Feeding and Energy Balance
1/20
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No study sessions yet.
21 Terms
[REVIEW] What is BMR and what factors affect it
Describe the Determinants of metabolic energy expenditure
What is the difference between Obligatory and Facultative Thermogenesis
BMR = minimum rate of energy production to sustain vital functions in waking state.
Factors:
age
gender
weight
hormonal status
Determinants of metabolic energy expenditure
Resting metabolism (60-75%)
BMR
Sleeping metabolism
Arousal metabolism
Physical Activity (15-30%)
At work
At home
Sports and recreation
Feeding thermogenesis (10%)
Other Factors
Thyroid hormone
Growth hormone
Androgens
Climate
Aging
Sleep
Fever
Stress
starvation
Obligatory vs Facultative
Obligatory thermogenesis:
Energy requiring processes related to assimilating food (motility, secretion, digestion, absorption)
Facultative thermogenesis:
Energy required for activation of the endocrine and ANS and their stimulating effect on:
metabolic substrate mobilization (glycogenolysis and lipolysis),
storage (glycogenesis and lipogenesis)
processing (gluconeogenesis)
Differentiate between the Hunger vs Satiety Center:
Location
Function
Hunger vs Satiety Center:
Hunger Center:
lateral hypothalamic area
Function: Stimulation elicits voracious appetite, even after ingestion of adequate food.
Satiety Center:
ventromedial nucleus (VMN)
Function:elicits sensations of satiety even in the presence of food
Describe Leptin:
Produced by?
Levels Rise in proportion to…
Difference between Leptin and Insulin?
Leptin:
Adipocytes are primary producers of leptin.
Leptin levels rise in proportion the mass of adipose tissue
Leptin vs Insulin:
Leptin: provides long-term feedback on body status
Acute changes in food intake does not affect it
Insulin: provides short-term feedback on body status
Levels change dramatically daily in response to food intake
What is the function of Leptin and mechanism
Leptin = anorexigenic (satiety) signals:
Stimulation decreases fat storage
Adipose tissue uses leptin as a signal to the brain that enough energy has been stored and that intake of food is no longer necessary
Mechanism:
Decreased production in the hypothalamus of appetite stimulators, (NPY and AGRP)
Activation of POMC neurons → release of α-MSH and activation of melanocortin receptors
Increased sympathetic nerve activity (through neural projections from the hypothalamus to the vasomotor centers) → increases metabolic rate and energy expenditure
Decreased insulin secretion by the pancreatic B-cells→ decreases energy storage.
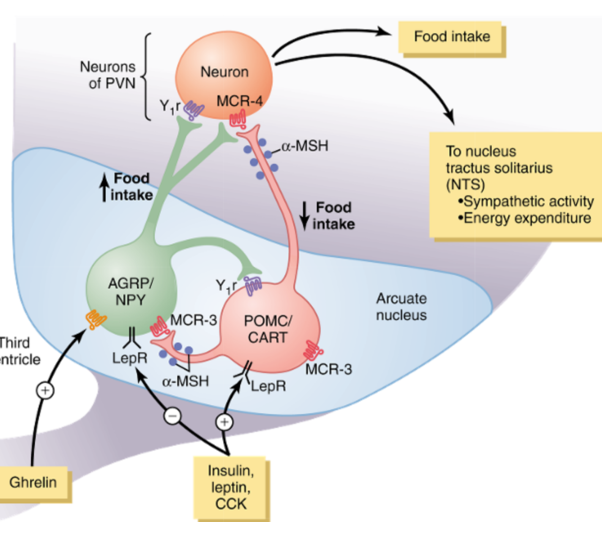
Differentiate between POMC and AGRP/NPY Neurons
Differentiate the effects on these neurons by insulin/leptin/CCK and Ghrelin
POMC:
Releases a-MSH/CART → decreasing food intake and increasing energy expenditure
Mechanism:
POMC → a-MSH → melanocortin receptors @ PVN → NTS → increases sympathetic activity and energy expenditure
AGRP/NPY:
increase food intake and reduce energy expenditure.
acts as an antagonist of MCR-4
Insulin, Leptin, CCK:
Inhibits AGRP/NPY
Stimulates POMC-CART
Thereby reducing food intake
Ghrelin:
Activates AGRP/NPY
Stimulates Food intake
Describe Ghrelin
Orexigenic signal (stimulates appetite): Ghrelin
released mainly by cells of the stomach.
