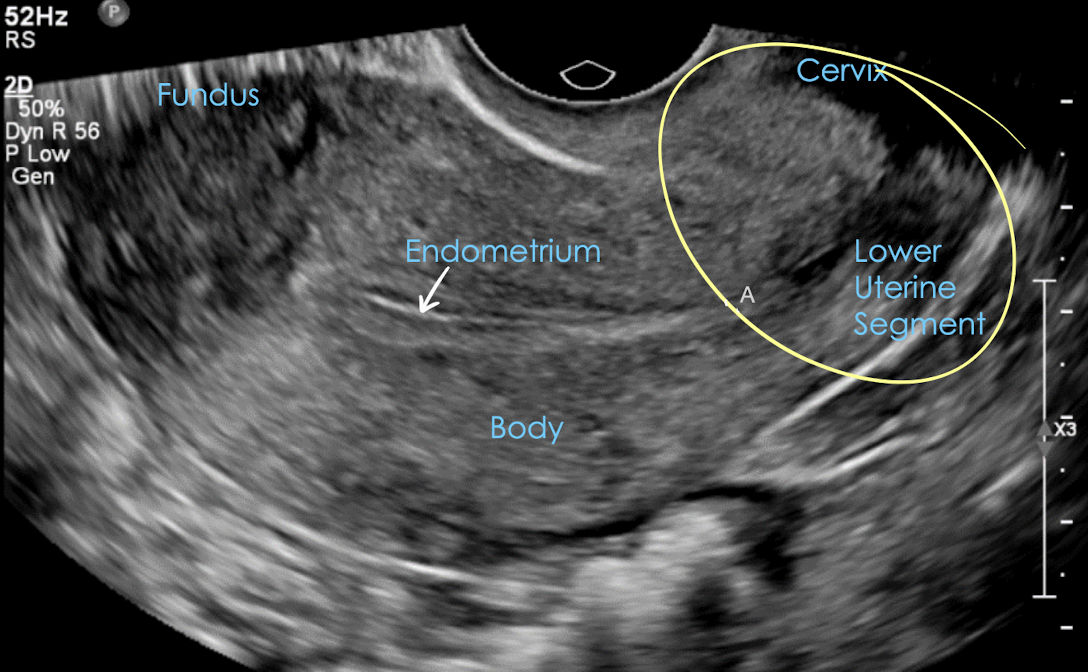
uterus anatomy
thick walled, pear-shaped, muscular organ
uterus must be able to stretch and flex to push baby out
3 major sections:
fundus
body
cervix
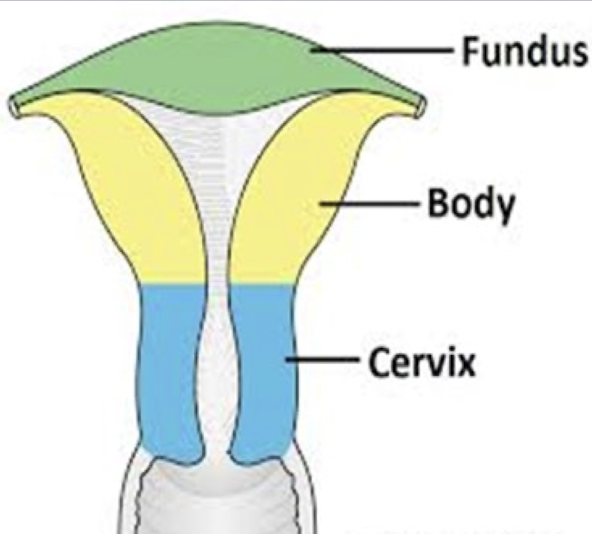
uterine fundus
widest, most superior portion
located above fallopian tubes
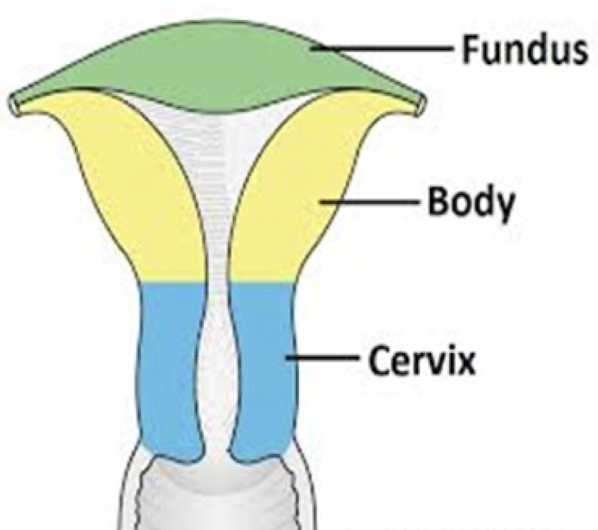
uterine body
aka corpus
main part of uterus
largest portion
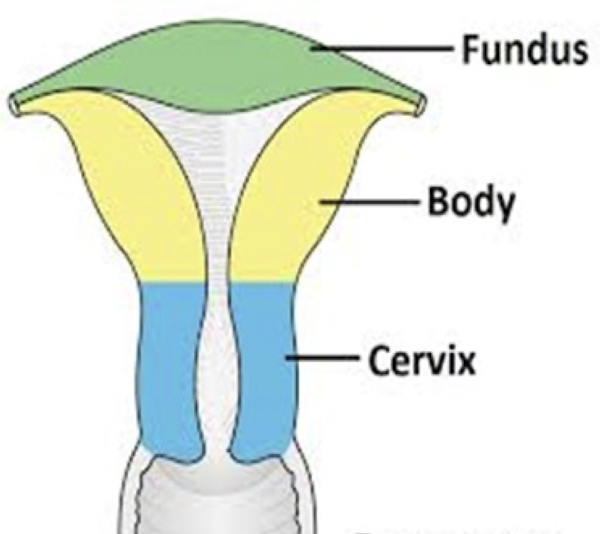
uterine cervix
1-inch long
projects into vagina
cylindrical and fibrous
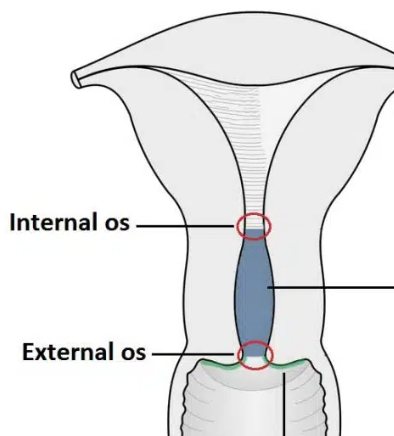
internos os
external os
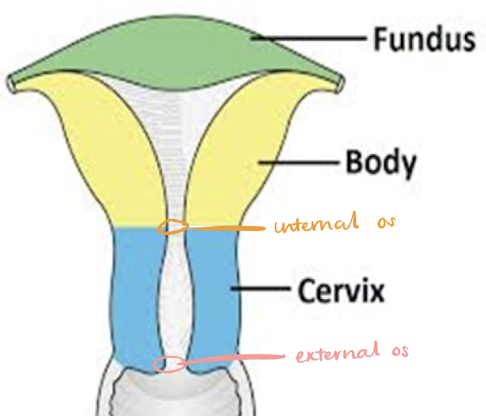
internal os
“os” = opening
junction of cervical canal and endometrial canal
“constricts upper end of cervix”
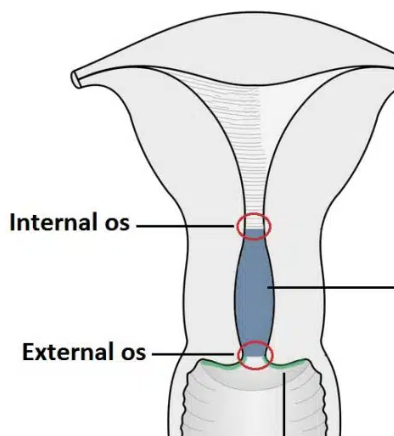
external os
“os” = opening
junction of cervical canal and vaginal canal (cervix to vagina)
“constricts lower end of cervix”
cornua
horn-shaped portion
where fallopian tube is attached to uterus
isthmus
narrow portion between uterine body and cervix
point where uterus bends anteriorly or posteriorly with an empty bladder
isthmus is the narrow region connecting the main uterine body to the cervix
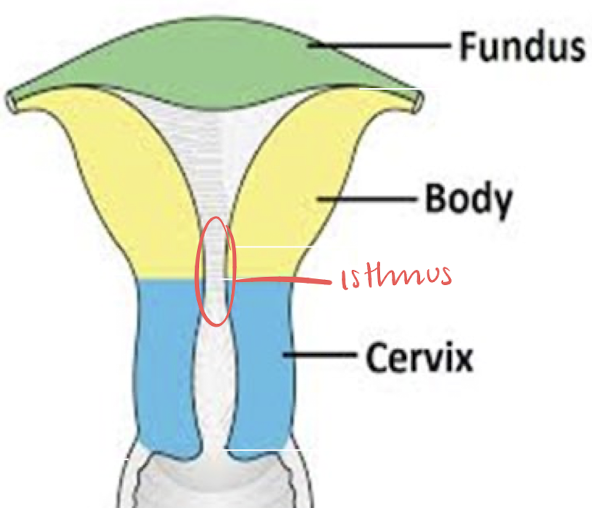
LUS
lower uterine segment (LUS)
lower portion of uterus
includes: internal os, cervical canal, and external os
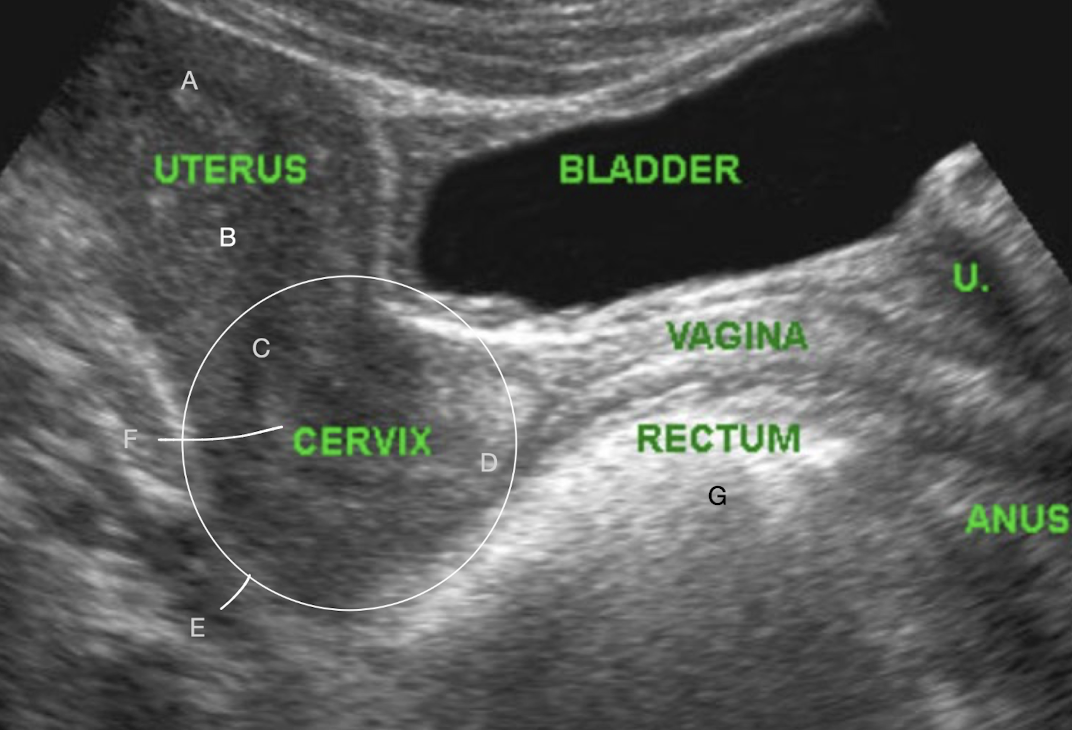
A?
