Autism Spectrum Disorder
1/25
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
26 Terms
Prevalence
•Neurodevelopmental disorder with a prevalence of 1 in every 31 children being diagnosed with ASD at age 8 in 2022 (CDC, 2025)
•3 times more common in boys than girls
•Earliest diagnosis by 18 months of age although commonly age 4 and over
•Spectrum disorder with wide variation in skill levels of individuals
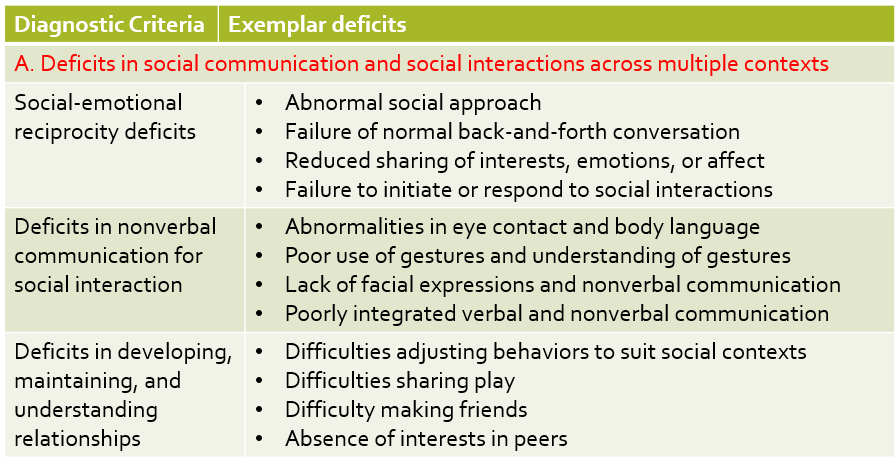
Diagnostic Criteria: DSM 5 Social
Deficits in social communication and social interactions across multiple contexts
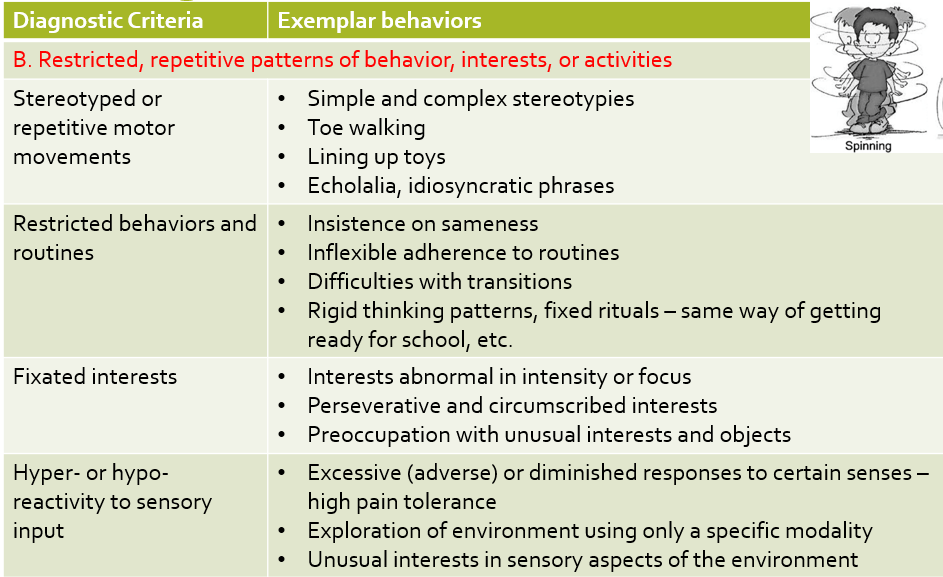
Diagnostic Criteria: DSM 5 Behavior Restrictions
Restricted, repetitive patterns of behavior, interests, or activities
Diagnostic Criteria for ASD: DSM 5
•Symptoms present in early development (may become manifest only when social demands exceed limited capacities) – some children mask by learned strategies
•Clinically significant impairment in social, occupational, and other areas of functioning
•Not explained by intellectual disability or global developmental delay
Specifiers –
•With or without accompanying intellectual impairment
•With or without accompanying language impairment
•Associated with a known medial or genetic condition or environmental factor
•Associated with other neurodevelopmental, mental, or behavioral disorders
•With catatonia
Marked deficits in social communication but do not meet criteria of ASD – social communication (pragmatic) disorder
Three Functional Levels
ASD Level 1: Requiring Support. Difficulty initiating social interactions, organization, and planning problems can hamper independence
ASD Level 2: Requiring Substantial Support. Social interactions limited to narrow special interests, frequent restricted/repetitive behaviors.