Blood levels of ghrelin rise during fasting, peak just before eating, and then fall rapidly after a meal.
stimulates secretion of growth hormone for GH metabolic effects
What are the short terms anorexigenic signals
Mechanism and Function
CCK and Stretch:
CCK activates receptors on local sensory nerves in the duodenum, → NTS via vagus → satiation and meal cessation.
short-lived
chronic administration of CCK (by itself) = no major effect on body weight.
Function = prevent overeating during meals
NO major role in the frequency of meals or the total energy consumed.
Describe how Glucose affect feeding behavior
Glucose is an independent anorexigenic (satiety) signal:
rise in blood glucose →:
increases rate of firing of gluco-receptor neurons in the satiety center in the ventromedial and paraventricular nuclei of the hypothalamus.
decreases the firing of gluco- sensitive neurons in the hunger center of the lateral hypothalamus.
***NOTE: some amino acids and lipid substances affect the rates of firing of these same neurons or other closely associated neurons.***
[REVIEW] What is Anabolism?
Mechanisms for normoglycemia after a meal
Suppression of hepatic glucose production
Stimulation of hepatic glucose update
Stimulation of glucose uptake by peripheral tissues (muscle)
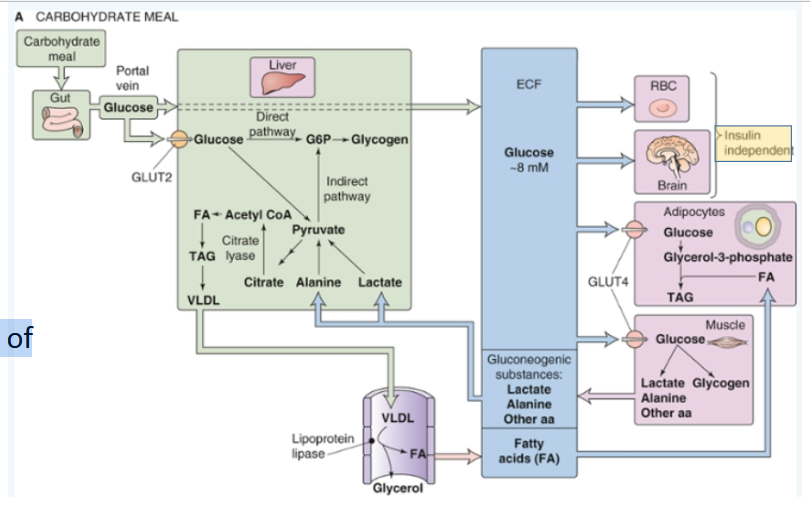
[REVIEW] Energy Capture of Carbohydrates