fundus
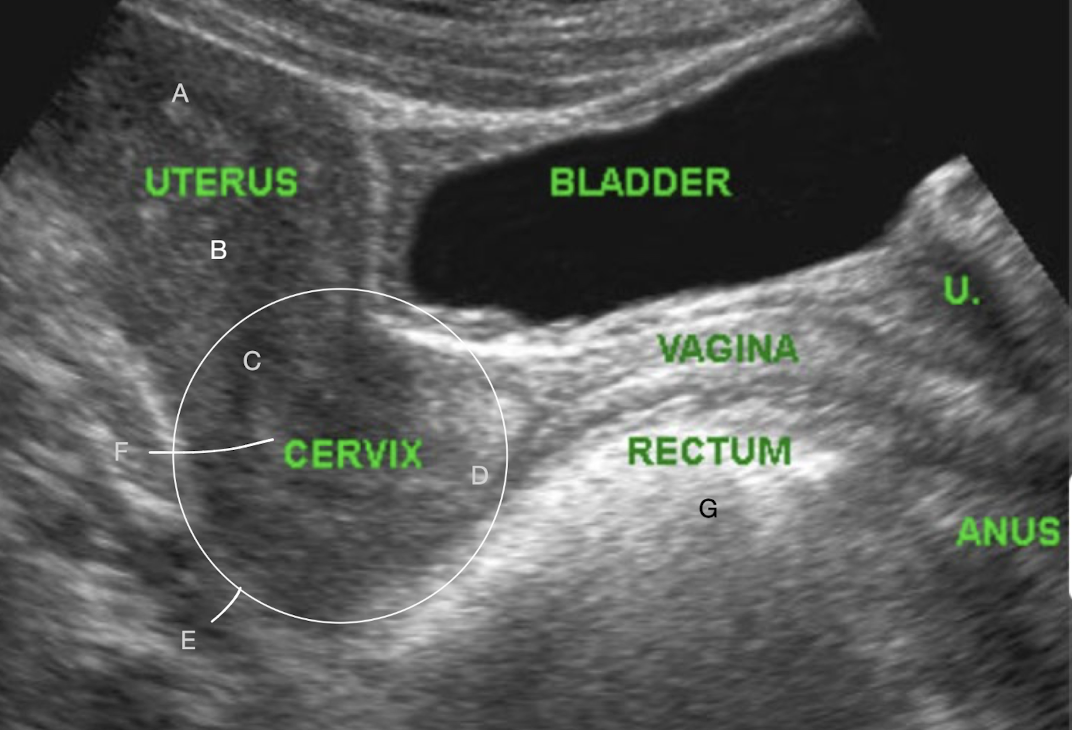
B?
body
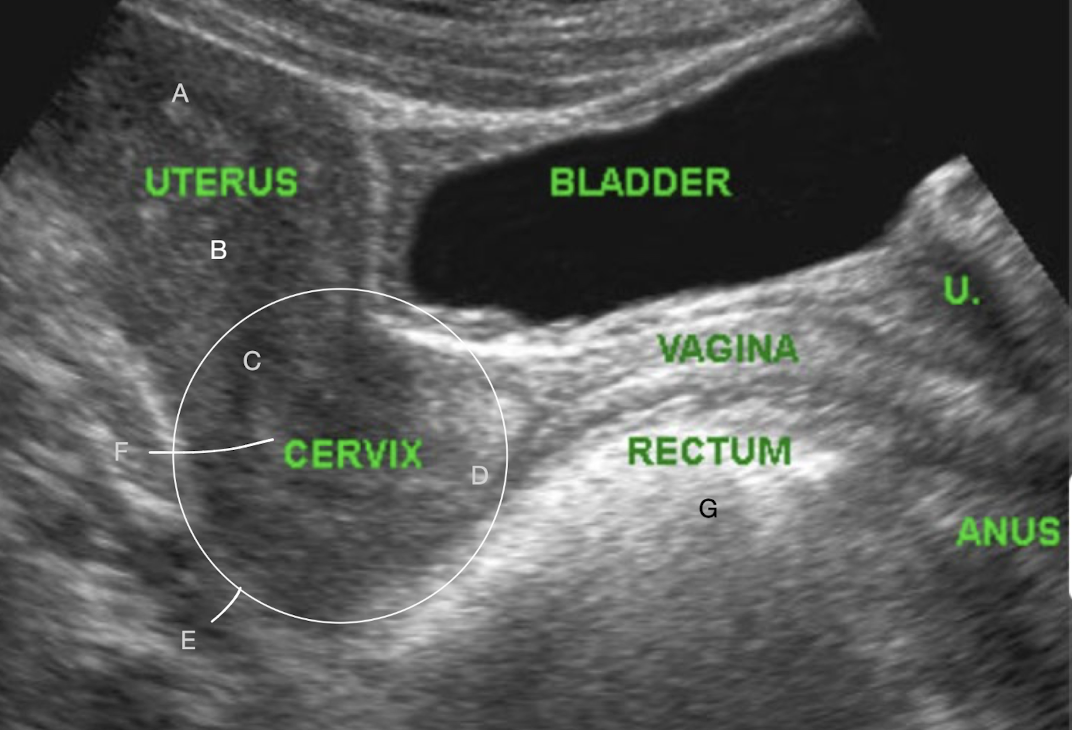
C?
internal os
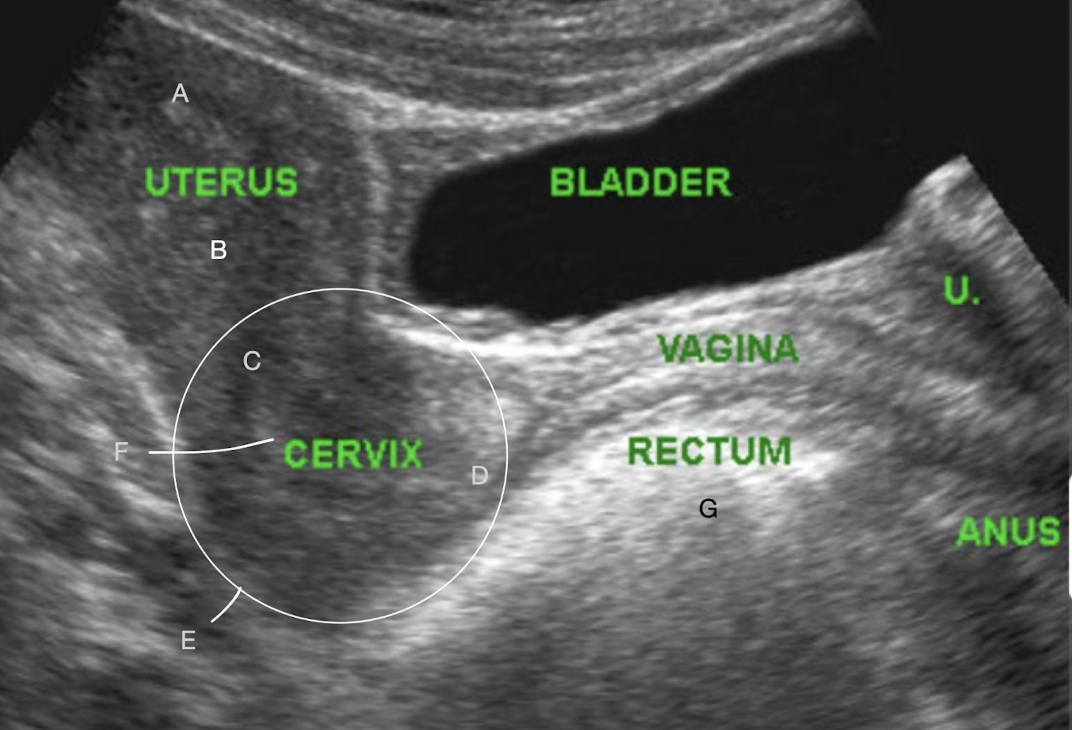
D?