ASD Level 3 Requiring Very Substantial Support. Severe deficits in verbal and nonverbal social communication and skills, great distress, difficulty changing actions or focus
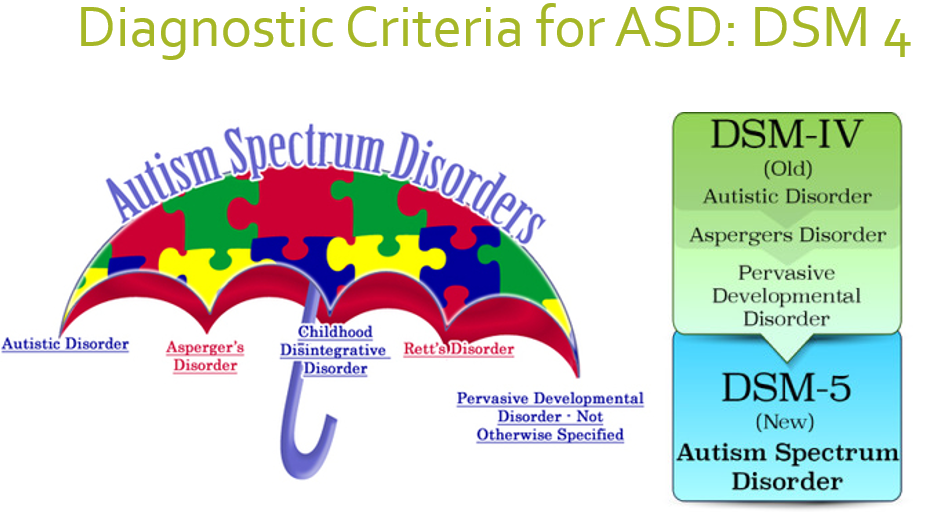
Diagnostic Criteria for ASD: DSM4
Etiology
No single known cause – but neuropathology of ASD begins in prenatal or perinatal period
Combination of genetic and environmental factors
Genetic component
Increased risk in families
Twin studies – identical twin also having ASD – 31-95% greater risk
Siblings of children with ASD – 25-50% chance of some delays - ~20% ASD, ~30% Broader Autism Phenotype (social, language, motor delays, unusual sensory interests)
Other populations at risk for ASD: Premature infants, children born to older parents, exposure to prescription medications like valproic acid and thalidomide
Associated genetic disorders: Fragile X, Tuberous Sclerosis, Down syndrome, Angelman, etc.
Specific environmental factors have not been identified
Brain Pathology 1
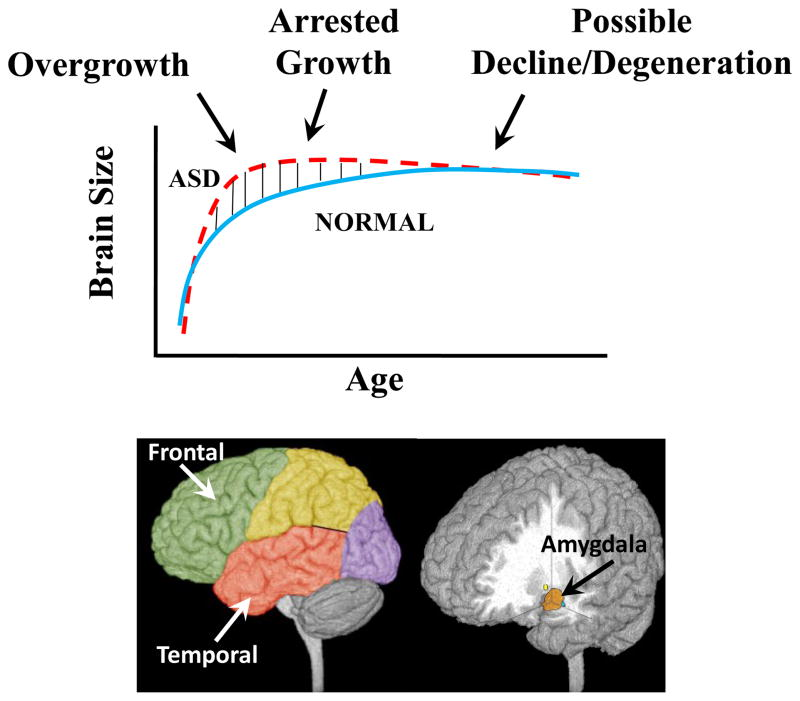
Early overgrowth followed by arrested development and early degeneration from adolescence to middle ages
Brain Pathology 2
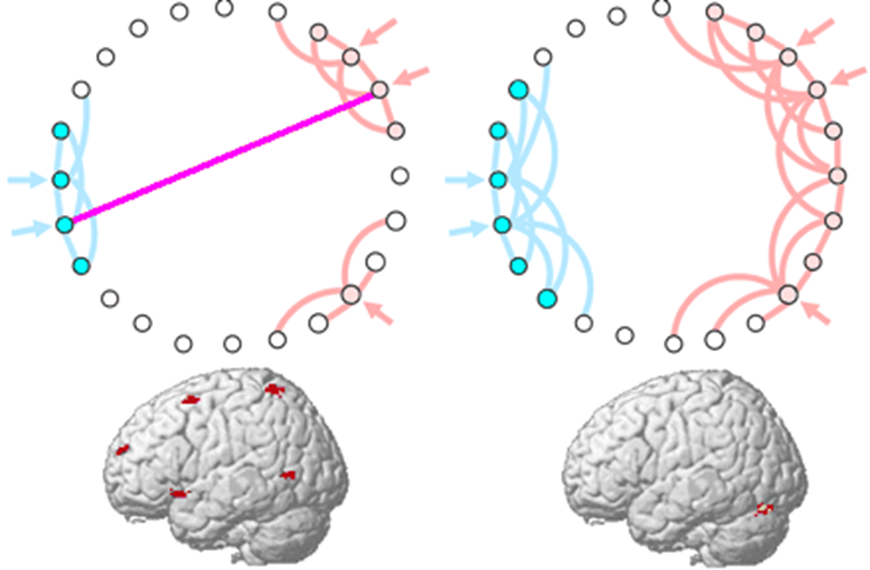
Long-distance under-connectivity and short-distance over-connectivity – poor integration of sensorimotor, social communication and cognitive functions
Brain Pathology Continued
•Cortex: Frontal and temporal lobes – planning, executive function, social communication skills
•Amygdala: Emotional processing
•Hippocampus: Learning and memory
•Basal ganglia and cerebellum: Coordination, clumsy gait, motor learning
•Mirror Neuron system deficits: Problems with imitation and empathy
Impairments Part 1 Social
Social and attentional – difficulties with eye contact, turn taking, joint attention, delayed response to name, attention more on non-social cues, difficulty disengaging attention
Communication –
Poor pragmatic language skills (use of nonverbal cues to communicate: eye gaze, facial expressions, body language),
Poor prosody (rhythm, stress, intonation)
Poor phonology (Word articulation)
Atypical language – echolalia (immediate or delayed imitation of words)
Cognition – Executive functioning deficits
Set of mental processes that allow problem-solving to achieve a goal
Includes response inhibition, interference control (selective attention), working memory, cognitive flexibility
Impairments Part 2 Sensory/Perceptual
Sensory-perceptual –
Sensory modulation –
Difficulty regulating and organizing nature and intensity of responses to specific sensory stimuli – tactile, olfactory, visual, auditory, proprioceptive, and vestibular inputs
Under-responsive – slow to respond, fail to react to pain
Over-responsive – Exaggerated responses to input
Sensory seeking – craves for sensory input – stereotypical movements of arm flapping, body rocking etc.