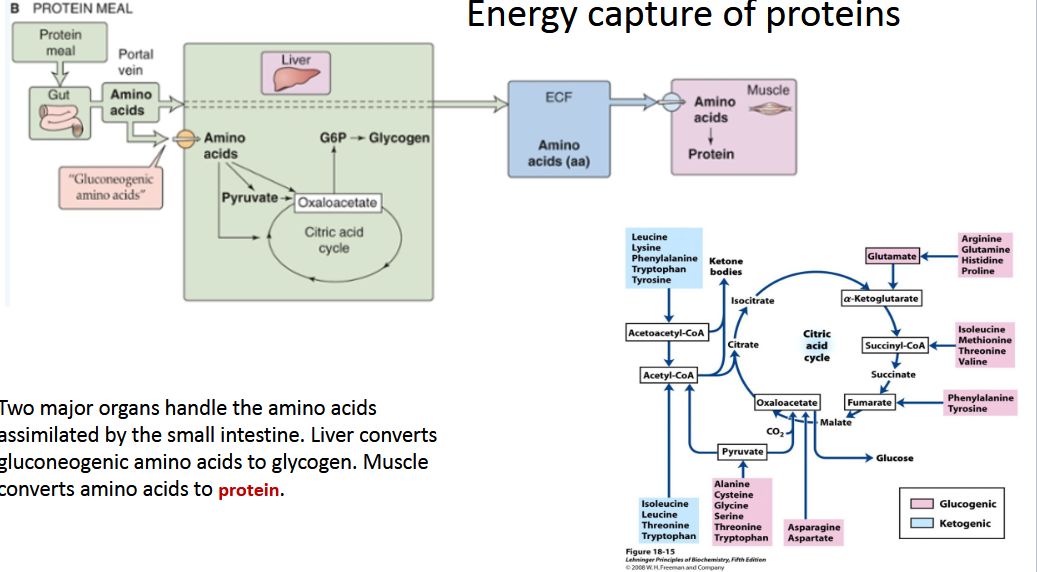
[REVIEW] Energy Capture of Proteins
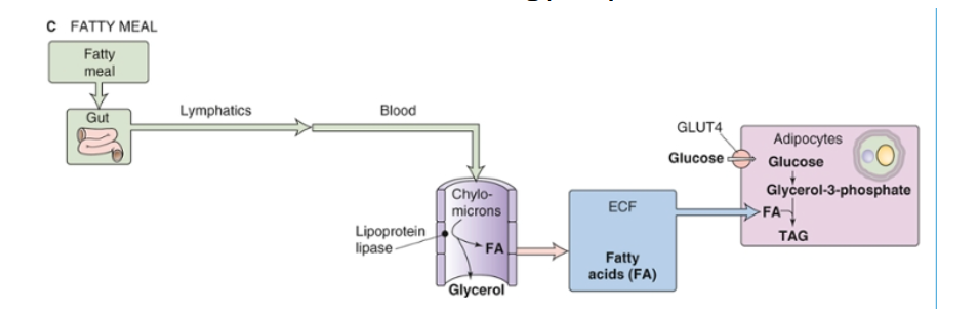
[REVIEW] Energy Capture of Fats
[REVIEW]Describe the catabolic effect of Epi in:
Muscle
Liver
Adipocytes
Muscle:
Epi promotes glycogenolysis and glycolysis
Liver:
glucagon + epinephrine → glycogenolysis (short term glucose) + GNG (Long term Glucose)
Because they have G6Pase, hepatocytes can generate glucose and export it to the blood.
Adipocytes:
Epi → triggers production of FAs and glycerol → Enters Blood
What are the Two priorities during Fasting Metabolism
Describe what is happening during fed/early fasting states?
Prolonged Fasting (>2days)?
2 Priorities:
stable supply of energy for CNS function in the form of glucose or ketone bodies.
Blood-brain barrier impermeable to FA’s
maintain protein reserves
Fed/Early Fasting:
glu is oxidized to meet CNS demands.
this is why the body has redundant mechanisms to maintain Glu between 60-140 mg/dl
other major organs are oxidizing FAs.
prolonged fasting (>2days),
liver metabolizes FA’s to raise levels of ketones for CNS use.
Describe what is happening on an overnight fast
Glucose requirements
fast decline in insulin → FA mobilization.
body still metabolizes glu at 7-10g/hr. Free glu only about 15-20g (2hours).
Body must produce glu at a rate to match ongoing consumption.