external os
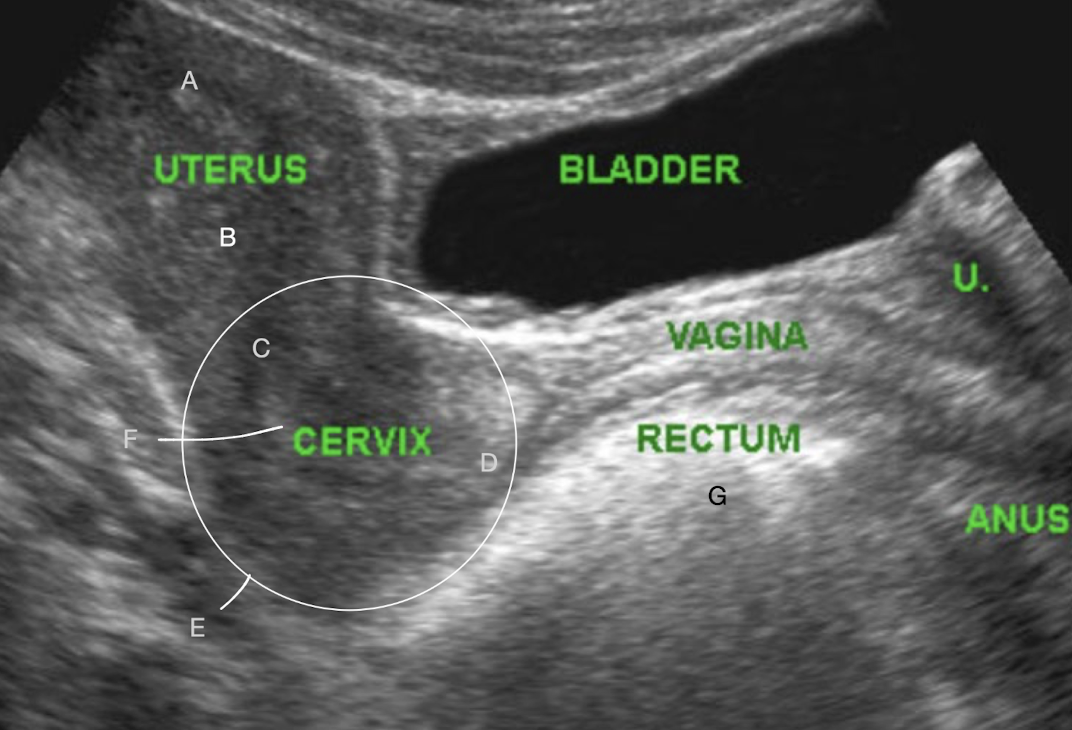
E?
LUS
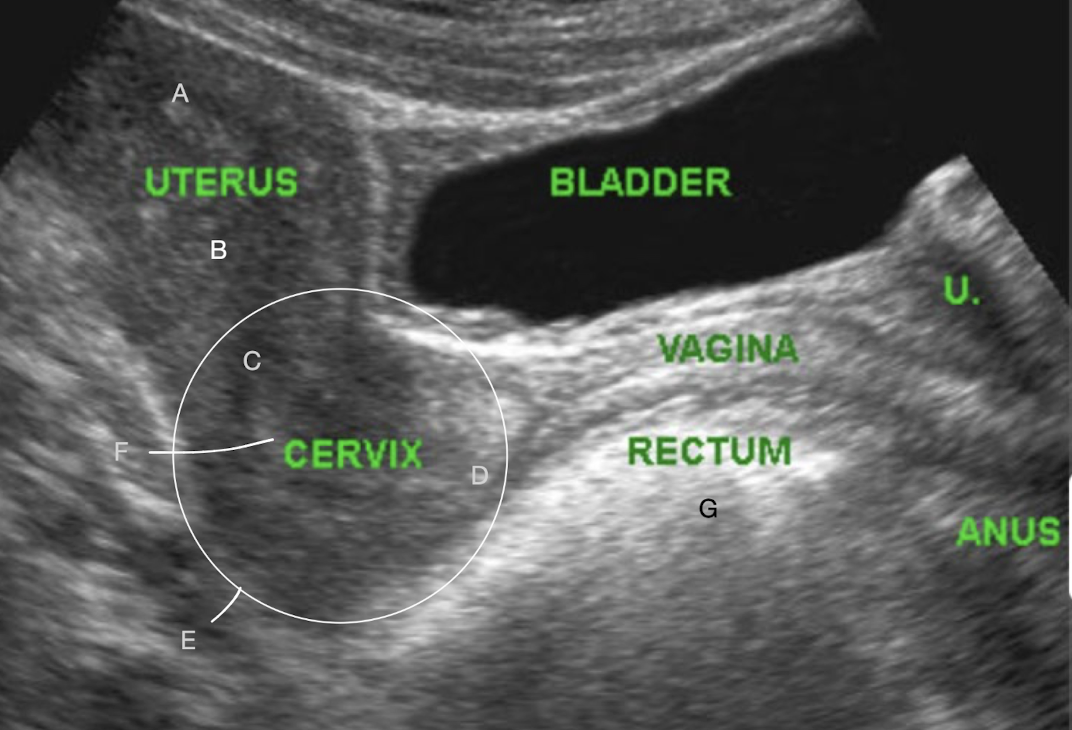
F?
cervical canal
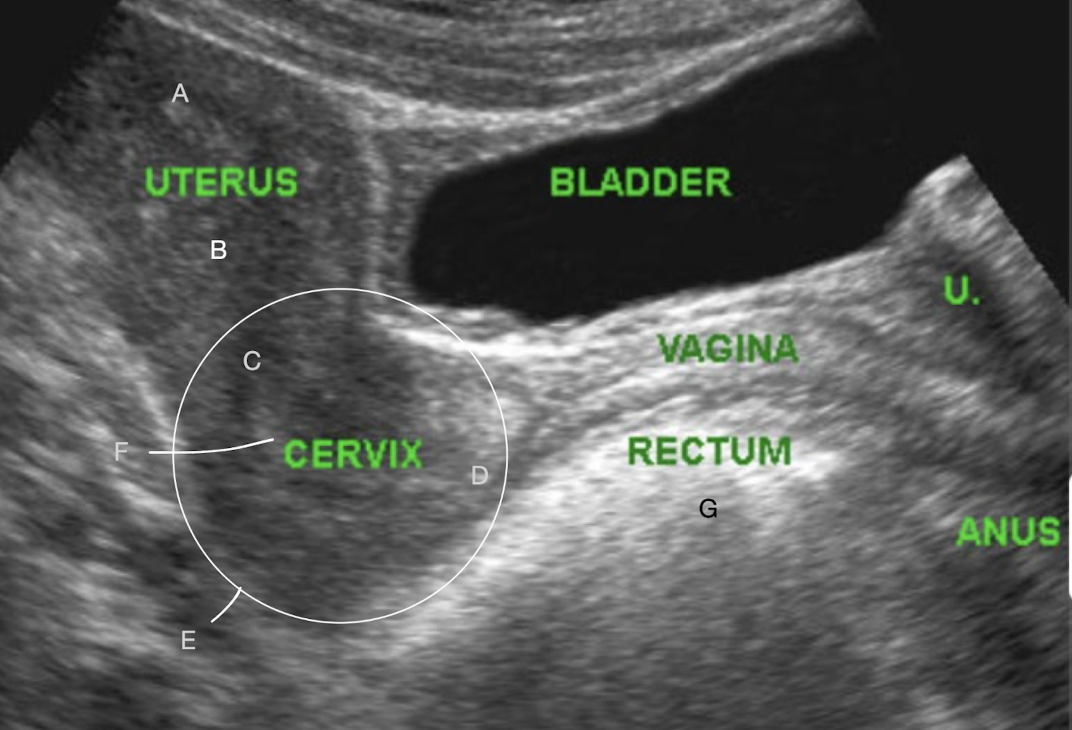
G?
bowel
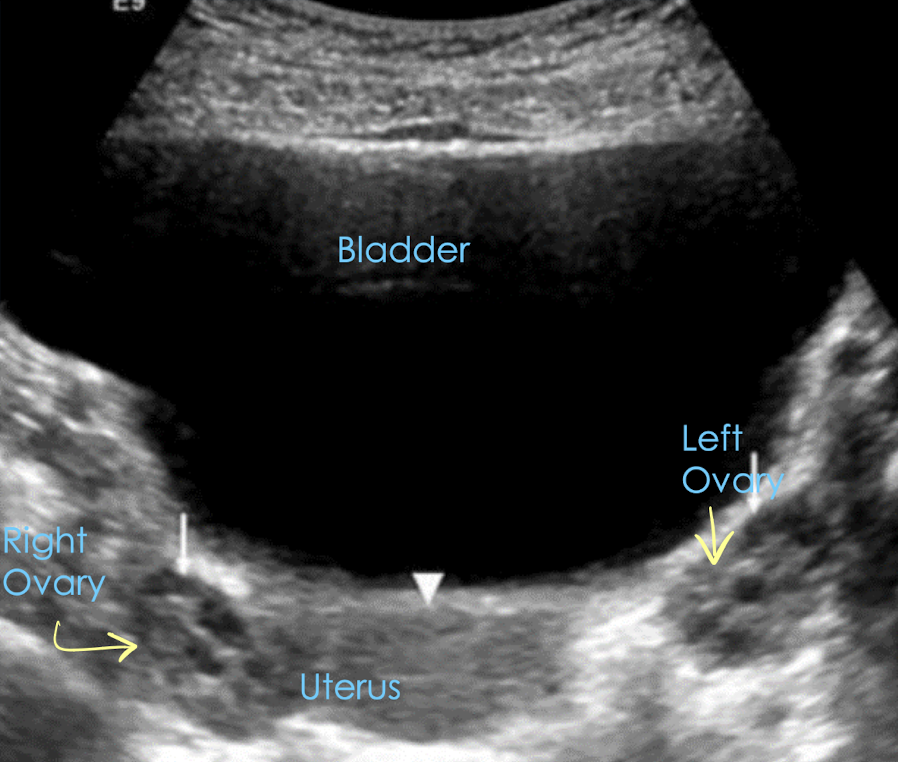
TA pelvic anatomy in TRANS
starting TRV is easiest way to find ovaries
A?