Enhanced/atypical visual and auditory perception –
Enhanced local processing compared to global processing of perceptual information
Unable to understand the “big picture” – get caught up in the details
Enhanced auditory and visual perception – heightened pitch perception, greater pitch discrimination
Impairments Part 3 - Motor
Motor – large effect sizes for motor impairments based on a meta-analysis
Motor stereotypies –
Movements with bodies (rocking, twirling, flapping, bouncing)
Object-related behaviors (spinning, poking, twirling, smelling, atypical peering at objects)
Inflexible routines
Recognize this could be a way to modulate their senses or as a form of communication
Motor delays – GM, FM, and oro-motor delays:
Delayed head holding, rolling, sitting, crawling, walking
Delayed reaching, clapping, scribbling, pointing – FM delays predictive of later communication delays
Limited movement repertoire and transitions
Gait and balance –
Toe walking
Deficits in feedback and feedforward balance
Motor planning, praxis, and imitation
Complex sports, handwriting,
Self-care – dressing, tying laces
Strength and tone
Persistence of abnormal reflexes
Truncal hypotonia
Poor strength – grip strength
Endurance and physical activity levels
High risk for developing obesity (3 times more likely than healthy peers)
Retrospective study – 23.4% older children & adolescents obese; 19% overweight; 35.7% at-risk for obesity
Lower physical activity levels, greater sedentary time
Dietary patterns
Social and motor impairments
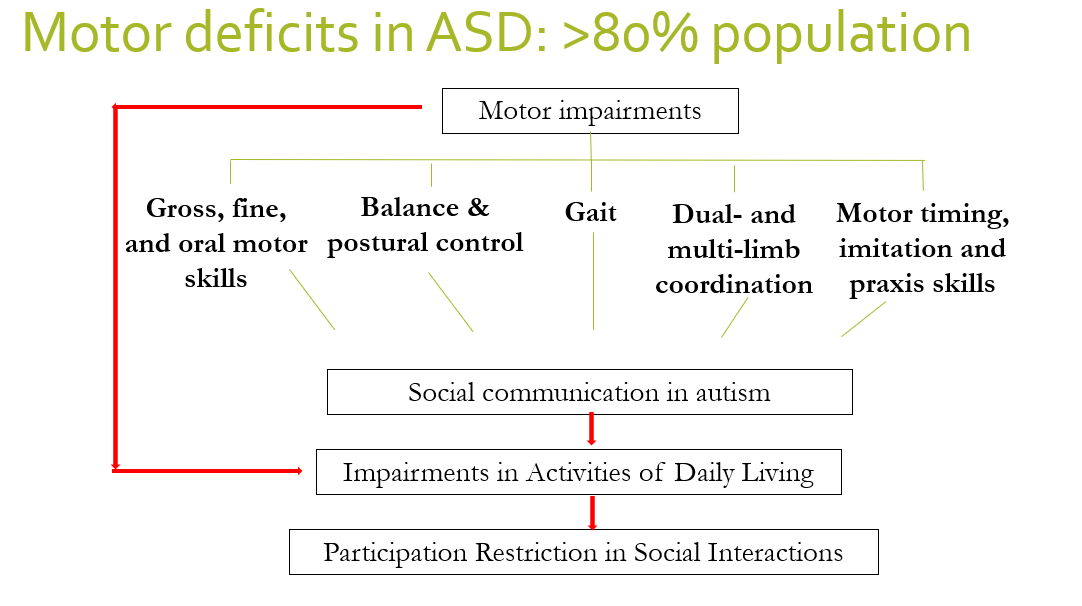
Motor Deficits in ASD
Co-occurring Conditions
•ADHD: 30-61%
•Gastrointestinal disorders (diarrhea, constipation, food regurgitation, food selectivity): 42%
•Sleep disturbances: 50-80%
•Communication disorders: 63.4%
•Motor planning disorders/dyspraxia: 34%
•Obesity & overweight: 32% overweight & 16% obese (2-5-year-olds)
•Toe-walking: 20%
•Sensory processing disorders: 15.7%
•Developmental Coordination Disorder: 18% (although 86.9% fail on the DCDQ)
•Intellectual disability: 18.3%
•Anxiety: 11-40%
•Depression: 7% children, 26% adults
•Schizophrenia: 4-35% adults
•Learning disabilities: 6.3%
•Epilepsy: 16-44%
Diagnosis: Early Screening
Early identification and intervention is related to better outcomes
Earliest signs within the first 2 years in the perceptuo-motor system:
•Gross motor delays –
•Delayed motor milestones, poor head and trunk control, reduced movement repertoire
•Fine motor delays –
•Poor fine motor & object manipulation skills, primitive repetitive manipulation of objects
Commonly used screening tools –
Modified Checklist for Autism in Toddlers (MCHAT) – 16-48 months
Ages and Stages Questionnaire (ASQ) – 1 month to 5.5 years
Social Communication Questionnaire (SCQ) > 4 years
Screening Tool for ASD in Two-year olds (STAT) – 24-36 months
Pervasive Developmental Disorders Screening Test (PDDST-II) – 18-48 months
Diagnosis
Earliest diagnosis by 18 months
Interdisciplinary team – clinical psychologist, developmental pediatrician, psychiatrist, PT, OT, SLP, special educator
Motor
Sensory
Social emotional
Communication – speech, language
Cognition
Adaptive and functional skills
Diagnosis Cont.