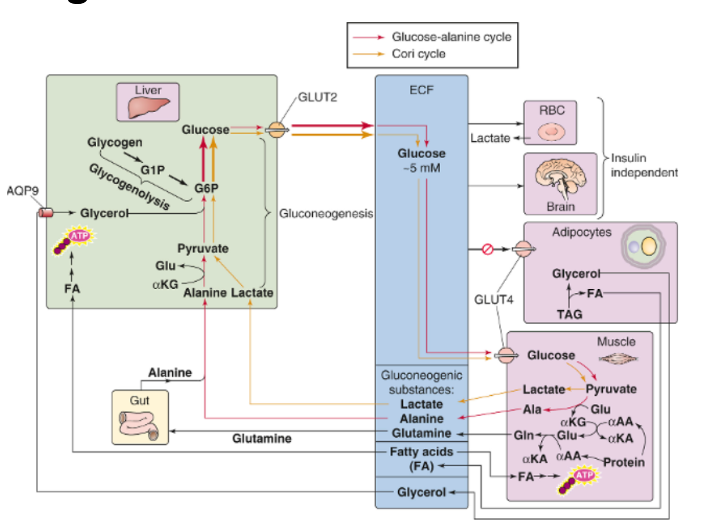
Gluconeogenesis vs. glycogenolysis
4-5 hr post prandial → decreased [insulin] +increased [glucagon] → glycogenolysis and gluconeogenesis (in liver)
Each contribute ~50% of output
Gluconeogenesis:
Cori cycle: glu → lactate + pyruvate → gluconeogenesis
Glucose-Alanine cycle: alanine + glutamine → liver → GNG
Lipolysis:
fall in [insulin] permits release of FA and glycerol from adipocyte
[REVIEW] Metabolism during an Overnight Fast
What happens beyond an overnight fast?
Prolonged fast?
Beyond an overnight fast
Low [insulin] → GNG (liver)
Muscle → proteolysis → alanine + glutamine (glycogenic)
low [insulin] → HSL → more FA and glycerol released from adipocytes.
increased [FA] → insulin resistance in muscle interfering with GLUT 4
Prolonged fast
Hepatic GNG → Renal GNG (up to 40%)
Body decreases use of protein for GNG
Hypoinsulemia + high glucagon → increase hepatic oxidation of FA’s → ketogenesis (liver)
Describe the use of ketones
Synthesized in the liver from FA.
Liver does not have β-ketoacyl CoA transferase so acetoacetate and D-β-hydroxybutyrate enter the blood stream.
CNS, skeletal muscle and cardiac muscle can consume one acetoacetate or one D-β-hydroxybutyrate to produce 2 acetyl- CoA molecules that enter the TCA cycle.
Describe what happen to women during prolonged starvation
As fat stores are depleted → levels of leptin decrease → affects the
Hypothalamic-pituitary- gonadal axis → decreasing LH and FSH → anovulation.
Protects fertile women in times of famine.
Draw out what happens to carbs, fats, and protein levels during starvation
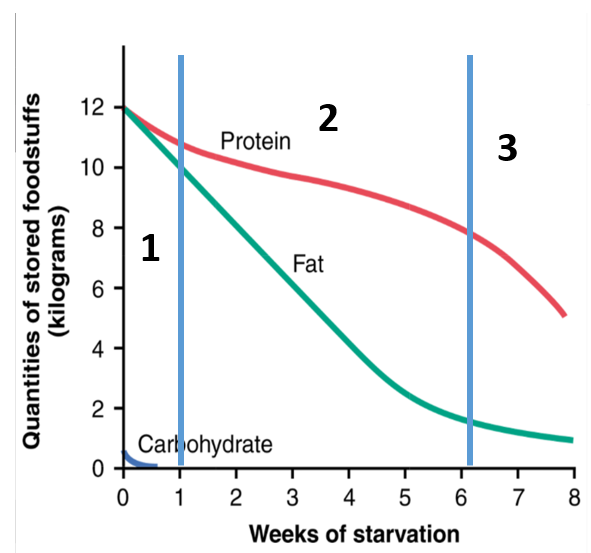
Describe the three phases of protein depletion
initial rapid depletion of easily mobilized protein → direct metabolism or conversion to glucose (mainly for brain)
Slow Depletion:
Rate of GNG decreases to 1/3 to 1/5 → excessive fat utilization and Ketogenesis
Covers two thirds of the brain’s energy (mainly from beta hydroxybutyrate.)
This sequence of events leads to at least partial preservation of the protein stores of the body.
fat stores almost depleted → protein stores once again enter a stage of rapid depletion.
Death ensues when the proteins of the body have been depleted to about half their normal level.