isthmus
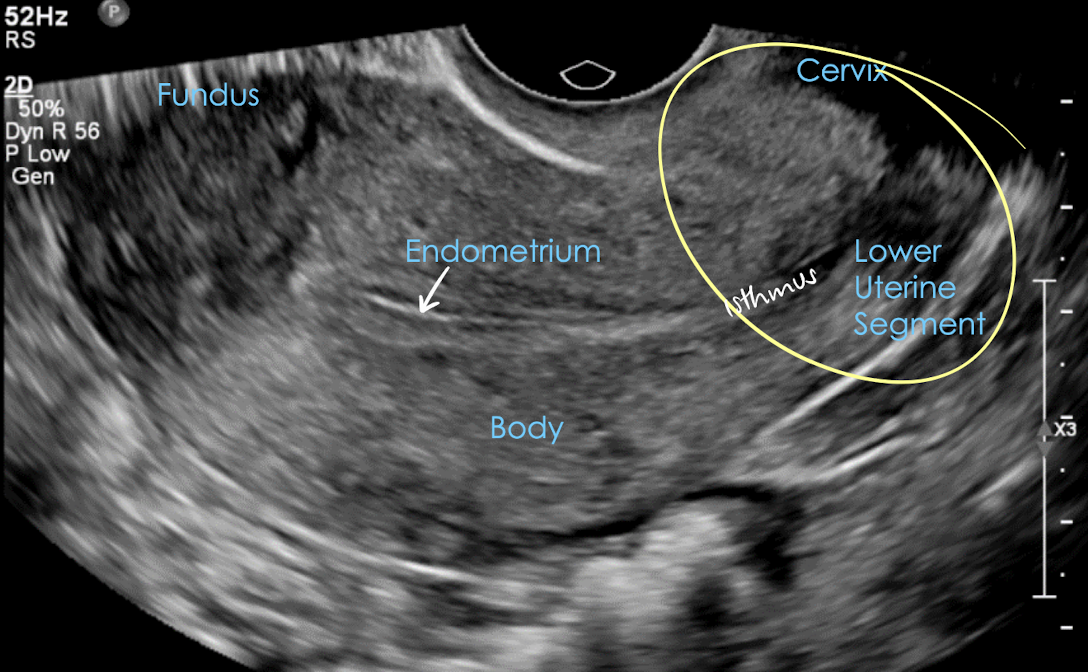
transvaginal pelvic anatomy in LONG
** patient must empty bladder
prepubertal (+ newborn) uterus size
length: 1-3 cm (2-4 cm)
width/AP: 0.5-1 cm
cervix/corpus ratio: 1:1 (2:1)
** newborns have bigger uterus and ovaries because of moms hormones
nulliparous uterus size
adult who has never been pregnant:
length: 6-8 cm
width/AP: 3-5 cm
cervix/corpus ratio: 1:2
parous uterus size
adult who has had a baby:
length: 8-10 cm
width/AP: 5-6 cm
cervix/corpus ratio: 1:2
postmenopausal uterus size
length: 3-5 cm
width/AP: 2-3 cm
cervix/corpus ratio: 1:1
is this uterus normal?
yes, for a normal adult
what is this image showing?
atrophic uterus in post-menopausal women
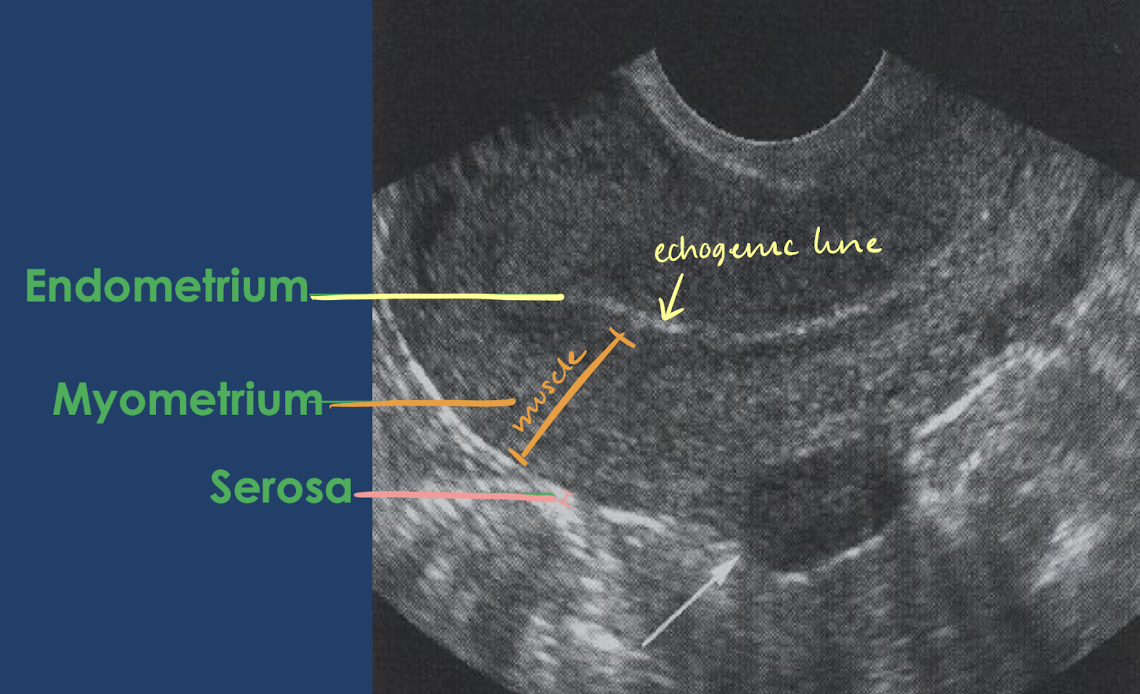
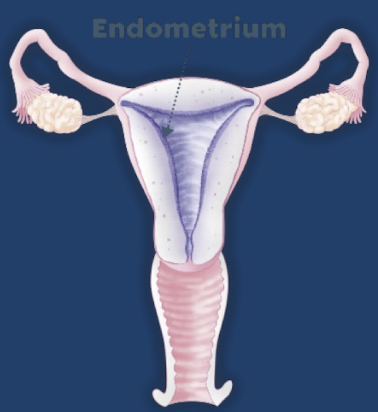
3 tissue layers of the uterus
perimetrium (serosa)
myometrium
endometrium
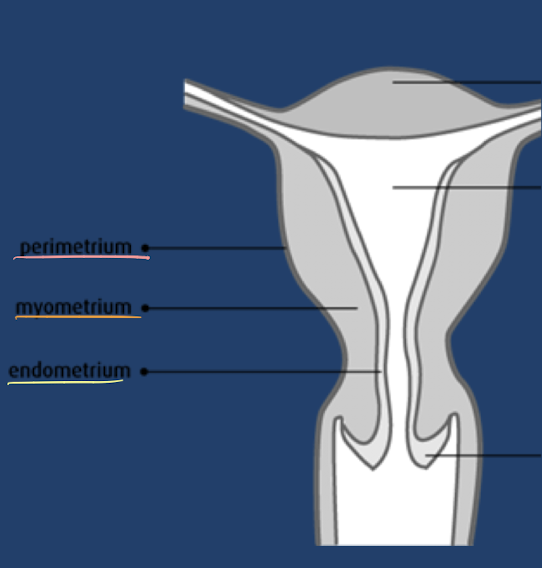
perimetrium (serosa)
thin, external layer
echogenic
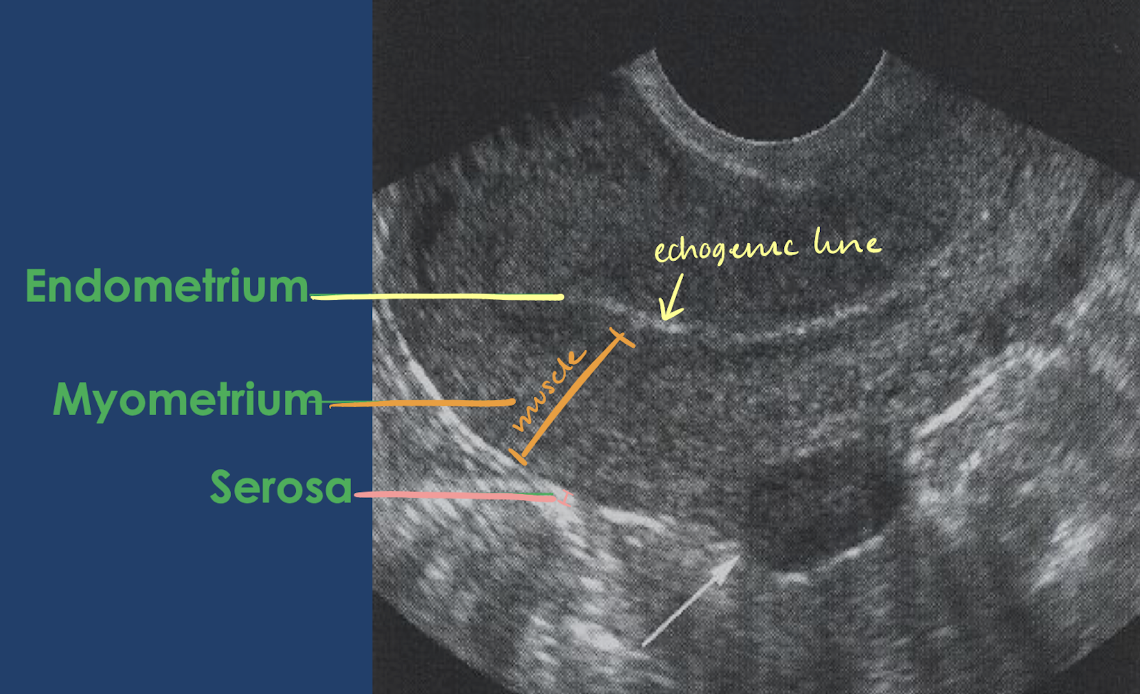
myometrium
middle, thickest layer
hypoechoic
made up of smooth muscle
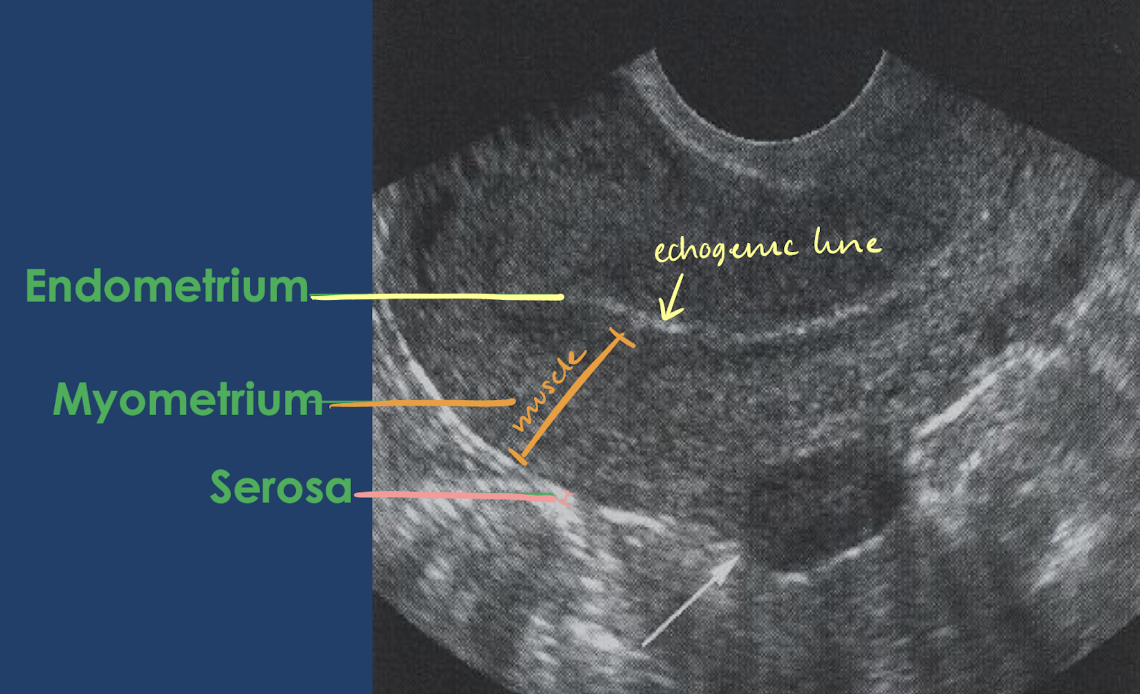
endometrium
innermost layer
thickness and appearance depends on menstruation cycle
echogenic-mildly hypoechoic
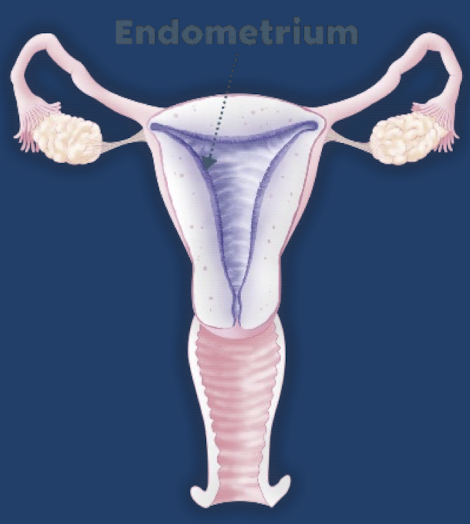
endometrium anatomy (layers)
superficial functional layer
deep basal layer
superficial functional layer
innermost layer of endometrium
sheds during menses
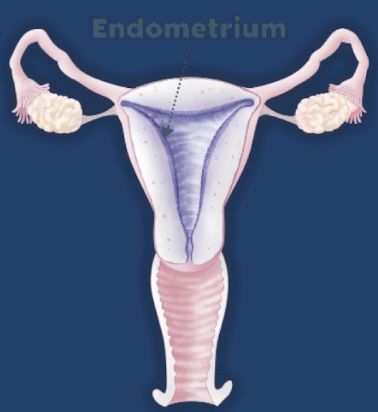
deep basal layer
layer of endometrium