History – ask about birth history, family history of ASD, milestones in different domains (motor, communication, social)
Interviews with caregivers – child’s current level of functioning
Observation of child in multiple, naturalistic settings –
Nature of play - variability
Exploration of objects – typical use versus fixated on certain parts
Gross motor skills – positions, transitions, balance, fundamental motor skills, navigating stairs, kicking a ball, ball skills
Fine motor skills – reaching, grasping, in-hand manipulation
Child’s mode of communication (verbal and nonverbal; spontaneous and responsive)
Sensory responses
Intellectual level, cognition, attention
Tools for Diagnosis
Autism Diagnostic Interview- Revised (ADI-R) – parent interview that gains information in language/communication, reciprocal social interactions, and restricted/repetitive behaviors
Autism Diagnostic Observation Schedule (ADOS) – 4 modules + Toddler module
Based on language level and age
Direct observation while making social presses (standardized qualitative assessment)
Score social communication and repetitive behaviors (0-3 scale with 0 being typical or near typical performance)
Childhood Autism Rating Scale (CARS-2) – Direct observation
Physical Therapy Assessment - Motor
Motor:
•Peabody Developmental Motor Scales (0-5 years)
•Bruininks Oseretsky Test of Motor Proficiency (4-21 years)
•Test of Gross Motor Development (3-10 years)
•Movement Assessment Battery for Children (3-16 years)
•Developmental Coordination Disorder- Questionnaire (5-15 years)
•Gait
•Functional skills
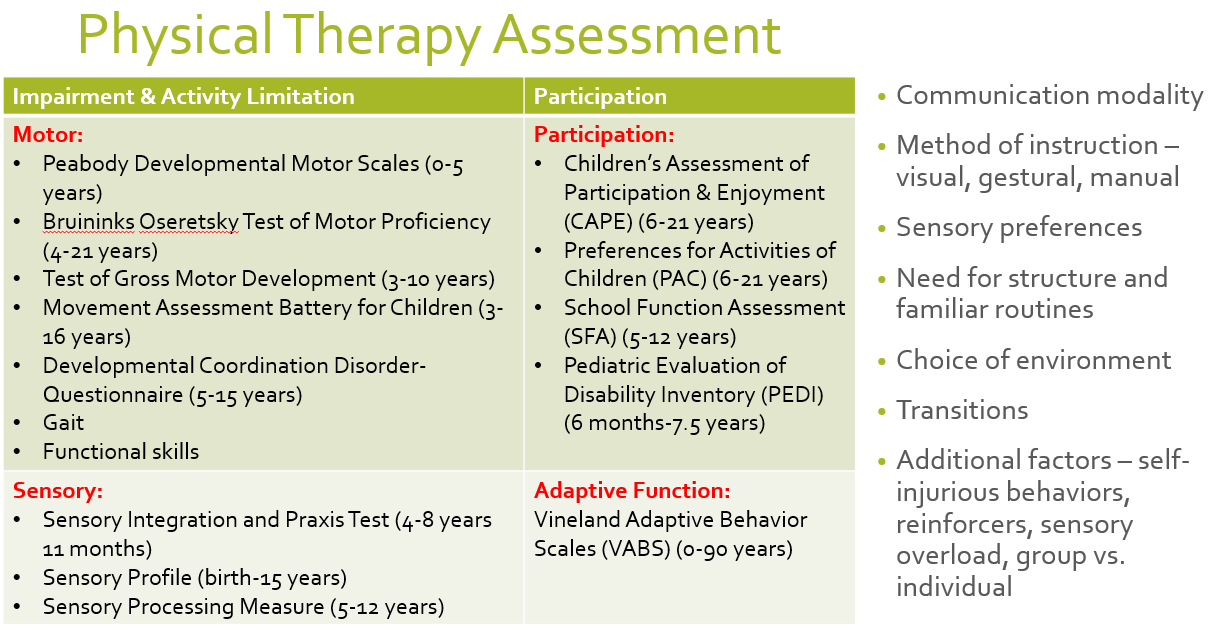
Physical Therapy Assessment - Sensory
Sensory:
•Sensory Integration and Praxis Test (4-8 years 11 months)
•Sensory Profile (birth-15 years)
•Sensory Processing Measure (5-12 years)
Physical Therapy Assessment - Participation and Adaptive Function
Participation:
•Children’s Assessment of Participation & Enjoyment (CAPE) (6-21 years)
•Preferences for Activities of Children (PAC) (6-21 years)
•School Function Assessment (SFA) (5-12 years)
•Pediatric Evaluation of Disability Inventory (PEDI) (6 months-7.5 years)
Adaptive Function:
Vineland Adaptive Behavior Scales (VABS) (0-90 years)
Communication modality
Method of instruction – visual, gestural, manual
Sensory preferences
Need for structure and familiar routines
Choice of environment
Transitions
Additional factors – self-injurious behaviors, reinforcers, sensory overload, group vs. individual
PT Interventions
Early intervention is associated with better outcomes
Individualized treatment program involving families (Individualized Education Program) – focus on child’s strengths and preferences and set goals in collaboration with family
Structured/predictable environments – consistency in environment, therapist, activities, schedule
Use of appropriate communication supports, behavioral supports, reinforcement schedules, motivating activities
Use of modeling strategies, graded prompting, varied practice, peer teaching
Remember multiple professionals – OT, PT, SLP, Special Educator, Behavioral therapist
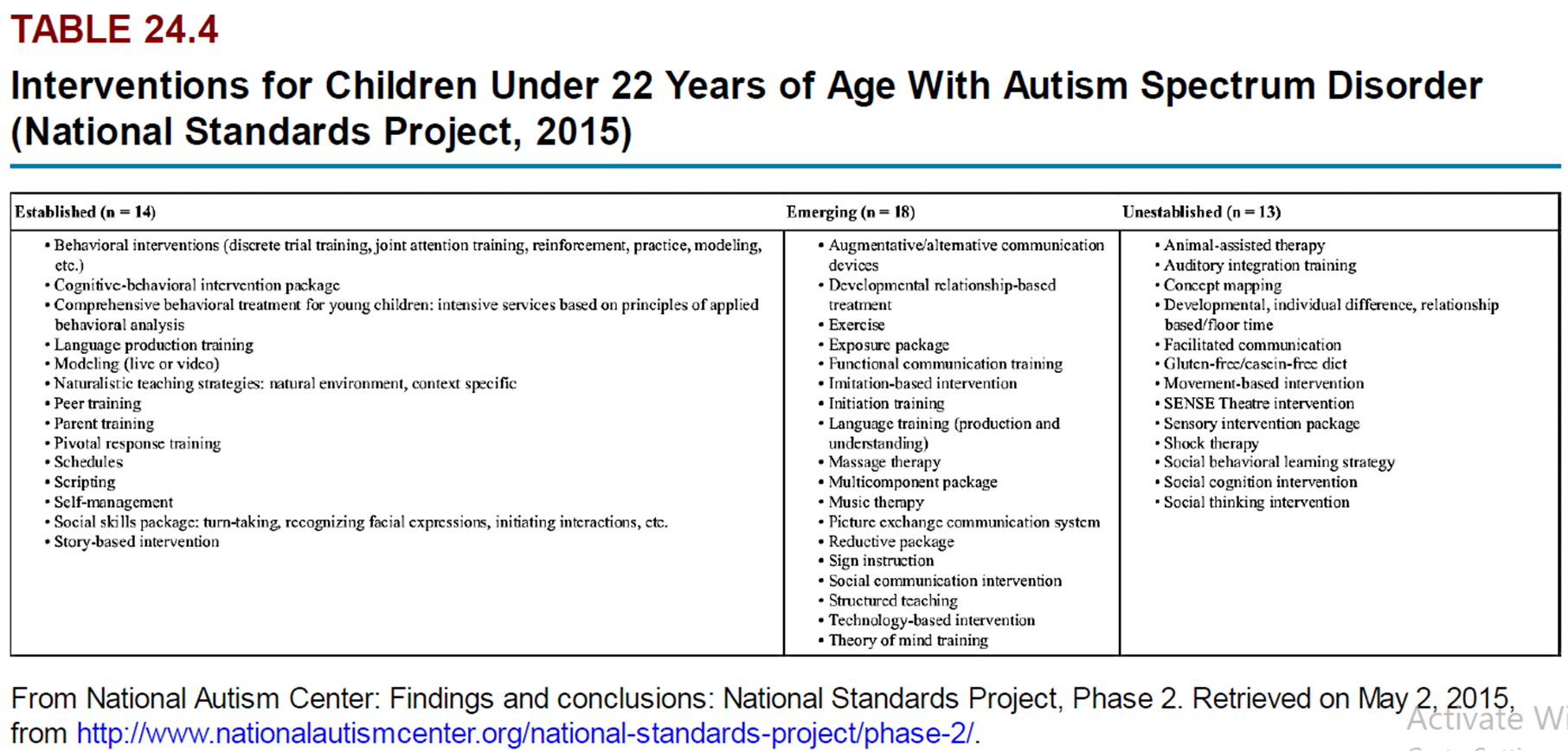
PT Interventions - ABA
Applied Behavior Analysis (ABA) – based on principles of operant conditioning
Reinforce desirable behaviors and reduce undesirable behaviors
Effective in reducing negative behaviors, increasing communication, teaching new skills
Task analysis of skill and teaching individual steps of the skill and providing reinforcement in a predictable manner
Systematic reinforcement schedules
Practice of components as
Discrete trials (discrete trial training – 1:1 blocked practice, controlled environments)
In naturalistic environments (incidental teaching – use child-preferred activities and natural rewards, more motivating)
Ongoing evaluation
Intensive – 40 hours/week one-on-one training