regenerates new endometrial tissues after menses
very vascular
normal uterus and endometrium values
uterus: 6-8 cm nulliparous; 8-10 cm multiparous
endometrium: <14 mm (less than 1.4 cm)
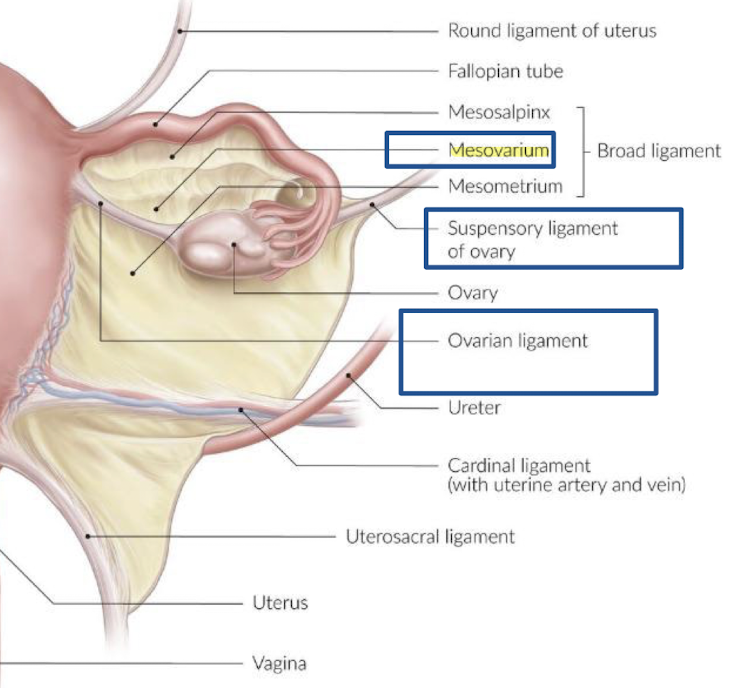
uterine ligaments
ligaments attach bone to bone or organ to organ
uterus is supported in its midline position by:
broad ligaments
round ligaments
cardinal ligaments
uterosacral ligaments
broad ligaments
double fold of peritoneum that drapes over uterus, fallopian tubes, and ovaries
lateral side of uterus to sidewall of pelvis
3 portions:
mesosalpinx
mesovarium
mesometrium
“broad fold of peritoneum draped over the fallopian tubes, uterus, and ovaries; extends from sides of uterus to side walls of the pelvis; divided into 3 portions—mesosalpinx, mesovarium, and mesometrium”
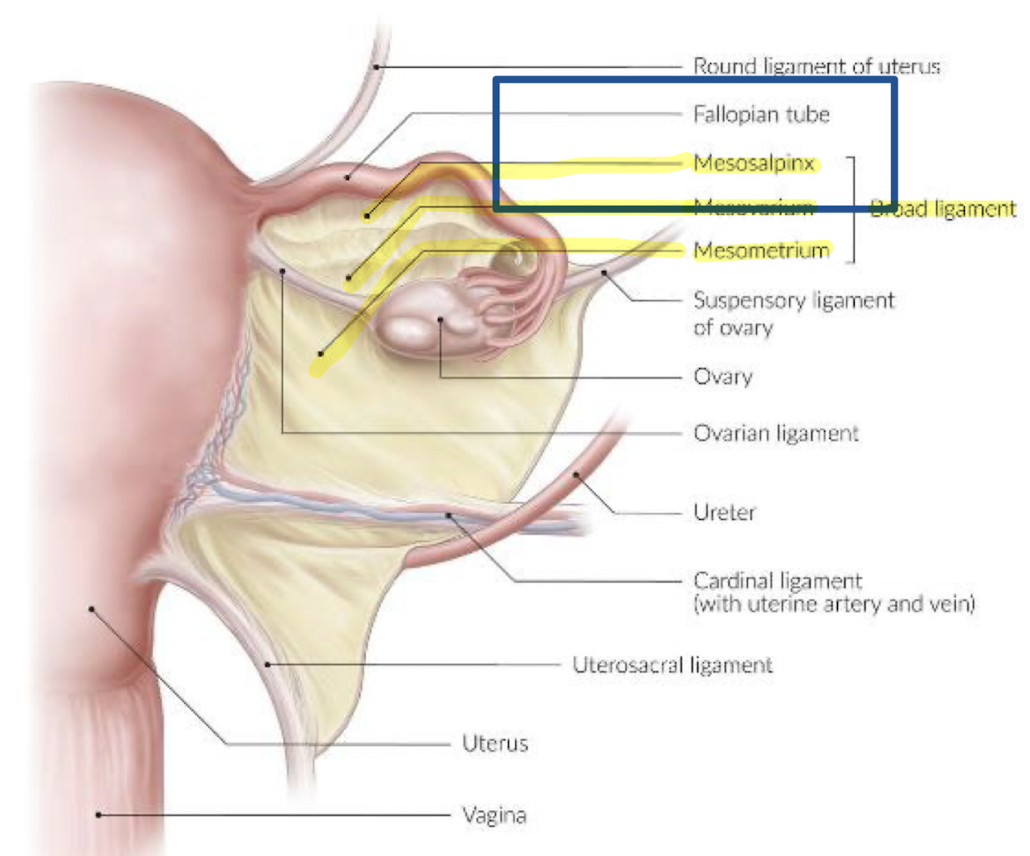
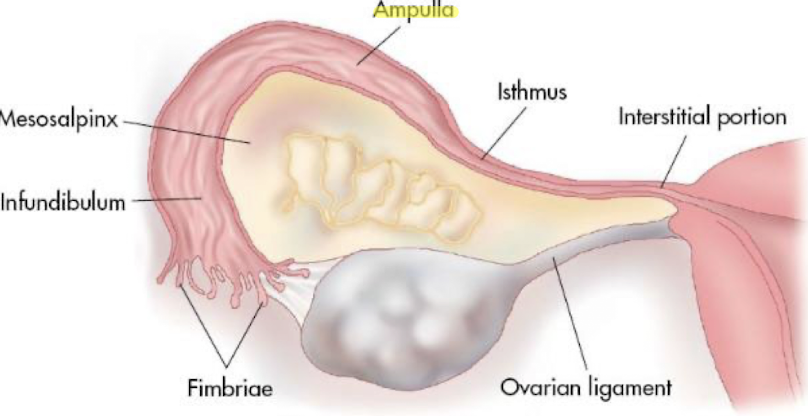
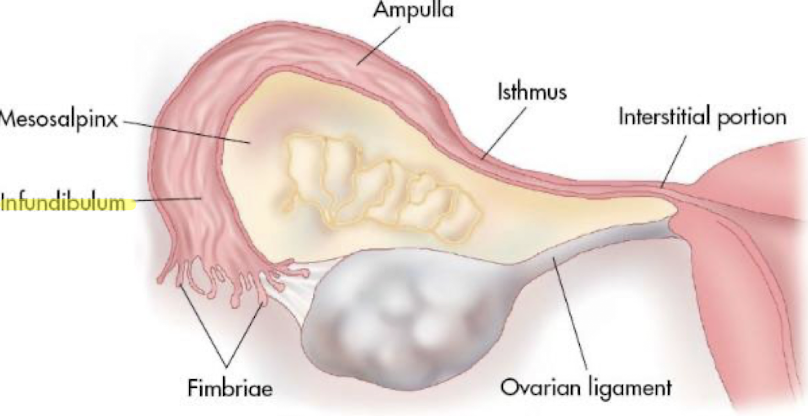
mesosalpinx
upper fold that drapes over fallopian tubes
“upper portion of broad ligament that encloses fallopian tubes”
** -salpinx=fallopian tubes
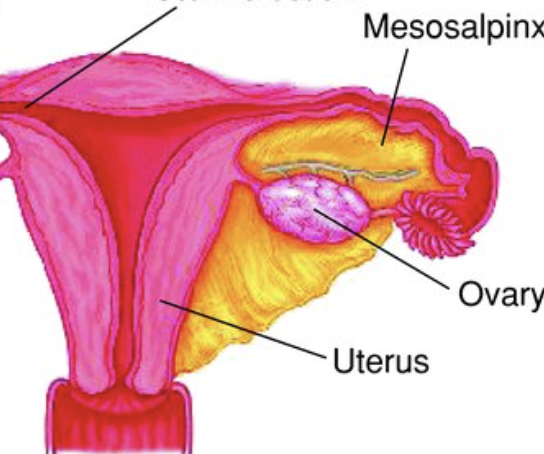
mesovarium
posterior portion that attaches to ovary
“posterior portion of broad ligament that enclose and hold the ovary in place”
** -ovarium=ovary
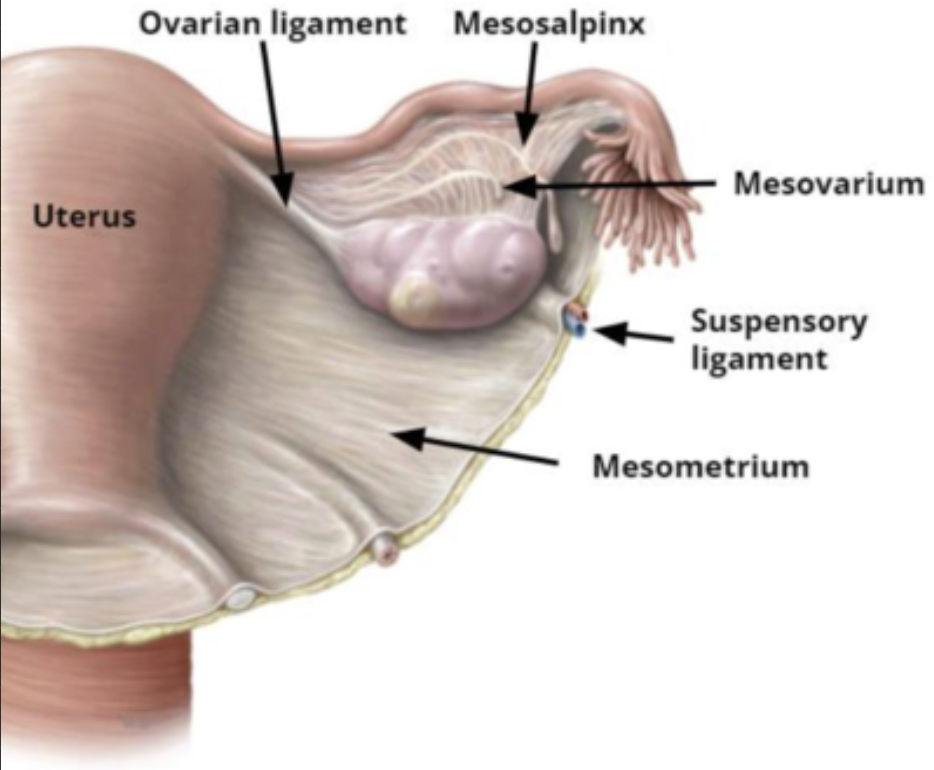
mesometrium
medial portion that drapes over uterus
** -metrium=uterus
which ligament is represented by green? red? yellow?
green=mesosalpinx
red=mesovarium
yellow=mesometrium
round ligaments
fibrous cords between layers of broad ligaments
cord on each side of superior aspect of uterus; courses upward and lateral to inguinal canal, inserting into labia majora
stabilizes uterine fundus and body in forward position
provides anterior support to uterus
“paired ligaments that originate at uterine cornua, anterior to fallopian tubes, and course anterolaterally within broad ligament to inert into the fascia of the labia majora; hold the uterus forward in its anteverted position”
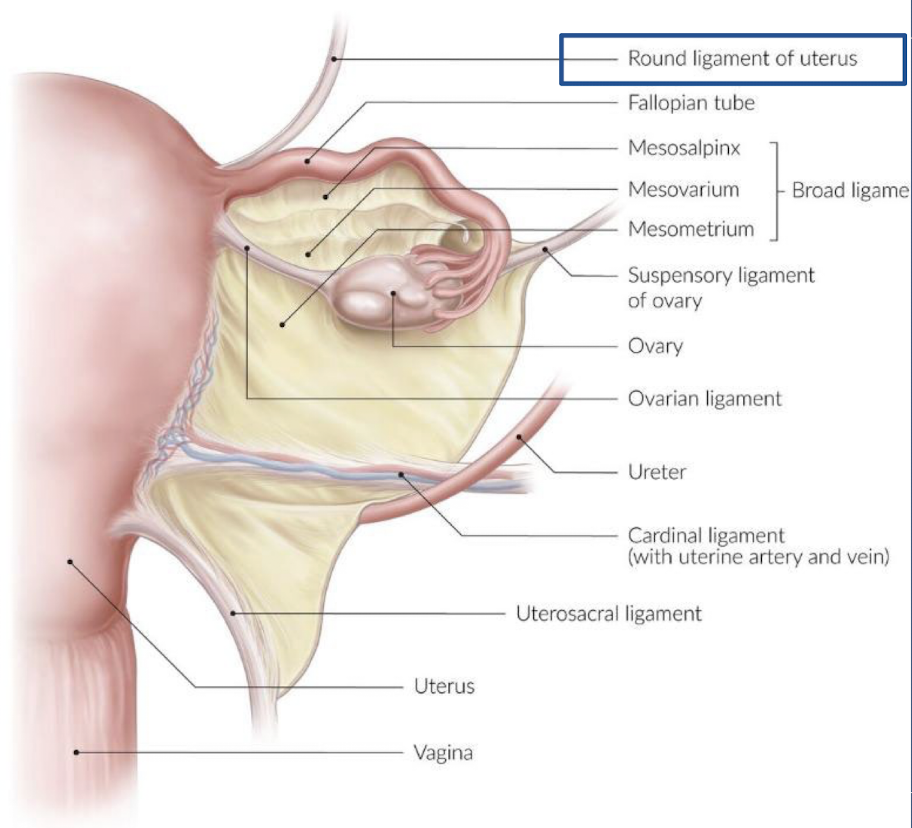
cardinal ligaments
one of the two ligaments that anchor the cervix (only portion of uterus that is fixed/firmly supported)
continuation of broad ligament
extend across lateral pelvic floor
“wide bands of fibromuscular tissue arising from lateral aspects of cervix and inserting along lateral pelvic floor; a continuation of the broad ligament that provides rigid support for the cervix”
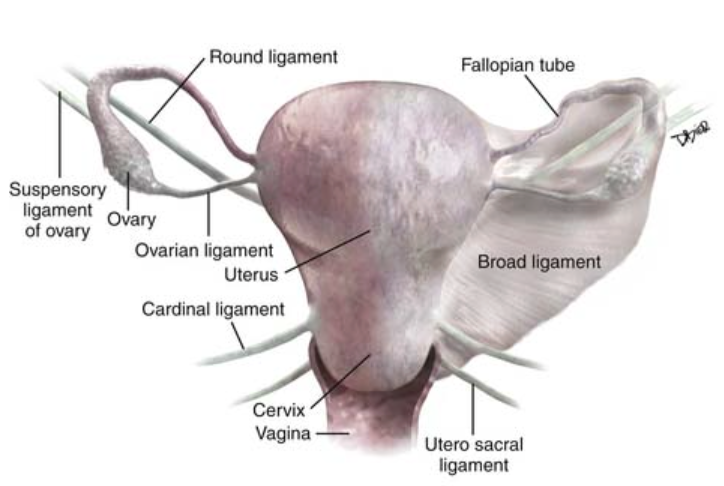
uterosacral ligaments
one of the two ligaments that anchor the cervix (only portion of uterus that is fixed/firmly supported)
attached at uterine isthmus
extends posterolaterally from cervix and insert over sacrum
“posterior portion of cardinal ligaments that extends from cervix to sacrum”
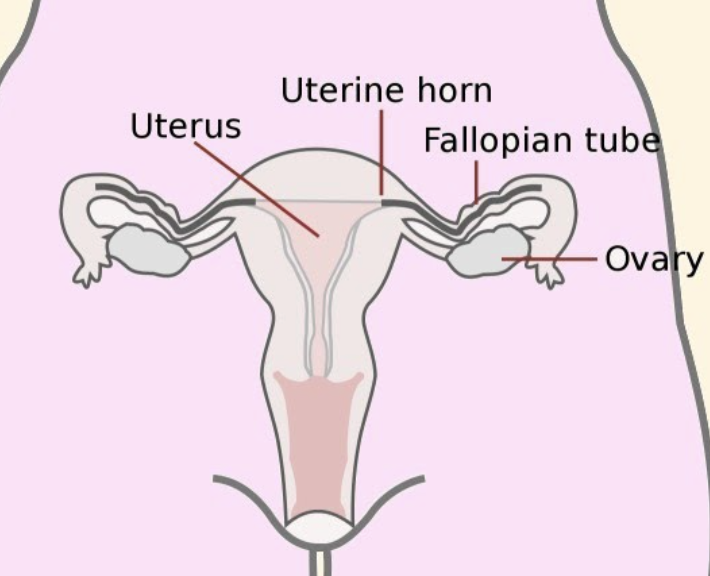
fallopian tubes
aka salpinx
paired, muscular tubes that extend from cornua laterally to fimbriae
10-12 cm in length
1-4 mm in diameter
3 layers:
serosa (outermost)
muscular (middle)
mucosal (innermost)
what is the middle layer of the fallopian tube called?