PT Interventions
Picture Exchange Communication System (PECS)
Treatment and Education of Autistic & Related Communication-Handicapped Children (TEACCH) – consistency and predictability in environment, therapists, space, supplies, schedule
Visual Schedules
Augmentative & Alternative Communication
Sensory Integration Approaches
Input modulated by child’s needs – use activities sought by the child
Sensory diet
Use of deep pressure (push-pull, weighted vests, hug machine), activities providing vestibular input (swings, vestibular ball)
Social stories
Targets
Balance
Bilateral coordination
Imitation and praxis
Sensory needs
Strength – core strength
Aerobic capacity and endurance
BMI
Novel modalities
Rhythm and music therapies
Use of technology – Exergaming, Robots
Aquatic interventions
Equine therapies
Yoga, Tai-chi, Martial arts
Cognizant of needs of adults with ASD – continuing needs
Interventions – vocational training, social skill training, behavioral supports
Need for PT interventions directed towards functional training and promotion of physical health, endurance, and fitness
Strategies
Structure in interactions – space, props, people, time of the day
Use picture schedules to help with transitions, rules sheet for behavior
Mode of communication – gestures/sign, AAC, verbal (brief, clear instructions - “Do this”, “copy me”, etc.)
Use props to help clarify instructions, wait for response, give them time to process
Least-to-most prompting (verbal, gestural, physical prompting)
Ensure optimal sensory state – warm-up activities, use of music
Provide modeling, hand-on-hand assistance, as needed
Repetition important, provide opportunities for free play, movement exploration
Provide reinforcement (verbal, gestural, token, earned breaks, healthy edibles)
Progression – start with just-right challenge, look for signs that activity may be too much
If…then
First we work, then we take a break…