muscular
what is the innermost layer of the fallopian tube called?
mucosal
4 segments of the fallopian tubes
interstitial
isthmus
ampulla
infundibulum
fallopian tubes: interstitial portion
comes right off uterus
proximal portion that passes through uterine wall
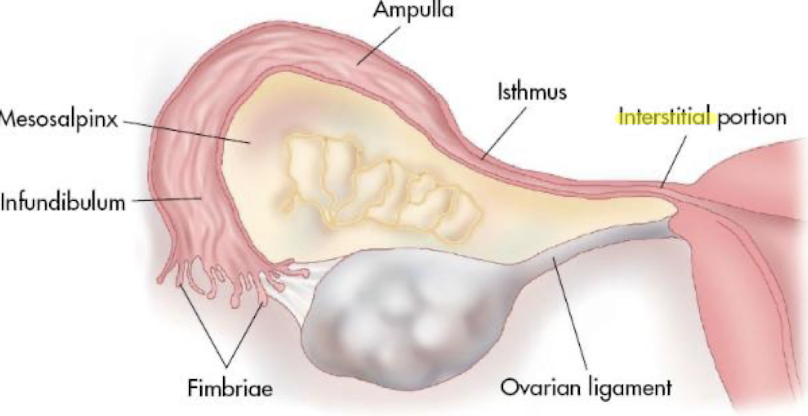
fallopian tubes: isthmus
medial (middle) segment after interstitial portion of uterus
longer than interstitial portion
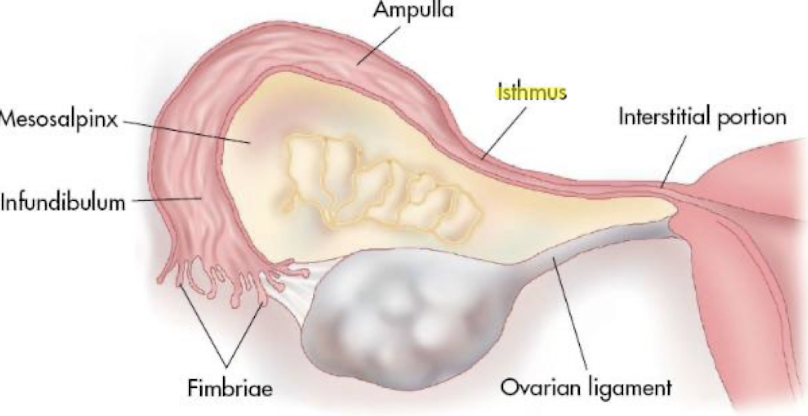
fallopian tubes: ampulla
longest segment
typical site of fertilization
fallopian tubes: infundibulum
widest portion of tube
contains fimbriae—fingerlike projections at end of tube that empties into peritoneal cavity
SONO: fallopian tubes
usually not seen unless significantly distended (from fluid, pus, blood)
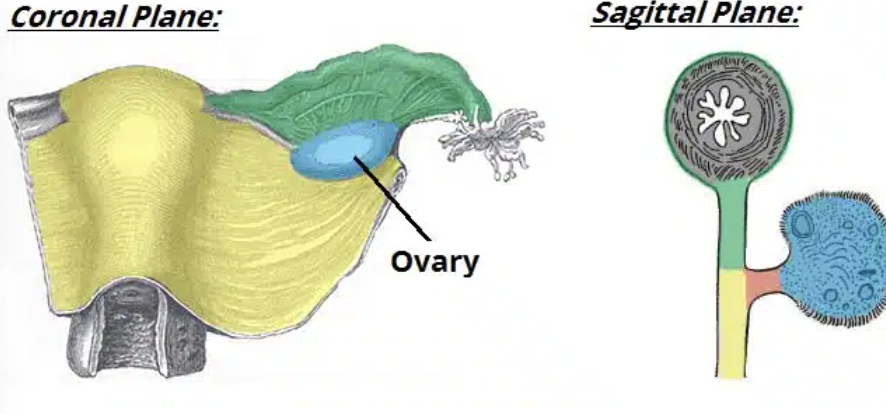
normal ovarian anatomy
ovaries:
paired, ovoid/almond-shaped organs
suspended in the pelvis by mesovarium
located medial to external iliac vessels and anterior to internal iliac vessels
consists of outer layer (cortex) that surrounds central medulla
cortex: contains mostly follicles
medulla: contains connective tissue, lymphatic vessels, nerves and blood
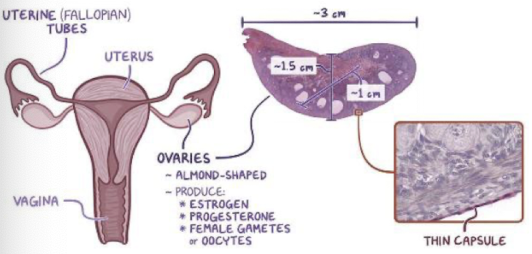
ovaries produce what cells and hormones?
produce reproductive cells (ovums)
2 hormones:
estrogen (secreted by follicles)
progesterone (secreted by corpus luteum)
normal ovarian measurements
ovary measures 3-4 cm with volume between 4-6 mL
ovarian follicles are normally visible
dominant follicle (aka Graafian cyst) develops prior to ovulation and measurements ≤ 3 cm
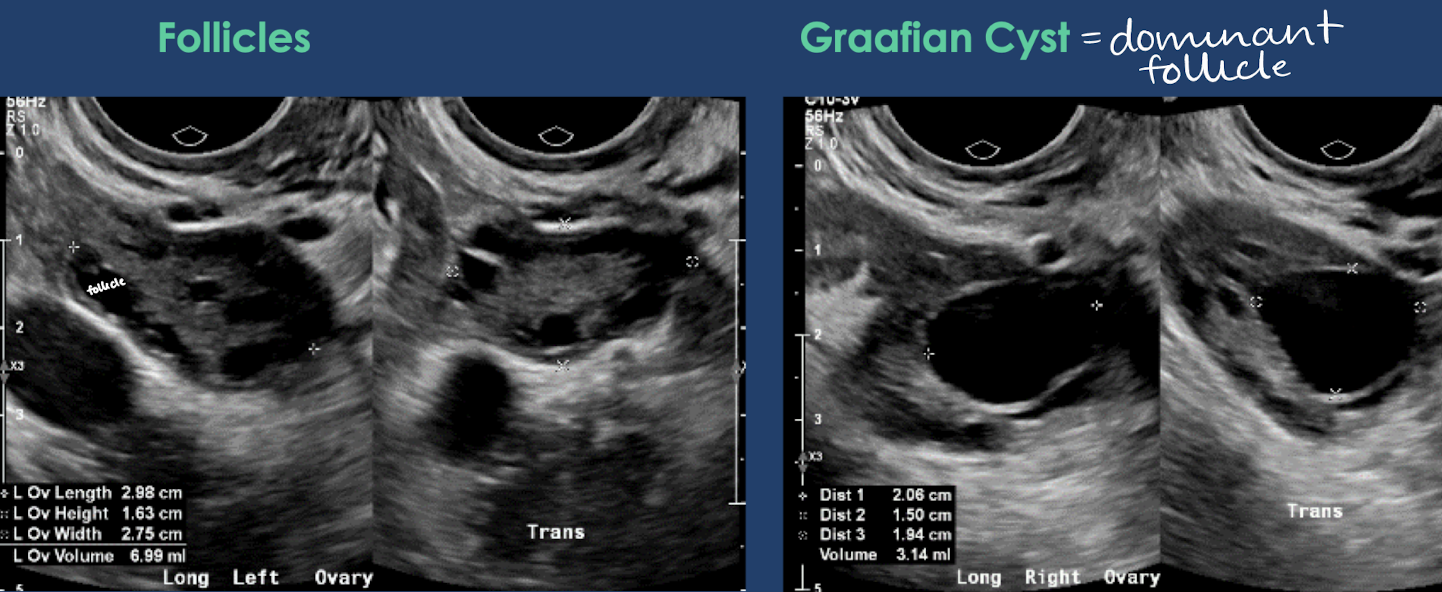
ovary size
premenarch (before puberty)
volume: <2 mL
menstrual age
length: 2.5-5.0 cm
width: 1.5-3.0 cm
height: 0.6-2.2 cm
postmenopausal
volume: 3-6 mL
what is the normal L x W x H for menstrual age ovary size?
length: 2.5-5 cm
width: 1.5-3 cm
height: 0.6-2.2 cm
ovarian ligaments
ovarian ligament
suspensory (infundibulopelvic) ligament
mesovarium (broad ligament)
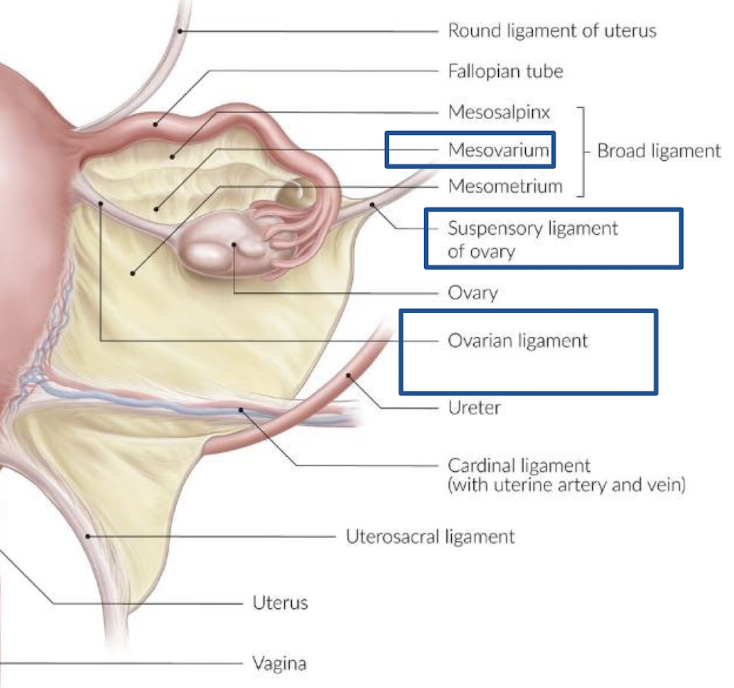
ovarian ligament
originate bilaterally at cornua of uterus
supports ovary medially
“paired ligament that extends from inferior/medial pole of ovary to the uterine cornua”
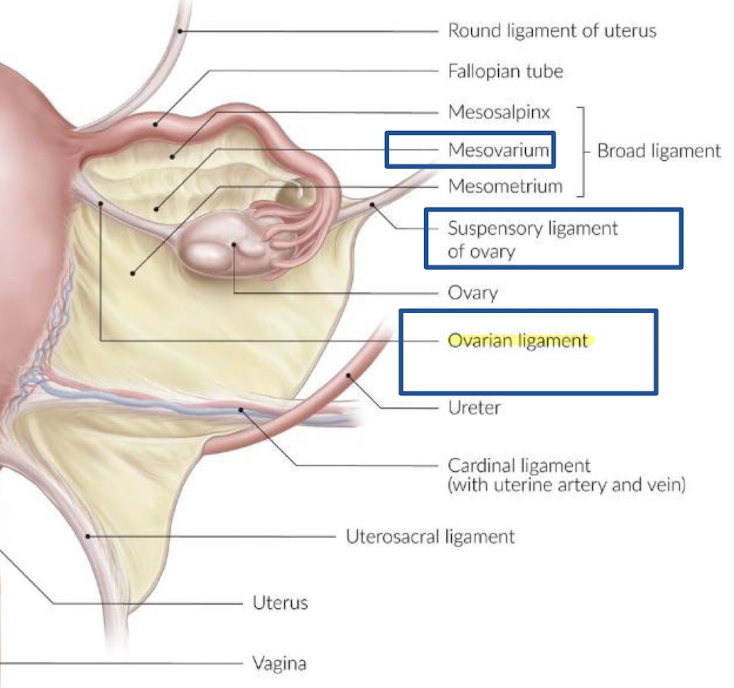
suspensory ligament
extends from infundibulum of fallopian tube and ovary to sidewall of pelvis
supports ovary laterally
“paired ligaments that extend from infundibulum of fallopian tube and lateral aspect of ovary to lateral pelvic wall”
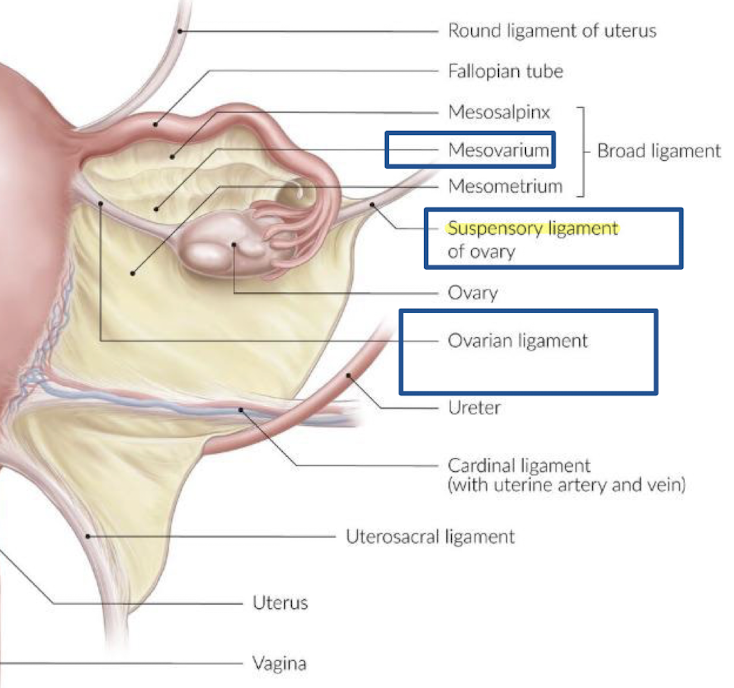
mesovarium
attaches ovary to posterior aspect of broad ligament
common iliac arteries
courses anterior and medial to psoas muscles
provides blood to lower extremities and pelvic cavity
bifurcates into external and internal iliacs
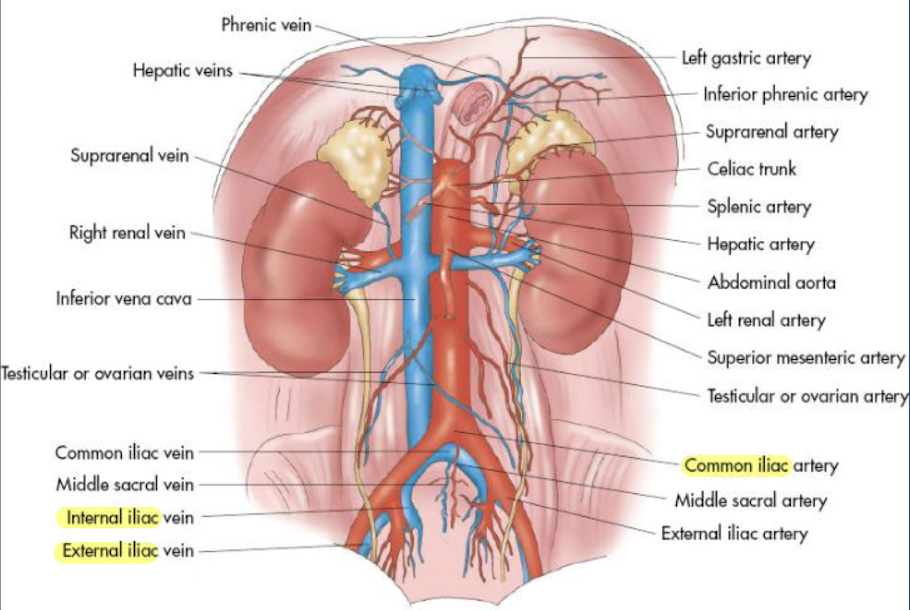
external iliacs
course along pelvic brim and continue inferiorly as common femoral arteries
internal iliacs
extend into pelvic cavity
multiple branches that perfuse pelvic structures: like bladder, uterus, vagina, and rectum
branches into uterine artery and vaginal artery
what branches off the internal iliac artery?
uterine artery
vaginal artery
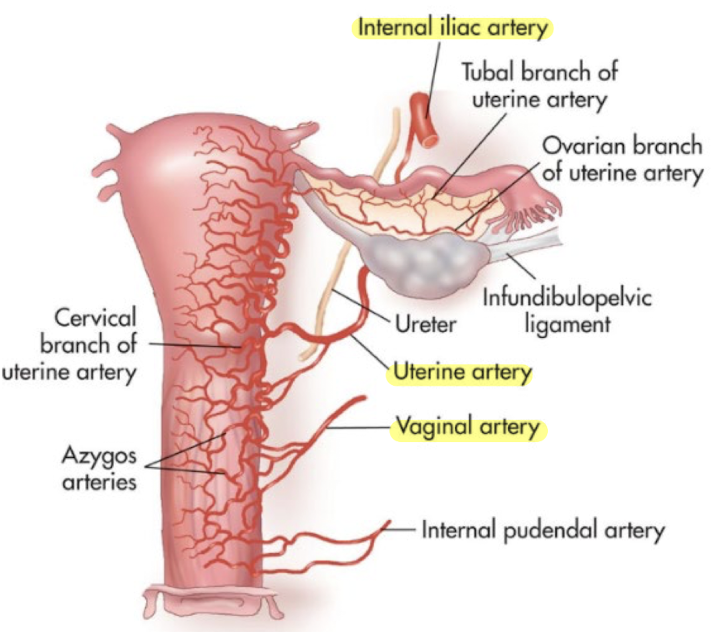
uterine artery
supplies the uterus
courses above and anterior to the ureter, extending medially in the base of the broad ligament to the uterus at the level of the cervix